Abstract
Background
There are few reports on the timing of onset and the symptoms of enterovirus A71 (EV-A71) infection, which can easily be misdiagnosed. This study aimed to explore the clinical characteristics of children with severe EV-A71 infection.
Methods
This retrospective observational study included children with severe EV-A71 infection admitted to Hebei Children’s Hospital between January 2016 and January 2018.
Results
A total of 101 patients were included: 57 males (56.4%) and 44 females (43.6%). They were 1–13 years of age. The symptoms were fever in 94 patients (93.1%), rash in 46 (45.5%), irritability in 70 (69.3%), and lethargy in 56 (55.4%). There were 19 (59.3%) patients with abnormal neurological magnetic resonance imaging [pontine tegmentum (n = 14, 43.8%), medulla oblongata (n = 11, 34.4%), midbrain (n = 9, 28.1%), cerebellum and dentate nucleus (n = 8, 25.0%), basal ganglia (n = 4, 12.5%), cortex (n = 4, 12.5%), spinal cord (n = 3, 9.3%), and meninges (n = 1, 3.1%)]. There was a positive correlation between the ratio of neutrophil count and white blood cell count in cerebrospinal fluid in the first 3 days of the disease (r = 0.415, P < 0.001).
Conclusion
The clinical symptoms of EV-A71 infection are fever and/or skin rash, irritability, and lethargy. Some patients have abnormal neurological magnetic resonance imaging. The white blood cell count in the cerebrospinal fluid of children with EV-A71 infection may increase alongside neutrophil counts.
Similar content being viewed by others
Introduction
EV-A71 is a non-enveloped icosahedron, single-stranded, positive-stranded RNA virus with a total genome length of 7.4 kb that was first isolated from the feces of children in California (USA) in 1969 and was detected in various countries since then [1,2,3]. Over the past 20 years, EV-A71 has also been widely detected in China [4, 5], causing outbreaks and several deaths [6,7,8]. The virus is neurotropic and can cause an inflammatory response in the body [9,10,11], leading to various neurological injuries and even death [12, 13].
There are many reports on the common clinical symptoms of infection by the EV-A71 virus in China [14,15,16], but there are few reports on the timing of onset and symptoms of children with severe EV-A71 infection, easily leading to misdiagnosis or misjudgment by clinicians, especially in rural hospitals, resulting in delayed treatment, improper treatment, or overtreatment.
Therefore, this study aimed to describe the clinical characteristics of children with severe EV-A71 infection.
Materials and methods
Study design and patients
This retrospective study included children with severe EV-A71 infection who were admitted to Hebei Children’s Hospital between January 2016 and January 2018. This study was approved by the Ethics Committee of Hebei Children’s Hospital (152). The requirement for informed consent was waived by the committee because of the retrospective nature of the study.
The inclusion criteria were (1) 28 days to 14 years of age, (2) a positive EV-A71-PCR throat swab, in line with the Guidelines for the Diagnosis and Treatment of Hand, Foot, and Mouth Disease (2018 version) [17], (3) one or more symptoms such as fever, rash, poor mental state, irritability, lethargy, limb weakness, ataxia, and cardiopulmonary failure, and (4) at least one symptom of alarm and lethargy. The exclusion criteria were (1) positive blood culture, (2) increased mycoplasma antibody titers, (3) elevated blood C-reactive protein (CRP) and procalcitonin, or (4) the physicians suspected the presence of other pathogens.
Data collection
The general data of children with a severe EV-A71 infection were obtained from the electronic medical records of the hospital, including sex, age, fever, dermatosis, irritability, lethargy, limb weakness, white blood cell count, the proportion of neutrophils, white blood cell count of cerebrospinal fluid (CSF), and magnetic resonance imaging (MRI) of the head and/or spinal cord. The MRI examinations were performed using a GE Signa Excite 1.5-T imaging system during the study period. Two senior radiologists and pediatric neurologists with more than 10 years of experience analyzed the images.
Statistical analysis
SPSS 23.0 (IBM, Armonk, NY, USA) was used to process and analyze the data. Continuous data with a normal distribution (according to the Shapiro-Wilk test) were expressed as means ± standard deviation and analyzed using Student’s t-test or the paired t-test. Categorical data were presented as n (%). Two-sided P-values < 0.05 were considered significant.
