Abstract
Background
The intrapulmonary ectopic thyroid gland is exceedingly rare since the ectopic thyroid was discovered. Only eight cases have been reported in the worldwide literature. We present a case of multiple intrapulmonary ectopic thyroid glands with nodular goiter in a 10-year-old girl.
Case presentation
The girl was found with multiple intrapulmonary nodules in bilateral lungs during the treatment of nodular goiter. The intrapulmonary lesions were initially thought to be a high possibility of metastatic cancer. A computed tomography-guided percutaneous lung biopsy was performed, and the pathological examination confirmed that the diagnosis was ectopic intrapulmonary thyroid.
Conclusion
The ectopic intrapulmonary thyroid should be considered when children with nodular goiter presenting with suspected metastases in the lung.
Similar content being viewed by others
Introduction
Ectopic thyroid gland (ETG) refers to the thyroid tissue present outside the normal location of the anterior neck region and is usually due to the abnormal migration of the thyroid gland during embryonic development [1]. ETG has an incidence of 1/100,000–1/300,000 in the normal population and 1/4000–1/8000 in the population with thyroid disorder [2]. It can occur at any age, with a predilection for the 30- to 50-year-olds; 65–80% of patients are female. ETG primarily occurs at the base of the tongue, around the course of the thyroglossal duct, or laterally in the neck. Less than 10% of cases are found in the periphery, including heart, lung, adrenal, duodenum, pancreas, intestine, and other regions of the body [3]. A majority of patients with ETG are usually asymptomatic and discovered incidentally. Local compressions caused by the ectopic nodule enlargement and the associated endocrine dysfunction are the main clinical presentations in symptomatic ETG. Generally, surgery, radiofrequency ablation, radioactive iodine ablation, and exogenous thyroid hormone treatment can be considered for treating symptomatic ETG.
Among the peripheral locations where ectopic thyroid occurs, the lung is a relatively peculiar site, and only a few cases have been reported so far. Moreover, among the cases of ectopic intrapulmonary thyroid, most ectopic nodules were in a single pulmonary lobe or homolateral lobes. ETG of the bilateral lung was rarely reported. In this study, we presented a case with ETG in multiple lobes in both lungs masquerading as metastatic lung carcinoma. Also, the pertinent literature was reviewed.
Case presentation
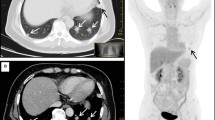
A 10-year-old girl came to Xiangyang No. 1 hospital in June 2021 due to the painless masses in the bilateral neck, which slowly increased in size in 1 year. The patient had no relevant clinical history. The ultrasound showed an enlarged thyroid gland with multiple cystic nodules in both lobes, according to the Thyroid Imaging Reporting and Data System Grade 3. The largest one was about 1.9 × 1.5 cm2 on the left lobe, and another one was 1.6 × 1.5 cm2 on the right lobe. The thyroid function test indicated that serum thyroid-stimulating hormone (TSH), free triiodothyronine (FT3), free thyroxine (FT4), and calcitonin levels were normal. But the thyroglobulin (TG) level raised to 441.4 ng/ml (normal range 0.2-70ng/ml). Ultrasonography-guided fine-needle aspiration(FNA) cytology of the thyroid gland was performed to confirm the diagnosis. The cytology results suggested nodular goiter. Radiofrequency ablation on the thyroid nodules was conducted for the main treatment. However, the routine preoperative enhanced chest computed tomography (CT) scanning showed a total of 4 nodules in both lungs, varying in size from 3 to 11 mm, with marked enhancement in the arterial phase and regression in the delayed phase (Fig. 1, Supplementary Fig. 1). The largest nodule was approximately 7.2 × 11 mm2 in size. The aforementioned imaging findings suggested metastatic carcinoma of both lungs. We performed a CT-guided lung biopsy of one nodule in each lung to define the nature of the metastases. The pathological examination showed lung tissue and well-differentiated thyroid follicular tissue, without cellular atypia. The immunohistochemistry staining showed thyroid transcription factor-1 (TTF1) and paired box gene 8 (Pax-8) positivity, thyroglobulin (TG), Cytokeratin 7 (CK7), and Cytokeratin 19 (CK19) partial positivity, and carcinoembryonic antigen (CEA), galectin 3, and Hector Battifora mesothelial-1 (HBME-1) negativity. Also, the Ki67 index suggested a low level of proliferation (Fig. 2). The pathological results of lung biopsy confirmed that the diagnosis was ectopic intrapulmonary thyroid. Considering thyroidectomy or radioactive iodine ablation might be harmful to the growth and development of the young girl, and the patient’s parents refused surgical treatment, radiofrequency ablation on the thyroid nodules was selected for the treatment of the neck mass. In view of the multiple intrapulmonary thyroid nodules in both lungs and the patient being asymptomatic, we applied the “wait and watch” strategy. One month after radiofrequency ablation, the patient is euthyroid (FT3:5.39pmol/L, FT4 :14.55pmol/L, TSH:1.02mIU/L) and has no associated complications. After the follow-up of 8 months, the CT scan showed no change in the pulmonary nodules in the bilateral lungs. Meanwhile, the patient’s serum FT3, FT4 and TSH were still in normal range, and TG level (80.72ng/ml) was nearly within the normal range (normal range 0.2-70ng/ml). The detailed diagnosis and treatment procedures are summarized in Fig. 3.
