Abstract
Aim
To assess the etiologies and adverse outcomes of infantile acquired hydrocephalus and predict prognosis.
Methods
A total of 129 infants diagnosed with acquired hydrocephalus were recruited from 2008 to 2021. Adverse outcomes included death and significant neurodevelopmental impairment which was defined as Bayley Scales of Infant and Toddler Development III score < 70, cerebral palsy, visual or hearing impairment, and epilepsy. Chi-squared was used to evaluate the prognostic factors of adverse outcomes. A receiver operating characteristic curve was calculated to determine the cutoff value.
Results
Of 113 patients with outcome data, 55 patients (48.7%) had adverse outcomes. Late surgical intervention time (13 days) and severe ventricular dilation were associated with adverse outcomes. The combination of surgical intervention time and cranial ultrasonography (cUS) indices was a better predictive marker compared with any of them (surgical intervention time, P = 0.05; cUS indices, P = 0.002). Post-hemorrhage (54/113, 48%), post-meningitis (28/113, 25%), and hydrocephalus arising from both hemorrhage and meningitis (17/113, 15%) accounted for a large proportion of the etiologies in our study. Hydrocephalus occurs secondary to post-hemorrhage and had a favorable outcome compared with other etiologies in both preterm and term groups. A significant difference in adverse outcomes between the inherited error of metabolism as a cause and other etiologies (P = 0.02).
Conclusion
Late surgical treatment times and severe ventricular dilation can predict adverse outcomes in infants with acquired hydrocephalus. It is crucial to identify the causes of acquired hydrocephalus to predict the adverse outcomes. Research into measures of improving adverse outcomes following infantile acquired hydrocephalus is urgently necessary.
Similar content being viewed by others
Introduction
Infantile hydrocephalus is a life-threatening condition resulting from excess cerebrospinal fluid accumulation in the ventricles of the brain. At a rate of approximately 0.7-1 every 1,000 live births, infantile hydrocephalus is not uncommon [1, 2]. In infants, hydrocephalus without an obvious extrinsic cause is referred to as congenital hydrocephalus [3]. Hydrocephalus occurring as a complication of another condition is called acquired hydrocephalus. The predominant forms of acquired hydrocephalus are posthemorrhagic hydrocephalus (PHH), which comprises approximately half of all neonatal hydrocephalus cases, followed by postinfectious hydrocephalus, and tumor-related hydrocephalus [4]. Neurodevelopmental outcomes in terms of social and neurocognitive function in congenital hydrocephalus have been reported [5, 6]. Although many studies have evaluated the long-term outcomes and short-term follow-up of post-hemorrhagic hydrocephalus (PHH) and postinfectious hydrocephalus for preterm neonates, [7,8,9] other etiologies and their prognostic predictors are rarely mentioned. Few studies have discussed the prognostic factors in predicting the neurodevelopmental outcomes of acquired infantile hydrocephalus [10].
Our study aimed to investigate the different causes of infantile hydrocephalus and determine the adverse outcomes and prognostic factors in infants (18 months) at our center, which is a referral center for hydrocephalus in northern China.
Materials and methods
Study design
This study conducted a retrospective analysis from the Peking University First Hospital between January 1st, 2008, and January 1st, 2021. Informed consent was obtained from the parents or legal guardians to participate in the study. Ethics approval for this study was granted by the Medical Ethics Committee of Peking University First Hospital.
Enrollment criteria were: (1) Hydrocephalus diagnosed based on clinical findings (large head, bulging anterior fontanel, suture separation, sunset phenomenon of the eyes, bradycardia, or hypotonia) and radiological features. The diagnostic criteria for infantile hydrocephalus are defined as the ventricular index (VI) > 97th centile. The following measurement indices were used for comprehensive evaluation [11]: anterior horn width > 4 mm, thalamo-occipital distance (TOD) > 26 mm and third ventricular width (TVW) > 3 mm (all > 1 mm over the 97th centile). Ventricular height (VH) (> 15 mm) was also measured because it was crucial for enhanced sensitivity to ventricular size, independently of subependymal hemorrhage in the anterior and occipital horns. (2) All patients performed routine cerebrospinal and/or ventricular fluid testing, and urine gas chromatography mass spectrometry and blood liquid chromatography-tandem mass spectrometry for detecting metabolic diseases. (3) Complete regular follow-up until 18 months or die within 18 months. Exclusion criteria were: severe perinatal brain injury from hypoxic-ischemic encephalopathy, brain damage followed by hypoglycemia, bilirubin encephalopathy, etc.
