Abstract
Background
The widespread presence of childhood obesity has increased considerably over three decades. The present study was designed to investigate expression patterns of miR-146a, miR-155, miR-15a, miR-193a, and miR-122 in peripheral blood mononuclear cells (PBMCs) in children who are obese along with their association with metabolic and inflammatory biomarkers.
Methods
Ninety test subjects were admitted. The profile of blood pressure, resting energy expenditure (REE), anthropometric measures, body composition, dietary intakes, physical activity levels, insulin, and lipid profile, fasting blood glucose (FBG), high-sensitivity C-reactive protein (hs-CRP), and pubertal stage have been measured. Total RNA (including small RNAs) was extracted from PBMCs. The expression levels of miRNAs were measured by stem-loop RT-qPCR.
Results
The miR-155a expression level was significantly lower in obese children, children with high hs-CRP, and children with high-fat mass. Obese girls had significantly higher PBMC levels of miR-122. MiR-155a had a significant negative association with fasting insulin, HOMA-IR, and hs-CRP. There were significant positive associations between miR-193a and miR-122 expression levels and fasting insulin, HOMA-IR, and TG. MiR-15a was positively correlated with fasting insulin and HOMA-IR. Children with metabolic syndrome, insulin resistance, and high-fat mass had higher PBMC levels of miR-122 and miR-193a. Higher miR-193a and miR-122 levels were also detected in PBMCs of children with fast REE, compared to those with slow REE, and the subjects with high hs-CRP, respectively.
Conclusion
lower level of miR-155 expression in obese subjects and significant associations unfolds the need for more studies to detect the possible underlying mechanisms.
Similar content being viewed by others
Introduction
Obesity is a by-product of interactions among many environmental and genetic factors [1]. The common occurrence of childhood and adolescent obesity has seen a dramatic increase over the past three decades, turning it into a global health issue [2,3,4]. Obesity is strongly associated with insulin resistance, chronic adipose tissue inflammation, and hyperlipidemia. Undeniably, childhood and adolescent obesity increases the risk of chronic disorders such as cardiovascular diseases, dyslipidemia, metabolic syndrome, and diabetes mellitus in adulthood [5, 6]. While some obese children are metabolically healthy (MHO), others show abnormalities ranging from mild chronic inflammation to insulin resistance [7, 8]. It is estimated about 20 to 30% of obese children and adolescents are metabolically healthy [7, 9]. In most studies, metabolically healthy obesity has been suggested to be defined as obesity with no indication for associated metabolic disorders, such as dyslipidemia, metabolic syndrome. etc. [10]. Various hypotheses have been raised to explain the underlying mechanisms of this bipartite among obese children, either being metabolically healthy or suffering from obesity-related metabolic disorders, but more investigations are needed to achieve a consensus about the exact mechanism [11]. There is an urgent need for discovering biomarkers that help in the early detection and prognosis of high-risk individuals and the prevention of childhood obesity-related disorders [3]. MicroRNAs (i.e. miRNAs), recognized as promising biomarkers for various diseases [12]. are short non-coding molecules (about 22 nucleotides in length) that play crucial roles in regulating gene expression in the post-transcription step by binding to 3′-UTR-RNA regions, and inhibiting mRNA translation or degradation [2, 4, 13,14,15]. Being sustainable and measurable, circulating miRNAs in body fluids, especially blood, have been extensively used as a biomarker for the diagnosis of disorders [16,17,18,19]. In addition, several studies have suggested that circulating miRNA concentrations are associated with various metabolic diseases such as obesity, hyperlipidemia, and type 2 diabetes [20,21,22]. For example, a higher level of miR-122 is coincidental with the increased risk of obesity and insulin resistance in young adults [23, 24]. It correlates with an increased risk of metabolic syndrome, type 2 diabetes, and liver damage [25]. Previous studies have reported that miR-193 blood level was higher in obese and pre-diabetic adults [26]. In addition, miR-15 is reduced in type 2 diabetes, metabolic syndrome, and obesity, and is used as a biomarker to diagnose obese children at risk of type 2 diabetes henceforward [2]. MiRNAs are involved in adipogenesis, obesity, lipid and fatty acid metabolism, insulin resistance, adipocyte differentiation, appetite regulation, inflammation, oxidative stress, and cytokines expression [27, 28]. For example, miR-146 plays a crucial role in adipose tissue inflammation and is one of the most essential and effective mediators contributing to obesity and subsequent problems [29]. MiR-155 is involved in the metabolism of cholesterol and fatty acids in the liver and regulates many of the genes related to fat metabolism [30, 31]. It speculates that expression patterns of miRNAs in obese children could be used as a predictor of metabolic diseases in adulthood. miRNA expression profile of obese children, relative to others, has not been extensively investigated. The current study specified to compare the expression levels of miR-193a, miR-122, miR-155, miR-15a, and miR-146a in peripheral blood mononuclear cells (PBMCs) of 10 to 18 years-old obese children and adolescents with matched normal-weight subjects. Also, the association of these levels with metabolic conditions and inflammatory parameters is investigated.
