Abstract
Background
Accessibility and utilization of postnatal newborn check-ups within 2 days after delivery are critical for a child’s survival, growth, and development. However, the service delivery is not yet improved and fluctuates across the geographical locations in Ethiopia. Therefore, this study aimed to assess the spatial distribution and determinants of newborns not received postnatal check-ups within 2 days after birth in Ethiopia.
Methods
A secondary data analysis of the Ethiopia Demographic and Health Survey (EDHS) 2016 was done among live births within 2 years preceding the survey. A multilevel binary logistic regression model was fitted to identify the factors associated with the outcome variable. Adjusted Odds Ratio with 95% (Confidence Interval) was calculated and used as a measure of associations and variables with a p-value < 0.05, were declared as statistically significant.
Results
A total of 4036 live newborns in Ethiopia were included in the analysis, of whom half (51.21%) were females. The mean age of the mothers was 33+ SD 1.3, and more than 60 % (61.56%) of the mothers were not educated. The national prevalence of newborns not receiving postnatal check-ups within 2 days after birth was 84.29 (95% CI: 83.10–85.41) with significant spatial variations across the study area. Mothers who had no ANC visits were 58% higher than (AOR = 0.42(0.27–0.66) mothers who had > 4 ANC visits. Mothers who gave birth at home and others were 80% (AOR = 0.02(0.01–0.29) and 25% (AOR = 0.76(0.59–0.99), higher than mothers delivered at hospital. Rural mothers were 1.90 times higher (AOR = 1.90(1.29–2.81) than urban mothers, and mothers live in administrative regions of Afar 66% (AOR = 0.34(0.16–0.69), Oromia 47% (AOR = 0.53(0.30–0.91), Somali 60% (AOR = 0.40 (0.22–0.74),Benishangul 50% (AOR = 0.50 (0.27–0.92), SNNPR 67% (AOR = 0.33(0.19–0.57), Gambela 70% (AOR = 0.30 (0.16–0.56), Harari 56% (AOR = 0.44 (0.25–0.78), and Dire Dawa70% (AOR = 0.30 (0.17–0.54) were higher than Addis Abeba for not receiving postnatal checkup of new born within the first 2 days, respectively.
Conclusions
Low postnatal check-up utilization remains a big challenge in Ethiopia, with significant spatial variations across regional and local levels. Spatial clustering of not receiving postanal check-ups within 2 days was observed in Afar, Oromia, Gambela, Benishangul, SNNPR, Harari, and Dire Dawa regions. Residence, ANC visits, place of delivery, and administrative regions were significantly associated with not receiving postnatal check-ups. Geographically targeted interventions to improve ANC follow-up and institutional delivery should be strengthened.
Similar content being viewed by others
Background
The postnatal period is a critical time for the survival of mothers and newborn babies. More than 50% of child death is within the first 2 days. Lack of postnatal care in this sensitive period might result in complications and deaths of the newborn and the mothers [1,2,3]. Hence, theWorld Health Organization (WHO) recommends, that all newborns and mothers should receive high-quality postnatal care within the first 42 days. For the mother who is delivered at home,the first postpartum visit must be as early as possible within 24 hours of birth. Aminimum of three postnatal health checks are suggested for both mothers and newborns on day 3 (48-72 hours), within7–14 days, and at 6 weeks [4,5,6]. Infant feeding, history of convulsion, fast breathing, spontaneous movement, hypothermia, hyperthermia, jaundice, cord, eyes, hygiene, and immunization status were assessed at each postnatal contact [2, 7].
Globally, 2.4 million newborns died in the first month of life, with nearly half (47%) of thedeaths having occurred in thefirst 2 days [8]. The burden of maternal and newborn mortality is high in Africa. Each year, nearly 125,000 women and 870,000 newborns die in the first week of life [9]. Sub-Sahara Africa is among the most affected area with an estimated1.16 million babies dying in the first 28 days and 850,000 in the first week of life [1, 7, 10, 11].
Even though progress has been made in reducing maternal and child mortality in Ethiopia, neonatal morality is still increasing from 29 in 2016 to 33 in 2019 [8], with significant spatial variations. Hince, understanding the spatial variations of low postnatal check-ups within 2 days after delivery is critical to come up with evidence-based geographically targeted interventions.
WHO recommends a postnatal check-up within 2 days after delivery to reduce neonatal mortality [1]. The first 2 days are the most critical time for the survival of the newborn. Unable to provide timely postnatal care at this stage will result in complications and even death. According to the 2019Ethiopian Demography Health Survey(EDHS), only 35% of newborns had received a postnatal check within 48 hrs after birth [12]. Postnatal care is the most neglected service in Ethiopia [4].
Previous studies identified different factors associated with low postnatal check-ups such as maternal age, birthorder, wealth status, delivery sites, residences, ANC follow-up, and maternal education [12].
