Abstract
Background
The role of serum Procalcitonin (PCT) in adults in diagnosis of Community acquired pneumonia (CAP) is well established, however, role in pediatric CAP remains controversial.
Objectives
The objective of this study was to investigate the utility of serum procalcitonin in differentiating bacterial community-acquired lower respiratory tract infection from non-bacterial respiratory infection in children; radiologically confirmed pneumonia was used as the reference. In addition, we assessed the utility of adding the PCT assay to the clinical criteria for diagnosis of pneumonia.
Study design
Subanalysis of a larger prospective,multicentriccohort study.
Participants
Children, 2 months to 59 months of age, attending paediatric OPD of 5 urban tertiary care hospitals, suffering from acute respiratory infection (ARI).
Intervention
Detailed clinical history and examination findings of enrolled children were recorded on predesigned case record form. Samples for PCT were obtained at admission and were measured centrally at the end of the study except for one site using VIDAS® B.R.A.H.M.S PCT kit (Biomerieux SA, France).
Outcomes
Sensitivity and specificity of procalcitonin for diagnosis of radiologically confirmed pneumonia.
Results
Serum Procalcitonin was measured in 370 patients; median (IQR) age of these children being 12 (7, 22) months, 235 (63.5%) were boys. The median (IQR) serum procalcitonin concentration was 0.1(0.05, 0.4) ng/mL.Sensitivity and specificity of raised PCT (> 0.5 ng/mL) for pneumonia as per any CXR abnormalities were 29.7% and87.5%,(P < 0.001) respectively. Raised PCT was also significantly associated with consolidation (34.5%,79.2%,P < 0.02)and pleural effusion(54.6%,79%,P < 001). Adding PCT to the existing clinical criteria of WHO did not improve the sensitivity for diagnosis of pneumonia. PCT was significantly higher in children with severe pneumonia.
Conclusion
Positive PCT (> 0.5 ng/mL) is significantly associated with radiographic pneumonia but not with pneumonia based on WHO criteria.However, it can act as a surrogate marker for severe pneumonia.
Similar content being viewed by others
Introduction
Community-acquired pneumonia (CAP) is a common clinical problem in childhood [1]. Bacterial pneumonia cannot be differentiated from viral pneumonia based on clinical or chest radiographic findings [2]. The use of biomarkers in clinical practice has increased substantially specially because proponents claim that biomarkers may improve the early diagnosis of infections and be available as a point-of-care tool [3]. This may allow earlier and better identification and treatment of patients with severe life-threatening infections.
Procalcitonin(PCT) is a protein, precursor of hormone Procalcitonin, normally produced by neuroedocrine cells present in thyroid, lung and intestine [4, 5]. Procalcitonin (PCT) has been introduced as a marker of bacterial infection, having been used to differentiate between septic and other infections in pediatric patients [6]. In many adult studies, it’s been well established that higher PCT concentration is associated with isolation of typical bacterial organisms [7, 8], especially, in relation to bacteraemic CAP [9, 10]. However,same evidence is lacking in children. Two studies in children [11, 12] found limited association between PCT concentration and identification of organisms in CAP where as in other studies found reasonably good association [13, 14]. Many previous studies were limited by sensitivity of PCT assays, identification of organisms and testing methods. The objective of this study was to investigate the utility of serum procalcitonin in differentiating bacterial community-acquired lower respiratory tract infection from non-bacterial respiratory infection in children; radiologically confirmed pneumonia was used as the reference. In addition, we assessed the utility of adding the PCT assay to the clinical criteria for diagnosis of pneumonia.
Methodology
Study design
Prospective cohort study. The currently reported study is a part of a larger study designed to evaluate the effectiveness of acute respiratory infection treatment unit (ATU) in management of acute respiratory tract infection (ARI).
Settings
Study was carried out at the following five urban tertiary care hospitals of India: 1. Sher-I-Kashmir Institute of Medical Sciences (SKIMS), Srinagar 2. All India Institute of Medical sciences (AIIMS), Jodhpur, 3. AIIMS, Bhubaneshwar 4. Karnataka Institute of Medical Sciences, Hubbali, Karnataka 5. MP Saha Medical College, Jamnagar; AIIMS, New Delhi was the coordinating centre.