Results
Characteristics of the patients
This study included 101 patients: 57 males (56.4%) and 44 females (43.6%). They were 1 to 13 years of age (mean: 2.3 ± 1.7 years). Ninety-four (93.1%) patients had a fever, and the onset time was 1.1 ± 0.4 days. Forty-six patients (45.5%) had a rash, and the onset time was 1.1 ± 0.4 days. Seventy (69.3%) children had an irritable mood, and the onset time was 2.7 ± 2.3 days. Fifty-six (55.4%) children were lethargic, and the onset time was 3.8 ± 1.7 days. Two children (2.0%) displayed limb weakness, and the onset time was 5.0 ± 0.0 days. Two patients (1.98%) suffered from ataxia, and the onset time was 3.0 ± 0.0 days (Table 1). Two patients died on the 2nd and 4th days after onset, respectively.
MRI characteristics
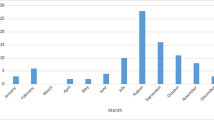
Thirty-two children underwent an MRI of the head and/or spinal cord. The MRI examination was performed in the acute phase (within 1 week), and the average time of the MRI examination was 3.2 ± 2.8 days from the onset of the disease. Among the 32 children, 19 showed abnormal neurological imaging, accounting for 59.3%. The abnormal sites were pontine tegmentum (n = 14, 43.8%), medulla oblongata (n = 11, 34.4%), midbrain (n = 9, 28.1%), cerebellum and dentate nucleus (n = 8, 25.0%), basal ganglia (n = 4, 12.5%), cortex (n = 4, 12.5%), spinal cord (n = 3, 9.3%), and meninges (n = 1, 3.1%) (Fig. 1).
Blood examinations
The white blood cell count within 3 days of the disease course was 5.7 × 109/L to 25.9 × 109/L. The proportion of neutrophils was 13.9–89.7%. Sixty-three patients underwent CSF examination within 3 days of the disease course. The white blood cell count in CSF was 0 to 587 × 106/L (Table 2). The proportion of neutrophils within 3 days was divided into quintiles, with 20% per quintile. The proportions of neutrophils in the quintiles were positively correlated with the white blood cell count in CSF within 3 days (r = 0.415, P < 0.001) (Table 3).
Electrophysiology
Forty patients were monitored using scalp electroencephalography (EEG) within the first 4 days of the disease. Among them, 37 (92.5%) children had a normal EEG. Three (7.5%) children showed slow waves of 1.0–2 Hz, and all three suffered from epilepsy-like seizures (Fig. 2).
Discussion
This study showed that fever and rash tended to appear earlier during severe EV-A71 infection, followed by irritability and lethargy, which might be related to the infection mechanism. Indeed, EV-A71 enters the human body through the mouth, initially replicates in the pharynx (tonsils) or intestinal tract, and then multiplies in the regional lymph nodes, which can cause mild viremia [18,19,20]. The illness of most patients can be controlled at this stage. In some infected people, the virus continues to invade the reticuloendothelial tissue, deep lymph nodes, liver, spleen, bone marrow, skin, mucous membranes, central nervous system, and heart, and further proliferate and cause corresponding lesions [21]. Generally, the symptoms of systemic viremia, such as fever and rash, appear first after viral replication through the respiratory or gastrointestinal tract. If the disease continues to progress, the nervous system can be impaired, leading to irritability and lethargy.
In this study, irritability usually appeared on the 1st to 4th day, especially on the 2nd or 3rd day. The essence of irritability is myoclonus, divided into myoclonus from the corticothalamic axis and subcutaneous non-epileptic myoclonus originating from the back of the pons. Considering that no epilepsy waves were found in the scalp EEG of the included children and MRI lesions were more common in the dorsal pons, irritability may be from myoclonus caused by the release of 5-HT from the dorsal pons (predominant raphe nucleus) [22]. Lethargy mostly occurred after the fever subsided and after irritability, mainly on the 3rd or 4th day, and lasted for 1–2 days. Impairment of the cortical or ascending reticular activation system can reduce consciousness [23,24,25]. Still, most children had normal EEG without obvious cognitive dysfunction during the recovery period, suggesting likely non-specific projection system damage of the ascending reticular activation system in the upper pons or lower part of the midbrain, leading to lethargy.
Among the 101 children included, two died. None of the remaining children entered the stage of pre-cardiopulmonary or cardiopulmonary failure. Nevertheless, the frequencies of irritability and lethargy were 69.3% and 55.4%, respectively, suggesting that irritability and lethargy are common clinical manifestations of central nervous system involvement in most children with severe EV-A71 infection. In recent years, with the use of immunoglobulin, the number of cases of limb weakness has decreased compared with early studies. Limb weakness mostly occurred after the 4th day and resulted from the anterior horn of the spinal cord being invaded by the virus. The two cases of death due to cardiopulmonary failure occurred in the first 3 days of the course of the disease, mostly without skin rash. Considering that the lesions involved the dorsal nucleus of the vagus nerve and the nucleus of the solitary tract, or the inner acceleration center or vasoconstriction center of the reticular structure [26, 27], it is possible that the lesions were caused by sympathetic excitation.