Microphotograph of pulmonary ectopic thyroid glands. (A) H&E show thyroid tissue in the pulmonary parenchyma, magnification ×200. (B) The immunohistochemistry staining of follicular epithelial cells showed low level of proliferation of Ki67, magnification ×200
(C) Positive immunohistochemistry staining for thyroglobulin (TG), magnification ×200. (D) Positive immunohistochemistry staining for transcription factor-1 (TTF1), magnification ×200
Discussion
In normal anatomy, the thyroid is located in the anterior neck region between the second and fourth tracheal rings. During embryonic development, the developing thyroid migrates from the thyroid primordia to its final position anterior to the trachea, and when the thyroid fails to descend along the midline to reach its normal position, ETG occurs [1, 4]. The majority of ETG is located at the base of the tongue, especially in the area of the foramen cecum, which accounts for approximately 90% of reported cases.
Cases with ectopic thyroid glands in both lungs are extremely rare. Only eight cases with ectopic intrapulmonary thyroid have been reported after searching PubMed and Medline (Table 1). Most patients were asymptomatic and usually discovered incidentally or during other medical visits. A small number of patients had primary thyroid disease, including thyroid nodules, hyperthyroidism, and thyroid cancer. Some case reports indicated that primary thyroid disease might be associated with ETG, but further studies were needed to confirm this conclusion.
To date, scintigraphy using Tc-99 m, I-131, or I-123 is commonly used for diagnosing ectopic thyroid. To some extent, other imaging modalities, such as magnetic resonance imaging, CT, and ultrasound help in the complementary diagnosis [2]. Diagnosis of intrapulmonary ectopic thyroid only by imaging is difficult, because the intrapulmonary ectopic thyroid may be misdiagnosed as thymoma, germ cell tumor, neuroma, or lung metastases when viewed using CT or MRI without pathology. Positron emission tomography/computed tomography (PET/CT) can be used to excluded metastatic cancer, but it has no specificity in the diagnosis of ectopic thyroid [12]. Thus, the histopathological diagnosis is still the gold standard.
The molecular mechanism of ETG development has not been elucidated yet. Previous studies found that some genes might be related to the incidence of the disease. Foxe1, formerly called thyroid transcription factor-2, was involved in regulating the TG and the thyroid peroxidase gene promoters [13]. The absence of Foxe1 in mice was associated with defective thyroid migration, which resulted in the ETG [14]. Titf1/Nkx2-1 (thyroid transcription factor-1) is a homeodomain-containing transcription factor expressed in the human lung and thyroid gland. Pax-8 is involved in thyroid follicular cell development and expression of thyroid-specific genes [13]. A previous study showed that Pax-8 and Titf1/Nkx2-1 interacted directly in thyroid cells and regulated the activation of the thyroglobulin promoter and differentiation of thyroid cells [15, 16]. However, currently, no evidence shows that the occurrence of ectopic thyroid is associated with these genetic mutations in humans. Further studies are needed to elucidate the mechanism.
The limitation of our study was that we did not perform a molecular biological examination, including the status of PAX8, Titf1/Nkx2-1, and Foxe1 because of the limited resources. And the radioiodine imaging of the nodules in both lungs could not be performed because of the COVID-19 pandemic. Furthermore, we chose FNA rather than surgical resection for the diagnosis of the neck mass, which resulted in a lack of sufficient pathological specimens to find out the pathological difference between neck and lung lesions.
Currently, no consensus exists on the treatment of ETG. The treatment varies depending on the tumor location, size, and appearance of the clinical symptom. Based on the results of previous studies and the experience from our center, we formulated a treatment strategy that might be helpful for clinicians. For asymptomatic and euthyroid patients, a “wait and watch” strategy can be recommended [12, 17,18,19,20]. Surgery or surgical ablation is recommended when symptoms of compression or obstruction occur. Moreover, suppressive hormone therapy with levothyroxine or I-131 therapy is an alternative to surgery for patients with surgical contraindication in whom surgical resection is not possible due to anatomical difficulties [17,18,19,20,21].
In conclusion, we reported an exceedingly rare case of multiple bilateral pulmonary ectopic thyroid glands with nodular goiter. The patient received thyroid radiofrequency ablation treatment and regular follow-up to observe the ectopic thyroid tissues in both lungs. We think this interesting case may provoke debates about the methods of precise diagnosis and management for cases with intrapulmonary ectopic thyroid tissues.