Meningitis, as an etiology, was represented as proven meningitis and suspected meningitis. Proven meningitis was defined as the detection of bacteria from cerebrospinal fluid (CSF) by culture. Suspected meningitis was defined as a negative CSF culture with all the following clinical signs and symptoms of meningitis (temperature instabilities, lethargy, respiratory distress, apnea, jaundice), and changes in the cerebrospinal fluid (CSF pleocytosis (> 30 × 106/L), lower initial CSF glucose (< 1.1mmol/L) and higher protein (> 2 g/L)).
Hydrocephalus management
Infants meeting enrollment criteria were monitored using cranial ultrasonography (cUS) and daily clinical assessments of the head circumference and anterior fontanel. Surgical intervention time is defined as the period of time from hydrocephalus diagnosis to the date of surgical intervention at our center.
Temporizing neurosurgical procedures (TNPs) were performed upon the surgeon’s discretion depending on whether the head circumference and cUS indices increased despite serial LPs or for VI over P97 + 4 mm [12]. The TNPs involved ventricular access devices or an Ommaya reservoir, external ventricular drainage (EVD), and ventriculosubgaleal shunts. The temporary measures aimed at reducing ventricular dilation by draining or aspirating 10–20 ml/kg of cerebral spinal fluid (CSF) daily, by continuous cUS monitoring.
The patients were treated with individualized temporizing measures to drain the CSF before permanent diversion via a ventriculoperitoneal shunt (VPS). VPS was offered in cases of continuous progressive hydrocephalus, such as those characterized by neurological deterioration, increased head circumference, and increased measurement indices on successive cUS under TNPs [13]. A detailed flowchart of infantile hydrocephalus management was shown (Fig. 1). All cUS was performed by an experienced technician following the guidelines of neurosonography in neonates and infants.
Flowchart of infantile hydrocephalus management
Definition of nonprogressive hydrocephalus: (1) the measurement indices are stable or decreased upon the latest continuous cranial ultrasonography (cUS) and (2) clinical manifestations include a large head, bulging anterior fontanel, suture separation, irritability, sunset phenomena of the eyes, and hypotonia, without neurological deterioration. Temporizing neurosurgical procedures (TNPs) were performed upon the surgeon’s discretion if the head circumference and cUS measurement indices increased. The surgical intervention time was according to the reference ventricular index (VI) value for the corrected age at hydrocephalus onset less than or equal to 40 weeks [30]. The VI greater than 18.5 mm (P97th + 4 mm at 40 week) or persistent progressive cUS indices with neurological deterioration were the surgical intervention time for the patients at onset corrected age greater than 40 weeks. TNPs include ventricular access devices or Ommaya reservoir, external ventricular drainage, and ventriculosubgaleal shunts. The appropriate technique was selected based on the surgeon’s discretion. The TNPs aimed at reducing ventricular dilation by draining or aspirating 10–20 ml/kg of cerebrospinal fluid daily as per continuous cUS monitoring and clinical assessment. Moreover, it is crucial to evaluate intraoperative and postoperative complications.