Study duration
Two years (from June 2016 to May 2018).
The methodology of the main study has been described in previous publications [15,16,17]. Briefly, previously healthy children, between 2 to 59 months of age with ARI were enrolled in the main study. Any cough and/or breathing difficulty for duration of less than 2 weeks were considered as ARI. Procalcitonin estimation was done in subset of patients with clinical pneumonia based on WHO criteria [18] at the time of admission.
Chest radiograph was done in all cases of clinical pneumonia and every fifth child with no pneumonia due to limited budget at the time of enrolment plus avoidance of unnecessary radiation exposure in children with URI.
Target condition and reference standard
Community acquired pneumonia (CAP) was target condition and radiological diagnosis was used as reference standard.
Primary outcome
Children with abnormal chest radiograph was considered suggestive of bacterial pneumonia. Sensitivity, specificity and likelihood ratios were calculated for different levels of serum procalcitonin levels for diagnosis of pneumonia, using radiological confirmed pneumonia as the reference.
Sample Size
As it was a sub-analysis, we did not perform sample size calculations for this separately. Within the budget availability, the sample size from all the sites for PCT was estimated to be 370 in children who were expected to be subjected to X ray chest.
Diagnosis of pneumonia
Clinical pneumonia
Clinical diagnosis of pneumonia was made by the physician before reading the CXR. The following WHO criteria were used for diagnosis of pneumonia (15):
-
1)
cough or difficulty breathing and
-
2)
age-specific tachypnea (≥ 50 breaths per minute for children 2–11 months of age and ≥ 40 breaths per minute for children 1–5 years of age).
Severe pneumonia
Along with presence of age specific fast breathing and/ or chest in drawing, Children with the presence of any danger signs like lethargy, inability to drink, drowsiness, were classified as severe pneumonia.
Radiologically confirmed pneumonia
It was defined as presence of pulmonary infiltrate or consolidation. Additional findings of interstitial infiltrates, peribronchial thickening and atelectasis were also recorded.
Chest X-ray
As there were no consensus for reference standard for diagnosis of pneumonia, in this study, we have taken chest radiographic abnormality as gold standard.Chest radiograph (an anterior–posterior or posterior-anterior view), preferably digital (analogue if digital is not available) was done in all cases of clinical pneumonia. The radiographs was interpreted by site investigator at the time of enrolment and appropriate treatment to the patient was administered as per WHO guideline. The films of chest X ray were digitalisedor soft copy of the digital x-ray or hard copy of X rays were sent to the coordinating centre at the All India Institute of Medical Sciences, New Delhi. All CXR were read by two independent pediatricians(SKK/KRJ), who were blinded for the clinical diagnosis of patient. In case of disagreement about the presence or absence of pneumonia, chest x-rays were read by a third pediatrician(RL) without knowledge of the previous evaluations and final findings matching for two of them were considered final for purpose of analysis.
Blood tests
It had been planned to collect two mL blood for procalcitonin (PCT) estimation at the time of admissionfrom all children with suspected pneumonia enrolled at all the sites, however due to budget constraints only 370 samples could be collected. The serum samples were kept frozen at -80 °C in respective centres before they were transported in a cold chain to AIIMS, New Delhi(from three sites AIIMS Bhubaneshwar; KIMS, Hubballi; and SKIMS, Srinagar) while samples collected at Jodhpur were tested locally.At AIIMS, Delhi, as well as in Jodhpur, the procalcitonin (PCT) assay was done using VIDAS® B.R.A.H.M.S. PCT kit (Biomerieux SA, France). Cut-off for positive serum procalcitonin level (PCT + ve) has been considered at > 0.5 ng/mL and PCT –ve if serum procalcitonin level ≤ 0.5 ng/mL. The cut-off was based on earlier studies [19, 20].
Ethical considerations
Ethical approval was obtained from Ethics Committee of KIMS and other five study sites.
Written informed consent was obtained from legal guardians/parents of participants. A copy of consent form was given to parents/ guardian. Personal information (paper and electronic registers) were stored in an appropriate manner to ensure full confidentiality.
