Abstract
Background
Kawasaki disease (KD) is a self-limiting vasculitis with an unknown etiology. It has been reported that breastfeeding has a potential protective effect on KD development. However, whether breastfeeding has an effect on the development of coronary artery lesions (CALs) remains unclear.
Methods
We retrospectively reviewed the medical records of patients with the main diagnosis of KD hospitalized in our hospital from May 2017 to November 2018. Standardized telephone interviews were carried out to obtain feeding practices before KD was onset.
Results
Two hundred and ninety-three (51.6%) were exclusively breastfed, 223 (39.3%) were partially breastfed and 52 (9.2%) were formula fed. There were no significant differences in the characteristics regarding age, gender, incomplete KD, intravenous immunoglobulin (IVIG) resistance, and the laboratory variables among the three groups. With formula feeding as a reference, patients exclusively breastfed and partially breastfed seemed to have a higher incidence of CALs, even after adjusting confounders, but were not statistically significant. After grouping patients who were older than six months into formula feeding, partial breastfeeding for < 2 months, partial breastfeeding for ≥ 2 and < 4 months, partial breastfeeding for ≥ 4 and < 6 months and exclusively breastfeeding based on the length of breastfeeding, the results remained the same (P > 0.05).
Conclusions
Breastfeeding has no protective effect on the development of CALs in KD.
Similar content being viewed by others
Introduction
Kawasaki disease (KD) is a self-limiting vasculitis, that predominantly occurs in children under five years old. It is the main contributor to acquired heart diseases in developed countries due to its cardiac complications [1]. However, its specific causes remain to be elucidated despite years of research. Existing researches have hypothesized that KD is a consequence of an abnormal immunological response triggered by undefined infectious agents in genetically susceptible individuals [2, 3].
Breastmilk contains abundant active immune factors, which help to establish the mature immune system of infants. There is a great interest in the association between breastfeeding and immune diseases [4,5,6]. KD is one of the most commonly seen immune vasculitis in children, and whether its disease onset was associated with feeding practices made us confused. In 2016, Japanese researchers conducted a nationwide survey that proved the protective effect of breastfeeding in the development of KD for the first time [7]. However, whether breastfeeding has an effect on the development of coronary artery lesions (CALs) remains unclear. There were few studies carried out [8, 9]. In the present study, we tried to investigate the effects of feeding practices, as well as the length of breastfeeding on the development of CALs.
Methods
Study participants
We retrospectively reviewed the medical records of patients with the main diagnosis of KD hospitalized in Children’s Hospital of Soochow University from May 2017 to November 2018. The institutional review board of Children’s Hospital of Soochow University approved this study (No: 2017LW008) and waived the requirement for informed consent because of the retrospective nature of the study.
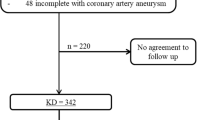
A total of 597 patients were initially diagnosed with KD and treated in our hospital during this study period. Thirteen patients were excluded, including one patient who showed a second episode of KD, one who did not receive initial intravenous immunoglobulin (IVIG) treatment due to defervescence before IVIG, 10 who received initial IVIG treatment in other hospitals prior to admission, and two who were auto-discharged with missing echocardiographic reports. Besides, 16 patients couldn’t be reached by telephone or caregivers couldn’t recall the feeding practices. As a result, 568 patients were enrolled in the study (Fig. 1).
Definition
KD was diagnosed when a patient was febrile for ≥ five days, together with more than four of the following five characteristics: 1. Rash, 2. Bilateral conjunctive injection, 3. Cervical lymphadenopathy, 4. Changes of the extremities, 5. Oral mucosal changes [1]. Incomplete KD (iKD) was diagnosed in a patient who had two or three compatible clinical characteristics when the other possible causes of fever were excluded. A total of 2 g/kg IVIG in a single dose together with 30–50 mg/kg aspirin was administered as soon as possible after diagnosis in the febrile patients. For patients who were afebrile for 3–4 days, aspirin was then reduced to 3–5 mg/kg/day until the patients showed no evidence of CALs by 6 to 8 weeks after the onset of illness. Delayed IVIG treatment was defined as IVIG initiation after the 10th day of illness. We calculated the z score of the left main coronary artery, left circumflex artery, left descending artery, and right coronary artery based on the method reported [10]. CALs were defined when the z score of any coronary artery ≥ 2.5; and/or the clearly irregular appearance of the intima. IVIG resistance was defined as persistent or recurrent fever > 38.0℃ lasting for more than 36 h [1]. A second dose of 2 g/kg IVIG was administered to these patients. Additional intravenous methylprednisolone of 2–4 mg/kg/day was also administered, which was switched to oral dose after defervescence and was tapered over 2 weeks. Exclusive breastfeeding was defined as totally breastfed while formula feeding was fed with formula milk when patients were under six months. Partial breastfeeding was intermediate. If a patient was now aged under six months and was breastfed since born, he was also defined as exclusive breastfeeding. Patients older than six months were included in further analysis to investigate the relationships between breastfeeding duration and the outcomes. Patients were grouped into five groups according to the length of breastfeeding, they were never breastfed (formula feeding), breastfed for < 2 months, breastfed for ≥ 2 and < 4 months, breastfed for ≥ 4 and < 6 months, and ≥ 6 months.
