Abstract
Background
In recent decades, a global increase in the prevalence of childhood overweight and obesity has been observed in children and adolescents with type 1 diabetes.
Methods
This retrospective, cross-sectional, population study examined three groups (1986, 2007, and 2018) of children and adolescents aged < 16 years diagnosed with type 1 diabetes. Overweight and obesity were defined according to the World Health Organization recommendations.
Results
The prevalence of overweight and obesity in diabetic children and adolescents was 30.2% (95% CI: 23.1–38.3). There was a significant increase from 1986 to 2007 (11.9% to 41.7%, p = 0.002) and from 1986 to 2018 (11.9% to 34.8%, p = 0.012), but no significant differences were found from 2007 to 2018 (41.7% to 34.8%, p = 0.492). The age at diagnosis was lower in the group with excess body mass (p = 0.037). No significant differences were observed in age (p = 0.690), duration of diabetes (p = 0.163), distribution according to sex (p = 0.452), metabolic control (HbA1c, p = 0.909), or insulin units kg/day (p = 0.566), between diabetic patients with overweight or obesity and those with normal weight. From 2007 to 2018, the use of insulin analogs (p = 0.009) and a higher number of insulin doses (p = 0.007) increased significantly, with no increase in the prevalence of overweight and obesity.
Conclusions
The prevalence of overweight and obesity in diabetic children and adolescents increased in the 1990s and the beginning of the twenty-first century, with stabilization in the last decade. Metabolic control and DM1 treatment showed no association with this trend.
Similar content being viewed by others
Background
A global increase in the prevalence of childhood overweight and obesity has been noted in the last few decades [1], with a tendency toward stabilization in recent population studies [2, 3]. Similarly, the incidence and prevalence of type 1 diabetes (DM1) has increased in the pediatric population [4,5,6], and excess weight has become increasingly common in diabetic children and adolescents [7]. The coexistence of overweight and obesity with DM1 should be considered both as a causal factor in the rise in incidence and as a consequence of the disease and its treatment [8]. The accelerator hypothesis postulates that insulin resistance associated with obesity accelerates the DM1 process [9]. Obesity, by promoting inflammation and autoimmunity, could lead to beta-cell failure, but the relationship is not as clear as that between obesity, increased peripheral tissue insulin resistance, and the development of type 2 diabetes [10]. A higher prevalence of overweight and obesity has been associated with intensive treatment [11], influenced by other factors such as lower educational level, onset during puberty, and sedentary lifestyle [12]. However, the increased prevalence of obesity in some diabetic patients may simply mirror an increase in obesity in the population [13].
In our study, we evaluated three groups (1986, 2007, and 2018) of children and adolescents with DM1. The objectives were: (a) to determine the variation over the last 30 years in the prevalence of overweight and obesity in these patients, according to international childhood growth criteria [14]; and (b) to observe possible associations between nutritional status and sociodemographic factors such as age, sex, and obesogenic environment, as well as clinical factors including duration of diabetes, metabolic control, and insulin therapy.
Methods
Design, setting, and study subjects
This retrospective cross-sectional population study comprised three cohorts (1986, 2007, and 2018) of all children and adolescents under 16 years of age followed in the Pediatric Endocrinology Unit of a tertiary hospital and diagnosed with DM1 according to the recommendations of the International Society for Pediatric and Adolescent Diabetes [15]. The 1986 and 2007 groups participated in a previous study assessing the relationship between metabolic control of DM1 and nutritional status [16]. All data were extracted from the last visit recorded in the medical record for the study year. We also obtained the data 6–12 months before the diagnosis of diabetes diagnosis from the electronic medical record for the 2018 group. The Ethics Committee approved the data analysis, and the parents signed the informed consent. Patients diagnosed with DM1 who were not receiving insulin therapy, cases of neonatal diabetes, type 2 diabetes, and those with other diseases in addition to DM1 were excluded.
