Abstract
Aim
To investigate the complete clinical spectrum of individuals with paediatric tuberous sclerosis complex in southern Sweden and explore changes over time.
Methods
In this retrospective observational study, 52 individuals aged up to 18 years at the study start were followed-up at regional hospitals and centres for habilitation from 2000 to 2020.
Results
Cardiac rhabdomyoma was detected prenatally/neonatally in 69.2% of the subjects born during the latest ten years of the study period. Epilepsy was diagnosed in 82.7% of subjects, and 10 (19%) were treated with everolimus, mainly (80%) for a neurological indication. Renal cysts were detected in 53%, angiomyolipomas in 47%, astrocytic hamartomas in 28% of the individuals. There was a paucity of standardized follow-up of cardiac, renal, and ophthalmological manifestations and no structured transition to adult care.
Conclusion
Our in-depth analysis shows a clear shift towards an earlier diagnosis of tuberous sclerosis complex in the latter part of the study period, where more than 60% of cases showed evidence of this condition already in utero due to the presence of a cardiac rhabdomyoma. This allows for preventive treatment of epilepsy with vigabatrin and early intervention with everolimus for potential mitigation of other symptoms of tuberous sclerosis complex.
Similar content being viewed by others
Introduction
Tuberous sclerosis complex (TSC) is a rare autosomal dominant disorder with almost complete penetrance that affects multiple organ systems [1]. The estimated prevalence of TSC in Sweden is 5.38/100 000 individuals [2]. TSC is caused by loss-of-function variants in tumour suppressor genes either TSC1 or TSC2, which cause upregulation of the mechanistic target of rapamycin1 (mTOR1) signalling pathway [3]. In TSC, mTOR1 signalling pathway disinhibition accelerates cell growth and proliferation, with subsequent growth of hamartomatous tumours in the brain, heart, kidneys, eyes, skin, and lungs [4]. TSC can be diagnosed based on clinical diagnostic criteria, or by finding a pathogenic TSC1 or TSC2 variant, or both [1].
In the last few decades, TSC diagnostics, treatment, and surveillance have advanced markedly [1, 5]. For instance, everolimus, an mTOR-inhibitor (mTORi), has been found particularly efficient for treating subependymal giant cell astrocytomas (SEGA), angiomyolipomas (AML), facial angiofibromas, and epilepsy in TSC patients, if used continuously [6,7,8,9].
Focal seizures and infantile spasms often occur in the first year of life [2, 4] and early seizure onset is associated with intellectual disability (ID) and drug-resistant epilepsy (DRE) in TSC patients [10]. Preventive treatment with vigabatrin, introduced at the first detection of epileptiform activity, before clinical seizure onset, may delay epilepsy onset and decrease its severity [11].
We reviewed the complete TSC clinical spectrum in a Swedish paediatric cohort and investigated changes in diagnostics and treatment over the last two decades. To our knowledge this is the first not registry-based retrospective study of all TSC manifestations in the modern era.
Methods
Patients and setting
All individuals younger than 18 years at the beginning of, or who were born during the study period (January 2000 to December 2020), fulfilling TSC diagnostic criteria, and followed up at the hospitals and centres for habilitation of children and adolescents in southern Sweden (Skåne, Kronoberg, and Blekinge counties), were included. Collected data included demographics, family history of TSC, genetics, clinical manifestations, radiological findings, and treatment. Medical records were reviewed by specialists in the respective areas.
Available echocardiographs and electrocardiograms (ECG) were reviewed for cardiac rhabdomyomas (CRs) and arrhythmias, respectively. The largest CR diameter on the earliest echocardiographic examination was recorded.
From brain images, taken from radiology reports, we recorded cortical tuber, subependymal noduli, SEGA, and hydrocephalus data. The earliest scans were obtained by computed tomography (CT), which was later replaced by magnetic resonance imaging (MRI). SEGA was defined as a caudothalamic groove lesion with a size > 1 cm in any direction, or any subependymal lesion that showed growth on serial imaging, regardless of size [12]. DRE was defined as continuous disabling seizures despite having trialled at least two appropriate antiseizure drugs (ASD) at adequate doses [13]. DRE presence was investigated in four different age-spans: < 5, 5 to < 10, 10 to < 15, and 15–18 years of age. If DRE occurred in any age-span, the individual was defined as having DRE in that period; however, not until having reached the upper limit of the age-group. Data were retrieved regarding epilepsy surgery and included: (1) discussions among colleagues, without further referral to a specialist team, (2) discussions only with the parents, without further referral to a specialist team, and (3) results from structured epilepsy surgery management rounds. We further recorded whether the individual had undergone epilepsy surgery, was accepted for surgical evaluation, or was deemed ineligible for surgery, and if the parents had declined epilepsy surgery despite having been offered this treatment.