In recent decades, efforts have been made to increase postnatal care, which in turn reduces neonatal mortality through the Sustainable Development Goal (SDG4), [13,14,15]. The Ethiopian government has also made a significant improvement to increase postnatal care by training and recruiting community health extension workers [2]. However, the postnatal care coverage is very low with significant spatial variations, which range from 0.1% in Afar to 74% in Addis Ababa [12]. Thus, investigating the spatial variations and determinants of low postnatal check-ups has important for the prevention and early identification of infant problemsand to meet the SDG4 goal, which aimed to reduce child mortality to 25/1000 live birth by 2030 [16]. A geographically linked data analysis using population and health facility data is important to map the low coverage of postnatal check-ups and identify inequalities in service access and provision [17, 18]. Therefore, this study aimed to investigate the spatial variations and determinants of low postnatal care coverage within two-day after birth in Ethiopia to come up with geographically targeted interventions to increase the postnatal check-ups within 2 days.
Methods
Study area
The study was done in Ethiopia using theEthiopian Demographic Health Survey 2016. Ethiopia is among the oldestcountry worldwide, which is located in the Horn of Africa at 3′ and 14.8″ latitude 33′ and 48′ longitude. The countryis bordered by Sudan in the west, Somalia and Djibouti in the east, Eritrea in the north, and Kenya in the south. The country has a surface area of1,112,000 km2. It is a rugged, landlocked country split by the Great Rift Valley, with archaeological finds dating back more than 3 million years; it’s a place of ancient culture. Among the important sites in Lalibela with its rock-cut Christian churches from the 12th–13th centuries. Aksum is the ruins of an ancient city with obelisks, tombs, Our Lady Mary of Zion church, and Gondar Fasil castles. Ethiopia is the 10th largest and the 2nd-most populous country in Africa after Nigeria. Administratively Ethiopia has ten regions (Tigray, Afar, Amhara, Benshangul, Gambela, Harari, Oromia, Somali, Southern, Nations, Nationalities, and People’s Region (SNNPR), and Sidama (a recently added and two city administrations (Addis Ababa and Dire Dawa). Concerning resident, 79.2% of the Ethiopian population lives in rural, and 43.3% is under fifteen ages [19]. Ethiopia uses a three-tier healthcare system; 1) primary healthcare systemconsists of health posts, health centers, and primary hospitals, 2) secondary healthcare consists of zonal hospitals, and 3) tertiary healthcare consists of comprehensive specialized hospitals [20].
Study Design
Across-sectional retrospective study design was conducted to assess the geospatial variation and determinants of newborns not receiving postnatal check-ups within 2 days after birth.
Source of data
The data used in this article were obtained from the Ethiopia Demography and Health Survey (EDHS) 2016, which was accessed at the MEASURE DHS website after securing a formal request to the MEASURE DHS program. The survey was carried out by the central statistics agency of Ethiopia, and the Ethiopia Public Health institute Ethiopia with the technical assistance provided by ICF International. The authors requested the measure DHS trough briefly stating the objectives of this analysis and access was granted to use the data on the (http://dhsprogram.com) website [21].
Sampling and populations
The source population of this study was all mothers with newborns born in the last 2 years preceding the survey. Multi-stage stratified cluster sampling was used to select the study participants. In the first stage, 645 clusters or enumerations areas were selected randomly, and stratified into urban and rural. In the second stage, a fixed number of 28 households in each cluster was randomly selected [21]. Geographic coordinates of each survey cluster were also collected using Global Positioning System (GPS) [21]. Mothers aged 15–49 and children born within the 2 years preceding the survey in each selected household were subjected to our study.
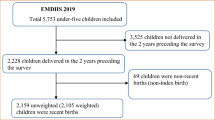
The study was conducted among (3832 un-weighted and 4036 weighted frequency) newborns to assess the postnatal health checkups within 2 days after delivery (Fig. 1).
Study variables
Outcome variable
The outcome variable for this study is postnatal check up within the first 2 days after birth. The under five data sets (KR) files, EDHS 2016 were used for this analysis, by computing the selected function of postnatal care for new born within the first 2 days after birth and relating variables. The computing variables were Cord examined (m78a) + Temperature measured (m78b) + Counseling on danger signs (m78c) + Counseling on breastfeeding (m78d) + Observation of breastfeeding (m78e). It was recorded as “No(0)” for new born not receiving a postnatal check within 2 days after birth and “yes [1]” new born receiving a postnatal check within 2 days after birth.