Abbreviation: cUS, cranial ultrasonography; VP, ventriculoperitoneal; VI, ventricular index; CA, corrected age
Clinical outcomes at corrected age of 18 months
Patient follow-up evaluations included physical examination (including head circumference, body length, and weight) and cranial ultrasound scans (performed by two professional neonatologists at a corrected age of 3, 6, 9, 12, and 18 months). All hydrocephalus infants evaluated in our center are subjected to a preventive management approach, as they are considered to have a high risk in terms of neurodevelopmental problems. Professional rehabilitation physicians provide a thorough evaluation and intervention (physiotherapy and infant stimulation of early intervention, teaching the parents exercises with the baby at home) for these infants during a stable period of the disease. The rehabilitation planned for infantile hydrocephalus would be an individual program of the best choice. Surviving infants were evaluated using the Bayley Scales of Infant and Toddler Development III (BSID-III), by certified examiners who were blinded to neonatal clinical variables during the follow-up period. BSID-III includes cognitive, language, and motor subscales and a score of < 70 represented a performance of 2SD or more below the mean [14].
A diagnosis of cerebral palsy is usually made between 12 and 24 months of age when there were clinical findings of impaired movement, posture, or balance, and the impairment is permanent and nonprogressive. Hearing impairment was defined as permanent hearing loss affecting language acquisition, education, and overall wellbeing. Visual impairment was defined as visual acuity less than 6/12 in better eyes [15]. Epilepsy is characterized by an enduring predisposition for epileptic seizures, diagnosed by electroencephalography (EEG) or neuroimaging.
Significant neurodevelopmental impairment (sNDI) was defined by having one or more of the following: a BSID score of < 70, epilepsy, cerebral palsy, and visual or hearing impairment.
Statistical analysis
Statistical analysis was performed using SPSS Statistics version 26.0 (SPSS Inc., Chicago, Illinois, USA) and MedCalc version 20.0.3 (MedCalc Software Ltd., Belgium). Continuous variables (such as age, birth weight, and CSF value) with normal distribution are presented as mean ± SD. Categorical variables are presented as frequency (percentage) and were compared using Pearson’s chi-squared or Fisher’s exact test for small samples. Significance was set at p < 0.05. A receiver operating characteristic (ROC) curve was calculated to determine the cutoff value (maximizing Younden’s index) of the measurement indices in cUS and the earliest treatment time.
Results
Over the 12 years, 137 infants were diagnosed with hydrocephalus at our hospital. Among these, 8 were considered to have congenital hydrocephalus and 16 were lost to follow-up at the time of data collection. Finally, 113 patients with outcome data were included in the analysis (Fig. 2). Of 113 cases, 55 patients (48.7%) had adverse outcomes (sNDI and death), and 58 (51.3%) did not. The baseline characteristics of the study group cases are shown in Table 1.
The multivariate analysis of the favorable vs. adverse groups was presented in Table 2. Variables including age at presentation, the occurrence of convulsions, and biochemical indicators of CSF were not significantly associated with neurodevelopmental outcomes. 18 cases in our study were considered spontaneous arrests. Of these, 6 patients had sNDI (6/55, 10.9%), and 12 (12/58, 20.7%) did not. 79 cases required TNP as the primary intervention. 33 (42%) patients need further permanent diversion due to the hydrocephalus progression. No significant difference (p = 0.16) in adverse outcomes was found between the two groups. Of the 54 cases of hydrocephalus of post- hemorrhagic etiology, cUS revealed that 48 involved Papile grade 3 hemorrhage and 6 involved grade 4 hemorrhage; grade 4 hemorrhage was associated with poorer outcome (p = 0.036).
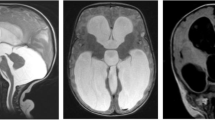
A significant difference in the surgical intervention time existed between the favorable and unfavorable groups: 12.5 ± 9.9 and 33.7 ± 38.1 days, respectively (p = 0.002). A cutoff point of 13 days was determined for surgical intervention time, with a sensitivity of 0.77 and specificity of 0.72. The differences in TVW and bilateral VI, VH, and TOD on cUS between the two groups were significant (Fig. 3). The mean cutoff points of VI, VH, and TOD were 2.13, 1.80, and 2.75 cm, respectively. The combination of surgical intervention time and cUS indices had a better predictive value compared with any of them (surgical intervention time, P = 0.05; cUS indices, P = 0.002).