Intellectual disability (ID) and neuropsychiatric (NP) disorders were diagnosed using standard psychological testing material. Non-NP linguistic problems were noted. Motor impairment was judged by physiotherapists.
Renal imaging data were taken from the radiology reports and presence of AML and cysts recorded. First and last available creatinine values, urine dipstick results, and blood pressure, if two or more values were available, were recorded. Hypertension was defined as systolic and/or diastolic blood pressure ≥ 95th percentile for sex-, age-, and height-matched children.
Ophthalmological records were reviewed for fundus appearance, electroretinography (ERG), and cerebral visual impairment (CVI). Due to the large spread in age at last available ophthalmologic examination, visual acuity was not compared, as the visual system is not fully developed in growing children.
Statistical method
Data were managed using the Research Electronic Data Capture database hosted by Lund University, Sweden, and were analysed using SPSS v27 software (IBM Corp., Armonk, NY). Data are presented as median and range. Differences between groups were assessed by the Mann–Whitney U test for continuous variables and Pearson Chi-square or Fischer´s exact test, as applicable, for two dichotomous variables. The level of significance was set at p < 0.05.
Ethical consideration
The study was approved by the Swedish Ethical Review Authority and performed in accordance with the declaration of Helsinki.
Results
Characteristics and genetic findings of study individuals are presented in Table 1.
Cardiac manifestations
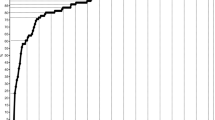
In the total cohort, CRs were detected in 77.5% (31/40) of the individuals, of which 38.7% (12/31) involved prenatal detection. As a feature leading to early diagnosis, CRs were significantly more often found in individuals born during 2010–2020 than in those born during 1983–2009 (p = 0.001) (Fig. 1). Furthermore, 9/13 (69.2%) individuals born during 2010–2020 presented with CRs in the neonatal period and the TSC diagnosis was confirmed within a month (Table 2; Fig. 2). There were significantly more individuals diagnosed prenatally of those born after (80%, 8/10) than before (33%, 4/12) 2010, (p = 0.043). Cardiac manifestations are presented in Table 3. No other cardiac manifestation than rhabdomyomas had a significant difference before and after 2010.
One boy with an intrauterine tentative diagnosis of CRs had pre- and postnatal tachycardia. Postnatal echocardiography confirmed multiple CRs localized in the right atrium and both ventricles, close to the tricuspid valve, completely obstructing the right ventricular (RV) inflow. He received a Blalock–Taussig shunt at 3 days old, which was catheter-closed at 11 months, due to CR regression and pulmonary over-circulation. Another boy had an intrauterine diagnosis of cardiac tumours and supraventricular tachycardia (SVT). A postnatal ECG displayed pre-excitation and SVT and he was treated with digoxin until 1 year old. The largest tumour obstructed RV outflow, necessitating surgical resection at age 1 week. Most CRs underwent spontaneous involution, but at least one remained detectable by 18 years old. Ventricular function was affected in two new-borns: in one, tumour masses occurred in both ventricles and filled the RV, although not necessitating any operative or medical treatment.
Neurological manifestations
Cortical tubers and subependymal nodules were found in 49 and 48/51 subjects (1/52 did not undergo CT or MRI). One individual that showed tubers, but not subependymal noduli, exhibited a mild phenotype with skin lesions and retinal astrocytic hamartomas, without clinical signs of neurological disease.
SEGA was identified in 16/51 (31.4%) individuals. Surgical treatment was performed in four and everolimus treatment was used in seven individuals (Table 4). Hydrocephalus was reported in four, with missing data in 15.
Forty-three individuals (82.7%) had an epilepsy history. Median age at seizure onset was 11 months (range 2–85 months). Twenty-three individuals developed epilepsy before the age of 1 year, of which 15 had infantile spasms. EEG showed hypsarrythmia in 12/15 individuals. Focal seizures were present 1–8 months before infantile spasm onset in 3/15 patients. These spasms developed to seizures with focal onset, either directly, or after a spasm-free period, with a semiology related to the seizure-onset zone. Three individuals had absences and drop attacks suggestive of Lennox–Gastaut syndrome.