Independent variables
The independent variables used in this study were as nested into; 1) individual levelfactorssuch as marital status, maternal age, religion, maternal occupation, maternal education, residence, sex of newborn, wealth index, number of ANC, place of delivery, size of the newborn at birth and number of living children inthe family. 2) Community level factors such as region,distance to the health facility, community illiteracy level, health insurance, media exposure, access to electricity, access to safe water, and community poverty. Some of the community-level factors were aggregated from the individual-level factors.
Data management and analysis
We performed a secondary analysis of the EDHS 2016, using the Kids Records (KR) dataset. STATA version 14 and Microsoft Excel 16 were used for data cleaning and coding, and the spatial analysis, and mapping were done using ArcGIS version 10.8. Descriptive statistics such as frequency and percentage of different variables were computed and presented using texts, tables, and graphs.
After preparing the data we imported the data to ArcGIS version 10.8. Joining the outcome with the GPS data and projections of the Geographically coordinated data to the projected coordinatedata were conducted before the analysis. Spatial autocorrelation analysis was done to test whether there is spatial variation across the study area. The spatial autocorrelation test signifies whether there is clustering or dispersion of postnatal check-ups within 2 days after birth. The value of the Morans Index is standardized into Z-score. Positive Morans Index value with positive Z-score (> 1.96, P-value< 0.05) indicates clustering/ hot spots areas. Negative Morans Index value with a negative Z-score (<− 1.96, P-value1.96 (P < 0.05) was considered a cold spot area. GetisOrd Gi* statistic was applied to detect hotspot area or spatial clustering of newborns not receiving postnatal check-ups. Ordinary kriging interpolation was used to estimate/ predict the spatial distributions of not receiving a postnatal check within 2 days after delivery.
A multilevel binary logistic regression model was applied for each independent variable and p-value < 0.2 were entered into the multivariable multilevel logistic regressions model. The adjusted odds ratio was calculated and used as the measure of association between the dependant and independent variables, and variables having a p-value < 0.05, 95% CI were considered statistically significant.
In the EDHS data, the newborn is nested within a cluster, newborns within the same cluster were more similar to each other than within different clusters. Therefore, this violates the standard regression model assumptions, which are independence of observation and equal variance across the cluster assumptions. This implies they need to take into account between-cluster variables by using an advanced model. Therefore, a multilevel random intercept logistic regression model was fitted to estimate the association between individual-level and community-level factors and the likelihood of new-born not receiving postnatal care within 2 days after birth. Models were compared based on deviance (−2log likelihood) since the models were nested. Log-likelihood and intracellular correlation coefficient (ICC) was computed to measure the variation between clusters. The ICC indicates the degree of heterogeneity of new- born not receiving postnatal care within 2 days after birth. A multilevel binary logistic regression analysis was performed to examine the effects of individual and community level factors on newborns not receiving postnatal check-ups within 2 days after birth to identify individual and community level factors.
Results
Socio-demographic characteristics of the newborn
A total of 4036 weighted live birthswere included in this analysis, of whom nearly half (48.79%) of the newborns were males. The mean ages of the mother were 33+ SD 1.3 and near to one-third of the mothers (29.26%) were between the age group of 25 and 29 years. Near to 60 % of mothers, (58.97%) were unemployed, and more than 60 % (61.59%) were not educated. The majority (88.77%) of the study participants were residing in rural and nearly half (47.5%) of the mothers were in a poor wealth status (Table 1).
Maternal and child characteristics
More than one-third (36.04%) of mothers hadnoANC visits, and 63.64% of the mother were delivered at home. Among mothers, 53.85% had 1–3 live children in their families. The majority (96.51%) of the study participants have not used health insurance, 61.28% of the mother had a big problem reaching the health facilities, and near to 50% of the community (47.39%) were illiterate. Around 40%, (38.98%) and (72.31%) of the mother have no access to media, and electricity (Table 2).
The prevalence of newborns not receiving postnatal check-ups within 2 days
The overall prevalence of not receiving postnatal check-ups within 2 days after birth in Ethiopia was 84% (Fig. 2). The postnatal check-ups within 2 days were higher in Addis Ababa and Tigray regions, whereas, low postnatal check-ups were observed in Afar, Somali and Gambela regions (Fig. 3).
Spatial analysis result
Spatial autocorrelation
The spatial autocorrelation analysis result showed that newborns not receiving a postnatal check-up within 2 days after delivery significantly varied across Ethiopia, with a Global Moran’s I value of 0.47, p-value< 0.0001, and z-score 7.13. This indicates that the newborn not receiving postnatal check-upswithin the first 2 days after birth in Ethiopia has spatial dependence (Fig. 4).
Hotspot analysis of the newborns not receiving postnatal check-upsin Ethiopia
In the hotspot map, significant spatial clustering of not receiving postanal check-ups within 2 days after birth was observed in Eastern (Somali), Northeastern (Afar), Southern (Oromia and SNNPR), and Western (Gembela and Benshangul) parts of Ethiopia. Whereas, spatial dispersion of newborns not receiving postnatal check-ups was observed in Northern, Central, and Southern parts of the country specifically in regions of Tigray, Amhara, and Addis Abeba (Fig. 5).
