Abstract
Background
Trisomy 18 syndrome (T18) is the second most common autosomal trisomy and has a high risk of fetal loss and stillbirth. Aggressive surgical treatments for the respiratory, cardiac, or digestive systems of patients with T18 were previously futile, while the results of recent studies are controversial. Over the past decade, there have been approximately 300,000 to 400,000 births annually in the Republic of Korea; however, there have been no nationwide studies on T18. This nationwide retrospective cohort study aimed to determine the prevalence of T18 in Korea and its prognosis according to the presence of congenital heart disease and relevant interventions.
Methods
This study utilized NHIS-registered data between 2008 and 2017. A child was defined as having T18 if the ICD-10 revision code Q91.0–3 was reported. Subgroup analysis was performed for children with congenital heart diseases, and survival rates were compared based on the history of cardiac surgical or catheter interventions. The primary outcomes in this study were the survival rate during the first hospitalization period and the 1-year survival rate.
Results
Of the children born between 2008 and 2017, 193 were diagnosed with T18. Of these, 86 died, with a median survival of 127 days. The 1-year survival rate for children with T18 was 63.2%. The survival rate in the first admission of children with T18 who did and did not have congenital heart disease was 58.3% and 94.1%, respectively. Children with heart disease who underwent surgical or catheter intervention had a longer survival time than those who did not.
Conclusions
We suggest these data could be used in ante- and postnatal counseling. Ethical concerns about the prolonged survival of children with T18 remain; however, the potential benefits of interventions for congenital heart disease in this population need further study.
Similar content being viewed by others
Background
Trisomy 18 syndrome (T18) is the second most common autosomal trisomy and has a high risk of fetal loss and stillbirth. The prevalence in live births is estimated as 1/6,000–1/8,000. However, the actual prevalence may be higher (1/2,500–1/2,600) because of the high risk of fetal death and pregnancy termination after prenatal diagnosis [1]. This syndrome is closely associated with preterm delivery, congenital malformations, feeding and breathing difficulties, and high neonatal mortality rates (40–60%) [2, 3]. Recent two population-based studies from the United States (US) have reported the median survival of T18 as 7–8 days, with a 1-year survival rate of 3.0–13.4% [4, 5]. Therefore, aggressive respiratory, cardiac, and digestive system surgical interventions have been regarded as futile by clinicians and parents of children with T18 until the early 2000s.
In contrast, some reports have indicated that the survival rate of children with T18 may increase while receiving active treatment. Data of vital statistics from Japan demonstrated that more surgical interventions provided during 1995–2016 increased the median survival time of children with T18 from 28 to 54 days [3]. A multicentre registry study in the US reported that patients who received cardiac intervention and were discharged from the hospital alive had a median survival rate of 16.2 years [6]. However, decisions for active treatment of T18 are challenging for families and healthcare professionals, as complex ethical issues often emerge during treatment because of their poor prognosis and the need for constant medical support throughout their lives [7].
In 2019, the Constitutional Court in the Republic of Korea (Korea) determined the anti-abortion law unconstitutional officially. Until then, abortion due to fetal disease was illegal [8]. The government started to amend the law, and medical professionals were asked to suggest the criteria for abortion. As the law is revised, the frequency of antenatal consultation for fetal diseases may increase. Therefore, establishing reliable clinical prognoses for this life-limiting condition is required to provide information during antenatal and postnatal consultation. In the last decade, there have been 300,000–400,000 annual births in Korea; however, there have been no nationwide studies on the epidemiology and outcomes of T18. Therefore, this nationwide retrospective cohort study aimed to determine the prevalence of T18 in Korea and its outcomes using the National Health Insurance System (NHIS) database.
Methods
Data source
NHIS data containing demographics, healthcare utilization, and diagnoses based on the International Classification of Diseases, 10th revision (ICD-10), were used in this study. Several studies utilizing the Korean NHIS cohorts have been conducted, and more recently, studies on the long-term outcomes of neonates using the NHIS database have been published [9,10,11,12]. This study was designed and performed according to the principles of the Declaration of Helsinki. The Seoul National University Hospital institutional review board exempted this study from deliberation (E-2207-050-1339) due to its retrospective nature, as it utilized anonymized NHIS data. Permission to access all the data of people born between 2008 and 2017 was provided by the NHIS review committee.