Methods
Study subjects
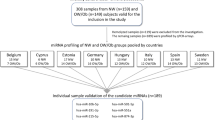
First of all, the methodology and objectives of the study were explained to all of the participants and their parents; then they signed the informed consent form completely optional. 45 obese and 45 normal-weight 10 to 18 years old participants were involved in the present cross-sectional study. The criteria for matching the obese and normal-weight groups were the age and sex of the participants. Based on the 2–20 years old growth charts of CDC, children, and adolescents with a 5 ≤ BMI < 85 percentile and with a BMI ≥ 95th percentile were categorized as normal-weight and obese groups, respectively [32]. The exclusion criteria for the current study were unwillingness to enroll in the study for any reason, history of using medications including steroids, antiepileptic, and anti-psychotic medications, and history of chronic systemic diseases, including gastrointestinal, respiratory, cardiovascular, or neurologic disease, and being involved with obesity-related syndromes including Prader-Willi.
Sample size
For sample size calculation, we used Mahdavi et al. study’s data [33]. Based on the reported correlation between mir-155 and BMI (r = -0.31). The final calculated sample size was 90 persons (refusal rate = 15%) α (two-tailed) = 0.05 β = 0.2 r = -0.31 n = 79.
Physical and anthropometric variables
The puberty status of children and adolescents was evaluated using a provided form of the Tanner stages (consisting of the pictures of five stages). The research team clarified the form to the participants; then they were asked to choose the proper stage that portrayed their physique in the most proper way. Weight, height, hip circumference (HC), waist circumference (WC), BMI (Body Mass Index), and blood pressure (systolic and diastolic) were measured after fasting for 12 h overnight. Waist to hip ratio (WHR) was calculated. Weight (Kg) was divided by height (m) square for calculating BMI. Body composition was analyzed using Tanita MC-780 S MA (Amsterdam, the Netherlands). Physical activity levels of children and adolescents were assessed by MAQ (Modifiable Activity Questionnaire). A previous study on an adolescent population has reported moderate validity and high reliability for the Persian translation of the MAQ in this age range [34].
Dietary assessment
To evaluate participants’ dietary intakes, trained interviewers used the 168 Quantitative Food Frequency Questionnaire. The validity and reliability of the questionnaire have been previously studied [35, 36]. Energy intake per day for every participant was calculated using Nutritionist IV software (version 3.5.2).
Resting energy expenditure (REE) estimation
Indirect Calorimetry using Fitmate Pro., Rome, Italy was done to measure REE (VO2 and VCO2) between 06:00 to 08:00 AM. For more accuracy, doing exercise during the day before and eating any food from 21:00 the night before the visit was forbidden for all of the children and adolescents.
Biochemical measurements
After overnight fasting of 12 hours, blood samples were taken. Levels of fasting insulin, FBG (Fasting Blood Glucose), lipid profile, and hs-CRP (high-sensitivity C - reactive protein) were measured for every participant. Enzymatic methods and colorimetry techniques were utilized for measuring serum HDL-C (High-Density Lipoprotein Cholesterol), TG (triglyceride), and FBG. The commercial kits for the calorimetry technique were provided by Pars-Azmoon Co., Tehran, Iran. ELISA method (Monobind, Lake Forest, CA, USA) was used to estimate insulin levels. Hyperinsulinemia was distinguished as following cut-off levels: higher than 30 μU/mL in the pubertal period, 20 μU/mL in the post-pubertal period, and 15 μU/mL in the pre-pubertal period [37, 38]. The equation below was used to calculate HOMA-IR [35]. (HOMA-IR= [fasting glucose (mg/dl) × fasting insulin (µIU/ml)]/405). Following cut-offs were considered for HOMA-IR to discern insulin resistance: ≥2.67 (specificity 65.5%, sensitivity 88.2%) and ≥ 2.22 (specificity 42.3%T sensitivity 100%) in boys and girls in the pre-pubertal stage respectively; ≥ 5.22 (specificity 93.3%, sensitivity 56%) and ≥ 3.82 (specificity 71.4%, sensitivity 77.1%) in boys and girls in the pubertal stage respectively [34]. Friedewald equation was employed for calculating LDL-C (Low-Density lipoprotein Cholesterol). Assessing hs-CRP levels in serum was done using the turbidimetric method. Based on gender and age, hs-CRP Reference values were spotted; Normal values in serum (mg/liter) including: (Boys: < 1.45 in 5–13 years old; < 2.13 in 14–18 years old) and (Girls: < 1.90 in 5–13 years old; < 3.33 in 14–18 years old). The subjects with MetS were diagnosed based on Cook et al. [39]. criteria, as follows: 1: HDL-C < 40 mg/dL. 2: TGs ≥ 110 mg/dL. 3: FBG ≥ 110 mg/dL . 4: WC ≥ 90th percentile for age and sex. 5: SBP and DBP ≥ 90th percentile for sex, age, and height .The subjects were categorized in the MetS group if they had at least three of the five mentioned criteria.