Satscan analysis of newborns not reciving postnatal check-up within 2 days after birth
Purely Spatial analysis scanning for clusters with high rates was applied using the Bernoulli model. A total of 287 significant clusters of newborns not receiving postnatal check-ups were specified, of which 41 and 100 were primary (most likely clusters) and secondary clusters, respectively. The primary cluster, was found in the Eastern (Somali region) of Ethiopia at 5.589269 N, 44.175032 E geospatial locations, with a relative risk of 1.47 and log-likelihood ratio (LLR) of 48.1 at a p-value< 0.0001. Those shows mothers who lived in this spatial window is 1.47 time at higher risk of not receiving postnatal check-up than those outside the window. Whereas the secondary clusters were honored in the Western parts of the country(Gambela and Benishangul) at 7.417914 N; and 35.317365 E geospatial locations, with relative risk and LLR of 1.29 and 31.2, respectively (Table 3).
Spatial scan statistical analysis of hotspot areas of newborns not receiving postnatal check-ups in Ethiopia, produced using Arc GIS version 10.8 (Fig. 6).
Interpolation of a newborn not receiving a postnatal check-up within the first 2 days
Ordinary Kriging interpolation was used to predict the prevalence ofnot receiving postnatal check-ups within the first 2 days among newborns in unobserved areas. The high predicted prevalence of not receiving postnatal check-ups was observed in the Eastern, Southeastern, and Southern parts of Ethiopia. Whereas low prediction of not receiving postnatal check-upsamong newborns was observed in the Southern, Western, and Northern parts of Ethiopia, specifically in Amhara, Tigray, and Addis Ababa regions (Fig. 7).
Factors associated with newborns not receiving postnatal check-ups inEthiopia
The multilevel binary logistic regression model was the best-fitted model for our data; after LR and ICC, tests were checked. Thus, the two-level logistic regression model was fitted to obtain an unbiased result and to come up with a valid inference. Deviance was used to check the model’s fitness and a model with the lowest deviance value is the best fit model. Hence,the final model was the best-fitted model in our data, which gives the lowest deviance value. The ICC value was 0.13 (95% CI: 0.11–0.16) in the null model, which indicates that about13% of the overall variability of the newborns not receiving postnatal check-ups was presented between cluster variability, and the deviance of the null model was (−2 × − 1571922) = 3, 142.78. An ICC value of the individual model was 0.3442 = 34.42,95% CI: (0.17–0.71), which indicates that about 34.42% of the overall variability of the newborn, not reciving postnatal check-up was presented between cluster variability and the deviance of the individual model II was (−2 × − 1136.6712) = 2, 273.34, the ICC value of community level model III was 0.4582245 = 45.82, 95% CI: (0.27–0.79%) random effect whereas the deviance was (rand1448.7476) = 2, 8 97.50 and the multilevel model IV ICC value was 0.0902263 = 9.02, 95% CI:(0.01–0.76), and its deviance was (, an1101.4277) = 2, 202.86.
In this study a two level binary logistic regression model was fitted to determine the factors associated with newborns not receiving postnatal check-up. Among the individual level factors (model II); ANC visit AOR = 0.37,95%CI:(0.24–0.58), place of delivery AOR = 0.02, 95%CI: (0.01–0.03), and health insurance AOR = 0.49,95%CI:(0.30–0.80) were significantly associated with newborns not receiving postnatal check-ups; wheras, in the model III (community level factors) regions such as Afar AOR = 0.16, 95%CI:(0.08–0.34), Oromia AOR = 0.27,95%CI:(0.15–0.48), Somali AOR = 0.25, 95%CI:(0.14–0.46), Benishangul AOR = 0.37, 95%CI:(0.22–0.69), SNNPR AOR = 0.32,95%CI:(0.18–0.57), Gambela AOR = 0.24,95%CI:(0.13–0.47), Harari AOR = 0.40,95%CI:(0.22–0.72), and Dire Dawa AOR = 0.32,95%CI:(0.17–0.59), community wealth status AOR = 0.59,95%CI:(0.43–0.81),community illiteracy AOR = 0.62, 95%CI:(0.46–0.83), and media exposure AOR = 0.79,95%CI:(0.62–0.99) were significantly associated with not receiving postnatal check-up among newborns. However, in the final model (model IV) ANC visit AOR = 0.42, 95%CI: (0.27–0.66), place of delivery AOR = 0.02, 95%CI: (0.01–0.92), residence AOR = 1.90, 95% CI: (1.29–2.81) and regions such as Afar AOR = 0.34, 95%CI:(0.16–0.69), Oromia AOR = 0.53,95%CI:(0.30–0.91), Somali AOR = 0.40, 95%CI:(0.22–0.74), Benishangul AOR = 0.50, 95%CI:(0.27–0.92), SNNPR AOR = 0.33,95%CI:(0.19–0.57), Gambela AOR = 0.30, 95%CI:(0.16–0.56), Harari AOR = 0.44, 95%CI:(0.25–0.78), and Dire Dawa AOR = 0.30, 95%CI:(0.17–0.54) remains statsically significant.