Data collection
Standardized telephone interviews were carried out with guardians or caregivers of each patient to obtain feeding practices before KD was onset, as well as the length of breastfeeding. The laboratory variables and birth factors regarding parity, singleton or multiple births, preterm were reviewed from the medical records. All blood samples were obtained within the first 24 h on admission and after defervescence for more than 72 h, or as appropriate. An echocardiogram was carried out before the initial IVIG and was repeated before discharge. In patients with severe abnormity, it was repeated as appropriate. We chose the largest coronary internal lumen dimension for further analysis. The details of missing data are summarized in Additional file 1. More than 20% of the missing data were removed from our analysis, and the remaining missing data were obtained with the multiple imputation method.
Statistical analyses
Statistical analyses were conducted using R for Windows (Version 4.0.4). Data were expressed as mean ± standard deviation (SD), median with quartiles, or number with percentage as appropriate. Descriptive statistics were performed on demographic characteristics. Parametric or nonparametric comparative tests for continuous data and χ2 test or Fisher exact test for categorical data were used to compare variables between groups. One-way ANOVA test or Kruskal–Wallis H test was used to compare continuous data among the three groups as appropriate. Bonferroni test was used to compare every two groups among the three groups based on the variance. Log-rank test for univariate analysis was performed to explore the risk factors for CALs on admission. The covariates, when added to the Cox regression model, changed the matched hazard ratio (HR) by at least 10% and were selected for adjustments. The variance inflation factor (VIF) method was used to examine multicollinearity of the covariances, and VIF ≥ 5 suggested multicollinearity. Feeding practices were chosen as categorical variables. In order to clearly describe the effect of breastfeeding on the outcomes. Three different models were established. Model 1 was a crude model. Model 2 adjusted for sex, delayed IVIG treatment, iKD, and IVIG resistance. Model 3 adjusted for confounders in model 2, plus singleton, prematurity, white blood cells (WBC), hematocrit, platelet, and alanine aminotransferase (ALT). We included IVIG resistance, sex, and delayed IVIG treatment into the Cox regression models because they were widely considered as the risk factors for CALs. Subgroup analyses regarding ages (< 1 yr, ≥ 1 and < 3 yrs, and ≥ 3 yrs) were carried out to analyze the associations between feeding practices and CALs. We included patients with complete medical data and did the statistics as a sensitivity analysis. Two-tailed P < 0.05 was considered statistically significant.
Results
There were 355 males and 213 females included in the study. iKD accounted for 121 (21.3%) of all patients. Among them, 26 (4.6%) patients were defined as IVIG resistance and 149 (26.2%) patients were considered to have CALs. Patients with missing feeding practice information tended to be older (median age: 18.0 vs 41.0 months, P < 0.001).
Two hundred and twenty-three (39.3%) patients were partially breastfed, 293 (51.6%) were exclusively breastfed while 52 (9.2%) were formula-fed. There was a significant difference in C-reactive protein (CRP) among the three groups (P < 0.05), although after post hoc test no significance was found between any two groups (formula breastfeeding vs. partial breastfeeding, P > 0.9, formula breastfeeding vs. exclusive breastfeeding, P = 0.19, partial breastfeeding vs. exclusive breastfeeding, P = 0.08). No significant differences were found in any other characteristics (Table 1).
The univariate analysis results by Log-rank test are shown in Table 2. Patients with CALs tended to be infants, and have higher levels of WBC, and platelet count, and have lower levels of hemoglobin, hematocrit, and albumin (P < 0.05). Besides, they tended to be iKD and have a lower level of ALT, although the differences were not statistically significant.
Singleton, prematurity, WBC, hematocrit, platelet, iKD, and ALT were selected as the confounders. Three Cox regression models were then established. With formula feeding as a reference, patients who were exclusively breastfed and partially breastfed seemed to have higher incidences of CALs. However, the differences were not significant in all of the three models (Table 3). P for trend in these models were insignificant.
