Abstract
Background
Globally, child mortality is remaining high, especially in sub-Saharan African countries like Ethiopia. Mortality which happens within 24 hours of admission is preventable. However, in Ethiopia little is known regarding pediatric emergency mortality. Therefore, this study was aimed to identify determinants of pediatric emergency mortality at compressive specialized hospitals found in South Nation Nationalities and people region, Southern Ethiopia.
Methods
A facility-based unmatched case-control study was conducted on 344 children (115 cases and 229 controls) at comprehensive specialized hospitals of South Nation Nationalities and people region, Ethiopia. The data collection checklist was checked for its consistency. Data were entered and cleaned for missed values by using Epi Data3.1, then exported to Stata version 14.1 for analysis. Logistic regression was done to identify the significant determinants for pediatric emergency mortality. Finally, AORs at 95% CI and P-value < 0.05 were used to declare statistical significance.
Result
A total of 344 charts were reviewed, of which 333 (97%) (112 cases and 221 controls) charts fulfilled the inclusion criteria.. In multivariable analysis, delayed diagnosis and treatment [AOR = 2.088, 95% of CI (1.128, 3.864)], acute respiratory distress syndrome [AOR = 2.804, 95% of CI (1.487, 5.250)], dehydration [AOR = 3.323, 95% of CI (1.260, 8.761)], meningitis [AOR = 5.282, 95% of CI (2.707, 10.310)], sepsis [AOR = 4.224, 95% of CI (2.220, 8.040)], accidental injury [AOR = 3.603, 95% of CI (1.877, 6.916)] and duration of sign/symptoms [AOR = 5.481, 95% of CI (2.457, 12.230)] were significantly associated with pediatric emergency mortality.
Conclusion
In the current study, delayed diagnosis and treatment, acute respiratory distress syndrome, dehydration, sepsis, meningitis, accidental injury and duration of signs/symptoms were significantly associated with pediatric emergency mortality. Healthcare professionals should identify and treat patients early at an emergency department and provide attention to patients with the above diseases. Furthermore, quality care should be provided.
Similar content being viewed by others
Introduction
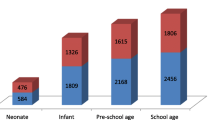
The child mortality rate remains high globally with around 3.1 million neonates, 2.3 million infants, and 2.3 million childhood deaths occurring every year. The mortality rate in children younger than 5 years has dropped [1]. However, the distribution of death in children fewer than 5 years of age is still high; 50% in Sub-Saharan Africa [2]. In Africa, the childhood mortality rate is 15 times more than well-resourced countries [3].
In low-income countries, most of the mortality which happens in the first 24 hours of admission is preventable [4]. Sub-Saharan African facilities have higher patient load and mortality than other regions particularly for pediatric emergency (PE) patients [5].
Out of 60 countries characterized as having high childhood mortality, Ethiopia is among the eight [6, 7]. If situations continue like this, more than 3,084,000 children will die by 2030. Child mortality rate range from as low as 39 per 1000 live births in Addis Ababa to as high as 125 per 1000 live births in Afar [8]. In Ethiopia, over the five-year study period, 4.1% of deaths were recorded at pediatric emergency department. Approximately 32% of the deaths were occurred within ≤24 hours of arrival in PED [9].
Pediatric emergency mortality is one of the most challenging problems for clinicians and a very painful issue in the community. In Ethiopia, Emergency triage assessment and treatment (ETAT) was initiated to decrease the pediatric emergency mortality. However, the mortality is still high [10].
In our country, there are several published articles which conducted to assess the magnitude and factors of under-five and neonatal mortality. However, there is a scarcity of data on determinants of pediatric mortality, especially within 24 hours of admission. Therefore, this study was aimed to identify the determinants of pediatric emergency mortality in the pediatric emergency unit.
Method
Study area and period
This study was conducted from Jun 20, 2022 - July 24, 2022 in all comprehensive specialized hospitals of Sothern Nation’s nationalities and peoples region (SNNPR), Ethiopia. SNNPR is one of the administrative regional states in Ethiopia. It is the third largest region in an area out of 11 administrative regions in Ethiopia. It is also the most diverse region in the country in terms of culture, language and ethnicity. There are three comperhensive specialised hospitals in the region. All comperhensive hospitals (Wolaita Sodo University comperhensive specialised hospital (WSUCSH), Wachamo university Nigist Eleni Mohammad memorial comprehensive specialized hospital (WUNEMMCSH) and worabe comprehensive specialized hospital (WUCSH) were included in this study.