Of all individuals with epilepsy, 27/43 (62.8%) had DRE in at least one age-span (Table 5). Among the 25 individuals who turned 18 years old during the study period (thus completing all age-spans), four (16.0%) were never diagnosed with epilepsy and three (14.3%) never developed DRE, whereas seven (33.3%) had DRE across all age-spans. Six (28.6%) of the 25 individuals did not have complete data for all age-spans.
There was no statistically significant difference between those born 1983–2009 and 2010–2020 regarding age of first seizure (p = 0.214), number of patients with infantile spasms (p = 1.0), or number of patients with DRE < 5 years of age (p = 1.0).
Two individuals with West syndrome responded to corticosteroids and nine to vigabatrin treatment. In 1/12 individuals with hypsarrythmia, treatment was unknown. Focal seizures were treated with the following drugs, either alone or in combination: carbamazepine (n = 12), clobazam (n = 11), clonazepam (n = 7), everolimus (n = 10), gabapentin (n = 2), lamotrigine (n = 20), levetiracetam (n = 19), oxcarbazepine (n = 23), perampanel (n = 2), phenobarbital (n = 5), pyridoxin (n = 6), sulthiame (n = 5), topiramate (n = 17), valproic acid (n = 29), vigabatrin (n = 24), and zonisamid (n = 3). Twelve individuals with previous epilepsy were seizure-free at study inclusion, four had discontinued their ASD, and two patients were on monotherapy. In a few individuals, vagus nerve stimulation (n = 2) or ketogenic diet (n = 1) were added, with a marked response. Twelve individuals became seizure-free on ASD monotherapy for more than 2 years. One individual became seizure-free with only a ketogenic diet.
Everolimus treatment
During 2011–2020, 8/10 individuals were treated with everolimus due to neurological indications (Table 4), the youngest being 4.5 months at treatment start. The longest treatment duration was 9.6 years. The mean everolimus concentration varied from 1.6 to 7.2 ng/mL and was generally well tolerated, with gingivitis and hypertriglyceridemia as the most frequently reported side-effects. Two of seven individuals with SEGA showed a tumour size reduction, whereas the rest remained stable. All eight individuals exhibited a decrease in seizure frequency and the number of concomitant ASDs could be reduced in 4/8 individuals.
Vigabatrin treatment
From 2013, 6/7 individuals with a neonatal TSC diagnosis were followed-up with regular EEG (Table 2; individuals 1–7), four of whom developed interictal epileptiform activity prior to clinical seizures. Preventive vigabatrin was initiated in two individuals, one of whom did not develop clinical seizures. There were significantly more individuals with epilepsy treated with vigabatrin after 2010 (10/11) compared to before (13/32), p = 0.004 (Fig. 2) but no significant difference in age of initiating vigabatrin (p = 0.868).
Epilepsy surgery discussion
Table 5 presents data on epilepsy surgery in individuals with DRE and reasons for not proceeding with surgery. Epilepsy surgery was performed in only 5/43 individuals with DRE. Among individuals with DRE across at least two age-groups (n = 14), surgical treatment was never discussed in only one. Among individuals with DRE in only one age-span of DRE, 6/13 never discussed epilepsy surgery. Discussions concerning epilepsy surgery most frequently involved individuals in the age-span 5 to < 10 years (9/14, 64.5%). In a few cases, surgical evaluation was interrupted due to seizure frequency decrease or the initiation of everolimus.
For those born 1983–2009, 4/13 had a discussion about epilepsy surgery before 5 years of age compared to 4/5 for those born 2010–2020 (p = 0.118).
Neuropsychiatric and motor disorders
Normal cognitive function was observed in 23/52 (44%) individuals. Thirteen showed mild, 14 moderate, and two severe ID. Attention deficit disorder (ADHD) was mild in seven and moderate in three, and autism was mild to moderate in 13, and severe in seven. Language impairment, not attributed to ID, autism, or ADHD, was reported in seven individuals, and was severe in two. Neuropsychiatric and cognitive symptoms, collectively known as TAND, were very common in our cohort, but was rarely formally reported in the patient chart. Motor impairment was recognised in 11 (22%) individuals.