Study population and variables
A child was defined as having T18 if the ICD-10 codes (Q91.0, Q91.1, Q91.2, and Q91.3) were reported during an inpatient admission or visit to outpatient clinics. Follow-up observations of these infants were conducted until December 31, 2018. The type of insurance (national health insurance or medical aid) and the NHIS premium depending on income levels were employed as proxies for measures of income level. The lowest income category was designated as those receiving medical aid. In addition, the NHIS group was split into four groups: category 1, < 25% premium; category 2, 25–50% premium; category 3, 50–75% premium; and category 4, > 25% premium. We reviewed and ranked all ICD-10 codes associated with congenital malformation, deformation, and chromosomal abnormalities (Q codes). A child was defined as having a history of congenital heart disease (CHD) if diagnosed with Q20–26. Heart anomalies that usually regress spontaneously, such as atrial septal defect (ASD) (Q21.1) and patent ductus arteriosus (PDA) (Q25.0), were excluded from CHD codes. Among CHDs, the annual number of children who underwent surgical or catheter intervention (intervention) for CHDs was counted using health insurance claim codes (eTable 1 in Supplement 1). Additionally, the number of children with T18 who had tracheotomy or gastrostomy was counted. The mortality rate was analyzed in two categories. We examined mortality during the first hospitalization period and before 1 year after birth.
Statistical analysis
The study employed Pearson’s chi-square analysis to compare the mortality rates between groups according to the history of cardiac intervention. Kaplan-Meier survival analysis and log-rank tests were utilized to describe long-term survival and compare groups, respectively. In this study, we used a two-sided test with a significance level of p < 0.05 to determine statistical significance. All analyses were performed using SAS (version 9.4; SAS Institute Inc., Cary, NC, USA).
Results
The NHIS database included 193 children diagnosed with T18 who were born between 2008 and 2017. Annually, 12–25 children are diagnosed with T18 (2.7–6.4 per 100,000 births) (Fig. 1). Of these, 86 children died, with a median survival of 127 days. There was no discernible trend in survival rate during the study period. Among these mortality cases, 48 (24.9%) and 71 (36.8%) children died during the first admission and their first year of life, respectively (Tables 1 and 2; Fig. 2). Tracheotomy and gastrostomy were performed in 14 children at a median of 129 and 175 days after birth, respectively (Table 1).
The most common congenital disease codes that children with T18 had were ‘congenital malformations of cardiac septa (Q21)’, which includes ASD and ventricular septal defect; ‘congenital malformations of great arteries (Q25)’, which subsume PDA; ‘congenital deformities of feet (Q66)’; and ‘other congenital malformations of the brain (Q04)’ (eTable 2 in Supplement 1). Except for PDA and ASD, the ventricular septal defect was the most common CHD, followed by coarctation of the aorta and double outflow of the right ventricle (eTable 3 in Supplement 1). Consequently, 108 (56.0%) children with T18 were diagnosed with CHDs, and 47 (43.5%) received cardiac intervention. In 2008 and 2009, few children with T18 underwent heart intervention; however, 23.1–77.8% of children with T18 and CHD underwent intervention from 2010. Only one or two infants underwent a tracheotomy yearly; however, approximately more infants underwent surgery in 2014 and 2017 (3 and 4, respectively).
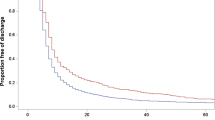
Notably, 94.1% of children without CHD survived until discharge from the first hospitalization. Among patients with heart disease, the survival rate during the first admission for children who underwent intervention was higher than for those who did not (70.2% vs. 49.2%, P = 0.028) (Table 3), with significantly longer survival days (686 days vs. 123 days, P < 0.001) (Fig. 3).
Survival curve for children with trisomy 18 and congenital heart disease in the Republic of Korea. (A) Survival curve for children with trisomy 18 and congenital heart disease. (B) Survival curve and log-rank test for children with trisomy 18 and congenital heart disease based on a history of heart surgery
Discussion
This nationwide population-based study was the largest on intervention and outcomes of children with T18 in Korea. The median survival time of mortality cases was 127 days and the 1-year survival rate was 63.2%, with no evident change in the survival rate for 10 years. Among 108 children with CHD, 47 (43.5%) underwent cardiac intervention, and their survival days were longer than those who did not undergo the intervention.
In this study, 193 children were diagnosed with T18 over 10 years (0.4 per 10,000 births), a lower number than in previous studies conducted in other countries. Approximately 1.5 per 10,000 live births in the US were affected by T18, and multinational research reported that the mean prevalence of T18 among live births was 1.07 (95% CI 0.77, 1.38) per 10,000 births [2, 6]. The low number of births with T18 may be attributed to the relatively higher rate of induced abortion in Korea [13, 14].