Statistical analysis
All data were entered in Microsoft Access software and analysed by statistical software STATAv.14 (College Station, TX, US). Sensitivity, specificity, likelihood ratios (positive and negative) and predictive values (positive and negative) were calculated for PCT considering the radiographic pneumonia as the standard for diagnosis of pneumonia. Receiver operating characteristic (ROC) curve was used to evaluate the ability of PCT to differentiate between pneumonia and no pneumonia diagnosed by various criteria.
Results
A total 7026 children with ARI (39% of screened children) were enrolled in the main study (Fig. 1). According to the WHO criteria, 13.4% (938) had pneumonia [37%(347) of them had severe pneumonia].Serum Procalcitonin was measured in 370 (235 boys) patients; median (IQR) age of these children being 12 (7, 22) months. Pneumonia as per WHO criteria was present in 312/370 children. The median (IQR) serum procalcitonin concentration was 0.1(0.05, 0.4) ng/mL.Positive PCT level (> 0.5 ng/mL) was seen in 83 (22.4%) children.
The demographic and clinical details of children in whom PCT level were measured are shown in Table 1. Of these children, 87.9% had pneumonia with raised PCT level as per WHO clinical case definition., However, 83.3% of those with normal PCT (< 0.5 ng/ml) also had pneumonia.
The association of PCT with chest X-ray abnormalities is detailed in Table 2. In the original study evaluating the effectiveness of ATU in treatment of ARI, 1273 CXR were readable. In the subset of 370 children, who had PCT levels estimated (inclusion criteria for this study), 337 CXRs were readable. Positive PCT is significantly associated with any abnormality on CXR (the gold standard of diagnosis of pneumonia). The sensitivity and specificity were 29.7% and 87.5% respectively (P < 0.001). And also consolidation on chest X-ray is significant(P < 0.02). However, PCT is not significantly associated with the existing WHO criteria for clinical pneumonia.
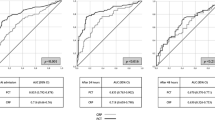
Figure 2 (a, b) shows ROC for PCT in relation to any abnormality on CXR (AUC: 0.61) and WHO clinical Pneumonia (area under curve(AUC): 0.57.Sensitivity, specificity, predictive values, likelihood ratios of PCT for pneumonia diagnosed by different criteria are shown in Table 3.
PCT levels were significantly higher in the 22 children with uncomplicated para-pneumonic pleural effusion [0.58 (0.17, 4.02) ng/mL vs. 0.1 (0.05, 0.35); p = 0.001] as compared to those who had no pleural effusion.
Tables 4 and 5 shows comparison of PCT (at different cut-offs) between any abnormality in CXR and no abnormality and non severe pneumonia and severe pneumonia (as per WHO clinical criteria, respectively. The PCT (> 0.25 ng/ml) is significantly associated with any abnormality in CXR, however no significant difference observed between severe and non severe pneumonia.
The sensitivity and specificity of PCT in various combination with the WHO criteria considering any abnormality on chest X-ray as the gold standard for diagnosis of pneumonia, are given in Table 6. The sensitivity and specificity of the existing WHO criteria was 56.5% and 66.2%, respectively (data sent for publication separately). Adding PCT level > 0.5 ng/mL increased the specificity at the cost of sensitivity. If both existing criteria and raised PCT levels were taken as and/or criteria, the sensitivity (57.7%) and specificity (65.9%) did not improve substantially.
Discussion
Although in adults, Procalcitonin as a biomarker for sepsis well established, its role in infections in neonates,children remains less conclusive. CAP is one of the most common infections in children and has been studied extensively because it’s the most frequent cause of hospitalisation and second most common cause of death in children in developing countries [21].