ROC analysis of cranial ultrasound indices and surgical intervention time.
Fig. 3. (A) (B) (C) (D) Receiver operating characteristics (ROC) curves demonstrating the ability of TVW and both sides of VI, VH, and TOD in predicting the adverse outcomes of significant neurodevelopmental impairment and death. (E) ROC curves demonstrating the ability of surgical intervention time (SIT), summary of cranial ultrasonography (cUS) indices, and SIT & cUS indices in predicting the adverse outcomes. There were significant differences in the area under the curves (AUCs) between measurements of SIT and SIT & cUS indices (P = 0.05), cUS indices and SIT & cUS indices (P = 0.002).
Abbreviations: VI, ventricular index; VH, ventricular height; TOD, thalamo-occipital distance; TVW, third ventricular width; AUC, area under the curve; SE, standard error; SIT, surgical intervention time
The etiologies and outcome analysis of the preterm vs. term groups were shown in Table 3. Post-hemorrhagic (n = 54 of 113; 48%), post-meningitic (n = 28 of 113; 25%) and hydrocephalus arising from both hemorrhage and meningitis (n = 17 of 113; 15%) accounted for a large proportion of the etiologies. Preterm infants acquire hydrocephalus caused by post-hemorrhage (37/59, 62.7%), meningitis (15/59, 25.4%), and both post hemorrhage and meningitis (7/59, 11.9%), and differing from the term cases with various etiologies (post-hemorrhage, 17/54, 31.4%; meningitis, 13/54, 24.1%; both post hemorrhage and meningitis, 10/54, 18.5%; inherited errors of metabolism, 11/54, 20.4%; tumor/cyst/mass lesions, 3/54, 5.6%). No significant difference was found in outcomes between the preterm and term groups. Totally, 31 patients with sNDI were in our study group. Of these, 13 patients with epilepsy (all cases have development delay evaluated by Bayley scales), 4 with hearing impairment (3 of them have cognitive or language impairment), 3 with visual impairment (1 patient has a global developmental delay, 1 has language impairment delay), and 1 case with cerebral palsy.
Figure 4 presents the proportion of adverse outcomes in term and preterm groups by etiology. The proportions in the preterm group of the adverse outcomes in post-hemorrhagic, post-meningitic, and both post-hemorrhagic and post-meningitic hydrocephalus were 41%, 46%, and 57%, which is higher than the term groups 35%, 39%, and 40%.
A total of 45 patients had a post-meningitic etiology, and 22 of these had a proven meningitis, including Escherichia coli (n = 10), Listeria monocytogenes (n = 4), Enterococcus Faecium (n = 3), Staphylococcus (n = 2), Klebsiella pneumoniae, group B beta-hemolytic Streptococcus and Enterobacter cloacae (all n = 1). Ten of eleven patients with hydrocephalus from inherited metabolic diseases had poor prognoses (90.9%). Among these, nine patients were diagnosed with methylmalonic aciduria and homocystinuria (MMA-HC, all are cblC type), one was diagnosed with glutaric acidemia type 1, and another patient had an unknown origin with hypertrophic cardiomyopathy, rhabdomyolysis, and liver damage. The mean value of homocysteine in the nine patients with MMA-HC was 120.8 ± 48.9µmol/L. Three patients had tumor/cyst/mass lesions as etiology (arachnoid cyst = 2, intracranial cyst = 1).
General outcomes of different etiologies
Tumor/cyst/mass lesion were rare cases; therefore, they were not counted.
Numbers and proportions of the adverse outcomes were shown in the bar chart. The proportions in preterm group of the adverse outcomes among with post-hemorrhagic, post-meningitic, and both post-hemorrhagic and post-meningitic hydrocephalus were 41%, 46%, and 57%, respectively. The proportions of term group in among those with post-hemorrhagic, post-meningitic, both post-hemorrhagic and post-meningitic hydrocephalus, and hydrocephalus from inherited metabolic diseases were 35%, 39%, 40%, and 91%, respectively. Significant difference in adverse outcome proportion between inherited error of metabolism as a cause and other etiologies (P = 0.02).