The median survival time (25–75 percentiles) of mortality cases was 127 (57, 262) days in our study, which was longer than those in previous studies with similar study periods. A recent study from Japan has reported that the median survival time of children with T18 who were born between 2006 and 2016 was 54 (1–196) days [3]. In another study that analyzed data from children with T18 who were born in the greater Cincinnati area between 2012 and 2018, the median length of survival was 29 days [15]. This phenomenon could be partly explained by more active treatment in Korea. Compared to a population-based study in the United States, the rates at which children with T18 received cardiac intervention and tracheotomy in this study were higher. In the United States study, 7.1% underwent cardiac surgery, and 4.5% underwent tracheostomy [16], whereas, in this study, it was 24.3% (n = 47) and 7.3%, respectively. In the United States, the average age for cardiac procedure and tracheotomy was 0.7 and 1.9 years, respectively. However, in this study, the median ages for these surgeries were 38 days and 129 days after birth, respectively [16]. The direct comparison between the two studies might be inappropriate as the measured values (average and median) were different, and there was a lack of data on the preoperative status of the patients in both studies. However, it was observed that procedures in Korea were relatively performed in the early life stages. Two single referral center studies conducted in Korea reported an increasing proportion of children with T18 receiving active treatment after birth [17, 18]. In one study, positive pressure ventilation and intubation were performed in 79.2% and 54.2% of children with T18, respectively [17]. Furthermore, another study reported that 77.2% were intubated, higher than those in previous studies [18]. Several studies, including the aforementioned Korean single-center studies, have discovered that active intervention in children with T18 increased survival [17,18,19,20,21]. Parents who decide to give birth despite the high rate of abortion in Korea may prefer active interventions for their affected infant. Additionally, as pediatric palliative care was unavailable in Korea until 2017 and advance care planning was not conducted actively, intensive treatment may have been conducted according to the doctors’ intentions [22, 23].
Our study included 108 children with T18 and CHD. In previous studies, there has been debate about the association between CHD and the survival of T18 [24]. However, congenital heart disease is generally known to be a major cause of mortality in T18 [25]. In this study, we observed T18 with ventricular septal defect, coarctation of the aorta, atrioventricular septal defect, and a few cases with complex heart disease (data not shown). Thease heart diseases can be a contributing factor to mortality and the risk may increase if left untreated. Among the patients with T18 and congenital heart diseases, 43.5% underwent cardiac intervention, and the survival rate was higher in this group. This finding still needs cautious interpretation because parents of children with T18 and severe heart disease may have denied receiving active treatment and only desired to provide comfort care for their infants. In a single-center study of prenatal counselling and parental decision-making after a fetal diagnosis of trisomy 13 or 18 from the US, more than half of the families decided to terminate the pregnancy. In contrast, only 2% of the family desired to provide active treatment [26]. Nevertheless, the result of this study was concordant with recent studies reporting that cardiac intervention prolonged survival in children with T18 [6, 27, 28]. When intervention is anticipated to improve patient outcomes, those interventions should be one of the options during the discussion for the patient’s best interest.
Severe developmental delay, long-term dependence on medical equipment, and survival have been considered in deciding on a treatment policy for T18 patients. However, several studies on the quality of life of children with T18 have further indicated that considering the family’s perspective and knowledge of natural history when formulating policies for T18 treatment is crucial. Parents of patients with T18 or trisomy 13 syndrome patients reported that their child was happy and enriched their family despite their children’s severe conditions [29]. In another study in Japan, parents of patients with T18 reported that their children interacted with their parents and siblings throughout their lives, resulting in quality family time, and that the parents were positive about raising their kids [30]. Moreover, parents of patients with T18, who underwent cardiac surgery, rated their child’s quality of life as ‘high.’ Qualitative analysis revealed a profound understanding of the child’s relationality and valued life meaning [31]. Qualitative studies on the quality of life of T18 patients and their families in Korea are required.
This study had some limitations. First, in this study, the observation period varied from 1 year to 11 years due to the children’s different birth years, and ended in December 2018. Although we attempted to mitigate this issue by using a survival curve, there were still limitations to this approach. We acknowledge the limitations of our analysis due to the absence of information on the number of patients at risk at each time point and censoring marks. We had access to this information at the time of analysis, but unfortunately overlooked it and are now unable to retrieve the data. Thus, our presented survival curve may not provide a comprehensive view of the survival outcomes, and readers should interpret our results with caution. Second, we did not have patient information on T18 mosaicism. Patients with T18 mosaicism revealed an extremely variable phenotype; they occupy a small portion of the disease group and may not affect the study’s result [1]. Third, as detailed medical history could not be obtained from national health insurance data, the severity of the disease could not be considered when cardiac interventions were determined. Owing to the nature of the study, there was no data on the decisions made by the clinicians and parents regarding active treatment or comfort care of the patient. These limitations can be overcome by conducting a cohort study and establishing a registry in the future. This is the first study identifying the nationwide prevalence of T18 in Korea and its prognosis. It appears improbable that many children with T18 were omitted from the analysis because approximately 99% of births in Korea occur in hospitals, and physicians have to register ICD-10 codes for reimbursement of medical costs [32]. In addition, the number of children with T18 who died and were identified in this study between 2010 and 2015 (55 children) represented 85.9% of the national death statistics data (64 children), and it was 97.6% between 2012 and 2015 [33].