miRNA extraction from PBMCs
A panel of 5 miRNAs that have previously been shown to correlate with obesity and markers of metabolic disease mainly in adults or experimental models was selected [2, 24, 26, 29, 31]. Using density gradient centrifugation (Ficoll-Paque PLUS, Amersham Pharmacia Biotech, Sweden), PBMCs were isolated from ~ 4 ml peripheral blood. Phosphate-buffered saline (PBS) was used for washing isolated PBMCs. Total RNA including small RNAs was extracted by Mini Kit of miRNeasy (Qiagen, Germany). The standard stem-loop miRNA RT-qPCR method [35] was employed to synthesize the first-strand cDNA of the studied miRNAs (hsa-miR-155-5p, hsa-miR-193a-3p, hsa-miR-15a-5p, hsa-miR-122-5p, hsa-miR-146a-5p). Reverse transcriptions were performed in 10 μl reactions and the following program: 30 min at 16 °C, 30 min at 42 °C, and 10 min at 75 °C Table 1. presents the sequence of primers that were exploited in reverse transcription and qPCR reactions.
Quantitative real-time PCR
Light cycler 96 (Roche Diagnostics, Mannheim, Germany) was used to perform quantitative Real-Time PCR (qPCR) reactions using a 2 × qPCR master mix (RealQ Plus 2 × Master Mix Green without ROX, Ampliqon). Each 10 μl qPCR reaction contained the following components: 2 μl of forwarding primer (5 pmol/μl concentration), 0.5 μl of reverse primer, and, 5 μl master mix (RealQ Plus 2 × Master Mix Green without ROX, Ampliqon), 1 μl cDNA, 2 μl nuclease-free water and 1.5 μl dNTP. The qPCR reactions were performed in the following program: 15 min at 95 °C, followed by 40 cycles of 10 s at 95 °C and 30 s at 60 °C. At the end of qPCR cycles, the specificity of the reactions was evaluated by interpreting the melting curve step. To evaluate relative quantifications, the framework of Hellemans et al. Was used [40]. For a gene of interest (GOI) in each sample, ΔCq was equal to (mean Cq (GOI) in [all samples]) minus (Cq(GOI) in [that sample]). Then, relative quantities (RQs) were computed for each sample-GOI as RQ equals E(ΔCq), in which “E” was the mean efficiency of qPCR reactions for each gene. Normalized relative quantity (NRQ) for each sample-GOI was then calculated as NRQ (GOI) equals RQ (GOI) divided by the geometric mean of RQ values of the reference genes. NRQ values were converted to the Cq′ values by log2 transformation for the statistical analysis [41]. For normalizing miRNA quantities, the RQ value RNU24 was used. RNU24 is one of the stable small RNAs in PBMC which has previously been evaluated and used for normalizing miRNA quantities in PBMC in other studies [42, 43].
Statistical analysis
SPSS Version 23.0 statistical software (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. P < 0.05 was considered statistically significant. Quantitative variables are reported as mean (SD) or median (interquartile range [IQR]), as appropriate. Categorical variables are presented as numbers and percentages. Continuous variables that failed the normality test were logarithmically transformed before analysis. Non-parametric tests were used for the data that still did not have a normal distribution after this transformation. To compare differences between groups, independent samples T-test, Mann–Whitney U, or Kruskal–Wallis test were used. Spearman rank correlation coefficient (R) was used to test the association between selected miRNAs expression levels with some metabolic and inflammatory biomarkers.
Results
Anthropometric, demographic, and laboratory characteristics of obese and normal-weight children were compared and the results were shown in Table2. There was no significant difference between the two groups in age, gender, and pubertal stage variables (P > 0.05); but the mean birth weight of obese children was significantly lower than normal-weight children (P = 0.03). As expected, the mean values of weight, BMI, waist circumference, hip circumference, and WHR of obese cases were higher than the control group (p < 0.001).
Obese children had significantly higher SBP, DBP, TC (P < 0.001), LDL-C, TG (P Z 0.001), Insulin, HOMA-IR, hs-CRP, and significantly Lower HDL-C (P < 0.001). The results related to these parameters are given in detail in our previous article [44].