Discussion
Infantile hydrocephalus is a relatively common but severe complication that predicts childhood neurodevelopmental risk. The association between hydrocephalus and poor long-term neurodevelopmental outcomes has been proven, [16] but the analysis of prognostic factors is limited. In this study, we report a general adverse outcomes rate of 48.7%. Late treatment times and ventricular dilation had relatively poor outcomes but were not associated with sex, age at presentation, convulsion at onset, EEG findings, and glucose, protein, and chloride levels in CSF. Besides, the combined measurements of surgical intervention time and cranial ultrasonography indices have a better predictive value for adverse outcome evaluation.
Recent studies have shown that infants with post-hemorrhagic ventricular dilatation require timely treatment for better neurodevelopmental outcomes [13]. These data support the retrospective study of Bassan et al. [17] that suggested early (< 25 days of life) external ventricular drainage (EVD) was associated with low rates of cognitive and communication disabilities than later EVD in infants with post-hemorrhagic hydrocephalus. The timing of drain implantation longer than 1 month after hydrocephalus is diagnosed might be a risk factor for poor mental and linguistic developmental outcomes [18]. However, a cutoff point of 13 days was determined for surgical intervention time in infantile acquired hydrocephalus, with 0.77 sensitivity and 0.72 specificity on ROC analysis. This supports the evidence that infants requiring treatment should be evaluated and operated on promptly on time.
Ventriculomegaly is associated with an increased risk of both cognitive and motor sequelae due to periventricular brain injury [1, 8] This suggests a direct association to prolonged pressure and indirectly, to ischemia and inflammation, leading to damage of white matter from which no recovery capacity exists [19]. A team had succeeded in predicting hydrocephalus outcomes in premature neonates using a cUS-based phenotyping tool [20]. However, these findings are difficult to apply in clinical practice. Herein, we prove that severe ventricular dilation is associated with adverse outcomes, and describe the cutoff point for the VI (2.13 cm), VH (1.80 cm), TOD (2.75 cm), and TVW (1.03 cm).
PHH is a common complication of IVH, and the PHH rate varies between 18% and 35% [21,22,23]. Adverse outcomes are related to the severity of IVH as the first significant risk factor for PHH. Our results are concordant with findings of reports stating that neurodevelopmental outcomes are worse for grade 4 IVH. Hydrocephalus has been rarely reported in adults with bacterial meningitis, but it is more common in younger children, especially in infants aged < 6 months [24]. 36–63% of patients with bacterial meningitis had a confirmed bacterial etiology [24,25,26]. In our study, 22 of the 45 patients (49%) with post-meningitic hydrocephalus had a definite pathogen. Of these, 45% reported E coli as the pathogenic bacteria, followed by L.monocytogenes (7.7%) and E.faecium (5.8%). Pediatricians in clinical practice should pay attention to infants who with above positive bacterial cultures for acquired hydrocephalus.
Hydrocephalus has rarely been reported as a sequela of inherited metabolic diseases [1]. MMA is a typical organic acidemia caused by defects in methylmalonyl-coenzyme A mutase or adenosyl-cobalamin synthesis; it is also the most common metabolic cause of hydrocephalus in China [27]. The MMACHC gene is the cause of the cblC type, which is the most common subtype always accompanied by homocysteine, of which, the main toxic effect is arterial wall injury; it further reduces the compliance of extracerebral intracranial arteries [27]. Herein, we describe 9 cases of MMA with hydrocephalus, all belonging to the cblC type with homocystinuria (120.8 ± 48.9µmol/L). A Dutch study [28] reported that in a patient with glutaric acidemia type 1 (GA-1) developing ventriculomegaly (9 in 18 individuals with GA-1), characteristically, the acute encephalopathic crisis and movement disorders also occurred. Thus, neurological imaging tests should be performed in patients with metabolic diseases.
