Abstract
Background
Anti-α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR) encephalitis is a rare autoimmune synaptic encephalitis associated with autoantibodies that cause a selective decrease in surface expression and changes in receptor localization. Anti-AMPAR encephalitis is poorly recognized, especially in children, and its clinical phenotype is incompletely described.
Case presentation
We report a case of anti-AMPAR GluR1 antibody-mediated autoimmune encephalitis in a 12-year-old male. The patient manifested as a fulminant course, with ataxia, cerebellar degeneration at the onset, and rapidly evolved into hyperthermia, coma and rhabdomyolysis. Antibodies against AMPAR GluR1 receptors were detected in the cerebrospinal fluid by cell-based assay. Diffuse slow waves were found by electroencephalograph, and the left cerebellar vermis and hemisphere were affected on brain magnetic resonance imaging (MRI). The patient was treated with intravenous immunoglobulin (IVIG), methylprednisolone combined with plasma exchange. Symptoms were alleviated after immunotherapy and the patient sustained clinical improvement. This is the first time that acute rhabdomyolysis symptom has been identified in a pediatric patient with anti-AMPAR encephalitis.
Conclusions
This case expands the clinical spectrum of anti-AMPAR encephalitis and highlights that despite poor clinical manifestation at the outset, recovery remains possible.
Similar content being viewed by others
Background
AMPAR is an ionotropic receptor belonging to the family of glutamate receptors that are located on the post-synaptic membrane and play essential roles in synaptic plasticity, memory, and learning [1]. AMPAR has four subunits—GluR1, GluR2, GluR3, and GluR4—and are mainly located in the cerebellum, cerebral cortex, and hippocampus.
Anti-AMPAR encephalitis is a rare, poorly recognized entity with varied clinical presentations including limbic encephalitis (LE), psychosis, and is frequently accompanied with neoplasms or paraneoplastic syndrome [2]. To date, only a few individual cases of pediatric anti-AMPAR encephalitis have been reported presenting with LE or seizure [3,4,5], with limited clinical experience. Fulminant encephalitis is a severe form of encephalitis, presenting a rapid neurological deterioration and evolving into loss of consciousness, hyperthermia, psychiatric and cognitive impairment [6]. Fulminant anti-AMPAR GluR1 antibody-mediated autoimmune encephalitis is very rare and most of the previously described patients had antibodies against GluR2. Herein, we aimed to report clinical features and follow-up for a patient with fulminant anti-AMPAR GluR1 antibodies encephalitis.
Case Presentation
A 12-year-old Chinese male was admitted to Children’s Hospital of Chongqing Medical University with an 8-day history of vomiting and a 3-day history of dizziness, blurred vision, and gait disturbance. No fever, seizure, sleep disorders, speech or abnormal behavior was observed. Initial neurological examinations showed unstable standing, positive finger-to-nose and heel-to-knee-to-shin tests and stage 5 of bilateral limbs muscle power. There was no recent history of infections such as herpes simplex virus, Japanese encephalitis virus or SARS-CoV2. There was no any family history of similar condition or other types of autoimmune diseases. The patient did not take any medications prior to the development of symptoms and did not have any unusual environmental exposures.
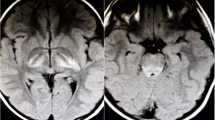
Routine blood and urine tests (Table S1), genetic metabolism screening, C-reactive protein, and autoantibody tests, including anti-nuclear antibody and anti-dsDNA, were normal. The cerebrospinal fluid (CSF) cell count was 310 (WBC cells: 230;90% mononuclear and 10% multinuclear cells), whereas CSF total protein (0.64 g/L), glucose (3.18 mmol/L), and chloride (120 mmol/L) levels were normal. PCR for herpes simplex virus, coxsackievirus, measles virus, varicella zoster virus and enterovirus in the serum and CSF were all negative. Diffuse delta waves were found by electroencephalography in awake stage (Figure S1). An initial brain MRI revealed T2 Fluid-Attenuated Inversion Recovery (FLAIR) hyperintense signals within the left cerebellar vermis and hemisphere (Fig. 1 and Figure S2). The initial diagnosis was cerebellar encephalitis. Intravenous immunoglobulin was administered at 400 mg /kg/day for five days, and dexamethasone was administered at 0.3 mg/kg/day for six days.