Conclusion
In this study, fewer children with T18 were reported in the NHIS database in Korea than in other countries; however, many of them received active treatments and had longer survival rates. Recently, advance care planning has been implemented, and the laws regarding abortion have been amended in Korea. Due to these social and legal changes, more ante- and postnatal consultation on T18 treatment are expected, and patient-centered care will be more warranted. Therefore, we expect these data to help determine the disease prognosis and find the best interests for children with T18.
Data Availability
The data that support the findings of this study are available from NHIS but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of NHIS.
Abbreviations
- ASD:
-
Atrial septal defect
- CHD:
-
Congenital heart disease
- NHIS:
-
National Health Insurance System
- PDA:
-
Patent ductus arteriosus
- T18:
-
Trisomy 18 syndrome
References
Cereda A, Carey JC. The trisomy 18 syndrome. Orphanet J Rare Dis. 2012;7:1–14.
Goel N, Morris JK, Tucker D, de Walle HEK, Bakker MK, Kancherla V, et al. Trisomy 13 and 18-Prevalence and mortality-A multi-registry population-based analysis. Am J Med Genet A. 2019;179:2382–92.
Suto M, Isayama T, Morisaki N. Population-based analysis of secular trends in age at death in trisomy 18 syndrome in Japan from 1975 to 2016. Neonatology. 2021;118:47–53.
Vendola C, Canfield M, Daiger SP, Gambello M, Hashmi SS, King T, et al. Survival of Texas infants born with trisomies 21, 18, and 13. Am J Med Genet A. 2010;18:13.
Meyer RE, Liu G, Gilboa SM, Ethen MK, Aylsworth AS, Powell CM, et al. Survival of children with trisomy 13 and trisomy 18: a multi-state population‐based study. Am J Med Genet A. 2016;170A:825–37.
Peterson JK, Kochilas LK, Catton KG, Moller JH, Setty SP. Long-term outcomes of children with trisomy 13 and 18 after congenital heart disease interventions. Ann Thorac Surg. 2017;103:1941–9.
Caines A. Trisomy 18 syndrome: an ethical dilemma in the neonatal intensive care unit. Clin Mother Child Health. 2018;15:2.
Korea Legislation Research Institute. Mother and child health act:article 14; 2009. https://elaw.klri.re.kr/kor_service/lawView.do?hseq=60031&lang=ENG. Accessed 19th September 2022.
Kim JH, Lee JE, Shim SM, Ha EK, Yon DK, Kim OH, et al. Cohort profile: national investigation of birth cohort in Korea study 2008 (NICKs-2008). Clin Exp Pediatr. 2021;64:480–8.
Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the national health insurance service-national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017;46:e15.
Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the national health insurance service-national health screening cohort (NHIS-HEALS) in Korea. BMJ Open. 2017;7:e016640.
Song IG, Kim HS, Cho YM, Lim YN, Moon DS, Shin SH, et al. Association between birth weight and neurodevelopmental disorders assessed using the Korean National Health Insurance Service claims data. Sci Rep. 2022;12:2080.
Ahn HS, Seol HJ, Lim JE, Hong SH, Lee SY, Park MI, et al. Estimates of induced abortion in South Korea: health facilities survey. J Obstet Gynaecol Res. 2012;38:324–8.
World population review. ; 2022. Abortion Rates by Country. https://worldpopulationreview.com/country-rankings/abortion-rates-by-country. Accessed 19th September 2022.
Cortezzo DE, Tolusso LK, Swarr DT. Perinatal outcomes of fetuses and infants diagnosed with trisomy 13 or trisomy 18. J Pediatr. 2022;247:116–123e5.
Katherine EN, Kari RH, Chris F. Inpatient hospital care of children with trisomy 13 and trisomy 18 in the United States. Pediatrics. 2012;129:869–76.