Hydrocephalus etiologies were strongly associated with significant neurodevelopmental impairment and mortality. Generally, compared to infants with hydrocephalus caused by other etiologies (infection, congenital malformation, spina bifida), the risk of adverse outcomes was markedly higher in patients with PHH, [10, 29] especially premature infants, which may be due to the ischemic or inflammatory injuries to periventricular brain structure [8, 18]. However, in this study, relatively favorable outcome observed in PHH compared with other etiologies except for the influences of prematurity and hemorrhage combined with central nervous system infection. Infantile acquired hydrocephalus caused by an inherited error of metabolism had a poorer outcome in this limited sample retrospective study and needs to pay more attention.
We are a tertiary referral center, and the sickest hydrocephalic infants from our province and adjoining regions are referred to our hospital. Most cases of delayed surgical intervention were outborn patients because they could not be referred due to severe conditions or refusal from parents, or because hydrocephalus could not be diagnosed early due to lack of regular monitoring. Early detection and intervention (besides surgical procedures) discussed by multiple disciplines with neonatologist, neurosurgeon, physiatrist, and child health doctor was taken for the patients. It likely leads to a better outcome for hydrocephalic infants.
Our study has some limitations. The first is the early endpoint of neurodevelopmental follow-up. Taking the progressive trajectories and longer follow-up of the neurobehavioral development as the child grows is essential for an accurate appraisal. Second, the use of different strategies in individual neurodevelopmental evaluation in the interpretation of outcomes is a limitation of this retrospective study. Finally, heterogeneous etiology was also a limitation of this study. Research into different adverse outcomes of specific etiologies for these patients is urgently required. Previous studies have found that the common causes of acquired hydrocephalus in infants are hemorrhage, neoplasm, and infection, usually bacterial meningitis [1, 3]. The reasons for the difference may be the selection bias of the inclusion criteria for the neonatal units and the high rate of critical disease at our referral center.
Conclusions
This study provides a comprehensive analysis of the prognostic factors related to infant hydrocephalus, as evaluated at our center over the last 12 years. We found that PHH had a relatively favorable outcome compared with other etiologies except for the influences of prematurity and hemorrhage combined with meningitis. Late surgical intervention time and severe ventricular dilation have relatively adverse outcomes. Further research to reduce the incidence and severity of hydrocephalus in infants and improve their subsequent neurodevelopmental outcomes is urgently needed.
Data Availability
All data generated or analyzed during this study are included in the submission. The raw data are available from the corresponding author on reasonable request.
References
Kahle KT, Kulkarni AV, Limbrick DD, Warf BC. Hydrocephalus in children. The Lancet. 2016;387:788–99. https://doi.org/10.1016/s0140-6736(15)60694-8.
Blackburn BL, Fineman RM. Epidemiology of congenital hydrocephalus in Utah, 1940–1979: report of an iatrogenically related “epidemic. Am J Med Genet. 1994;52:123–9. https://doi.org/10.1002/ajmg.1320520202.
Tully HM, Dobyns WB. Infantile hydrocephalus: a review of epidemiology, classification and causes. Eur J Med Genet. 2014;57:359–68. https://doi.org/10.1016/j.ejmg.2014.06.002.
Dewan MC, Rattani A, Mekary R et al. Global hydrocephalus epidemiology and incidence: systematic review and meta-analysis. J Neurosurg. 2018:1–15 doi: https://doi.org/10.3171/2017.10.JNS17439.
Kutscher A, Nestler U, Bernhard MK, et al. Adult long-term health-related quality of life of congenital hydrocephalus patients. J Neurosurg Pediatr. 2015;16:621–5. https://doi.org/10.3171/2015.4.PEDS15106.
Gmeiner M, Wagner H, Schlogl C, et al. Adult outcome in shunted Pediatric Hydrocephalus: Long-Term Functional, Social, and neurocognitive results. World Neurosurg. 2019;132:e314–e23. https://doi.org/10.1016/j.wneu.2019.08.167.