Among laboratory indices, WBC count was higher in obese children in comparison to normal-weight children (P = 0.01). Considering the effect of WBC count on the miRNA’s expression levels, we divided obtained miRNAs expression levels by the average WBC count in each group (obese and normal children). So, selected miRNAs expression levels per unit of WBC count among children with and without obesity are estimated and presented in Table 3. Among the five studied miRNAs, the miR-155 expression level was significantly lower in obese children compared to the normal-weight group (P-value = 0.01). After disaggregating the data by gender, the miR-155 expression level difference was significant in girls (P-value = 0.03), but not in boys. Although the expression levels of miR-122 and miR-193a were higher in obese children than in normal-weight children, the differences were not statistically significant (P-values = 0.07). Considering the gender distribution, only the difference between obese and normal girls became significant for miR-122 (P-value = 0.04). The expressions of the other two miRNAs did not differ between the two groups Table 4. presents the association of the five studied miRNAs expression levels with serum levels of insulin, HOMA-IR, fasting blood glucose, hs-CRP, IL-1ß, IL-10, and lipid profile. There was a significant positive association between the expression level of miR-122 and fasting insulin, HOMA-IR, hs-CRP, and TG (P < 0.05). The expression level of miR-193a was associated with fasting insulin, HOMA-IR, and TG level (P < 0.05) significantly and directly. MiR-155 showed a significant negative association with fasting insulin, HOMA-IR, and TG level (P < 0.05). MiR15a expression had a significant association with fasting insulin and HOMA-IR, (P < 0.05) Table 5, 6, and 7. present the comparison of miR-193a, mir122, and mir155 expression levels among children with and without some metabolic status (including obesity, metabolic syndrome indices, and different levels of REE, different body composition, hyper-insulinemia, insulin resistance, and high hs-CRP respectively. The median (IQR) expression level of miR-193a was significantly higher in children with metabolic syndrome, high TG, larger WC, insulin resistance, and high-fat mass (for a review of P-values between two groups, cf Table 5). There was also a significant difference in the expression level of miR-193a among children with slow REE and fast REE (P = 0.008). We couldn’t find any significant difference in miR-193a expression level of children with increased FBG, hyperinsulinemia, higher SBP/DBP, lower HDL, and higher hs-CRP with children who were in the normal spectrum for these biomarkers. Also, the expression level of miR-193a was not significantly different among children with different muscle mass.
The median (IQR) expression level of miR-122 was higher in children with metabolic syndrome, high-fat mass, high hs-CRP, larger WC, and insulin resistance significantly (for a review of P-values between two groups, cf Table 6). We found no significant difference in the miR-122 expression level of children with increased FBG, higher TG, higher SBP-DBP, lower HDL, hyperinsulinemia, and children with different REE with children who were in the normal range for these factors. Also, the expression level of miR-122 was not significantly different among children with different muscle mass. The median (IQR) expression level of miR-155 was significantly lower in children with high hs-CRP and high-fat mass compared to the normal group (for a review of P-values between two groups, cf Table 7). Similar analyses were done for miR-15a and miR-146 expression levels; we find no significant association between miR-15a and miR-146 with metabolic status, so the data were not reported.
Discussion
Circulating miRNA concentrations have been suggested to be associated with a variety of metabolic diseases such as obesity and type 2 diabetes [20, 21, 45, 46]. Obesity-related miRNAs have been called potential biomarkers for the prevention and diagnosis of obesity and obesity-related metabolic disorders [46]. Obtained evidence also indicated that obesity-related miRNAs are promising new therapeutic tools for curing obesity and related diseases [46]. The current cross-sectional study was performed to compare the expression levels of miR-193a, miR-122, miR-155, miR-15a, and miR-146a, in peripheral blood mononuclear cells of obese children and adolescents with normal weight groups. The relation of expressed miRNAs with fasting insulin, HOMA-IR, fasting blood glucose, lipid profile and some inflammatory biomarkers were also assessed. Furthermore, the relation of differentially expressed miRNAs with some metabolic status (including metabolic syndrome, different body composition, hyper-insulinemia, insulin resistance, REE and high hs-CRP was evaluated.
Among the five studied miRNAs, obese children significantly had lower miR-155 than normal-weight children. After disaggregating the data by gender, the observed relationship was in place only for girls. MiR-155 had a negative association with fasting insulin, HOMA-IR, and hs-CRP. Mahdavi et al. showed that obese non-diabetic subjects had lower serum levels of miR-155 than normal-weight non-diabetic individuals [33]. Mazloom et al. reported that the expression of miR-155 in PBMC cells of diabetic patients was reduced compared to the control group [47]. They also reported a negative association between miR-155 and BMI, serum cholesterol, fasting insulin, HOMA-IR, and WC in the diabetic group [47]. According to previous studies, miR-155 plays a crucial role in the metabolism of cholesterol, and fatty acids in the liver through a direct effect on the regulatory factor X receptor alpha (LXRa). LXRa is involved in the regulation of many genes that contribute to fat metabolism [30, 31]. In animal models, reduction of miR-155 levels increases the risk of NAFLD in diabetic patients. In return, the miR-155 increase has a protective role in slowing NAFLD progression [31]. In line with these observations, in our study, the miR-155 was significantly lower in children with high fat-mass and insulin resistance compared to normal children.