In our study, the odds of not receiving postnatal check-ups within 2 days after birth was increased by 58% among mothers who have not attended ANC visits as compared to their counterparts. The odds of not receiving postnatal check-ups among mothers who delivered at home and others were increased by 80 and 25% higher than mothers who had delivered at the hospital (AOR = .0.02(0.01–0.0.29)) and (AOR = 0.76(0.59–0.99)), respectively. The majority of Ethiopian communities who have lived in different regions were significantly associated with new- borns not receiving postnatal check-ups. The odds of new borns not receiving postnatal check-up among mothers in Afar 66% (AOR = 0.34(0.16–0.69)), Oromia 47%(AOR = 0.53(0.30–0.91), Somali 60%(AOR = 0.40(0.22–0.74)),Benishangul 50%(AOR = 0.50(0.27–0.92), SNNPR 67%(AOR = 0.33(0.19–0.57)), Gambela 70% (AOR = 0.30(0.16–0.56), Harari 56% (AOR = 0.44(0.25–0.78)), and Dire Dawa 70% (AOR = 0.30(0.17–0.54) were higher than mothers in Addis Ababa, respectively. The odds of new born not receiving postnatal checks among mothers who had lived in rural were 1.90 times higher than in urban mothers (AOR = 1.90(1.29–2.81)) (Table 4).
Discussion
Neonatal death is unexpectedly increased in Ethiopia in recent years, the postnatal check-up within 2 days after birth is essential to improve the survival of both the mothers and the newborns. Lack of proper care within the first 2 days leads to complications for the newborn as well as the mother. Hence, this study aimed to investigate the spatial variations and determinants of not receiving a postnatal check-up within 2 days among live births in Ethiopia [1, 22].
The overall national prevalence of newborns not receiving postnatal check-ups within 2 days after birth in Ethiopia was 84.29, 95% CI: (83.11–85.41), which is in line with the study conducted in Ethiopia 83% [23]. However, the finding of our study was slightly lower than those of the study conducted in rural Bangladesh at 90%, and in Ethiopia at 90% [5, 24]. This could be because the study conducted in Bangladesh was conducted in the rural population, which might inhibit the utilization of postnatal check-ups. The study period might be the other reason for the variations in the result. The higher non-utilization of postnatal check-ups in the previous Ethiopian study might be linked to the study period, in recent years efforts have been made to increase the maternal health service utilization through training and recruiting community health extension workers.
On the other hand, the finding of this study was higher than the study conducted in the United Kindom 44.8%, in the Southern Ethiopia 61.6% [25],Ezha district, Ethiopia 76.1% [26], Addis Abeba, Ethiopia 63% [27],and a study conducted in low and middle-income countries such as Malawi 74%, Senegal 21%, Mali 74.82% [28], and Nepal 66% [29,30,31]. The discrepancy of our study with the United Kingdom could be explained by the fact that, healthcare access, infrastructure, and awareness of the population towards the utilization of postnatal check-ups in the united kingdom [32]. The difference in studies conducted in Ethiopia might be explained by the study period and most studies conducted in Ethiopia were conducted in urban, which increases the utilization of postnatal check-ups. Furthermore, the discrepancy in the study conducted in low and middle-income countries might be explained by the low healthcare access in Ethiopia. The difference for the Nepal study might be due to the differences in socio-cultural practice, sample size and geographical differences. For instance, in the African study data were collected using house to house survey, mothers may have good health care awareness, whereas our study was conducted using a nationally representative data and 88% of the population have been lived in the rural area have little awareness of postnatal care service after birth for mothers and newborn. In Ethiopia, child birth at home is also very high, which might contribute to the low utilization of postnatal check-ups [33].
Consistent with the previous studies conducted in Ethiopia [34, 35], significant autocorrelation of not receiving postnatal check-ups were detected among newborns. Spatial clustering of early postnatal non-utilization was observed in Eastern, Northeastern, Southern, southeastern, and western parts of the country, which was supported by studies conducted in Ethiopia [35,36,37]. This could be linked with health care access, education, and population awareness in these areas.