Variables and data collection
The variables studied are presented in Table 1. Body mass index (BMI) was calculated using weight (SECA®700 scale, with a precision of 100 g) and height (SECA®220 stadiometer, with a precision of 1 mm). To describe nutritional status, the Z-scores for height and BMI were used, applying the LMS method [17, 18] and the World Health Organization (WHO) Child Growth Standards. The main study variable was the prevalence of overweight and obesity, which was determined according to the WHO references, as follows: for children under 5 years of age, overweight is defined as a BMI-Z > 2 SD and obesity as a BMI-Z > 3 SD, and for children over 5 years of age, overweight is defined as a BMI-Z > 1 SD and obesity as a BMI-Z > 2 SD.
HbA1c, an important indicator of metabolic control in DM1, was determined in 1986 using chromatography (Menarini®) with JDS/JSCC calibration and in 2007 and 2018 using high-performance liquid chromatography (Bio-Rad®) with NGSP/DCCT calibration. To allow comparison, the values were expressed in NGSP/DCCT units (%) following the recommendations of the Global Consensus for Standardization of HbA1c measurement [19]. Intensive therapy was considered to be administration of three or more daily insulin injections or treatment with an external insulin pump, with dose adjustments based on at least four glucose readings per day with test strips or continuous glucose monitoring [20, 21].
Statistical analysis
All statistical analyses were performed with SPSS Statistics, version 27.0 (IBM Corporation, Armonk, NY, USA). To determine the normality of the quantitative variables, the Lilliefors (Kolmogorov–Smirnov) test (n ≥ 50) or the Shapiro–Wilk test (n < 50) was applied. Qualitative variables were expressed as frequencies and percentages with their 95% confidence intervals (CI). Quantitative variables with a normal distribution were described using the mean and standard deviation (SD) and nonparametric variables with the median and interquartile range (IQR). The Chi2 test (Pearson), Fisher’s exact test, and comparison of proportions were used to compare the qualitative variables. The analysis of parametric quantitative variables between two groups was conducted using Student’s t-test and for nonparametric variables the Mann–Whitney U test. The ANOVA test was used for categorical variables with more than two groups with a normal distribution, and the Kruskal–Wallis test was used when the distribution was not normal. To test for differences within each group, a post hoc analysis was performed with the Bonferroni correction for multiple comparisons. To study the association between BMI-Z and the continuous quantitative variables, the Pearson test was used when the variables had a normal distribution or the Spearman test when they did not. To determine the risk of being overweight or obese, the odds ratio (OR) was calculated. A value of p < 0.05 was considered statistically significant.
Results
Table 1 describes the characteristics of the overweight and obese diabetic children and adolescents. Table 2 summarizes the prevalence of overweight and obesity in the three groups studied, and its evolution from 1986 to 2018 is depicted in Fig. 1. The proportion of overweight, including obesity, increased significantly from 1986 to 2007 and from 1986 to 2018, but not from 2007 to 2018.
When comparing the overweight and obese diabetic children and adolescents with those of normal weight (Table 1), no significant differences were found in the distribution by age, sex, years with diabetes, continuous insulin infusion pump therapy, glucose monitoring, or proportion at diagnosis of children aged < 5 years and > 10 years.
No correlation was found between BMI-Z at the time of the study (median 0.42, IQR 1.1) and age at onset of diabetes (median 7.2, IQR 4.3) in the total sample (p = 0.202) or BMI-Z at diagnosis (mean 0.67 ± 1.14) and age at onset of diabetes (median 7.1, IQR 4.5) in the 2018 group (p = 0.632).The age at diagnosis was lower in the overweight and obese children and adolescents (Table 1), but this significant difference was only observed in the 2018 group (p = 0.045). The children aged < 5 years had a BMI-Z at diagnosis similar to the children > 5 years (0.82 versus 0.62, p = 0.616) and at the time of the study (0.60 versus 0.45, p = 0.438), while the adolescents aged > 10 years had a significantly higher BMI-Z at diagnosis than those < 10 years (1.45 versus 0.45, p = 0.014) but not at the time of the study (0.51 versus 0.48, p = 0.878). Age at diagnosis < 5 years (OR = 1.77; 0.76–4.12) or > 10 years (OR = 0.65; 0.25–1.65) was not a risk factor for being overweight or obese. In the 2018 group, the rate of overweight and obesity was similar at diagnosis and at the end of the study (30.4% versus 34.8%, p = 0.092), and the risk estimate for the association between overweight and obesity at diagnosis and being overweight at the time of the study was not significant (OR = 0.214; 0.04–1.12).