In the present study, although the expression levels of miR-193a and miR-122 were higher in obese children, these observations were statistically significant only for Mir122 in girls. We found no previous study that compared the miR-193a expression level of obese children and adolescents with normal-weight controls, but similar studies had been done on adult participants. Some studies reported blood levels of miR-193a and miR-122 are elevated in participants with obesity, pre-diabetes, diabetes, insulin resistance, liver damage, and cardiovascular disorders significantly [48,49,50,51,52,53,54]. The possible reasons for this inconsistency could be due to different participant ages, the low sample size, and the metabolic phenotype of the studied children than the other studies. In this study, 55% of obese children did not have any obesity associated metabolic disorders like as metabolic syndrome and insulin resistance, While this percentage has been reported as 20-30% in other previous studies [7, 9]. Hess et al. (2020) assessed the serum levels of some miRNAs before and after a weight loss diet [55]. They showed that serum levels of miR-122 and miR-193a were reduced after an average weight loss of 5.7 Kg. They also demonstrated the levels of these miRNAs were positively correlated with metabolic syndrome, serum insulin, HOMA-IR, BMI, waist circumference, lean body mass, and visceral adipose tissue at the baseline. MiR-122 and miR-193a also had a positive correlation with TG level and fat mass, respectively [55]. In a recent study, serum levels of miR-29a and miR-122 were compared between obese with T2DM, obese without T2DM, and normal-weight children [56]. They also reported the positive relationship between the assessed miRNAs and waist circumference, BMI, TG, insulin, HOMA-IR, IL-6, hs-CRP, and TNF-a [56]. Wang et al. showed serum levels of miR-122 had a significant direct correlation with BMI, triglyceride, and HOMA-IR index, and a significant inverse correlation with HDL cholesterol levels [24]. Also, in this study, miR-122 was associated with an increased odds of insulin resistance in humans. Therefore, they suggested circulating miR-122 levels may act as a marker of obesity and insulin resistance [24]. Lischka et al. (2021) reported that miR-122 is positively correlated with HOMA-IR, TG, cholesterol and ALT as metabolic biomarkers and TNF-α, IL-1Ra, and pro-calcitonin as inflammatory biomarkers in pediatric patients. They also reported positive correlation of miR-193b with cholesterol, ALT, and MRI PDFF (magnetic resonance imaging-proton density fat fraction). On the other hand, miR-122 and miR-193b had no significant association with CRP and IL-6. Moreover, Lischka et al. revealed miR-122 expression level of patients with pre diabetes, impaired glucose tolerance or metabolic syndrome was significantly different from those obese children without these conditions [57].
In line with the mentioned studies, in the current study, miR-193a and miR-122 had a significant positive association with fasting insulin level, HOMA-IR, and TG. There was also a positive significant association between miR-122 and hs-CRP. The following comparative analysis conducted between these two miRNAs and some metabolic status showed expression levels of both were higher in children with metabolic syndrome, insulin resistance, and high-fat mass. Furthermore, expression levels of miR-193a and miR-122 were also higher in children with fast REE (than slow REE) and children with high hs-CRP, respectively.
Also, the present study could not find a significant difference in the expression of miR-15 between the two groups. However, previous studies have shown that miR-15 expression is reduced in type 2 diabetes, metabolic syndrome, and obesity, thereby miR-15 is known as a diagnostic biomarker for obese children at risk of type 2 diabetes mellitus [2]. Lischka et al., in 2021 reported miR-15a expression level was significantly lower in IGT pediatric patients [57]. In the current study, miR-15a had a significant association with serum insulin and HOMA-IR. this result was in line with previous observations regarding miR-15a importance as a predictor of diabetes in obese people regarding down-regulation of miR-15a in hyperglycemic conditions [58]. In the present study, none of the children had FBS higher than the normal range (neither obese children nor normal weight children), which may be the reason for observing no significant difference in the miR-15a level between the two study groups. In the present study, there was no significant difference between the two groups for the expression of miR-146a. Chartoumpekis et al. compared the expression levels of 530 miRNAs in adipose tissue of mice feeding a standard diet and mice feeding a high-fat diet. For the first time, they showed that miR-146a, miR-146b, and miR-379 were up-regulated during the development of obesity [59]. Ortego et al. reported that obese participants after Bariatric Surgery lost about 30 percent of their original weight and miR-146a was up-regulated by about 146% [60]. Sharma et al. designed a case-control study to investigate the relation of adipose tissue miRNAs with insulin sensitivity. They couldn’t find a significant difference in miR-146 expression level between the participants with and without insulin resistance, but the miR-146a and miR-146b had a significant correlation with body fat percentage, BMI, and insulin sensitivity index [29].
A few shortcomings of the study that can be improved in the future is to have a group of overweight children included to compare with obese and normal-weight children. Secondly, due to the cross-sectional design of the study cause and effect relationship could not be marked. Therefore, planning further studies to assess cause-effect correlations seems essential. For future studies, it is recommended that participants be categorized into two groups, metabolically healthy obese and metabolically unhealthy obese. Besides, considering groups of obese children with diabetes and metabolic syndrome will help grasp the affiliation of miRNAs with these diseases.
Conclusions and future directions
In conclusion, among the five studied miRNAs (miR-193a, miR-122, miR-155a, miR-15a, and miR-146), only the expression level of miR-155 was significantly different in PBMC of obese children compared to the normal group (lower in obese children). Moreover, the expression level of miR-155 was negatively associated with fasting insulin and HOMA and also significantly lower in children with high hs-CRP and high-fat mass compared to the normal group. MiR-193a and miR-122 were positively correlated with insulin, HOMA, and TG. MiR-122 also was correlated with hs-CRP. After disaggregating the data by gender, the expression levels of miR-122 were higher in obese girls than normal-weight girls.