An ordinary school program was attended or finished by 23 (44%; two with special support), 20 (38%) were in special schools for individuals with ID, two (4%) had not started school, and data were missing for seven (13%).
Renal manifestations
Appropriate renal imaging was available for 49/52 individuals. Eleven individuals underwent repeat ultrasound (US) examinations, and the remaining individuals underwent both US and MRI or occasionally CT and urography. Median follow-up was 4.83 years (0.25–16.67 years). Median renal lesion-detection age for individuals born during 2010–2020 was 4 months vs. 116 months for those born 1983–2009 (p = 0.0001, Fig. 2). No renal lesions were observed in 6/22 (27.3%) individuals who had passed 18 years of age, and in 4/27 (14.8%) who were younger than 18 years. No renal cell carcinoma was found in this cohort.
AMLs were found in 23 (47%) individuals. These were single in three, multiple unilateral in four, and multiple bilateral in the remaining individuals. Two individuals underwent embolization of asymptomatic large AMLs before everolimus introduction. In one girl, everolimus treatment significantly reduced AML size, as well as multiple small renal cysts. The effect on renal manifestations in individuals treated with everolimus for neurological indications is presented in Table 4.
Renal cysts were detected in 26 (53%) individuals: these were single in five, multiple unilateral in one, and multiple bilateral in the remainder. Contiguous deletion of TSC2/PKD1 was found in one individual, who presented with renal cysts at age 6 months, hypertension at 14 months, and developed a clinical course akin to autosomal dominant polycystic kidney disease. Everolimus treatment was initiated at age 14 years, due to suspicion of AMLs, but was discontinued because of side effects and uncertain benefits. She developed end-stage renal disease and underwent successful kidney transplantation at age 17.5 years. The right kidney removed on this occasion contained multiple AMLs.
Eleven individuals (22.4%) exhibited both renal cysts and AMLs. Small hyperechoic lesions in six individuals, considered as AMLs on US by a radiologist, were interpreted as renal cysts on MRI. In all eight individuals with CRs identified prenatally, renal lesions were detected during the first year of life. Small lesions could not be defined in 3/5 individuals who underwent US during the first month of life. Follow-up investigations showed renal cysts in all these individuals.
Kidney function tests were available for 37 (71%) and blood pressure measurements for 17 (32.6%) individuals. Only the individual with the TSC2/PKD1 deletion was diagnosed with hypertension and decreased kidney function. Urinalysis was available in 15 (28.8%) individuals. Intermittent microscopic haematuria was found in four (one with AML, two with renal cysts and one with no lesions on renal imaging), and proteinuria in one. No proteinuria was found in individuals treated with everolimus.
Renal data were available for 22/25 individuals at 18 years. Ten individuals were transferred for follow-up care under an adult urologist or nephrologist, four to primary care, and two to a neurologist. One individual without renal manifestations was transferred to primary care while the remaining five had no planned follow-up.
Hepatic manifestations
One individual with renal cysts had hepatic cysts. AMLs in both the kidneys and the liver were detected in three individuals. One patient had suspicious, non-defined liver lesions.
Ophthalmological manifestations
Ophthalmological records were available for 50 individuals. At the last registered ophthalmological examination, the median age was 13 (range 1.3–29.7) years. Astrocytic hamartomas in one or both eyes were detected in 16/50 (32%) individuals, and achromatic patches in 4/50 (8%). One individual developed a growing opticus astrocytoma necessitating eye enucleation, and optic atrophy because of SEGA growth. Vigabatrin treatment was used in 23/52 (44.2%). Full-field ERG was performed in 10 patients. Reduced ERG response was measured in 3/10, resulting in medication reduced or cessation. Some recovery was observed at follow-up examination. No individual was investigated for cerebral visual impairment.
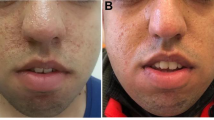
Dermatological manifestations
In many cases, skin manifestations were not documented in detail in medical records and therefore only treatment is presented. Before age 18 years, 11 (21.2%, three missing data) had laser therapy and 11 (21.2%, two missing data) were prescribed topical rapamycin for facial angiofibromas. Of these, six (11.5%, four missing data) underwent both treatments.
Pulmonary manifestations
No lung manifestations were reported in this cohort.