WSUCSH is located in Sodo town of Wolaita Zone, which is 380 km away from the national capital. The hospital is serving more than 2 million people in the catchment area in since 1928. The T#town has 28,499 under- five age children and 4576 infants less than 1 year of age [11]. WUNEMMCSH is located in the Hadiya Zone which is 232 kms far from Addis Ababa. Worabe comprehensive specialized hospital is found in the Silte Zone. Worabe town is located 172 kms away from Addis Ababa. It has an estimated total population of 29,600, of which 4618 are under-five children [12].
Study design
An institution-based unmatched case-control study design was employed to identify determinants of pediatric emergency mortality in all comprehensive specialized hospitals of SNNPR, Ethiopia.
Source population
All children admitted to pediatric emergency units of all comprehensive specialized hospitals of SNNPR, Ethiopia.
Study population
All children who died within 24 hr. of admission to the emergency department for the case groups.
All children who survived 24 hrs emergency unit admission in all comprehensive specialized hospitals of the south region for the control group.
Inclusion and exclusion criteria
Inclusion
This study included children aged 29 days to 14 years who died and were discharged within 24 hrs of emergency unit admission.
Exclusion
Children with self-discharge (against clinical the decision), children died at arrival and charts of children who died in the intensive care unit (ICU) and pediatric ward were excluded.
Sample size determination
The sample size was calculated by Epi-Info version 7.2.5 statistical software designed for an unmatched case-control studies. The following assumptions were considered during sample size calculation a 95% level of confidence, a power of 80%, and a case to control ratio of one to two (1:2) with a 2.1 odds ratio. By taking the duration of signs and symptoms ≥2 days as an independent exposure variable which gives the largest sample size [9]. The final sample size after adding a 10% non-response rate was 344 (115 cases and 229 controls).
Sampling technique and sampling procedure
A systematic random sampling technique was used to select children’s card. The total number of pediatric mortality and discharge at ETAT during the data collection period was estimated from the registration book. Total pediatric mortality within 24 hrs (Cases) in Wachamo, Wolaita Sodo and Worabe respectively were 147, 125 and 73 with a total of 345 children in 2 years. The number of children included in the study from each hospital was calculated using the proportionate to size (PS) allocation technique as follows; ni = (n/N) Ni, where ni = sample size of each hospital, n: total sample size, Ni: population of each hospital and N: total population of three hospitals.
Therefore, based on the above formula sample size for cases from Wachemo, Wolaita Sodo and Worabe hospitals were 49, 42 and 24, respectively. Totally it gives 115 cases. Cases. To get the individual sample units (patient card who died within 24 hours), systematic random sampling technique was used with \(\textrm{K}=\left(\frac{N}{n}\right)\) which is \(\left(\frac{345}{115}\right)=3.\)
Hence, about 115 children who died within 24 hours were selected using systematic random sampling technique every 3 chart interval after the first chart was determined by lottery method which was the second children who died within 24 hours in registration book.
The total number of patients discharged from ETAT within 24 hours (controls) in Wachamo, Wolaita Sodo and Worabe in the past 2 years was 1157, 978 and 616 respectively. Subsequently, based on the above formula the sample size for controls from Wachemo, Wolaita Sodo and Worabe hospitals was 96, 82 and 51. It gives the total number of 229 controls every 12 children (Fig. 1).
Operational definition
Delay in seeking a health facility is as staying home for 48 hours or more before consulting any formal healthcare facility [13].
An incomplete chart means a chart without triage paper and death summary.
Poor nursing follow-up means not giving medication timely and also not taking vital signs within appropriate time interval.
Pediatrics emergency mortality is a record of death that occurred children aged 29 days − 14 years with in 24 hrs of admission to the emergency unit [14].
Treatment delay is not starting any treatment within 1 hour of emergency unit admission [15].
Variables
Dependent variable
-
❖ Pediatrics death in an emergency unit (≤24 hours.)