According to the multilevel regression analysis results, the odds of not receiving postnatal check-ups among mothers who had no ANC visits were 58% higher than mothers who had four and above ANC visits, which is supported by studies done in Ethiopia [5, 38, 39], Tanzania [40], Uganda [41], and Kenya [41, 42]. The possible reasons might be mothers who have four and above ANC visits might get counseling regarding birth preparedness, skilled delivery, and early postnatal care, which might increase the postnatal check-up utilizations.
The odds of not receiving postnatal check-ups within 2 days after birth were higher among neonates delivered at home and others by 80 and 25% respectively as compared to mothers who gave birth at hospitals. Similar reports had been released in the previous studies conducted in Ethiopia [27, 43], Tanzania [40], and Uganda [41]. The possible reason might be mothers who gave birth in hospital might have a possibility of staying for 2 days or be counseled to have a follow-up 2 days after birth stayed and can get appropriate health care follow-up for the newborns and mothers. Whereas, mothers who gave birth at home; are culturally restricted to move out of their homes for a certain period, which reduces the postnatal care utilization.
Similar to the previous study conducted in Ethiopia [38, 44], Uganda [41], and Kenya [42], the odds of not receiving a postnatal check-up among rural mothers were 1.9 times higher as compared to their counterparts. The possible reasons might be due to the difficulty of getting healthcare access and infrastructure in rural. Education, health information, and antenatal follow-up were lower in rural, which contributes to the low utilization of postnatal check-ups.
In agreement with the previous studies conducted in Ethiopia [33,34,35,36], West African countries [45], and Pakistan [46],the odds of a newborn not receiving a postnatal check-up within 2 days after birth were higher by 66% in Afar, 47% in Oromia, 60% in Somali, 50% in Benishangul, 67% in SNNPR, 70% in Gambela, 56% in Harari and 70% in Dire Dawa as compared with Addis Abeba. The possible explanation for the low utilization of postnatal check-ups within 2 days after birth in regions other than Addis Ababa might be related to population awareness of the importance of postnatal check-ups. Moreover, socio-cultural practice, socio-economicvariation, access to healthcare facilities, availability of skilled healthcare providers for postnatal care counseling, and access to transport, that might influence the utilization of postnatal check-ups.
This study has paramount importance in reducing neonatal mortality, especially in the first 2 days by improving the postanal check-ups. High-risk areas for not receiving postnatal check-ups could be very important to design effective local, geographically targeted interventions to increase the postnatal check-ups utilizations.
Strengeth and limitations
The strength of our study is using large sample size and a country representative data. The other strength of this study is using advanced statistical models (geo-spacial and multilevel analysis), which account the cluster variabilities. However, our study has some limitations, first, since we used secondary data analysis, we fail to incorporate some clinical variables, which might effect on the outcome variable. The second limitation of this study was we coundn’t include the paternalinformations, which might infulunce our result.
Conclusion
Low postnatal check-up utilization remains a big challenge in Ethiopia, with significant spatial variationsacross regional and local levels. Spatial clustering of not receivingpostanal check-ups within 2 days was observed in Afar, Oromia, Gambela, Benishangul, SNNPR, Harari, and Dire Dawa regions. Residence, ANC visits, place of delivery, and administrative regions were significantly associated with not receiving postnatal check-ups. Geographically targeted interventions to improve ANC follow-up and institutional delivery should be strengthened.
Availability of data and materials
The corresponding author will give the data for formal requesters.
Abbreviations
- ANC:
-
Antenatal Care
- ANC:
-
Antenatal Care Visits
- CRS:
-
Coordinate Reference System
- DHS:
-
Demographic and Health Survey
- EAs:
-
Enumeration Areas
- EDHS :
-
Ethiopia Demographic and Health Survey
- GIS:
-
Geographic Information Systems
- ICC:
-
Intra-class Correlation Coefficient
- SNNPR:
-
Southern Nations, Nationalities and Peoples Region
- WHO:
-
World Health Organization
References
Organization WH. WHO recommendations on postnatal care of the mother and newborn: World Health Organization; 2014.
Bwalya BB, Mulenga MC, Mulenga JN. Factors associated with postnatal care for newborns in Zambia: analysis of the 2013-14 Zambia demographic and health survey. BMC Pregnancy Childbirth. 2017;17(1):1–13.
Organization WH. HRP annual report 2019; 2020.
Organization WH. Counseling for maternal and newborn health care: A handbook for building skills: World Health Organization; 2013.
Seid A, Ahmed M. Determinants of postnatal checkup for newborns in Ethiopia: Further analysis of 2016 Ethiopia demographic and health survey. BMC Pregnancy Childbirth. 2020;20(1):1–7.
Kmietowicz Z. Postnatal care: WHO highlights the urgency of physical and mental support: British Medical Journal Publishing Group; 2022.
Organization WH. WHO recommendations on maternal and newborn care for a positive postnatal experience: executive summary; 2022.