Discussion
As the presenting feature suggestive of TSC, CRs were significantly more commonly detected in individuals born during 2010–2020 than during 1983–2009. A low neonatal diagnostic frequency of CRs in the late nineteen-nineties and early two-thousands has been published previously [14]. A CR was the most common first diagnostic feature (2/3) of children born during 2010–2020, in contrast to seizure onset, which was the presenting TSC feature in > 70% of the older individuals in our cohort. CR led to diagnosis of TSC, within their first month of life, in all children born during the last decade. This is important, as early diagnosis allows identification of emerging problems, such as epilepsy, and provides an opportunity for therapeutic interventions that can potentially alter the disease course [15]. CRs have been diagnosable by foetal ultrasound techniques since 1982 [16], but increasing awareness amongst paediatric cardiologists, improved high-resolution US technologies. Moreover, availability of foetal MRI may explain this significant change during the last 10 years [17].
CRs are usually asymptomatic, but may cause severe morbidity requiring surgical intervention [14], as experienced in two new-borns in this cohort. Pre-excitation was observed in 15% of the individuals, and is a well-known ECG-feature in TSC, where the CR itself is believed to serve as an accessory pathway [18]. Tachycardia was supraventricular in all but one individual, who developed ventricular tachycardia over time. Serial echocardiographic examinations are advised every 1–3 years in the absence of inflow/outflow obstruction and ventricular dysfunction, until the tumour regresses [17]. Thereafter, continued cardiac follow-up with ECG is recommended every 3–5 years [1, 17]. Our study subjects were followed with echocardiography in early life more frequently than these recommendations. However, when cardiac surveillance was stopped, ECG controls also seemed to halt. Echocardiography was the only modality used for cardiac imaging in this retrospective cohort, although MRI is also used [17]. Some case reports indicate successful treatment, with rapid tumour reduction, using both everolimus and sirolimus [19, 20], even for obstructive disease. No patient was treated with mTORi for cardiac indications during the study period; however, we have experience of this as later treatment (Björk Werner, Eklund, personal comm.).
The epilepsy frequency in our cohort (82.7%) agreed with the recently published TOSCA study [21], but was higher than national Swedish data on TSC and epilepsy published by Welin et al. [2]. This may be because epilepsy frequency is overestimated in data from non-population-based studies, as most TSC cohorts, including ours, contain severely affected individuals that require hospital-based care. Furthermore, 34.9% of the epilepsy individuals developed infantile spasms, in line with the TOSCA study [21]. The spasms were the presenting epileptic feature in 80%. Various drugs were used to treat seizures. GABA-potentiating drugs (e.g., valproate, benzodiazepines, barbiturates, and vigabatrin) were predominant (> 40% of prescriptions), similar to the TOSCA study [21]. The use of vigabatrin increased in the most recent decade, in line with recent guidelines [5]. Epilepsy in TSC is often difficult to treat and almost two-thirds had DRE lasting at least one age-span. As epilepsy surgery is the only curative option for DRE, it is noteworthy that half the individuals were never referred for specialist team discussion, thus missing this opportunity. Since 2011, eight individuals were treated with an mTORi for a neurological indication, with an effect both on SEGA growth and seizure frequency. In 4/8 individuals, the number of ASDs could be reduced. ID is often aggravated by DRE. Of our study subjects, 56% fulfilled ID criteria, similar to the findings of the Tuberous Sclerosis 2000 study group [22]. ADHD and autism were also common, but were probably under-appreciated [23], which calls for attention to the related symptoms in daily TSC care.
AMLs and renal cysts were equally observed in this population, as described previously [4, 24]. Renal cysts, however, were found in the first year of life in all individuals with CRs identified prenatally during the latest decade compared to 34,6% of individuals screened for renal lesions in previous decades. Abdominal imaging is mandatory at diagnosis, regardless of age [1]. In our study renal lesions were difficult to define by US during the first month of life. Small AMLs may be hard to distinguish from cysts on US, even in older children, in daily practice [25]. MRI is the preferred modality because of the better structural assessment of the lesions, but requires general anaesthesia in small children and children who are unable to cooperate with the procedure. Progress of renal lesions in our cohort could not be evaluated due to the use of different imaging modalities during the follow-up of the study individuals.