Independent variable
-
➢ Socio-demographic and environmental characteristics: age, sex, birth weight, area, season
-
➢ Disease factors: medical emergency disease and surgical cases, accidental/injuries, sign and symptoms, disease severity
-
➢ Delay in seeking health facility: referral source, duration of signs and symptoms, treatment delay
-
➢ Previous hospital history: repeated hospital visit, previous hospital admission, congenital problem
-
➢ Poor nursing follow-up-Complete vital signs and medication chart
Data collection tools
The data were collected by 9 BSC nurses and 3 supervisors using a structured checklist from pediatric patient’s chart. The checklist was adapted from different literatures [9, 16, 17]. The data collection checklist includes socio-demographic characteristics, clinical presenting features, and the main medical cause of mortality. The disease cause of mortality was defined according to the HMIS and IDC at the hospital level across the country with related different pediatric age groups.
Data quality assurance
Two-day training was given by the principal investigator on the data extraction checklist and procedure. Before actual data collection, the checklist was pre-tested at WSCSH to check the appropriateness of the checklist with 5% of the sample size. After the pretest, the tool was checked for its consistency by the principal investigator. Finally, the coded data were entered into password-protected computer statistical software.
Data processing and analysis
Data were entered and cleaned for missed values by using EpiData3.1 then exported to Stata version 14.1 for analysis. The description of means, simple frequencies, proportions, and SD of the given data on each variable were computed to compare the exposure status between cases and controls. The normality of the data was tested by skewness and kurtosis test. The degree of association between each independent and dependent variable was assessed by the logistic regression analysis model. The variables with p-value < 0.25 during bivariate analysis were selected as candidate variables for multivariable analysis. Model goodness of fit was tested by Hosmer-Lemeshow’s goodness of fit test with the estat gof command on Stata. Multi-Collinearity was checked by the variance inflation factor (VIF) test. An adjusted odds ratio (AORs) at 95% CI was used to show the strength of the association, and statistical significance was declared at a p-value of < 0.05 as a determinant for pediatric mortality.
Result
A total of 344 charts were reviewed, of these 333 (97%) (112 cases and 221 controls) charts fulfilled the criteria. More deaths occurred in males (53.6%), with a male to female ratio of 1.2:1. Approximately 45.5% of deaths were documented as early death (within 1–12 h of arrival in the pediatric emergency department) (Table 1) (Fig. 2).
The mean ages of cases were 70 (S.D ± 9) months and 49 (S.D. ± 7) months for controls. Also, the mean weight of children in cases and controls was 11.21 (S.D ± 3.47) and 12.73 (S.D ± 3.71) kilogram respectively. Of those cases 55.9% had appropriate weight for age but 50.7% of controls were underweight.
One hundred one (90.2%) of the cases and one hundred nine (49.3%) of the controls visited health facility after one day of signs and/or symptoms. More than half of cases came from urban region with 40.2% referrals from internal health institutions and 59.7% of controls from an urban with 38.9% self-referral. Concerning treatment delay, 64 (57.1%) of cases and 160 (72.4%) of controls were taken medication timely (Table 1).
Eighty-five (75.9%) of cases presented with more than two sign/symptoms and for controls, 95 (43%) presented with more than two signs/symptoms (Table 2). Surgical cases including intestinal perforation and obstruction contributed to 5.4% of cases and 5.4% of control plus to these accidental cases including motor accidents and poisoning were presented in 34.8% of cases and 24% of controls. The contribution of secondary causes for death from both DHN and shock was 77.7%. Comorbidity contributed 49.1% of death (Fig. 3)
While examining specific charts for a specific disease, from cases 62 (55.4%) used appropriate charts regarding with disease and 179 (81%) was appropriate for controls. When vital sign charts completeness evaluated 68 (60.7%) cases and 154 (69.7%) controls completed. Seventy-six (67.9%) of the cases and 151 (68.3%) of controls, were have completed medication chart.
Determinants associated with pediatric emergency mortality
After bivariate analysis 13 variables were selected for multivariable analysis. However, only the seven remained significant determinates which were acute respiratory distress syndrome (ARDS), dehydration (DHN), meningitis, sepsis, unintentional accident, duration of sign/symptoms (> = 1 day) and the right time of medication (treatment delay).