In this study, an attempt was made to find the association between procalcitonin and pneumonia as per both clinical and radiological criteria of WHO. We found positive PCT (> 0.5 ng/mL) was significantly associated with any abnormality on CXR (the gold standard of diagnosis of pneumonia) as well as consolidation on chest X-ray. However, PCT was not significantly associated with the existing WHO criteria for clinical pneumonia. Long et al. reported that chest radiograph has a sensitivity of 46–77%, and biomarkers including white blood cell count, procalcitonin, and C-reactive protein provide little benefit in diagnosis of pneumonia [22]. Korpi et al. evaluated serum PCT in 190 children with radiologically confirmed CAP in a prospective population based study and concluded that there was no useful role for PCT in diagnosis of pneumonia in children in primary health care settings [23]. They concluded that Procalcitonin was poor biomarker to identify radiographic pneumonia (a surrogate for bacterial pneumonia). Using serum procalcitonin may improve specificity but sensitivity remains very low.
In the current study, we used cut off level for PCT as > 0.5 ng/ml. as Some earlier studies have suggested use of a cut-off of > 0.5 ng/mL for identify respiratory tract infections needing antibiotics [19, 20]. However, when we analysed even with lower cut off level(PCT > 0.25 ng/ml),significance was found with any abnormality in CXR and not with clinical pneumonia. Esposito et al. using a 0.25 ng/ml PCT threshold in children found a significant reduction of both antibiotic treatment rate and duration [14]. Conversely, Baer et al., showed no significant reduction in antibiotic treatment rates [24]. A reason for such difference could be that the PCT threshold defined in adult studies (0.25 ng/ml) might be too low for decision making in children with CAP.
In an effort to improve the clinical diagnosis of pneumonia and adding point of care test like PCT levels, we evaluated the sensitivity and specificity of some of the pertinent clinical features, and PCT levels alone or in combination. The sensitivity and specificity of the existing WHO criteria was 56.5% and 66.2%, respectively. Adding PCT level > 0.5 ng/mL increased the specificity at the cost of sensitivity. If both existing criteria and PCT were taken as and/or criteria, the sensitivity and specificity did not change much (57.7%% and 65.9%, respectively). However, when used as part of an algorithm in adults in combination with clinical judgment in patients with LRTIs, procalcitonin has been shown to reduce unnecessary antibiotic use by about 25 to 50% without increasing morbidity or mortality [25,26,27]. The data regarding children despite being limited, were consistent with those in adults [14]. Dudognon et al. cautioned to promote a rational implementation of PCT especially in children with community acquired pneumonia [28].
We also found that procalcitonin was higher in children with severe pneumonia than in those with non-severe pneumonia. Don et al. and Yadav et al. found that serum PCT was a useful indicator of the severity of CAP in children when comparing the PCT values between those who needed hospitalization and those who did not(P < 0.0012), and in comparing the alveolar(P < 0.0003) and interstitial pulmonary involvement on chest radiograph [29, 30]. Lee et al. have reported that both PCT and CRP was increased in lobar pneumonia compared to bronchopneumonia; however, only PCT was raised in pneumonia with radiologic finding suggestive of severity [31].
Our findings show that serum PCT values are higher in children with pneumonia with pleural effusion (PE) than in children with pneumonia without pleural effusion. Fonseca et al. reported PE in 10.2% cases. In their study, the PCT level on admission ≥ 1.0 ng/ml was associated with PE [32]. Though the relationship between pleural inflammation and biomarkers has not been well established in children, it has been suggested that pleural inflammation associated with CAP is a continuous process, and inflammatory cytokines are significantly higher according to the stage of disease in the evaluated children [33].
The main strengths of our study were i)prospective collection of samples and ii) multicentric nature involving various regions of the country; however, the study was limited by small sample size in relation to number of pneumonia cases recruited in the study. Additionally, there was lack of use of optimised bacterial diagnostic tests like cultures, antigen detection tests and polymerase chain reaction.
Conclusion
Positive PCT is significantly associated with radiographic pneumonia but not with pneumonia as per WHO criteria. Adding PCT as a point of care test to existing WHO clinical criteria, didn’t add much value.However, it can act as a surrogate marker for severe pneumonia.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
All data generated or analysed during this study are included in this published.