The expression levels of both miR-122 and miR-193a were higher in children with metabolic syndrome, insulin resistance, and high fat mass. Furthermore, the expression levels of miR-193a and miR-122 were also higher in children with fast REE (than slow REE) and high hs-CRP, respectively. Despite the limitations of our study, expression levels of miR-193a, miR-122, and miR-155a seem to be associated with some metabolic statuses, including obesity, metabolic syndrome, hyperinsulinemia, insulin resistance, and hyperlipidemia in obese children. Thereby, using the expression pattern of miRNAs in obese children and adolescents as a predictive marker of adulthood chronic disease appears to be very helpful. Further studies are suggested to evaluate the relationships and underlying mechanisms to achieve therapeutic interventions.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PBMC:
-
Peripheral blood mononuclear cells
- REE:
-
Resting energy expenditure
- hs-CRP:
-
High-sensitivity C-reactive protein
- WC:
-
Waist circumference
- HC:
-
Hip circumference
- BMI:
-
Body mass index
- WHR:
-
Waist to hip ratio
- TG:
-
Triglyceride
- HDL-C:
-
High-density lipoprotein cholesterol
- CVD:
-
Cardiovascular disease
- FFQ:
-
Food frequency questionnaire
- IL:
-
Interleukin
- LDL-C:
-
Low-density lipoproteins cholesterol
- MetS:
-
Metabolic syndrome
- IR:
-
Insulin resistance
- FBG:
-
Fasting blood glucose
- HOMA-IR:
-
The homeostatic model assessment of insulin resistance
- TNF-α:
-
Tumor necrosis factor-α
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- MAQ:
-
Modifiable Activity Questionnaire
- CDC:
-
Charts of centers for disease control and prevention
- GOI:
-
Gene of interest
- RQ:
-
Relative quantities
- NRQ:
-
Normalized relative quantity
References
Youssef EM, et al. Expression profiling and analysis of some miRNAs in subcutaneous white adipose tissue during development of obesity. Genes Nutr. 2020;15(1):8. https://doi.org/10.1186/s12263-020-00666-0.
Cui X, et al. Change in circulating microRNA profile of obese children indicates future risk of adult diabetes. Metabolism. 2018;78:95–105.
Hatipoglu N, et al. Waist circumference percentiles for 7- to 17-year-old Turkish children and adolescents. Eur J Pediatr. 2008;167(4):383–9. https://doi.org/10.1007/s00431-007-0502-3. (Epub 9 May 2007).
Fau Kissebah Ah, Vydelingum N, et al. Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab. 1982;54(2):254–60. https://doi.org/10.1210/jcem-54-2-254.
Akinci G, et al. Evaluation of markers of inflammation, insulin resistance and endothelial dysfunction in children at risk for overweight. Hormones. 2008;7(2):156–62. https://doi.org/10.1007/BF03401507.
Park JH, et al. Murine hepatic miRNAs expression and regulation of gene expression in diet-induced obese mice. Mol Cells. 2010;31(1):33–8. https://doi.org/10.1007/s10059-011-0009-7. (Epub 25 Nov 2010).
Blüher S, Schwarz P. Metabolically healthy obesity from childhood to adulthood - Does weight status alone matter? Metabolism. 2014;63(9):1084–92. https://doi.org/10.1016/j.metabol.2014.06.009. (Epub 19 Jun 2014).
Landgraf K, et al. Evidence of early alterations in adipose tissue biology and function and its association with obesity-related inflammation and insulin resistance in children. Diabetes. 2015;64(4):1249–61. https://doi.org/10.2337/db14-0744. (Epub 12 Nov 2014).
Prince RL, et al. Predictors of metabolically healthy obesity in children. Diabetes Care. 2014;37(5):1462–8.
Blüher M. The distinction of metabolically “healthy” from “unhealthy” obese individuals. Curr Opin Lipidol. 2010;21(1):38–43. https://doi.org/10.1097/MOL.0b013e3283346ccc.
Vukovic R, et al. Children With Metabolically Healthy Obesity: A Review. Front Endocrinol. 2019:10(865):865–75. https://doi.org/10.3389/fendo.2019.00865.
Dexheimer PJ, Cochella L. MicroRNAs: From Mechanism to Organism. Front Dev Biol. 2020;8:409–26. https://doi.org/10.3389/fcell.2020.00409.
Foltz JL, et al. Population-level intervention strategies and examples for obesity prevention in children. Annu Rev Nutr. 2012;32:391–415.
Kumar S, et al. Decreased Circulating Levels of Spexin in Obese Children. J Clin Endocrinol Metab. 2016;101(7):2931–6.
Pandita A, et al. Childhood obesity: prevention is better than cure. Diabetes, metabolic syndrome and obesity : targets and therapy. 2016;9:83–9.
Dumortier, O., E. Hinault C Fau - Van Obberghen, and E. Van Obberghen, MicroRNAs and metabolism crosstalk in energy homeostasis, in Cell Metab 312–24. doi: https://doi.org/10.1016/j.cmet.2013.06.004. Epub 2013 Jul 11.