In this study, patients with treatment delay were 2 times more likely to die than without delay (AOR = 2.088, CI = 1.128–3.864). Pediatrics who had ARDS were 2.8 times more likely to die in the emergency unit than pediatrics who did not diagnose with ARDS (AOR =2.804, CI = 1.497–5.250). Children diagnosed with meningitis had 5.2 times more risk for mortality (AOR = 5.282, CI = 2.707–10.310), and those pediatrics presented with sepsis had 4.8 times more odds of death within 24 hours of hospital visit as compared to their counterparts (AOR = 4.224, CI = 2.220–8.040).
Children who visit the pediatric emergency unit with unintentional accidental injury had 3.6 times more risk for mortality (AOR = 3.603, CI = 1.877–6.916) in comparison to their opposite group. Patients whose duration of signs/symptoms was greater than 24 hours before presenting to the emergency unit had a 5.8 times more risk for mortality in the pediatric emergency unit (AOR = 5.481, CI = 2.457–12.230) as compared to their counterparts (Table 3).
Discussion
In this study, seven determinants ARDS, DHN, meningitis, sepsis, unintentional accident, duration of sign/symptoms (> = 1 day), and treatment delay were identified for pediatric emergency unit mortality.
Patients who were not early identified and treated had 2 times more risk to die than those without delay. This finding is consistent with a study done in central America and Tanzania [18, 19]. This might be due to many hospitals in low-income countries serve large number of patients and has few staffs, so patients often have to wait before being assessed and treated which leads to deterioration of patient condition [19]. Furthermore, in most the African countries including Ethiopia, children are not checked before a senior health worker examines them; as a result, some seriously ill patients have to wait a very long time before they are seen and treated [20].
In the present study, children with ARDS had 2.8 times more risk for mortality at the emergency unit than pediatrics who were not diagnosed with ARDS. This is supported by studies conducted in South Asia, Sub-Saharan Africa, and Tikur Anbessa Hospital, Ethiopia [9, 21, 22]. This similarity might be due to ARDS can cause multiple organ failure, including lung collapse which is responsible for most of the child early mortality [23].
In the current study, children diagnosed with meningitis and sepsis had 5.2 and 4.8 times more risk for mortality as compared to their counterparts, respectively. This finding is supported by studies done in China, India, Ghana and World Health Organization (WHO) reports [24,25,26,27]. This similarity might be due to both meningitis and sepsis being more common in low and middle-income countries (85%) and they have a potential for organ failure and they need early diagnosis and treatment but as mentioned above in low and middle-income countries including Ethiopia there is a high rate of treatment delay for children. Moreover, in most countries, bacterial antibiotic resistance is increased which leads the child into deteriorating clinical condition, and finally to death.
Children with dehydration had 4.8 times more odds of death as compared to their comparison group. This finding is consistent with studies conducted in Uganda and Brazil [28, 29], This similarity might be due to there is lack of oral rehydration therapy (ORT) and low immunization coverage in developing countries. Also, it might be due to dehydration can cause severe metabolic and electrolyte disturbance and treatment delay for dehydration in Ethiopia is high which leads to mortality [30].
Children who visit the pediatric emergency unit with unintentional accidental injury had 3.6 times more risk for mortality. This finding is consistent with previous studies conducted in Bahir Dar, Addis Ababa, and low- and middle-income settings [31,32,33]. This might be because of accidental injury being able to cause excessive blood loss and there is the low quality of first aid service at the time of an accident in Africa. Moreover, might be due to in sub-Saharan settings accidental injury is among the leading causes of mortality for children [33].
Lastly, children whose signs/symptoms greater than 24 hours before presenting to the emergency unit had 5.8 times more odds for mortality. This finding is consistent with studies done in Addis Ababa and Nepal [9, 34]. This could be due to timely and appropriate treatment within 24 hours of the onset of illness symptoms can reduce severe morbidity and mortality among children in most African countries. Moreover, in Africa most families visit health institutions at the end after religious prayer and traditional medicine treatment which makes unable to early identify critically ill children and poor treatment seeking behavior of caregivers [35].
In this study, incomplete chart record and the presence of multiple diagnoses were the limitations.
Conclusion
The majority of pediatric emergency mortality occurs within 24 hours of admission. In this study, ARDS, sepsis, meningitis and dehydration, delayed diagnosis and treatment, duration of signs and symptoms, and accidental injury were also significantly associated with early pediatric emergency mortality. To decrease this mortality, ETAT training should be provided for healthcare providers and its implementation should be strengthened. Furthermore, healthcare professionals should provide special attention and provide early treatment for children with ARDS, sepsis, meningitis and dehydration. Lastly, the concerned bodies also design strategies to increase the community health-seeking behavior.