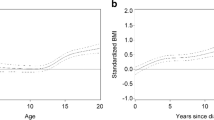
The amount of insulin used and metabolic control in the overweight and obese diabetic patients was similar to those with normal weight (Table 1). The insulin dose did not vary significantly from 1986 to 2018 (p = 0.493), but metabolic control improved from 1986 to 2018 (p < 0.001). The post-hoc analysis showed differences in HbA1c from 1986 to 2018 (8.5 to 7.4, p < 0.001) and from 2007 to 2018 (8.2 to 7.4, p = 0.005) but not from 1986 to 2007 (p = 0.090), the period in which the prevalence of overweight and obesity showed the greatest increase (Fig. 2). The use of intensive therapy (≥ 3 doses) was higher in the overweight and obese patients in all three groups (p = 0.007), but this type of therapy was only used in 2007 (91.8%) and 2018 (100%). In these patients, the use of ≥ 3 doses of insulin was not associated with a higher prevalence of overweight and obesity (p = 0.636). The proportion of patients with excess body mass receiving ≥ 4 daily insulin doses was also significantly higher (p = 0.003), but this type of therapy was only used in 2007 and 2018. From 2007 to 2018 this proportion rose from 52.1% to 82.6% (p = 0.002) but was not associated with changes in the rate of overweight and obesity in the period 2007 to 2018 (Table 1, Fig. 3).
The overweight and obese diabetic children and adolescents in the total sample showed a greater use of insulin analogs (p = 0.009). Rapid- and long-acting analogs were only used in 2007 and 2018 (56.3% to 100%, p < 0.001), but the rate of overweight and obesity showed no significant differences (p = 0.492) from 2007 to 2018 (Table 1, Fig. 4).
Discussion
Over the three decades studied, diabetic children and adolescents showed improved metabolic control, and the use of rapid- and long-acting insulin analogs and intensive therapy with stricter glycemic monitoring has become widespread. In parallel, an increase in the prevalence of overweight and obesity in children and adolescents with DM1 of over 29% was observed from 1986 to 2007, with stabilization from 2007 to 2018, although with very high figures. These rates of overweight and obesity are similar to those reported in diabetic children in other Mediterranean areas [22].
In the sample studied, although the age at diagnosis of DM1 was significantly lower in the overweight and obese diabetic patients, there was no positive correlation between BMI-Z and age at diagnosis as observed by other authors [23], and the duration of diabetes showed no correlation with excess weight, as reported in other studies [24]. No significant differences were observed in BMI-Z at diagnosis in the children with DM1 who had onset before 5 years of age, as postulated by the accelerator hypothesis, and being younger than 5 years of age at diagnosis was not associated with increased risk of overweight or obesity [9]. The patients with onset from the age of 10 years had higher BMI-Z at diagnosis, but being > 10 years of age at diabetes onset was not associated with an increased risk of overweight or obesity.
Intensive therapy and improved metabolic control have been associated with excessive weight gain in diabetic children and adolescents [11, 25] which could partially diminish the beneficial effects of improved diabetes control on microvascular and macrovascular complications [26], although other studies have not been able to confirm this relationship [22]. In our study, metabolic control improved throughout the period analyzed (Fig. 2), and the use of intensive therapy and insulin analogs in the 2007 and 2018 groups was not associated with a higher risk of overweight and obesity. The number of patients on intensive therapy and using insulin analogs increased significantly from 1986 to 2007 as did the rate of overweight and obesity, coinciding with the obesity pandemic. From 2007 to 2018 the proportion of children and adolescents receiving higher doses of insulin and using insulin analogs continued to increase to 100% in 2018, but the prevalence of overweight and obesity observed did not change from 2007 to 2018 (Figs. 3 and 4), in contrast to other studies [27].