Representative brain magnetic resonance imaging at disease onset, after 1 month,2 months and 4 months in the fulminant encephalitis patient. The lesions of cerebellar hemisphere and cerebellar vermis(arrowhead) were identified in T2/fluid-attenuated inversion recovery (FLAIR) imaging. T2 Signal were shown cerebral parenchymal atrophy(arrowhead) after 1 month of disease and basically recovered after 4 months
Four days after admission, the patient developed delirium and urinary incontinence with aggravated dystonia and strong resting tremors on both limbs. Eight days after admission, the patient had a high-grade fever up to 39.2 °C and became unconscious. Repeat serological testing nine days after admission showed a creatine kinase (CK) of 15,153U/L, a creatine kinase myocardial band of 8.07 U/L, a myoglobin of > 1,000 μg/L, and an aspartate aminotransferase of 192 U/L, and urinalysis showed occult blood “ + + + ”; moreover, the CK value gradually increased to 98,076 U/L.
Due to the new onset symptom of delirium and dystonia, the diagnosis of autoimmune encephalitis was suspected, antibodies against cell surface or synaptic proteins were assessed in the serum and CSF obtained using transfected HEK-293 cell by the cell-based assay and indirect immunofluorescence method (KingMed Diagnostics, Guangzhou, China). The results showed high levels of CSF (1:100) antibodies against the α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR) GluR1 but no antibodies in the serum (Fig. 2). Antibodies against AMPAR GluR2, N-methyl-D-aspartate receptor, GABA B type receptor, leucine-rich glioma inactivated protein 1 (LGI1) and Casper were negative both in serum and CSF (Figure S3). Paraneoplastic syndrome antibody (including GAD65, Zic, Tr (DNER), SOX1,Ma2,Ma1,Amphiphysin,CV2,Yo,Hu and Ri) test was negative in the serum. Tumor markers (including CEA, AFP, Ferritin and NSE), bone marrow puncture test, Chest and abdomen computed tomography (CT) were normal.
The CK value and urinalysis resolved following alkaline urine and plasma exchange, which was applied twice on the 12th and 14th days after admission. Intravenous methylprednisolone was initiated at 15 mg/kg/day for three days and then 8 mg/kg/day for three days, followed by oral prednisone at a dose of 1 mg/kg/day. The patient gradually recovered consciousness. A modified Rankin Scale (mRS) score of 4 and severe neurological deficits was observed, and the patient was transferred to the rehabilitation department 28 days after admission. Follow-up brain MRI FLAIR, one month after disease onset, showed that the cerebellar vermis lesions have partially absorbed but revealed new lesion in the right cerebellar hemisphere. Moreover, lesion evolved to cortical atrophy at 1 month but recovery at 4 months after onset (Fig. 2). Four-month later, mRS was 1, with ataxia and mild cognitive disorder.
Discussion and Conclusion
Dizziness and ataxia at the onset of the adult patients with Anti-AMPAR encephalitis account for around 18% of previous reports [7], and coma, hyperthermia, rapid diffuse cortical atrophy also reported in 2 adult fulminant encephalitis cases before [6]. To our knowledge, this is the first time reported fulminant anti-AMPAR GluR1 encephalitis in children. Cerebellar signs in the case probably due to the strong expression of GluR1 receptor mainly located in the cerebellum.
Another noteworthy feature of this case is the presence of acute rhabdomyolysis after immunotherapy. Rhabdomyolysis is a critical syndrome in which destroyed muscle fibers degrade, and muscle components leak and are released into the circulation, resulting in acute renal failure. Acute rhabdomyolysis has been observed in other autoimmune encephalitis, particularly in anti-NMDAR encephalitis; however, to our knowledge, this is the first case in the literature where prominent rhabdomyolysis was observed in anti-AMPAR antibody encephalitis. A previous study indicated that rhabdomyolysis is a frequent complication in anti-NMDAR encephalitis [8]. Li et al. [9] have reported anti-voltage-gated potassium channel-complex antibody encephalitis complicated with rhabdomyolysis. However, the precise mechanisms underlying acute rhabdomyolysis induction remain unknown. It has been indicated that immunotherapy and the use of dopamine receptor blockers (DRBs) increase the risk of rhabdomyolysis [8]. In our case, we suspected it probably due to status dystonicus. Alternatively, it could be due to the aggravation of dyskinesia, high fever, and hypersensitivity to DRB. No obvious associations were observed between disease severity and rhabdomyolysis development or CK level as observed in our case. Acute rhabdomyolysis may be a rare complication of fulminant forms of anti-AMPAR encephalitis.