Abbreviations
- PCT:
-
Procalcitonin
- CAP:
-
Community acquired pneumonia
- ATU:
-
Acute respiratory infection treatment unit
- ARI:
-
Aacute respiratory tract infection
- BPD:
-
Bronchopulmonary Dysplasia
- GER:
-
Gastro-oesophageal reflux
- HIV:
-
Human immunodefiency virus
- CXR:
-
Chest –X-Ray
- WHO:
-
World Health Organisation
- SpO2:
-
Oxygen saturation
- ROC:
-
Receiver operating characteristic curves
- PE:
-
Pleural effusion
References
PrincipiN ES. Biomarkers in pediatric community-acquired pneumonia. Int J Mol Sci. 2017;18:447.
Lee JY, Hwang SJ, Shim JW, Jung HL, Park MS, Woo HY, Shim JY. Clinical significance of serum procalcitonin in patients with community-acquired lobar pneumonia. Korean J Lab Med. 2010;30:406–13.
Hoshina T, Nanishi E, Kanno S, Nishio H, Kusuhara K, Hara T. The utility of biomarkers in differentiating bacterial from nonbacterial lower respiratory tract infection in hospitalized children: Difference of the diagnostic performance between acute pneumonia and bronchitis. J Infect Chemother. 2014;10:616–20.
Jacobs JW, Lund PK, Potts JT Jr, Bell NH, Habener JF. Procalcitonin is a glycoprotein. J BiolChem. 1981;256:2803–7.
Reinhart K, Karzai W, Meisner M. Procalcitonin as a marker of the systemic inflammatory response to infection. Intensive Care Med. 2000;26:1193–200.
Zhu F, Jiang Z, Li WH, Wei HY, SuGD. Clinical significance of serum procalcitonin level monitoring on early diagnosis of severe pneumonia on children. Eur Rev Med Pharmacol Sci. 2015;19:4300–3.
Stockmann C, Ampofo K, Killpack J, Williams DJ, Edwards KM, Grijalva CG, et al. Procalcitonin accurately identifies hospitalizedchildren with low risk of bacterial community-acquired pneumonia. J Pediatric Infect Dis Soc. 2018;7:46–53.
SalluhJIF, Souza-Danta VC, Po´vo P. The current status of biomarkers for the diagnosis of nosocomial pneumonias. CurrOpinCrit Care. 2017;23:000–000.
Mahajan P, Grzybowski M, Chen X, Kannikeswaran N, Stanley R, Singal B, et al. Procalcitonin as a marker of serious bacterial infections in febrile children younger than 3 years old. AcadEmerg Med. 2014;21:171–9.
Zhu F, Wei H, Li W. Significance of serum procalcitonin levels in differential diagnosis of pediatric pneumonia. Cell BiochemBiophys. 2015;73:619–22.
Agnello L, Bellia C, Di Gangi M, Lo Sasso B, Calvaruso L, Bivona G, et al. Utility of serum procalcitonin and C-reactive protein in severity assessment of community-acquired pneumonia in children. Clin Biochem. 2016;49:47–50.
Toikka P, Irjala K, Juven T, Virkki R, Mertsola J, Leinonen M, Ruuskanen O. Serum procalcitonin, C-reactive protein and interleukin-6 for distinguishing bacterial and viral pneumonia in children. Pediatr Infect Dis J. 2000;19:598–602.
Luaces-Cubells C, Mintegi S, García-García JJ, Astobiza E, Garrido-Romero R, Velasco-Rodríguez J, Benito J. Procalcitonin to detect invasive bacterial infection in non-toxic-appearing infants with fever without apparent source in the emergency department. Pediatr Infect Dis J. 2012;31:645–7.
Esposito S, Tagliabue C, Picciolli I, Semino M, Sabatini C, Consolo S, et al. Procalcitonin measurements for guiding antibiotic treatment in pediatric pneumonia. Respir Med. 2011;105:1939–45.
Goyal JP, Kumar P, Mukherjee A, Das RR, Bhat JI, Ratageri V, Vyas B, Lodha R, Acute Respiratory Infection Treatment Unit Study Group. Risk Factors for the Development of Pneumonia and Severe Pneumonia in Children. Indian Pediatr. 2021;58(11):1036–9.