Subgroup analysis was carried out and even after adjusting all covariates (model 3), no significant difference was found in all three age groups (see Additional file 2).
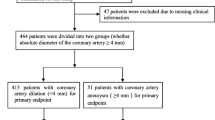
We further tried to seek the effects of the length of breastfeeding on CALs. A total of 508 (89.4%) patients were older than six months and were enrolled in the analysis. Forty-nine patients (9.6%) were formula fed, 26 (5.1%) were breastfed for < 2 months, 56 (11.0%) were breastfed for ≥ 2 and < 4 months, 119 (23.4%) were breastfed for ≥ 4 and < 6 months, 258 (50.8%) were exclusively breastfed for the first 6 months in their lives. Incidence of CALs showed no significant differences among these groups, even after adjusting the potential confounders (P > 0.05, see Table 4). Also, P for trend in these models were not significant.
We included 397 and 359 patients with complete medical data respectively, to carry out the sensitivity analyses, and found the same results (see Additional file 3).
Discussion
In the present study, we did a retrospective study and tried to investigate the effects of feeding practices and breastfeeding duration on CALs. We found that breastfeeding had no protective effects on the occurrences of CALs in all age groups. Besides, breastfeeding duration was neither associated with CALs.
Breastmilk contains many active immune factors such as secretory immunoglobulin A, oligosaccharides, lactoferrin, nucleotides that have potential protective effects on infectious diseases [11], obesity [12], autoimmune diseases [4, 5], allergic diseases [4], et al. Actually, breastfeeding could potentially reduce hospital admissions for any cause excluding injuries [7]. Thus, breastfeeding has become the preferred method for infant nutrition intake and 90.8% of patients had ever been breastfed in the present study.
There was a significant difference in CRP level, although no difference was found after post hoc tests, seemingly reflecting a protective role of breastfeeding in the disease inflammation. CRP elevation was frequently seen in both infection and inflammation. It was recognized as an important biomarker in the diagnosis of suspected iKD [1] and moreover, was considered as a risk factor for CALs and IVIG resistance in previous studies [13,14,15,16]. Besides, no other differences were found regarding ages of disease onset, the subtypes of KD (iKD or complete KD), responses to initial IVIG treatment, or other inflammatory parameters among the three groups.
It seemed that exclusive breastfeeding and partial breastfeeding had no benefit for CALs. Our results were in consistent with a case–control study which was conducted in Central China [9]. Given that breastfeeding practices had no protective effects on CALs, we further explored if the length of breastfeeding played a role. Unfortunately, the results remained the same. In a previous study from Germany, the authors found no difference in CALs with respect to the duration of breastfeeding when they divided breastfeeding duration into longer and shorter than two weeks [8]. However, in a recent study carried out in Taiwan, the authors found that patients who were breastfed for longer than six months had lower occurrences of persisting CALs than those who were breastfed for shorter than six months in univariable analysis. After adjusting the confounders, the difference turned insignificant [17]. Despite infants are better to be exclusively breastfed until 6 months old, and be breastfed until two years old as recommended [18], there are no potential benefits of breastfeeding practice and prolonged breastfeeding regarding the occurrences of CALs in KD in a series of studies. Thus, we could speculate that although exclusive breastfeeding, especially colostrum had a potential role in the prevention of KD onset [7,8,9], inflammation in patients with CALs was so severe that the protective effects of breastmilk on KD development were partly counteracted. The potential roles of other risk factors for CALs should be explored.
CALs are good indicators of KD severity because they are the main complications of the disease. A higher incidence of CALs was noted in our study than those in Japan and Korea’s national study [19,20,21]. We largely attributed the divergence to the definition of CALs. The definition of CALs in the two studies [19, 20] was based on the Japanese criteria. In Kim SH’s study [21], the authors reported 24.2% (1666/6889) CALs based on Dallaire’s method, which was also slightly lower than that in our study. It might partly be because we defined patients with clearly irregular appearance of the intima as CALs regardless z scores of the coronary arteries, whereas the luminal irregularity was absent in their study. The cascaded inflammation by immune cells is activated during the acute stage, consequently causing coronary arterial endothelial dysfunction and finally leading to CALs. Although the specific mechanisms are not fully understood, it is generally considered that T cells play important roles in the disease process [22, 23]. Breastmilk is well characterized to be helpful to establish infants’ mature immune systems including T cells [24, 25]. Apart from the reason mentioned above, the reason why breastfeeding has no protective effect likely lies in these aspects, such as genetic backgrounds, meteorological factors, et.al.