The laboratory analysis and blood pressure measurement showed absence of systematic examination. Both renal cysts and AMLs can cause hypertension and chronic kidney disease with increasing age. Annual assessment of renal function and blood pressure was already recommended in older guidelines [26], and proteinuria assessment has been included in the most recent guidelines [1]. Proteinuria may be a marker of early kidney damage and a potential side effect of mTORi treatment [27, 28]. Everolimus is approved for treatment of asymptomatic growing AMLs > 3 cm in diameter. Some data indicate that mTORi may reduce cyst number and size in individuals with TSC [29], but the effectiveness in TSC-associated renal cystic disease has not yet been fully evaluated. Interestingly, the decreased renal cyst size during everolimus treatment was observed in two individuals in this study.
The occurrence of astrocytic hamartomas and achromatic patches in this paediatric cohort was please merge the text here from the next row somewhat lower than the reported frequency in other cohorts including adults [4]. Of 10 individuals controlled with ERG during vigabatrin medication, retinal effects could be seen in three, with some improvement during the follow-up. Despite involving a small group of individuals, this highlights the importance of closely monitoring these patients for retinal changes. No individual was investigated for CVI problems despite a clear correlation in the literature between neurological ailment and CVI [30]. Ophthalmologists should be encouraged to focus on this diagnosis. Learning ability and quality of life for CVI patients may be substantially improved by a specially trained vision therapist.
Our study has limitations common in retrospective analyses, including incomplete data due to lack of documentation in medical records. No primary healthcare assessment was available and data collection was focused on regional hospitals and centres for habilitation thus some cases with mild disease might have been missed.
Conclusions
This cohort study of TSC individuals from southern Sweden revealed a paradigm shift in TSC diagnosis, in that the finding of CRs on intrauterine US investigations is often the first sign of TSC, allowing early diagnosis. This allows for preventive treatment of epilepsy with vigabatrin and an early intervention with everolimus for potential mitigation of other TSC symptoms. Despite clear and updated treatment guidelines, we found that adequate follow-up is lacking in some areas, the transition from paediatric to adult care is often insufficiently prepared, and TAND data are often missing. These results confirm the previous proposal on the need for involvement of multidisciplinary teams in TSC care.
Data Availability
The datasets generated and analyzed during this study is not publicly available as some of these data will be used for another research study. The datasets can be shared from to the corresponding author by reasonable request.
Abbreviations
- AML:
-
Angiomyolipoma
- ASD:
-
Antiseizure drugs
- ADHD:
-
Attention deficit disorder
- CR:
-
Cardiac rhabdomyoma
- CVI:
-
Cerebral visual impairment
- CT:
-
Computed tomography
- DRE:
-
Drug-resistant epilepsy
- ECG:
-
Electrocardiogram
- EEG:
-
Electroencephalography
- ERG:
-
Electroretinography
- ID:
-
Intellectual disability
- MRI:
-
Magnetic resonance imaging
- mTOR1:
-
Mechanistic target of rapamycin1
- mTORi:
-
mTOR-inhibitor
- NP:
-
Neuropsychiatric
- RV:
-
Right ventricular
- SEGA:
-
Subependymal giant cell astrocytoma
- SVT:
-
Supraventricular tachycardia
- TSC:
-
Tuberous sclerosis complex
- US:
-
Ultrasound
References
Northrup H, Aronow ME, Bebin EM, Bissler J, Darling TN, de Vries PJ, Frost MD, Fuchs Z, Gosnell ES, Gupta N, et al. Updated International Tuberous Sclerosis Complex Diagnostic Criteria and Surveillance and Management Recommendations. Pediatr Neurol. 2021;123:50–66.
Welin KO, Carlqvist P, Svensson A, Althin R, Eklund E, Rask O. Epilepsy in tuberous sclerosis patients in Sweden - Healthcare utilization, treatment, morbidity, and mortality using national register data. Seizure. 2017;53:4–9.
Salussolia CL, Klonowska K, Kwiatkowski DJ, Sahin M. Genetic etiologies, diagnosis, and treatment of Tuberous Sclerosis Complex. Annu Rev Genomics Hum Genet. 2019;20:217–40.
Henske EP, Jozwiak S, Kingswood JC, Sampson JR, Thiele EA. Tuberous sclerosis complex. Nat Rev Dis Primers. 2016;2:16035.
Krueger DA, Northrup H, International Tuberous Sclerosis Complex Consensus G. : Tuberous sclerosis complex surveillance and management: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference. Pediatr Neurol 2013, 49(4):255–265.