Availability of data and materials
The data used in this manuscript are available upon reasonable request by contacting the corresponding authors via email.
Abbreviations
- AHR:
-
Adjusted Hazard Ratio
- ARDS:
-
Acute respiratory Distress Syndrome
- CHR:
-
Crude Hazard Ratio
- DHN:
-
Dehydration
- NICU:
-
Neonatal Intensive Care Unit
- ETAT:
-
Emergency triage assessment and treatment
- PED:
-
Pediatric emergency department
- SNNP:
-
South nation and nationalities people
- WSUCSH:
-
Wolayita Sodo University Comprehensive Specialized Hospital
- WUNEMMCSH:
-
Wachemo University Nigist Eleni Mohammed Memorial comprehensive specialized hospital
References
Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards millennium development goal 4. Lancet. 2010;375(9730):1988–2008.
World Health Organization. World health statistics 2010. World Health Organization; 2010.
Michalski T. The differentiation of the health situation in European post-Communist countries after 1990. Geography and Tourism. 2016;1(4):33-42.
Moss WJ, Ramakrishnan M, Storms D, Henderson Siegle A, Weiss WM, Lejnev I, et al. Child health in complex emergencies. Bull World Health Organ. 2006;84:58–64.
Obermeyer Z, Abujaber S, Makar M, Stoll S, Kayden SR, Wallis LA, et al. Emergency care in 59 low-and middle-income countries: a systematic review. Bull World Health Organ. 2015;93:577–86.
World Bank. Africa development indicators 2012/2013. The World Bank; 2013.
United Nations Children's Fund: ‘’United Nations Children's Fund Committing to child survival: a promise renewed—progress report 2013’’ 2013.
Gedefaw G, Goedert MH, Abebe E, Demis A. Effect of cesarean section on initiation of breast feeding: findings from 2016 Ethiopian demographic and health survey. PLoS One. 2020;15(12):e0244229.
Jofiro G, Jemal K, Beza L, Bacha Heye T. Prevalence and associated factors of pediatric emergency mortality at Tikur Anbessa specialized tertiary hospital: a 5 year retrospective case review study. BMC Pediatr. 2018;18(1):316.
Germa F, Bayleyegn T, Kebede T, Ducharme J, Bartolomeos K. Emergency medicine development in Ethiopia: challenges, progress and possibilities. Afr J Emerg Med. 2013;3(1):3–9.
Negasi KB, Tefera Gonete A, Getachew M, Assimamaw NT, Terefe B. Length of stay in the emergency department and its associated factors among pediatric patients attending Wolaita Sodo University Teaching and Referral Hospital, Southern, Ethiopia. BMC Emergency Medicine. 2022;22(1):203.
Awol SM, Wabe YA, Ali MM. Determinants of pneumonia among children attending public health facilities in Worabe town. Sci Rep. 2022;12(1):1–9.
Chandwani H, Pandor J. Healthcare-seeking behaviors of mothers regarding their children in a tribal community of Gujarat, India. Electron Physician. 2015;7(1):990.
Jofiro G, Jemal K, Beza L, Bacha Heye T. Prevalence and associated factors of pediatric emergency mortality at Tikur Anbessa specialized tertiary hospital: a 5 year retrospective case review study. BMC Pediatr. 2018;18(1):1–10.
Commission J. Preventing delays in treatment. Quick Safety. 2015;9:1–2.
Duke T, Cheema B. Paediatric emergency and acute care in resource poor settings. J Paediatr Child Health. 2016;52(2):221–6.
Lahmini W, Bourrous M. Mortality at the pediatric emergency unit of the Mohammed VI teaching hospital of Marrakech. BMC Emerg Med. 2020;20(1):57.
Crouse HL, Torres F, Vaides H, Walsh MT, Ishigami EM, Cruz AT, et al. Impact of an emergency triage assessment and treatment (ETAT)-based triage process in the paediatric emergency department of a Guatemalan public hospital. Paediatrics Int Child Health. 2016;36(3):219–24.
Safari SR. Perceptions and challenges of using emergency triage assessment treatment guideline in emergency department at Muhimbili national hospital. Tanzania: Muhimbili University of Health and Allied Sciences; 2012.