MRI was performed on 32 patients in this study. The lesions involved pontine tegmentum (43.8%), medulla oblongata (34.3%), midbrain (28.1%), cerebellum and dentate nucleus (25.0%), basal ganglia (12.5%), cortex (12.5%), spinal cord (9.3%), and meninges (3.1%), consistent with the pattern reported by Lee et al. [28]. In this study, the incidence of radiographic infection sites was consistent with the incidence of the corresponding clinical manifestations in children: irritability (raphe nucleus), lethargy (ascending reticular activation system), ataxia (cerebellum and dental nucleus), limb weakness (anterior horn of the spinal cord), seizures (cortical) and meningeal irritation (meningeal).
Sixty-three patients underwent CSF examination within 3 days of the onset of the disease. The proportion of neutrophils was positively correlated with the white blood cell count in CSF within 3 days of the onset of the disease, suggesting that with the increase of the proportion, the white blood cell count in the cerebrospinal fluid has a gradually increasing trend, which has not been reported before and has certain significance for guiding the clinical cerebrospinal fluid examination of children with severe EV-A71 infection.
There were some limitations. Only one center was involved, leading to a small sample size. In addition, the numbers of patients with EV-A71 infection in the third and fourth stages were small. The retrospective nature of the study limited the data to those available in the charts. The mechanism of the EV-A71 virus invading the nervous system and the relationship between different mechanisms and the speed and severity of disease progression are not fully understood, and further research is needed.
Conclusions
This study showed that the common clinical symptoms of EV-A71 infection were generally fever and/or rash, irritability, and lethargy. Some children were with abnormal neurological magnetic resonance imaging. There was a positive correlation between the ratio of neutrophil count and white blood cell count in CSF in the first 3 days of the course of the disease. EV-A71 infection may involve multiple parts of the nervous system, mainly the pontine tegmentum, consistent with corresponding clinical manifestations.
Data Availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- EV-A71:
-
Enterovirus A71
- CSF:
-
Cerebrospinal fluid
References
Han Y, Chen Z, Zheng K, Li X, Kong J, Duan X, et al. Epidemiology of Hand, Foot, and Mouth Disease before and after the introduction of Enterovirus 71 Vaccines in Chengdu, China, 2009–2018. Pediatr Infect Dis J. 2020;39:969–78. https://doi.org/10.1097/INF.0000000000002745.
Sun YS, Yang ZN, Xu F, Chen C, Lu HJ, Jiang JM, et al. Global gene expression analysis of the Brainstem in EV71- and CVA16-Infected gerbils. Viruses. 2019;12. https://doi.org/10.3390/v12010046.
Del Giudice P. Enterovirus A71 infection and neurologic disease, Madrid, Spain, 2016. Emerg Infect Dis. 2020;26:1638. https://doi.org/10.3201/eid2607.190037.
Wang J, Teng Z, Cui X, Li C, Pan H, Zheng Y, et al. Epidemiological and serological surveillance of hand-foot-and-mouth disease in Shanghai, China, 2012–2016. Emerg Microbes Infect. 2018;7:8. https://doi.org/10.1038/s41426-017-0011-z.
Zhao MQ, Wang LH, Lian GW, Lin ZF, Li YH, Guo M, et al. Characterization of lymphocyte subsets in peripheral blood cells of children with EV71 infection. J Microbiol Immunol Infect. 2020;53:705–14. https://doi.org/10.1016/j.jmii.2019.03.001.
Hong J, Liu F, Qi H, Tu W, Ward MP, Ren M, et al. Changing epidemiology of hand, foot, and mouth disease in China, 2013–2019: a population-based study. Lancet Reg Health West Pac. 2022;20:100370. https://doi.org/10.1016/j.lanwpc.2021.100370.
Puenpa J, Wanlapakorn N, Vongpunsawad S, Poovorawan Y. The history of Enterovirus A71 Outbreaks and Molecular Epidemiology in the Asia-Pacific Region. J Biomed Sci. 2019;26:75. https://doi.org/10.1186/s12929-019-0573-2.
Chen B, Yang Y, Xu X, Zhao H, Li Y, Yin S, et al. Epidemiological characteristics of hand, foot, and mouth disease in China: a meta-analysis. Med (Baltim). 2021;100:e25930. https://doi.org/10.1097/MD.0000000000025930.
Jin Y, Zhang R, Wu W, Duan G. Antiviral and inflammatory Cellular Signaling Associated with Enterovirus 71 infection. Viruses. 2018;10. https://doi.org/10.3390/v10040155.