It should be noted that a small proportion of patients were IVIG resistant in our study. Previously, we have observed that IVIG resistance rate was only 4.7% during 2006 and 2014 in this area [26]. It was reported that patients who received earlier IVIG treatment than the 4th day were easier to be IVIG resistant [15]. Although IVIG was administered immediately after the diagnosis of KD since 2017 in our hospital as recommended by the latest guidelines [1], there was no significant increase in IVIG non-responders overall.
The present study had some limitations. First, telephone interviews were carried out to obtain the feeding practices of patients, which might cause bias because it was retrospective. Second, we only included KD patients hospitalized in an 18-month period, because the height of patients before May 2017 was not documented. We calculated the z score of each coronary artery rather than the Japanese criteria to better avoid underestimation of CALs in younger patients, especially in infants. However, in the lack of Chinese-originated z score, we used z score equations based on the normal values in the Canadian which might also cause bias. Third, it was reported that maternal factors were also associated with the outcomes of KD [27]. Unfortunately, we were unable to obtain these because they were not routinely recorded on the medical records.
Conclusion
Although it is reported that breastfeeding lowers the incidence of KD, our results indicate that breastfeeding practice and longer breastfeeding duration couldn’t reduce CALs in those patients who have already developed KD.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALT:
-
Alanine aminotransferase
- CALs:
-
Coronary artery lesions
- CRP:
-
C-reactive protein
- HR:
-
Hazard ratio
- IVIG:
-
Intravenous immunoglobulin
- KD:
-
Kawasaki disease
- SD:
-
Standard deviation
- VIF:
-
Variance inflation factor
- WBC:
-
White blood cells
References
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of kawasaki disease: a scientific statement for health professionals from the american heart association. Circulation. 2017;135(17):e927–99.
Galeotti C, Bayry J, Kone-Paut I, Kaveri SV. Kawasaki disease: aetiopathogenesis and therapeutic utility of intravenous immunoglobulin. Autoimmun Rev. 2010;9(6):441–8.
Lo MS. A framework for understanding Kawasaki disease pathogenesis. Clin Immunol. 2020;214: 108385.
Hyrich KL, Baildam E, Pickford H, Chieng A, Davidson JE, Foster H, et al. Influence of past breast feeding on pattern and severity of presentation of juvenile idiopathic arthritis. Arch Dis Child. 2016;101(4):348–51.
Conradi S, Malzahn U, Paul F, Quill S, Harms L, Then Bergh F, et al. Breastfeeding is associated with lower risk for multiple sclerosis. Mult Scler. 2013;19(5):553–8.
Vieira Borba V, Sharif K, Shoenfeld Y. Breastfeeding and autoimmunity: Programing health from the beginning. Am J Reprod Immunol. 2018;79(1):e12778.
Yorifuji T, Tsukahara H, Doi H. Breastfeeding and Risk of Kawasaki Disease: A Nationwide Longitudinal Survey in Japan. Pediatrics. 2016;137(6):e20153919.
Meyer K, Volkmann A, Hufnagel M, Schachinger E, Klau S, Horstmann J, et al. Breastfeeding and vitamin D supplementation reduce the risk of Kawasaki disease in a German population-based case-control study. BMC Pediatr. 2019;19(1):66.
Wang S, Xiang D, Fang C, Yao B. Association between breastfeeding and Kawasaki disease: a case-control study. Eur J Pediatr. 2020;179(3):447–53.
Dallaire F, Dahdah N. New equations and a critical appraisal of coronary artery Z scores in healthy children. J Am Soc Echocardiogr. 2011;24:60–74.
Sankar MJ, Sinha B, Chowdhury R, Bhandari N, Taneja S, Martines J, et al. Optimal breastfeeding practices and infant and child mortality: a systematic review and meta-analysis. Acta Paediatr. 2015;104(467):3–13.
Yan J, Liu L, Zhu Y, Huang G. Wang PP The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health. 2014;14:1267.
Lodge CJ, Tan DJ, Lau MX, Dai X, Tham R, Lowe AJ, et al. Breastfeeding and asthma and allergies: a systematic review and meta-analysis. Acta Paediatr. 2015;104(467):38–53.
Sano T, Kurotobi S, Matsuzaki K, Yamamoto T, Maki I, Miki K, et al. Prediction of non-responsiveness to standard high-dose gamma-globulin therapy in patients with acute Kawasaki disease before starting initial treatment. Eur J Pediatr. 2007;166(2):131–7.
Egami K, Muta H, Ishii M, Suda K, Sugahara Y, Iemura M, et al. Prediction of resistance to intravenous immunoglobulin treatment in patients with Kawasaki disease. J Pediatr. 2006;149(2):237–40.