Data Availability
The clinical data supporting the conclusions of this manuscript are available from the corresponding author upon reasonable request.
Abbreviations
- ETG:
-
Ectopic thyroid gland
- TSH:
-
Thyroid-stimulating hormone
- TG:
-
Thyroglobulin
- FNA:
-
Fine-needle aspiration
- CT:
-
Computed tomography
References
De Felice M, Lauro RD. Thyroid development and its Disorders: Genetics and Molecular Mechanisms. Endocr Rev. 2004;25(5):722–46.
Noussios G, et al. Ectopic thyroid tissue: anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol. 2011;165(3):375–82.
Basaria S, Westra WH, Cooper DS. Ectopic lingual thyroid masquerading as thyroid cancer metastases. J Clin Endocrinol Metab. 2001;86(1):392–5.
Rosai J, Ackerman LV. Surgical pathology. 5th ed. St. Louis: Mosby; 1974. p. 1394.
Cheng H et al. Multiple thyroid nodules in the lung: metastasis or ectopia?Diagnostic Pathology, 2015. 10(1).
Ko HH, et al. Ectopic Intrapulmonary thyroid: a Case Report. Korean J Thorac Cardiovasc Surg. 2013;46(3):237–9.
Bando T, et al. Ectopic intrapulmonary thyroid. Chest. 1993;103(4):1278–9.
Di Mari N, et al. Ectopic thyroid of the lung. An additional case. Pathologica. 2010;102(3):102.
Ryu HS, et al. Ectopic intrapulmonary thyroid tissue mimicking metastatic tissue. Thyroid. 2012;22(7):755–9.
Weng LP, et al. Multilokuläre Schilddrüsenektopie. DMW - Deutsche Medizinische Wochenschrift. 2008;125(14):421–4.
Simon M, Baczako K. Thyroid inclusion in the lung. Metastasis of an occult papillary carcinoma or ectopia?Pathol Res Pract, 1989. 184(2): p. 263 – 67; discussion 268 – 70.
Cheng L, Jiang X, Jiang Y. Ectopic thyroid as multiple nodules in bilateral lung lobes: a case report. Gland Surg. 2020;9(3):806–11.
Damante G, Tell G, Di Lauro R. A unique combination of transcription factors controls differentiation of thyroid cells. Prog Nucleic Acid Res Mol Biol. 2001;66:307–56.
De Felice M, et al. A mouse model for hereditary thyroid dysgenesis and cleft palate. Nat Genet. 1998;19(4):395–8.
Mansouri A, Chowdhury K, Gruss P. Follicular cells of the thyroid gland require Pax8 gene function. Nat Genet. 1998;19(1):87–90.
Di Pasca M, Di Lauro R, Zannini M. Pax8 Has a Key Role in Thyroid Cell Differentiation. Proceedings of the National Academy of Sciences - PNAS, 2000. 97(24): p. 13144–13149.
Chawla M, Kumar R, Malhotra A. Dual ectopic thyroid: case series and review of the literature. Clin Nucl Med. 2007;32(1):1–5.
Bersaneti JA, et al. Ectopic thyroid presenting as a submandibular mass. Head Neck Pathol. 2011;5(1):63–6.
Douglas PS, Baker AW. Lingual thyroid. Br J Oral Maxillofac Surg. 1994;32(2):123–4.
Toso A, et al. Lingual thyroid causing dysphagia and dyspnoea. Case reports and review of the literature. Acta Otorhinolaryngol Ital. 2009;29(4):213–7.
Xu G, Fu X. One-stage video-assisted thoracic surgery for bilateral multiple pulmonary nodules. J Thorac Dis. 2019;11(2):535–41.
Acknowledgements
Not applicable.
Funding
This study was supported by Innovative Research Program of Xiangyang No.1 People’s Hospital (Grants number: XYY2021Q02), Platform Special Fund for Scientific Research of Xiangyang No.1 People’s Hospital (Grants number: XYY2022P05) and Key projects of Xiangyang Science and Technology Bureau (2021YL26).
Author information
Authors and Affiliations
Contributions
Conceptualization, D.Z.; data curation and writing, writing—review and editing, Y.Z, H.Y, and X.Z.; funding acquisition, D.Z. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethics and Scientific Committee of Hubei University of Medicine with approval number XYY2021002.
Consent for publication
An informed consent was received from parent authorized representative for publication of identifying information/images in an online open-access publication.
Competing interests
The authors declare that they have no competing interests.
Consent to participate
Everything under Ethical approval and consent to participate.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhuo, Y., Yu, H., Zhou, X. et al. Ectopic intrapulmonary thyroid masquerading as metastatic carcinoma of the lung: a rare case scenario. BMC Pediatr 23, 178 (2023). https://doi.org/10.1186/s12887-023-04003-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04003-3