Kulkarni AV, Schiff SJ, Mbabazi-Kabachelor E, et al. Endoscopic treatment versus shunting for Infant Hydrocephalus in Uganda. N Engl J Med. 2017;377:2456–64. https://doi.org/10.1056/NEJMoa1707568.
Dorner RA, Burton VJ, Allen MC, Robinson S, Soares BP. Preterm neuroimaging and neurodevelopmental outcome: a focus on intraventricular hemorrhage, post-hemorrhagic hydrocephalus, and associated brain injury. J Perinatol. 2018;38:1431–43. https://doi.org/10.1038/s41372-018-0209-5.
Schiff SJ, Kulkarni AV, Mbabazi-Kabachelor E et al. Brain growth after surgical treatment for infant postinfectious hydrocephalus in Sub-Saharan Africa: 2-year results of a randomized trial. J Neurosurg Pediatr. 2021:1–9 doi: https://doi.org/10.3171/2021.2.PEDS20949.
Mohamed M, Mediratta S, Chari A, et al. Post-haemorrhagic hydrocephalus is associated with poorer surgical and neurodevelopmental sequelae than other causes of infant hydrocephalus. Childs Nerv Syst. 2021. https://doi.org/10.1007/s00381-021-05226-4.
Whitelaw A, Aquilina K. Management of posthaemorrhagic ventricular dilatation. Arch Dis Child Fetal Neonatal Ed. 2012;97:F229–3. https://doi.org/10.1136/adc.2010.190173.
Valdez Sandoval P, Hernandez Rosales P, Quinones Hernandez DG, Chavana Naranjo EA, Garcia Navarro V. Intraventricular hemorrhage and posthemorrhagic hydrocephalus in preterm infants: diagnosis, classification, and treatment options. Childs Nerv Syst. 2019;35:917–27. https://doi.org/10.1007/s00381-019-04127-x.
Leijser LM, Miller SP, van Wezel-Meijler G, et al. Posthemorrhagic ventricular dilatation in preterm infants: when best to intervene? Neurology. 2018;90:e698–e706. https://doi.org/10.1212/WNL.0000000000004984.
N B. Bayley Scales ofInfant Development. 3rd ed. San Antonio, TX: The Psychological Corporation. 2006.
Wei S, Sun Y, Li SM, et al. Visual impairment and spectacle use in University students in Central China: the Anyang University Students Eye Study. Am J Ophthalmol. 2019;206:168–75. https://doi.org/10.1016/j.ajo.2019.04.026.
Melot A, Labarre A, Vanhulle C, et al. Neurodevelopmental long-term outcome in children with hydrocephalus requiring neonatal surgical treatment. Neurochirurgie. 2016;62:94–9. https://doi.org/10.1016/j.neuchi.2015.10.009.
Bassan H, Eshel R, Golan I, et al. Timing of external ventricular drainage and neurodevelopmental outcome in preterm infants with posthemorrhagic hydrocephalus. Eur J Paediatr Neurol. 2012;16:662–70. https://doi.org/10.1016/j.ejpn.2012.04.002.
Heinsbergen I, Rotteveel J, Roeleveld N, Grotenhuis A. Outcome in shunted hydrocephalic children. Eur J Paediatr Neurol. 2002;6:99–107. https://doi.org/10.1053/ejpn.2001.0555.
Brouwer MJ, de Vries LS, Kersbergen KJ, et al. Effects of Posthemorrhagic Ventricular Dilatation in the Preterm Infant on Brain volumes and White Matter Diffusion variables at term-equivalent age. J Pediatr. 2016;168:41–9e1. https://doi.org/10.1016/j.jpeds.2015.09.083.
Tabrizi PR, Mansoor A, Obeid R, et al. Ultrasound-based phenotyping of lateral ventricles to Predict Hydrocephalus Outcome in premature neonates. IEEE Trans Biomed Eng. 2020;67:3026–34. https://doi.org/10.1109/TBME.2020.2974650.