Oh M-Y, Lee BS, Cha T, Jeong J, Jung E, Kim EA-R, et al. Surgical interventions and clinical outcomes of patients with trisomy 18: a single center experience. Perinatology. 2020;31:129–36.
Nam SY, Ahn SY, Chun JY, Yoon SA, Park GY, Choi SY, et al. Survival of patients with trisomy 18 based on the treatment policy at a single center in Korea. Neonatal Med. 2014;21:251.
Dotters-Katz SK, Carlson LM, Johnson J, Patterson J, Grace MR, Price W, et al. Management of pregnancy and survival of infants with trisomy 13 or trisomy 18. Am J Perinatol. 2016;33:1121–7.
Subramaniam A, Jacobs AP, Tang Y, Neely C, Philips JB III, Biggio JR, et al. Trisomy 18: a single-center evaluation of management trends and experience with aggressive obstetric or neonatal intervention. Am J Med Genet A. 2016;170A:838–46.
Jacobs AP, Subramaniam A, Tang Y, Philips JB III, Biggio JR, Edwards RK, et al. Trisomy 18: a survey of opinions, attitudes, and practices of neonatologists. Am J Med Genet A. 2016;170:2638–43.
Song IG, Kang SH, Kim MS, Kim CH, Moon YJ, Lee J. Differences in perspectives of pediatricians on advance care planning: a cross-sectional survey. BMC Palliat Care. 2020;19:145.
Kim CH, Song IG, Kim MS, Lee JY, Lim NG, Shin HY. Healthcare utilization among children and young people with life-limiting conditions: exploring palliative care needs using National Health Insurance claims data. Sci Rep. 2020;10:1.
Rasmussen SA, Wong LYC, Yang Q, May KM, Friedman JM. Population-Based analyses of Mortality in Trisomy 13 and Trisomy 18. Pediatrics. 2003;111:777–84.
Palani Kumar B, Indira Priya DA. Edwards syndrome. StatPearls [Internet]; 2022. https://www.ncbi.nlm.nih.gov/books/NBK570597/.
Winn P, Acharya K, Peterson E, Leuthner S. Prenatal counseling and parental decision-making following a fetal diagnosis of trisomy 13 or 18. J Perinatol. 2018;38:788–96.
Nelson KE, Rosella LC, Mahant S, Guttmann A. Survival and surgical interventions for children with trisomy 13 and 18. JAMA. 2016;316:420–8.
Janvier A, Farlow B, Barrington K. Cardiac surgery for children with trisomies 13 and 18: where are we now? Semin Perinatol. 2016;13:254–60.
Janvier A, Farlow B, Wilfond BS. The experience of families with children with trisomy 13 and 18 in social networks. Pediatrics. 2012;130:293–8.
Kosho T, Kuniba H, Tanikawa Y, Hashimoto Y, Sakurai H. Natural history and parental experience of children with trisomy 18 based on a questionnaire given to a japanese trisomy 18 parental support group. Am J Med Genet A. 2013;161A:1531–42.
Weaver MS, Birge N, Hsu H, Woell C, Robinson JE, Wichman C, et al. Mixed method study of quality of life for children with trisomy 18 and 13 after cardiac surgery. Cardiol Young. 2020;30:231–7.
Birth data. (Population trends) [Internet]. Micro Data Integrated Service; 2022. https://mdis.kostat.go.kr/dwnlSvc/ofrSurvSearch.do?curMenuNo=UI_POR_P9240#. Accessed 19th September 2022.
Birth. and death link data [Internet]. Micro Data Integrated Service; 2015. https://mdis.kostat.go.kr/dwnlSvc/ofrSurvSearch.do?curMenuNo=UI_POR_P9240. Accessed 19th September 2022.
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: Song IG, Shin SH.
Data curation: Cho Y-M, Lim Y.
Formal analysis: Cho Y-M, Lim Y.
Investigation: Song IG, Shin SH.
Writing - original draft: Song IG.
Writing - review & editing: Song IG, Cho Y-M, Lim Y, Shin SH.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was designed and performed according to the principles of the Declaration of Helsinki. The Seoul National University Hospital institutional review board exempted this study from deliberation and waived the need for informed consent (E-2207-050-1339) due to its retrospective nature, as it utilized anonymized NHIS data. We were allowed to access all data of people born between 2008 and 2017 by the NHIS review committee.
Consent to publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, I.G., Shin, S.H., Cho, YM. et al. Survival of children with trisomy 18 associated with the presence of congenital heart disease and intervention in the Republic of Korea. BMC Pediatr 23, 252 (2023). https://doi.org/10.1186/s12887-023-04056-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04056-4