WHO. Newborn death and illness www.who.int › pmnch › media › press_materials › fs_newborn death illness. 2020.
Sakeah E, Aborigo R, Sakeah JK, Dalaba M, Kanyomse E, Azongo D, et al. The role of community-based health services in influencing postnatal care visits in the Builsa and the West Mamprusi districts in rural Ghana. BMC Pregnancy Childbirth. 2018;18(1):1–9.
Mengesha HG, Sahle BW. Cause of neonatal deaths in Northern Ethiopia: a prospective cohort study. BMC Public Health. 2017;17(1):1–8.
Soubeiga D, Gauvin L, Hatem MA, Johri M. Birth Preparedness and Complication Readiness (BPCR) interventions to reduce maternal and neonatal mortality in developing countries: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2014;14(1):1–11.
Central Statistics Agency E. Ethiopia Mini Demographic and Health Survey 2019, Ethiopian Public Health Institute Addis Ababa Federal Ministry of Health Addis Ababa. Rockville: The DHS Program ICF; 2021.
Black RE, Levin C, Walker N, Chou D, Liu L, Temmerman M, et al. Reproductive, maternal, newborn, and child health: key messages from disease control priorities 3rd edition. Lancet. 2016;388(10061):2811–24.
Child EWE. Partnership for Maternal Newborn & Child Health. Progress in Partnership. 2017.
Bhutta ZA, Black RE. Global maternal, newborn, and child health—so near and yet so far. N Engl J Med. 2013;369(23):2226–35.
Lozano R, Fullman N, Abate D, Abay SM, Abbafati C, Abbasi N, et al. Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):2091–138.
Warren C, Daly P, Toure L, Mongi P. Postnatal care. Opportunities for Africa’s newborns. Cape Town: Partnership for maternal, newborn and child health; 2006. p. 79–90.
Berhe A, Bayray A, Berhe Y, Teklu A, Desta A, Araya T, et al. Determinants of postnatal care utilization in Tigray, Northern Ethiopia: A community based cross-sectional study. PLoS One. 2019;14(8):e0221161.
Marcus HG, Mehretu A, Crummey DE. "Ethiopia". Encyclopedia Britannica. 2021. https://www.britannica.com/place/Ethiopia. Accessed 9 Dec 2021.
care Ehpoh. Ethiopian health policy of health care. Three-tier Ethiopian health care system (Source: Ethiopian health sector development plan 2010–2015).
Demographic E. Health Survey 2016 (EDHS). Central Statistical Agency, The DHS Program ICF. 2017.
Macdonald C, Sharma S, Kallioinen M, Jewell D. Postnatal care: new NICE guideline for the ‘Cinderella service’. Br J Gen Pract. 2021;71 (710): 394–5. https://doi.org/10.3399/bjgp21X716825.
Tadele A, Getinet M. Determinants of Postnatal Care Check-ups in Ethiopia: A Multi-Level Analysis. Ethiop J Health Sci. 2021;31(4):1029–857.
UNICEF. Maternal and Newborn Health Disparities Ethiopia; 2017. Available from: Maternal and Newborn Health Disparities in Ethiopia. https://data.Unicef.org/resources/maternal-newborn-health-disparities-country-profiles
Mersha A, Assefa N, Teji K, Shibiru S, Darghawth R, Bante A. Essential newborn care practice and its predictors among mother who delivered within the past six months in Chencha District, Southern Ethiopia, 2017. PLoS One. 2018;13(12):e0208984.
Habte A, Gebiremeskel F, Shewangizaw M, Dessu S, Glagn M. Uptake of complete postnatal care services and its determinants among rural women in Southern Ethiopia: Community-based cross-sectional study based on the current WHO recommendation. PLoS One. 2021;16(2):e0246243.
Tiruneh GT, Worku A, Berhane Y, Betemariam W, Demissie M. Determinants of postnatal care utilization in Ethiopia: a multilevel analysis. BMC Pregnancy Childbirth. 2020;20(1):1–12.
Peven K, Day LT, Bick D, Purssell E, Taylor C, Akuze J, et al. Household Survey Measurement of Newborn Postnatal Care: Coverage, Quality Gaps, and Internal Inconsistencies in Responses. Glob Health: Sci Pract. 2021;9(4):737–51.
Dhakal S, Chapman GN, Simkhada PP, Van Teijlingen ER, Stephens J, Raja AE. Utilization of postnatal care among rural women in Nepal. BMC Pregnancy Childbirth. 2007;7(1):1–9.
Keya KT, Rahman MM, Rob U, Bellows B. Distance traveled and cost of transport for use of facility-based maternity services in rural Bangladesh: a cross-sectional survey. Lancet. 2013;382:17.