The various environmental and biological factors that contribute to overweight and obesity in the general population, other than the insulin regimen, could partly explain the evolution of the prevalence of overweight and obesity in diabetic children and adolescents during the period studied [8, 28]. The global rise in childhood overweight and obesity observed in the last forty years has shown a tendency to stabilize in recent studies [3]. The pediatric population in our healthcare area, which was the source of the sample studied, has shown a similar evolution [2] with very high figures for overweight and obesity. Nonetheless, as other authors have reported [10], the incidence of DM1 does not show a linear relationship with excess body mass, and during the period studied, the incidence of DM1 in children and adolescents continued to increase steadily in Europe [4], North America [29, 30], and Spain [5]. As other authors have observed in the adult population with DM1 [31], our findings reveal an increase in the prevalence of overweight and obesity in diabetic children and adolescents, with stabilization in the last ten years, similar to that seen in the population from which the sample was drawn [2, 32], as shown in Fig. 5. The relationship between the distribution of overweight and obesity in diabetic children and adolescents and the childhood obesity epidemic has also been suggested by other authors [28]. Factors such as genetic predisposition [33], an obesogenic environment [24], and the microbiome [8], which promote obesity and increased insulin resistance in the general population, would also affect diabetic children and adolescents.
Although the rate of obesity and overweight in diabetic children and adolescents has stabilized in our healthcare area, the figures are still very high, contributing to an increased risk of hypertension, dyslipidemia, and early cardiovascular disease in this susceptible population [30]. The effect of overweight and obesity on the metabolic syndrome in diabetic patients has been studied in children [13, 30] and especially in adults [11, 31], in whom obesity has been associated with an increased risk of hospitalization [34]. These findings underscore the importance of early diagnosis and treatment of excess weight and its metabolic consequences in this at-risk group. Diabetes management encouraging healthy eating and exercise is key to preventing obesity, overweight, and cardiovascular disease.
Limitations
This study has several limitations, including its retrospective design and that it was undertaken at a single center serving a single health department, and therefore the number of patients was small. Other limitations were the lack of data on the pubertal status of the patients and the lack of waist circumference to estimate the metabolic syndrome with the criteria currently used. As strengths, this study covers the evolution of three groups of children with DM1 (n = 136) over the last 30 years in a health area for which we have data on overweight and obesity in the source population. The criteria used to define these groups were homogeneous and based on international standards.
Conclusions
The number of overweight and obese diabetic children and adolescents has stabilized in the last decade but continues to be very high. In each group, the prevalence mirrored that observed in the source population. If, as our study suggests, the increased prevalence of overweight and obesity in some diabetic patients could simply reflect an increase in obesity in the general population, continued identification of the emerging factors behind the obesity epidemic in the general and diabetic populations will be needed in order to implement health policies that promote healthy eating and reduce sedentary lifestyles. The relationship between overweight and obesity in diabetic children with age at diagnosis, accelerated onset, intensive therapy, duration of diabetes, and its long-term effects requires further investigation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DM1:
-
Type 1 diabetes
- WHO:
-
World Health Organization
- BMI:
-
Body mass index
- BMI-Z:
-
Body mass index z-score
- CI:
-
95% Confidence interval
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- RAIA-LAIA:
-
Rapid-acting and long-acting insulin analogs
- Regular-NPH:
-
Regular and NPH insulin
- CGM:
-
Continuous glucose monitoring
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42.
Pastor-Fajardo MT, Bosch-Giménez VM, Larqué E, Navarro CS, Fuentes-Castelló MÁ, Pastor-Rosado J. Child and Adolescent Obesity Prevalence and secular trend of childhood overweight and obesity in a Mediterranean area of Southeast Spain. Child Adolesc Obes. 2020;3(1):136–49.
Garrido-Miguel M, Cavero-Redondo I, Álvarez-Bueno C, Rodríguez-Artalejo F, Moreno LA, Ruiz JR, et al. Prevalence and Trends of Overweight and Obesity in European Children from 1999 to 2016: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019;173(10): e192430.