No evidence of neoplasm or spectrum of paraneoplastic syndrome has been found. However, long-term follow-up is still needed because neurological symptoms may develop prior to an oncologic diagnosis being made.
Due to the limited number of fulminant cases reported in the literature, the reasons why some patients develop severe encephalitis, and what causes such variable presentation, are not known. Our case report highlights the severity and complexity of anti-AMPAR encephalitis. It is important for pediatricians to recognize this rare disease because, despite severe clinical deficits of anti-AMPAR fulminant encephalitis, recovery is still possible with effective and timely treatment.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- AMPAR:
-
Anti-α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor
- LE:
-
Limbic encephalitis
- CSF:
-
Cerebrospinal fluid
- FLAIR:
-
Fluid-Attenuated Inversion Recovery
- CK:
-
Creatine kinase
- mRS:
-
Modified Rankin Scale
- DRBs:
-
Dopamine receptor blockers
References
Benke T, Traynelis SF. AMPA-Type Glutamate Receptor Conductance Changes and Plasticity: Still a Lot of Noise. Neurochem Res. 2019;44:539–48.
Lancaster E, Martinez-Hernandez E, Dalmau J. Encephalitis and antibodies to synaptic and neuronal cell surface proteins. Neurology. 2011;77:179–89.
Gleichman AJ, Panzer JA, Baumann BH, Dalmau J, Lynch DR. Antigenic and mechanistic characterization of anti-AMPA receptor encephalitis. Ann Clin Transl Neurol. 2014;1:180–9.
Trung Hieu NL, Minh Duc Duc, Tra My TT, Hieu Anh B, Tan Lien Bang M, Minh Thong P. First Reported Case of Anti-Ampa Receptor Encephalitis in a Vietnamese Adolescent. Clinical medicine insights Case reports. 2021;14:11795476211037782.
Zhang TY, Cai MT, Zheng Y, Lai QL, Shen CH, Qiao S, et al. Anti-Alpha-Amino-3-Hydroxy-5-Methyl-4-Isoxazolepropionic Acid Receptor Encephalitis: A Review. Front Immunol. 2021;12: 652820.
Joubert B, Kerschen P, Zekeridou A, Desestret V, Rogemond V, Chaffois MO, et al. Clinical Spectrum of Encephalitis Associated With Antibodies Against the α-Amino-3-Hydroxy-5-Methyl-4-Isoxazolepropionic Acid Receptor: Case Series and Review of the Literature. JAMA Neurol. 2015;72:1163–9.
Laurido-Soto O, Brier MR, Simon LE, McCullough A, Bucelli RC, Day GS. Patient characteristics and outcome associations in AMPA receptor encephalitis. J Neurol. 2019;266:450–60.
Lim JA, Lee ST, Kim TJ, Moon J, Sunwoo JS, Byun JI, et al. Frequent rhabdomyolysis inanti-NMDA receptor encephalitis. J Neuroimmunol. 2016;298:178–80.
Li R, Jiang L, Li XJ, Hong SQ, Zhong M, Hu Y. Analysis and discussion of the rare complication of autoimmune encephalitis: Two case reports. Medicine. 2018;97:e11202.
Acknowledgements
We gratefully thank the participant and his families provided consent for the publication. Besides, we would like to thank the anonymous reviewers for their critical and constructive comments and suggestions.
Funding
This work was supported by the Postdoctoral Science Fund Project of Chongqing Natural Science Foundation (No. cstc2021jcyj-bshX0243).
Author information
Authors and Affiliations
Contributions
J NM analyzed and interpreted the patient clinic data, L J substantively revised the manuscript, M C contributed to the conception and substantively revised the manuscript, W H was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were approved by the ethics committee of Children’s Hospital of Chongqing Medical University. The ethical approval number is 2021(85). Written informed consent toparticipate in this study was provided by the participants’ legal guardian of kin.
Consent for publication
Written informed consent was obtained from the patient’s parent for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Han, W., Ma, J., Jiang, L. et al. Fulminant anti-α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor GluR1 antibodies encephalitis in a Chinese boy: a case report. BMC Pediatr 22, 287 (2022). https://doi.org/10.1186/s12887-022-03356-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03356-5