Fritz JV, et al. Sources and Functions of Extracellular Small RNAs in Human Circulation. Annu Rev Nutr. 2016;17(36):301–36. https://doi.org/10.1146/annurev-nutr-071715-050711. (Epub 13 May 2016).
Ross SA, Davis CD. The emerging role of microRNAs and nutrition in modulating health and disease. Annu Rev Nutr. 2014;34:305–36.
Sun W, et al. microRNA: a master regulator of cellular processes for bioengineering systems. Annu Rev Biomed Eng. 2010;12:1–27.
Fischer-Posovszky P, et al. Functional Significance and Predictive Value of MicroRNAs in Pediatric Obesity: Tiny Molecules with Huge Impact? Horm Res Paediatr. 2016;86(1):3–10.
Nesca V, et al. Identification of particular groups of microRNAs that positively or negatively impact on beta cell function in obese models of type 2 diabetes. Diabetologia. 2013;56(10):2203–12. https://doi.org/10.1007/s00125-013-2993-y. (Epub 2013 Jul 11).
Xu J, et al. Several circulating miRNAs related to hyperlipidemia and atherosclerotic cardiovascular diseases. Lipids Health Dis. 2019;18(1):104.
Shah R, et al. Extracellular RNAs are associated with insulin resistance and metabolic phenotypes. Diabetes Care. 2017;40(4):546–53.
Wang R, et al. Elevated circulating microRNA-122 is associated with obesity and insulin resistance in young adults. Eur J Endocrinol. 2015;172(3):291–300.
Chakraborty C, et al. Influence of miRNA in insulin signaling pathway and insulin resistance: micro-molecules with a major role in type-2 diabetes. Wiley Interdiscip Rev RNA. 2014;5(5):697–712. https://doi.org/10.1002/wrna.1240. (Epub 18 Jun 2014).
Párrizas M, et al. Circulating miR-192 and miR-193b are markers of prediabetes and are modulated by an exercise intervention. J Clin Endocrinol Metab. 2015;100(3):E407–15.
Alexander R, L. Lodish H Fau - Sun, and L. Sun,. MicroRNAs in adipogenesis and as therapeutic targets for obesity. Expert Opin Ther Targets. 2011;15(5):623–36. https://doi.org/10.1517/14728222.2011.561317. (Epub 28 Feb 2011).
Williams, M.D. and G.M. Mitchell, MicroRNAs in insulin resistance and obesity, in Exp Diabetes Res. 2012;2012:484696. doi: https://doi.org/10.1155/2012/484696. Epub 2012 Jul 18.
Sharma NK, et al. Obesity associated modulation of miRNA and co-regulated target transcripts in human adipose tissue of non-diabetic subjects. Microrna. 2015;4(3):194–204.
Miller, A.M., et al., MiR-155 has a protective role in the development of non-alcoholic hepatosteatosis in mice, in PLoS One. p. e72324. doi: https://doi.org/10.1371/journal.pone.0072324. eCollection 2013.
Wang, B., et al., Role of microRNA-155 at early stages of hepatocarcinogenesis induced by choline-deficient and amino acid-defined diet in C57BL/6 mice, in Hepatology. p. 1152–61. doi: https://doi.org/10.1002/hep.23100.
Kuczmarski RJ, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190.
Mahdavi R, et al. Decreased serum level of miR-155 is associated with obesity and its related metabolic traits. Clinical Laboratory. 2018;64(1):77–84.
Delshad M, et al. Reliability and validity of the modifiable activity questionnaire for an Iranian urban adolescent population. Int J Prev Med. 2015;6:3.
Esfahani FH, et al. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. J Epidemiol. 2010;20(2):150–8.
Asghari G, et al. Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran Lipid and Glucose Study. Br J Nutr. 2012;108(6):1109–17.
Ten S, Maclaren N. Insulin resistance syndrome in children. J Clin Endocrinol Metab. 2004;89(6):2526–39.
Kurtoglu S, et al. Insulin resistance in obese children and adolescents: HOMA-IR cut-off levels in the prepubertal and pubertal periods. J Clin Res Pediatr Endocrinol. 2010;2(3):100–6.
Cook S, et al. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988–1994. Arch Pediatr Adolesc Med. 2003;157(8):821–7. https://doi.org/10.1001/archpedi.157.8.821.
Hellemans J, et al. qBase relative quantification framework and software for management and automated analysis of real-time quantitative PCR data. Genome Biol. 2007;8(2):R19.
Rieu I, Powers SJ. Real-Time Quantitative RT-PCR: Design, Calculations, and Statistics. Plant Cell. 2009;21(4):1031–3.
Bastami M, et al. Perturbation of miR-146b and relevant inflammatory elements in esophageal carcinoma patients supports an immune downregulatory mechanism. Pathol Res Pract. 2021;225(153560):20.
Saadatian, Z., et al.,Dysregulated expression of STAT1, miR-150, and miR-223 in peripheral blood mononuclear cells of coronary artery disease patients with significant or insignificant stenosis, in J Cell Biochem. 2019. p. 19810–19824. doi: https://doi.org/10.1002/jcb.29286. Epub 2019 Jul 18.