Kobayashi T, Inoue Y, Takeuchi K, Okada Y, Tamura K, Tomomasa T, et al. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation. 2006;113(22):2606–12.
Kim MK, Song MS, Kim GB. Factors predicting resistance to intravenous immunoglobulin treatment and coronary artery lesion in patients with kawasaki disease: analysis of the korean nationwide multicenter survey from 2012 to 2014. Korean Circ J. 2018;48(1):71–9.
Guo MM, Tsai IH, Kuo HC. Effect of breastfeeding for 6 months on disease outcomes in patients with Kawasaki disease. PLoS ONE. 2021;16(12): e0261156.
WHO Working Group on the Growth Reference Protocol and the WHO Task Force on Methods for the Natural Regulation of Fertility. Growth of healthy infants and the timing, type, and frequency of complementary foods. Am J Clin Nutr. 2002;76(3):620–7.
Ae R, Makino N, Kosami K, Kuwabara M, Matsubara Y, Nakamura Y. Epidemiology, treatments, and cardiac complications in patients with kawasaki disease: the Nationwide survey in Japan, 2017–2018. J Pediatr. 2020;225(23–9): e2.
Kim GB, Eun LY, Han JW, Kim SH, Yoon KL, Han MY, et al. Epidemiology of kawasaki disease in South Korea: a Nationwide survey 2015–2017. Pediatr Infect Dis J. 2020;39(11):1012–6.
Kim SH, Kim JY, Kim GB, Yu JJ, Choi JW. Diagnosis of Coronary Artery Abnormalities in Patients with Kawasaki Disease According to Established Guidelines and Z Score Formulas J Am Soc Echocardiogr. 2021;34(6):662–72 (e3).
Lee SB, Kim YH, Hyun MC, Kim YH, Kim HS, Lee YH. T-Helper Cytokine Profiles in Patients with Kawasaki Disease. Korean Circ J. 2015;45(6):516–21.
Xie Z, Huang Y, Li X, Lun Y, Li X, He Y, et al. Atlas of circulating immune cells in Kawasaki disease. Int Immunopharmacol. 2022;102: 108396.
Wood H, Acharjee A, Pearce H, Quraishi MN, Powell R, Rossiter A, et al. Breastfeeding promotes early neonatal regulatory T-cell expansion and immune tolerance of non-inherited maternal antigens. Allergy. 2021;76(8):2447–60.
Laouar A. Maternal Leukocytes and Infant Immune Programming during Breastfeeding. Trends Immunol. 2020;41(3):225–39.
Tang Y, Gao X, Shen J, Sun L, Yan W. Epidemiological and clinical characteristics of kawasaki disease and factors associated with coronary artery abnormalities in East China: Nine Years Experience. J Trop Pediatr. 2016;62(2):86–93.
Huang WD, Lin YT, Tsai ZY, Chang LS, Liu SF, Lin YJ, et al. Association between maternal age and outcomes in Kawasaki disease patients. Pediatr Rheumatol Online J. 2019;17(1):46.
Acknowledgements
Special thanks to the physicians reporting Kawasaki disease cases and to the patients enrolled in this study. Additional thanks to Dr. Hao Peng for methodological guidance.
Funding
This work was financially supported by the National Natural Science Foundation of China (grant number 81700439, and 81900450), Gusu health personnel training project (grant number GSWS2019048, 2020054), Suzhou Science and Technology Development Plan Project (grant number SYS2019084 and SS202066), and Jiangsu province key medical young talents (grant number QNRC 2016765).
Author information
Authors and Affiliations
Contributions
YT contributed to conceptualization, data curation, funding acquisition, and writing – review & editing. HW contributed to investigation, methodology and writing original draft. XL, QX, and WQ contributed to investigation, funding acquisition, and methodology. WY contributed to investigation, and project administration. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional review board of Children’s Hospital of Soochow University approved this study (No: 2017LW008). The requirement for informed consent was waived because of the retrospective nature of the study. All methods were performed in accordance with relevant guidelines and regulations and had been performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Missing number (%) for included variables in dataset.
Additional file 2.
Subgroup analysis by ages for the associations between feeding practices and CALs.
Additional file 3.
Cox regression models of feeding practices, breastfeeding duration and CALs among patients with Kawasaki disease.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, H., Tang, Y., Yan, W. et al. Breastfeeding has no protective effects on the development of coronary artery lesions in Kawasaki disease: a retrospective cohort study. BMC Pediatr 22, 353 (2022). https://doi.org/10.1186/s12887-022-03422-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03422-y