Smith HC, Saxena S, Petersen I. Postnatal checks and primary care consultations in the year following childbirth: an observational cohort study of 309 573 women in the UK, 2006–2016. BMJ Open. 2020;10(11):e036835.
Walker SB, Rossi DM, Sander TM. Women's successful transition to motherhood during the early postnatal period: A qualitative systematic review of postnatal and midwifery home care literature. Midwifery. 2019;79:102552.
Tessema ZT, Tiruneh SA. Spatio-temporal distribution and associated factors of home delivery in Ethiopia. Further multilevel and spatial analysis of Ethiopian demographic and health surveys 2005–2016. BMC Pregnancy Childbirth. 2020;20(1):1–16.
Sisay MM, Geremew TT, Demlie YW, Alem AT, Beyene DK, Melak MF, et al. Spatial patterns and determinants of postnatal care use in Ethiopia: findings from the 2016 demographic and health survey. BMJ Open. 2019;9(6):e025066.
Melaku MS, Aemro A, Aychiluhm SB, Muche A, Bizuneh GK, Kebede SD. Geographical variation and predictors of zero utilization for a standard maternal continuum of care among women in Ethiopia: a spatial and geographically weighted regression analysis. BMC Pregnancy Childbirth. 2022;22(1):1–18.
Alemu K. Spatial Patterns and Determinants of Postnatal Care Use in Ethiopia: A finding from Demographic and Health Survey.
Defar A, Okwaraji YB, Tigabu Z, Persson LÅ, Alemu K. Geographic differences in maternal and child health care utilization in four Ethiopian regions; a cross-sectional study. Int J Equity Health. 2019;18(1):1–11.
Ayele BG, Woldu MA, Gebrehiwot HW, Gebre-Egziabher EG, Gebretnsae H, Hadgu T, et al. Magnitude and determinants for the place of postnatal care utilization among mothers who delivered at home in Ethiopia: a multinomial analysis from the 2016 Ethiopian demographic health survey. Reprod Health. 2019;16(1):1–10.
Abraha TH, Gebrezgiabher BB, Aregawi BG, Belay DS, Tikue LT, Reda EB. Factors associated with compliance with the recommended frequency of postnatal care services in four rural districts of Tigray region, north Ethiopia. Kor J Fam Med. 2019;40(5):329.
Kanté AM, Chung CE, Larsen AM, Exavery A, Tani K, Phillips JF. Factors associated with compliance with the recommended frequency of postnatal care services in three rural districts of Tanzania. BMC Pregnancy Childbirth. 2015;15(1):341.
Ndugga P, Namiyonga NK, Sebuwufu D. Determinants of early postnatal care attendance: analysis of the 2016 Uganda demographic and health survey. BMC Pregnancy Childbirth. 2020;20(1):163.
Akunga D, Menya D, Kabue M. Determinants of postnatal care use in Kenya. Afr Popul Stud. 2014;28(3):1447–59.
Chaka EE, Abdurahman AA, Nedjat S, Majdzadeh R. Utilization and determinants of postnatal care services in Ethiopia: a systematic review and meta-analysis. Ethiop J Health Sci. 2019;29(1):1029–857.
Tesema GA, Mekonnen TH, Teshale AB. Individual and community-level determinants, and spatial distribution of institutional delivery in Ethiopia, 2016: Spatial and multilevel analysis. PLoS One. 2020;15(11):e0242242.
Solanke BL, Amoo EO, Idowu AE. Improving postnatal checkups for mothers in West Africa: A multilevel analysis. Women Health. 2018;58(2):221–45.
Saira A, Wilson LA, Ezeh KO, Lim D, Osuagwu UL, Agho KE. Factors associated with non-utilization of postnatal care among newborns in the first 2 days after birth in Pakistan: a nationwide cross-sectional study. Glob Health Action. 2021;14(1):1973714.
Acknowledgments
We thank the University of Gondar College of Medicine and Health Sciences for offering free access to the digital online library for searching the electronic databases. We also thank the MEASURE DHS Programfor accessing the data.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
DGK& KAA conceptualized, designed, analyzed, developed, and drafted the manuscript. NTA and TTT participated in the design and analysis. All authors critically reviewed the manuscript for important intellectual content and contributed to the final approval of the version to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We registered and granted a letter from the online database of DHS program and the Ethiopian Public Health Institute through: https://dhsprogram.com/methodology/survey/survey-display-478.cfm.to access the data and all methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kassie, D.G., Assimamaw, N.T., Tamir, T.T. et al. Spatial distribution and determinants of newbornsnot receiving postnatal check-up withintwodays after birth in Ethiopia: a spatial and multilevel analysis of EDHS 2016. BMC Pediatr 22, 495 (2022). https://doi.org/10.1186/s12887-022-03506-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03506-9