Behrooz M, Vaghef-Mehrabany E, Ostadrahimi A. Different spexin level in obese vs normal weight children and its relationship with obesity related risk factors. Nutr Metab Cardiovasc Dis. 2020;30(4):674–82.
Peng M, Yang X. Controlling diabetes by chromium complexes: The role of the ligands. J Inorg Biochem. 2015;146:97–103.
Ji CA-O, Guo XA-O. The clinical potential of circulating microRNAs in obesity. Nat Rev Endocrinol. 2019;15(12):731–43. https://doi.org/10.1038/s41574-019-0260-0. (Epub 2019 Oct 14).
Mazloom H, et al. Downregulated microRNA-155 expression in peripheral blood mononuclear cells of type 2 diabetic patients is not correlated with increased inflammatory cytokine production. Cytokine. 2015;76(2):403–8.
Chang K-P, et al. MicroRNA signatures in ischemia-reperfusion injury. Annals of plastic surgery. 2012;69(6):668–71.
Fang L, et al. Circulating microRNAs as biomarkers for diffuse myocardial fibrosis in patients with hypertrophic cardiomyopathy. Journal of translational medicine. 2015;13(1):314.
Holvoet P, et al. The metabolic syndrome, circulating oxidized LDL, and risk of myocardial infarction in well-functioning elderly people in the health, aging, and body composition cohort. Diabetes. 2004;53(4):1068–73.
Luo X, et al. Regulation of human cardiac ion channel genes by microRNAs: theoretical perspective and pathophysiological implications. Cellular Physiology and Biochemistry. 2010;25(6):571–86.
Yamada H, et al. Associations between circulating microRNAs (miR-21, miR-34a, miR-122 and miR-451) and non-alcoholic fatty liver. Clin Chim Acta. 2013;424:99–103.
Yi F, et al. MicroRNA-193-5p modulates angiogenesis through IGF2 in type 2 diabetic cardiomyopathy. Biochemical and biophysical research communications. 2017;491(4):876–82.
Oses MA-O, et al. Circulating miRNAs as Biomarkers of Obesity and Obesity-Associated Comorbidities in Children and Adolescents: A Systematic Review. Nutrients. 2019;11(12):2890. https://doi.org/10.3390/nu11122890.
Hess AL, et al. Levels of Circulating miR-122 are Associated with Weight Loss and Metabolic Syndrome. Obesity. 2020;28(3):493–501.
Mohany KM, et al. Investigation of the levels of circulating miR-29a, miR-122, sestrin 2 and inflammatory markers in obese children with/without type 2 diabetes: a case control study. BMC Endocrine Disorders. 2021;21(1):152.
Lischka JA-O, et al. Circulating microRNAs 34a, 122, and 192 are linked to obesity-associated inflammation and metabolic disease in pediatric patients. Int J Obes (Lond). 2021;45(8):1763–72. https://doi.org/10.1038/s41366-021-00842-1. (Epub 2021 May 13).
Ye E-A, Steinle JJ. miR-15b/16 protects primary human retinal microvascular endothelial cells against hyperglycemia-induced increases in tumor necrosis factor alpha and suppressor of cytokine signaling 3. Journal of neuroinflammation. 2015;12(1):1–8.
Chartoumpekis DV, et al. Differential expression of microRNAs in adipose tissue after long-term high-fat diet-induced obesity in mice. PLOS ONE. 2012;7(4):e34872.
Ortega FJ, et al. Targeting the circulating microRNA signature of obesity. Clin Chem. 2013;59(5):781–92.
Acknowledgements
The authors would like to thank all the subjects who eagerly participated in the current study. Although, we would like to thank Miss. A. Daneshvar for reviewing the article and editing English spelling
Funding
The study was supported financially by Research Vice Chancellor, and Nutrition Research Center of Tabriz University of Medical Sciences, as a thesis proposal for Ph.D. degree of the First author.
Author information
Authors and Affiliations
Contributions
This study was conceptualized by Milad B, AO and Maryam B Data collection was performed by Maryam B and HK. Formal analysis was conducted by Maryam B and SH, and funding acquisition was by Maryam B. Investigation was carried out by Maryam B and SH, and methodology was set by Milad B and Maryam B. The study was supervised by AO and Milad B. Writing of the original draft was performed by Maryam B and SH. Reviewing and editing were carried out by AO, Milad B, Maryam B, SH and HK. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the research ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1397.179). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all subjects or parents on behalf of children after explaining the objective of the study to each of the study participants.
Consent for publication
Written informed consent for publication of their clinical details and/or clinical images was obtained from the patient/parent/guardian/ relative of the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Behrooz, M., Hajjarzadeh, S., Kahroba, H. et al. Expression pattern of miR-193a, miR122, miR155, miR-15a, and miR146a in peripheral blood mononuclear cells of children with obesity and their relation to some metabolic and inflammatory biomarkers. BMC Pediatr 23, 95 (2023). https://doi.org/10.1186/s12887-023-03867-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-03867-9