Patterson CC, Gyürüs E, Rosenbauer J, Cinek O, Neu A, Schober E, et al. Trends in childhood type 1 diabetes incidence in Europe during 1989–2008: Evidence of non-uniformity over time in rates of increase. Vol. 55, Diabetologia. 2012. p. 2142–7.
Conde Barreiro S, Rodríguez Rigual M, Bueno Lozano G, López Siguero JP, González Pelegrín B, Rodrigo Val MP, et al. Epidemiology of type 1 diabetes mellitus in children in Spain. An Pediatr (Barc). 2014;81(3):189.e1-189.e12.
Mayer-Davis EJ, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, et al. Incidence Trends of Type 1 and Type 2 Diabetes among Youths, 2002–2012. N Engl J Med. 2017;376(15):1419–29.
Dubose SN, Hermann JM, Tamborlane WV, Beck RW, Dost A, Dimeglio LA, et al. Obesity in Youth with Type 1 Diabetes in Germany, Austria, and the United States. J Pediatr. 2015;167(3):627-632.e4.
Chobot A, Górowska-Kowolik K, Sokołowska M, Jarosz-Chobot P. Obesity and diabetes—Not only a simple link between two epidemics. Diabetes Metab Res Rev. 2018;34(7):1–9.
Wilkin TJ. The convergence of type 1 and type 2 diabetes in childhood: The accelerator hypothesis Wilkin Convergence of type 1 and type 2 diabetes. Pediatr Diabetes. 2012;13(4):334–9.
Abbasi A, Juszczyk D, van Jaarsveld CHM, Gulliford MC. Body Mass Index and Incident Type 1 and Type 2 Diabetes in Children and Young Adults: A Retrospective Cohort Study. J Endocr Soc. 2017;1(5):524–37.
Nathan DM. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: Overview. Diabetes Care. 2014;37(1):9–16.
Liese AD, Ma X, Maahs DM, Trilk JL. Physical activity, sedentary behaviors, physical fitness, and their relation to health outcomes in youth with type 1 and type 2 diabetes: A review of the epidemiologic literature. J Sport Heal Sci. 2013;2(1):21–38.
Pinhas-Hamiel O, Levek-Motola N, Kaidar K, Boyko V, Tisch E, Mazor-Aronovitch K, et al. Prevalence of overweight, obesity and metabolic syndrome components in children, adolescents and young adults with type 1 diabetes mellitus. Diabetes Metab Res Rev. 2015;31(1):76–84.
World Health Organization. Childhood overweight and obesity [Internet]. [Accessed April-2021]. Available from: https://www.who.int/dietphysicalactivity/childhood/es/
Mayer-Davis EJ, Kahkoska AR, Jefferies C, Dabelea D, Balde N, Gong CX, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Definition, epidemiology, and classification of diabetes in children and adolescents. Pediatr Diabetes. 2018;19(June):7–19.
Pastor J, Bosch V, Fajardo MT, Goberna F, Vargas F. Diferencias de estado nutricional, control metabólico y tratamiento de la diabetes tipo 1 en dos décadas. An Pediatr. 2011;75(4):259–65.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. Br Med J. 2000;320(7244):1240–3.
Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284–94.
Hanas R, John G. Consensus statement on the worldwide standardization of the hemoglobin A1C measurement. Diabetes Care. 2010;2010:1903–4.
Nathan DM, Cleary PA, Backlund JC, Genuth SM, Lachin JM, Orchard TJ, Raskin Ph ZB. Intensive Diabetes Treatment and Cardiovascular Disease in Patients with Type 1 Diabetes. N Engl J Med. 2005;353(25):2643–53.
Chiang JL, Kirkman MS, Laffel LMB, Peters AL. Type 1 diabetes through the life span: A position statement of the American Diabetes Association. Diabetes Care. 2014;37(7):2034–54.
Sevaliev N, Strich D, Avnon-Ziv C, Levy-Khademi F. The metabolic consequences of overweight in a cohort of children with type 1 diabetes. J Pediatr Endocrinol Metab. 2019;32(7):715–9.
Gimenez M, Aguilera E, Castell C, de Lara N, Nicolau J, Conget I. Relationship Between BMI and Age at Diagnosis of Type 1 Diabetes in a Mediterranean Area in the Period of 1990–2004. Diabetes Care. 2007;30(6):1593–5.