Wei CC, Hsiao YP, Gau SY, Wu YT, Wu CT, Wu MH, Tsai JD. The efficacy of Everolimus for Facial Angiofibromas in Tuberous Sclerosis Complex Patients treated for renal Angiomyolipoma/Subependymal giant cell astrocytoma. Dermatology. 2021;237(3):444–9.
French JA, Lawson JA, Yapici Z, Ikeda H, Polster T, Nabbout R, Curatolo P, de Vries PJ, Dlugos DJ, Berkowitz N, et al. Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): a phase 3, randomised, double-blind, placebo-controlled study. Lancet. 2016;388(10056):2153–63.
Franz DN, Belousova E, Sparagana S, Bebin EM, Frost MD, Kuperman R, Witt O, Kohrman MH, Flamini JR, Wu JY, et al. Long-term use of Everolimus in patients with tuberous sclerosis complex: final results from the EXIST-1 study. PLoS ONE. 2016;11(6):e0158476.
Lam HC, Siroky BJ, Henske EP. Renal disease in tuberous sclerosis complex: pathogenesis and therapy. Nat Rev Nephrol. 2018;14(11):704–16.
Chu-Shore CJ, Major P, Camposano S, Muzykewicz D, Thiele EA. The natural history of epilepsy in tuberous sclerosis complex. Epilepsia. 2010;51(7):1236–41.
Kotulska K, Kwiatkowski DJ, Curatolo P, Weschke B, Riney K, Jansen F, Feucht M, Krsek P, Nabbout R, Jansen AC, et al. Prevention of Epilepsy in Infants with Tuberous Sclerosis Complex in the EPISTOP Trial. Ann Neurol. 2021;89(2):304–14.
Roth J, Roach ES, Bartels U, Jozwiak S, Koenig MK, Weiner HL, Franz DN, Wang HZ. Subependymal giant cell astrocytoma: diagnosis, screening, and treatment. Recommendations from the International Tuberous Sclerosis Complex Consensus Conference 2012. Pediatr Neurol. 2013;49(6):439–44.
Kwan P, Arzimanoglou A, Berg AT, Brodie MJ, Allen Hauser W, Mathern G, Moshe SL, Perucca E, Wiebe S, French J. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on therapeutic strategies. Epilepsia. 2010;51(6):1069–77.
Kocabas A, Ekici F, Cetin II, Emir S, Demir HA, Ari ME, Degerliyurt A, Guven A. Cardiac rhabdomyomas associated with tuberous sclerosis complex in 11 children: presentation to outcome. Pediatr Hematol Oncol. 2013;30(2):71–9.
Slowinska M, Jozwiak S, Peron A, Borkowska J, Chmielewski D, Sadowski K, Jurkiewicz E, Vignoli A, La Briola F, Canevini MP, et al. Early diagnosis of tuberous sclerosis complex: a race against time. How to make the diagnosis before seizures? Orphanet J Rare Dis. 2018;13(1):25.
DeVore GR, Hakim S, Kleinman CS, Hobbins JC. The in utero diagnosis of an interventricular septal cardiac rhabdomyoma by means of real-time-directed, M-mode echocardiography. Am J Obstet Gynecol. 1982;143(8):967–9.
Hinton RB, Prakash A, Romp RL, Krueger DA, Knilans TK, International Tuberous Sclerosis, Consensus G. Cardiovascular manifestations of tuberous sclerosis complex and summary of the revised diagnostic criteria and surveillance and management recommendations from the International Tuberous Sclerosis Consensus Group. J Am Heart Assoc. 2014;3(6):e001493.
Emmel M, Brockmeier K, Sreeram N. Rhabdomyoma as accessory pathway: electrophysiologic and morphologic confirmation. Heart. 2004;90(1):43.
Nir-David Y, Brosilow S, Khoury A. Rapid response of a cardiac rhabdomyoma causing severe right ventricular outflow obstruction to Sirolimus in an infant with negative genetics for tuberous sclerosis. Cardiol Young. 2021;31(2):312–4.
Wagner R, Riede FT, Seki H, Hornemann F, Syrbe S, Daehnert I, Weidenbach M. Oral Everolimus for treatment of a Giant Left Ventricular Rhabdomyoma in a Neonate-Rapid Tumor Regression documented by real time 3D Echocardiography. Echocardiography. 2015;32(12):1876–9.