Molyneux E, Ahmad S, Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource-constrained setting. Bull World Health Organ. 2006;84:314–9.
Pneumonia U. Diarrhoea-tackling the deadliest diseases for the world’s poorest children. New York: UNICEF; 2012.
Walker CLF, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405–16.
Berhanu A, Alemayehu M, Daka K, Binu W, Suleiman M. Utilization of integrated community case management of childhood illnesses at health posts in southern Ethiopia. Pediatric Health, Medicine and Therapeutics. 2020:459-67.
World Health Organization. Guideline: updates on pediatric emergency triage, assessment and treatment: care of critically-ill children, 2016.
Zhu CP, Wu XH, Liang YT, Ma WC, Ren L. The mortality of patients in a pediatric emergency department at a tertiary medical center in China: an observational study. World J Emerg Med. 2015;6(3):212–6.
Santhanam I, Pai M, Kasturi K, Radhamani MP. Mortality after admission in the pediatric emergency department: a prospective study from a referral children's hospital in southern India. Pediatr Crit Care Med. 2002;3(4):358–63.
Sylverken J, Robison JA, Osei-Akoto A, Nguah SB, Addo-Yobo E, Balch A, et al. Decreased mortality after establishing a pediatric emergency unit at an urban referral Hospital in Ghana. Pediatr Emerg Care. 2021;37(7):e391–5.
Grenov B, Lanyero B, Nabukeera-Barungi N, Namusoke H, Ritz C, Friis H, et al. Diarrhea, Dehydration, and the Associated Mortality in Children with Complicated Severe Acute Malnutrition: A Prospective Cohort Study in Uganda. J Pediatr. 2019;210:26–33.e23.
Merino VR, Nakano V, Delannoy S, Fach P, Alberca GG, Farfan MJ, et al. Prevalence of enteropathogens and virulence traits in Brazilian children with and without diarrhea. Front Cell Infect Microbiol. 2020;10:549919.
Cavalcante e Silva A, Correia LL, Campos JS, Andrade FM, Silveira DM, Leite Á J, Rocha HA, Machado MM, Cunha AJ: Reducing child mortality: the contribution of Ceará state, northeast of Brazil, on achieving the Millennium Development Goal 4 in Brazil. Matern Child Health J. 2015; 19(4):700–706.
He S, Lunnen JC, Puvanachandra P, Zia N, Hyder AA. Global childhood unintentional injury study: multisite surveillance data. Am J Public Health. 2014;104(3):e79–84.
Adnan A, David E, Prasanthi P, Junaid R, Hesham E, Andres I, et al. Global childhood unintentional injury surveillance in four cities in developing countries. Bull World Health Organ. 2009;87(5):345–52.
Nordberg E. Injuries in Africa: a review. East Afr Med J. 1994;71(6):339–45.
Tinuade O, Iyabo RA, Durotoye O. Health-care-seeking behaviour for childhood illnesses in a resource-poor setting. J Paediatr Child Health. 2010;46(5):238–42.
Wiseman V, Scott A, Conteh L, McElroy B, Stevens W. Determinants of provider choice for malaria treatment: experiences from the Gambia. Soc Sci Med. 2008;67(4):487–96.
Acknowledgments
The authors thank the staff of Wolayita Sodo University Comprehensive Specialized Hospital and Wachemo University Nigist Eleni Mohammed Memorial comprehensive specialized hospital
Funding
The authors have also confirmed that no financial funding was received for the study, authorship, and publication of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to data analysis, writing and revising the article. All authors agreed on the journal to which the article will be submitted, gave final approval for the version to be published, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. Ethical clearance was obtained from Debre Berhan University College of Medicine and Health Science, Ethical Review Board. Then officials at different levels of the hospital were communicated through formal letters. Informed consent was obtained from the children’s parents. Confidentiality of the information was secured throughout the study process. Furthermore, the collected data were anonymous.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tsegaye, H., Demelash, A., Aklilu, D. et al. Determinants of pediatrics emergency mortality at comprehensive specialized hospitals of South nation nationalities and people region, Ethiopia, 2022: unmatched case-control study. BMC Pediatr 23, 192 (2023). https://doi.org/10.1186/s12887-023-04011-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04011-3