Maffeis C, Birkebaek NH, Konstantinova M, Schwandt A, Vazeou A, Casteels K, et al. Prevalence of underweight, overweight, and obesity in children and adolescents with type 1 diabetes: Data from the international SWEET registry. Pediatr Diabetes. 2018;19(7):1211–20.
Nansel TR, Lipsky LM, Iannotti RJ. Cross-sectional and longitudinal relationships of body mass index with glycemic control in children and adolescents with type 1 diabetes mellitus. Diabetes Res Clin Pract. 2013;100(1):126–32.
Babar G, Clements M, Dai H, Raghuveer G. Assessment of biomarkers of inflammation and premature atherosclerosis in adolescents with type-1 diabetes mellitus. J Pediatr Endocrinol Metab. 2019;32(2):109–13.
Fullerton B, Jeitler K, Seitz M, Horvath K, Berghold A, Siebenhofer A. Intensive glucose control versus conventional glucose control for type 1 diabetes mellitus. Cochrane Database Syst Rev. 2014;2014(2):CD009122.
Corbin KD, Driscoll KA, Pratley RE, Smith SR, Maahs DM, Mayer-Davis EJ. Obesity in type 1 diabetes: Pathophysiology, clinical impact, and mechanisms. Endocr Rev. 2018;39(5):629–63.
Liese AD. The burden of diabetes mellitus among US youth: Prevalence estimates from the SEARCH for Diabetes in Youth Study: SEARCH for Diabetes in Youth Study Group. Pediatrics. 2006;118(4):1510–8.
Hamman RF, Bell RA, Dabelea D, D’Agostino RB, Dolan L, Imperatore G, et al. The SEARCH for diabetes in youth study: Rationale, findings, and future directions. Diabetes Care. 2014;37(12):3336–44.
Fellinger P, Fuchs D, Wolf P, Heinze G, Luger A, Krebs M, et al. Overweight and obesity in type 1 diabetes equal those of the general population. Wien Klin Wochenschr. 2019;131(3–4):55–60.
Bataller, A. Redondo, MJ. Rioja, L. Villena J. La Salud Infantil en la edad escolar en la Comunitat Valenciana. Análisis de la hoja de Seguimiento Infantil. Año 2018. [Internet]. València; 2020. Available from: http://www.sp.san.gva.es/DgspPortal/docs/Informe_Salud_Escolar_2018_cas.pdf
Censin JC, Nowak C, Cooper N, Bergsten P, Todd JA, Fall T. Childhood adiposity and risk of type 1 diabetes: A Mendelian randomization study. PLoS Med. 2017 Aug 1;14(8).
Vestberg D, Rosengren A, Olsson M, Gudbjörnsdottir S, Svensson AM, Lind M. Relationship between overweight and obesity with hospitalization for heart failure in 20,985 patients with type 1 diabetes: A population-based study from the Swedish National Diabetes Registry. Diabetes Care. 2013;36(9):2857–61.
Acknowledgements
The authors thank Maria Repice for her help with the English language version of the text.
Funding
This study has received no funding.
Author information
Authors and Affiliations
Contributions
MP and JP conceptualized the study. MP and JP collected the anthropometric and clinical variables. MF collected and analyzed the laboratory data. MP, JP and VB carried out the statistical analysis and interpreted the results. MP and JP wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval consent to participate
All methods were performed in accordance with the Declaration of Helsinki. This study was approved by the Clinical Research Ethics Committee of Hospital General Universitario de Elche (reference number PI 46/2020). The signed informed consent to participate in the study was obtained from all children parents or legal guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pastor-Fajardo, M.T., Fajardo-Giménez, M.T., Bosch-Giménez, V.M. et al. Changes from 1986 to 2018 in the prevalence of obesity and overweight, metabolic control and treatment in children with type 1 diabetes mellitus in a Mediterranean area of Southeast Spain. BMC Pediatr 22, 274 (2022). https://doi.org/10.1186/s12887-022-03330-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03330-1