Kazan S, Gura A, Ucar T, Korkmaz E, Ongun H, Akyuz M. Hydrocephalus after intraventricular hemorrhage in preterm and low-birth weight infants: analysis of associated risk factors for ventriculoperitoneal shunting. Surg Neurol. 2005;64 Suppl 2:S77-81; discussion S doi: https://doi.org/10.1016/j.surneu.2005.07.035.
Alan N, Manjila S, Minich N, et al. Reduced ventricular shunt rate in very preterm infants with severe intraventricular hemorrhage: an institutional experience. J Neurosurg Pediatr. 2012;10:357–64. https://doi.org/10.3171/2012.7.PEDS11504.
Gilard V, Chadie A, Ferracci FX, et al. Post hemorrhagic hydrocephalus and neurodevelopmental outcomes in a context of neonatal intraventricular hemorrhage: an institutional experience in 122 preterm children. BMC Pediatr. 2018;18:288. https://doi.org/10.1186/s12887-018-1249-x.
Huo L, Fan Y, Jiang C, et al. Clinical features of and risk factors for Hydrocephalus in Childhood bacterial meningitis. J Child Neurol. 2019;34:11–6. https://doi.org/10.1177/0883073818799155.
Ouchenir L, Renaud C, Khan S, et al. The Epidemiology, Management, and outcomes of bacterial meningitis in infants. Pediatrics. 2017;140. https://doi.org/10.1542/peds.2017-0476.
Xu M, Hu L, Huang H, et al. Etiology and clinical features of full-term neonatal bacterial meningitis: a Multicenter Retrospective Cohort Study. Front Pediatr. 2019;7:31. https://doi.org/10.3389/fped.2019.00031.
Zhang K, Gao M, Wang G, et al. Hydrocephalus in cblC type methylmalonic acidemia. Metab Brain Dis. 2019;34:451–8. https://doi.org/10.1007/s11011-018-0351-y.
Vester ME, Visser G, Wijburg FA, van Spronsen FJ, Williams M, van Rijn RR. Occurrence of subdural hematomas in dutch glutaric aciduria type 1 patients. Eur J Pediatr. 2016;175:1001–6. https://doi.org/10.1007/s00431-016-2734-6.
Tully HM, Doherty D, Wainwright M. Mortality in pediatric hydrocephalus. Dev Med Child Neurol. 2022;64:112–7. https://doi.org/10.1111/dmcn.14975.
Levene MI. Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch Dis Child. 1981;56:900–4. https://doi.org/10.1136/adc.56.12.900.
Acknowledgements
The authors would like to thank the patients and all clinicians who provided data in our center.
Funding
This study was funded by Young Scientists Fund of the NSFC (82101806), Beijing Municipal Science & Technology Commission (Z211100002921050), National Key Research and Development Program of China (2021YFC2700700), Capital’s Funds for Health Improvement and Research (2022-3-40715), and National High Level Hospital Clinical Research Funding (2022CR68).
Author information
Authors and Affiliations
Contributions
Faliang Zhou, Zhao Yang and Zezhong Tang contributed equally. Xinlin Hou and Lili Liu conceptualized this study and were in charge of follow-up upon discharge. Faliang Zhou and Zhao Yang are responsible for analyzing the data and writing the manuscript. Congle Zhou, Yi Jiang, Yang Zhang, Hongmei Wang, Guoyu Sun, Rui Zhang are responsible for collecting the data, as well as being coordinators for parents and doctors. Xinlin Hou and Lili Liu are both corresponding authors in this study. All authors reviewed the manuscript. The authors have no conflicts of interest to declare.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work was carried out in accordance with the World Medical Association’s Helsinki Declaration. Ethics approval for this study was granted by the Medical Ethics Committee of Peking University First Hospital. Informed consents of participants were obtained from their parents or guardians in this study.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, F., Yang, Z., Tang, Z. et al. Outcomes and prognostic factors of infantile acquired hydrocephalus: a single-center experience. BMC Pediatr 23, 260 (2023). https://doi.org/10.1186/s12887-023-04034-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04034-w