Nabbout R, Belousova E, Benedik MP, Carter T, Cottin V, Curatolo P, Dahlin M, d’Augeres LDA, de Vries GB. Epilepsy in tuberous sclerosis complex: findings from the TOSCA Study. Epilepsia Open. 2019;4(1):73–84.
Tye C, McEwen FS, Liang H, Underwood L, Woodhouse E, Barker ED, Sheerin F, Yates JRW, Bolton PF. Tuberous sclerosis study G: long-term cognitive outcomes in tuberous sclerosis complex. Dev Med Child Neurol. 2020;62(3):322–9.
Vanclooster S, Bissell S, van Eeghen AM, Chambers N, De Waele L, Byars AW, Capal JK, Cukier S, Davis P, Flinn J, et al. The research landscape of tuberous sclerosis complex-associated neuropsychiatric disorders (TAND)-a comprehensive scoping review. J Neurodev Disord. 2022;14(1):13.
Rakowski SK, Winterkorn EB, Paul E, Steele DJ, Halpern EF, Thiele EA. Renal manifestations of tuberous sclerosis complex: incidence, prognosis, and predictive factors. Kidney Int. 2006;70(10):1777–82.
Buj Pradilla MJ, Marti Balleste T, Torra R, Villacampa Auba F. Recommendations for imaging-based diagnosis and management of renal angiomyolipoma associated with tuberous sclerosis complex. Clin Kidney J. 2017;10(6):728–37.
Northrup H, Krueger DA, International Tuberous Sclerosis Complex Consensus G. : Tuberous sclerosis complex diagnostic criteria update: recommendations of the 2012 Iinternational Tuberous Sclerosis Complex Consensus Conference. Pediatr Neurol 2013, 49(4):243–254.
Letavernier E, Legendre C. mToR inhibitors-induced proteinuria: mechanisms, significance, and management. Transpl Rev (Orlando). 2008;22(2):125–30.
Kingswood JC, Bissler JJ, Budde K, Hulbert J, Guay-Woodford L, Sampson JR, Sauter M, Cox J, Patel U, Elmslie F, et al. Review of the tuberous sclerosis renal guidelines from the 2012 Consensus Conference: Current Data and Future Study. Nephron. 2016;134(2):51–8.
Siroky BJ, Towbin AJ, Trout AT, Schafer H, Thamann AR, Agricola KD, Tudor C, Capal J, Dixon BP, Krueger DA, et al. Improvement in renal cystic disease of Tuberous Sclerosis Complex after treatment with mammalian target of rapamycin inhibitor. J Pediatr. 2017;187:318–322e312.
Wan MJ, Chan KL, Jastrzembski BG, Ali A. Neuro-ophthalmological manifestations of tuberous sclerosis: current perspectives. Eye Brain. 2019;11:13–23.
Acknowledgements
Not applicable.
Funding
The study was funded by independent research grants from SUS Stiftelser och Donationer (EA) the Margarethahem Foundation, Stig & Ragna Gorthon Foundation (grant number 2018 − 1468 and 2019–2615) and Region Skåne (KP). ZB acknowledges Skåne Center for Excellence in Health for generous support. Neither of the sponsors had any impact on the study design, data collection, analysis, and interpretation of data, writing the manuscript, or the decision to submit the article for publication.
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
KP, EE, KK, and ZB conceptualized the study. Collection of the data and manuscript draft for respective areas: neurology and neuropsychology: KP, JL, and EK; cardiology: JBW; ophthalmology: LG; nephrology and hepatology: ZB; dermatology: KP. ZB and EE did the overall editing of the manuscript. KK had additional input regarding the conceptualization of epilepsy surgery section.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Swedish Ethical Review Authority (reference no. 2020–05201). Data disclosure was approved by the consultation group for quality registries, care databases, and preparation in Region Skåne (reference no. 214 − 19). As the nature of the study was retrospective, the Swedish Ethical Review Authority waived Informed consent for this study.
The study was performed in accordance with the declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to report.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pearsson, K., Björk Werner, J., Lundgren, J. et al. Childhood tuberous sclerosis complex in southern Sweden: a paradigm shift in diagnosis and treatment. BMC Pediatr 23, 329 (2023). https://doi.org/10.1186/s12887-023-04137-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04137-4