Huang HI, Lin JY, Chen SH. EV71 infection induces IFNbeta expression in neural cells. Viruses. 2019;11. https://doi.org/10.3390/v11121121.
Cheng ML, Chien KY, Lai CH, Li GJ, Lin JF, Ho HY. Metabolic reprogramming of host cells in response to enteroviral infection. Cells. 2020;9. https://doi.org/10.3390/cells9020473.
Cheng Y, Zhou C, Song C. Analysis of influencing factors for critical HFMD and construction of a risk Scoring System. Chin Gen Pract. 2018;21:1573–9.
Bai J, Chen X, Liu Q, Zhou X, Long JE. Characteristics of enterovirus 71-induced cell death and genome scanning to identify viral genes involved in virus-induced cell apoptosis. Virus Res. 2019;265:104–14. https://doi.org/10.1016/j.virusres.2019.03.017.
Zhang H. Epidemiological characteristics of hand, foot and mouth disease in Nanning high-tech zone in recent years. Appl Prev Med. 2020;26:438–40.
Han W, Li C. Analysis of characteristics and risk factors in Children with EV71-infected HFMD. J Math Med. 2019;32:870–2.
Li WH, Li WJ, Chen SS. Effect of double infection of EV71 virus and mycoplasma pneumoniae on immunity of children with hand foot mouth disease. Chin J Mod Med. 2018;28:53–7.
National Health Commission of the People’s Republic of China. Guidelines for the diagnosis and treatment of hand foot and mouth disease (2018 version). Chin Pract J Rural Doc. 2018;25:8–13.
Sarma N. Hand, foot, and mouth disease: current scenario and indian perspective. Indian J Dermatol Venereol Leprol. 2013;79:165–75. https://doi.org/10.4103/0378-6323.107631.
Aswathyraj S, Arunkumar G, Alidjinou EK, Hober D. Hand, foot and mouth disease (HFMD): emerging epidemiology and the need for a vaccine strategy. Med Microbiol Immunol. 2016;205:397–407. https://doi.org/10.1007/s00430-016-0465-y.
Repass GL, Palmer WC, Stancampiano FF. Hand, foot, and mouth disease: identifying and managing an acute viral syndrome. Cleve Clin J Med. 2014;81:537–43. https://doi.org/10.3949/ccjm.81a.13132.
Xiao X, Qi J, Lei X, Wang J. Interactions between enteroviruses and the Inflammasome: New Insights into viral pathogenesis. Front Microbiol. 2019;10:321. https://doi.org/10.3389/fmicb.2019.00321.
He Z, Cao J, Cai F. Brain damage induced by experimental myoclonus seizures with different origins. Chin J Neuromed. 2011;10:596–601.
Liu Q, Sun WM, Geng Z. Establishment of animal models of disturbance of consciousness. J Nanchang Univ Med Sci. 2020;60:83–7.
Benghanem S, Mazeraud A, Azabou E, Chhor V, Shinotsuka CR, Claassen J, et al. Brainstem dysfunction in critically ill patients. Crit Care. 2020;24:5. https://doi.org/10.1186/s13054-019-2718-9.
Leon-Dominguez U, Leon-Carrion J. [A neurofunctional model of consciousness: its neurophysiological and cognitive bases]. Rev Neurol. 2019;69:159–66. https://doi.org/10.33588/rn.6904.2019072.
Wang MG, Sun HM, Liu XM, Deng XQ. Clinical analysis of 59 children with hand foot and mouth diseases due to enterovirus EV71 and concomitant viral encephalitis. Eur Rev Med Pharmacol Sci. 2017;21:43–9.
Diarimalala RO, Hu M, Wei Y, Hu K. Recent advances of enterovirus 71 [Formula: see text] targeting inhibitors. Virol J. 2020;17:173. https://doi.org/10.1186/s12985-020-01430-x.
Lee KY. Enterovirus 71 infection and neurological complications. Korean J Pediatr. 2016;59:395–401. https://doi.org/10.3345/kjp.2016.59.10.395.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Wenjuan Wu and Baoguang Li carried out the studies, participated in collecting data, and drafted the manuscript. Baoguang Li and Tao Xie performed the statistical analysis and participated in its design. Wenjuan Wu and Tao Xie participated in the acquisition, analysis, or interpretation of data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study was approved by the Ethics Committee of Hebei Children’s Hospital (152). The need for informed consent was waived by the Ethics Committee of Hebei Children’s Hospital, because of the retrospective nature of the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, W., Li, B. & Xie, T. Children with severe enterovirus A71 infection. BMC Pediatr 23, 172 (2023). https://doi.org/10.1186/s12887-023-03980-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-03980-9