Das RR, Satapathy AK, Mukherjee A, Goyal JP, Bhat JI, Ratageri VH, Vyas B, Lodha R, Members of The ATU (Acute Respiratory Infection Treatment Unit) Group. Role of Clinical Criteria and Oxygen Saturation Monitoring in Diagnosis of Childhood Pneumonia in Children Aged 2 to 59 Months. Indian Pediatr. 2021;58(11):1024–9.
Bhat JI, Charoo BA, Mukherjee A, Ahad R, Das RR, Goyal JP, Vyas B, Ratageri VH, Lodha R, Members of The ATU (Acute Respiratory Infection Treatment Unit) Group. Risk of hospitalization in under-five children with community-acquired pneumonia: a multicentric prospective cohort study. Indian Pediatr. 2021;58(11):1019–23.
Revised WHO classification and treatment of pneumonia in children at health facilities: evidence summaries. https://apps.who.int/iris/bitstream/handle/10665/137319/9789241507813_eng.pdf. Accessed 4 Mar 2022
Christ-Crain M, Müller B. Procalcitonin in bacterial infections–hype, hope, more or less? Swiss Med Wkly. 2005;135:451.
Christ-Crain M, Jaccard-Stolz D, Bingisser R, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet. 2004;363(9409):600–7.
Giulia B, Luisa A, Concetta S, Bruna LS, Chiara B, Marcello C. Procalcitonin and community-acquired pneumonia (CAP) in children. ClinicaChimica Acta. 2015;451:215–8.
Long B, Long D, Koyfman A. Emergency medicine evaluation of community-acquired pneumonia: history, examination, imaging and laboratory assessment, and risk scores. J Emerg Med. 2017;53:642–52.
Korppi M, Remes S, Heiskanen-Kosma T. Serum procalcitonin concentrations in bacterial pneumonia in children: a negative result in primary healthcare settings. Pediatr Pulmonol. 2003;35:56–61.
Baer G, Baumann P, Buettcher M, Heininger U, Berthet G, Schafer J, et al. Procalcitonin guidance to reduce antibiotic treatmentof lower respiratory tract infection in children and adolescents (ProPAED): a randomized controlled trial. PLoS ONE. 2013;8:e68419.
Huang DT, Yealy DM, Filbin MR, Brown AM, Chang CH, Doi Y, et al. ProACT Investigators. Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N Engl J Med. 2018;379:236–49.
Schuetz P, Wirz Y, Sager R, Christ-Crain M, Stolz D, Tamm M, et al. Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst Rev. 2017;10:CD007498.
Self WH, Balk RA, Grijalva CG, Williams DJ, Zhu Y, Anderson EJ, et al. Procalcitonin as a marker of etiology in adults hospitalized with community-acquired pneumonia. Clin Infect Dis. 2017;65:183.
Dudognon D, Levy C, Chalumeau M, Biscardi S, Dommergues MA, Dubos F, et al. Diagnostic Accuracy of Routinely Available Biomarkers to Predict Bacteremia in Children With Community-Acquired Pneumonia: A Secondary Analysis of the GPIP/ACTIV Pneumonia Study in France, 2009–2018. Front Pediatr. 2021;9:684628.
Don M, Valent F, Korppi M, Falleti E, De Candia A, Fasoli L, et al. Efficacy of serum procalcitonin in evaluating severity of community-acquired pneumonia in childhood. Scand J Infect Dis. 2007;39:129–37.
Yadav KK, Awasthi S, Takia L, Agarwal J, Agarwal GG. Procalcitonin and C-reactive protein in WHO defined severe and very severe community acquired pneumonia: A hospital based cross-sectional study. Clin Epidemiol Global Health. 2015;3(Suppl 1):S3–9.
Lee JY, Hwang SJ, Shim JW, Jung HL, Park MS, Woo HY, Shim JY. Clinical significance of serum procalcitonin in patients with community-acquired lobar pneumonia. Korean J Lab Med. 2010;30:406–13.
Fonseca TS, Gendrel D, Ruuskanen O, Nascimento-Carvalho CM. Pleural Effusion Increases Serum Procalcitonin Values in Children with Community-acquired Pneumonia. Pediatr Infect Dis J. 2015;34:914–5.
Chiu CY, Wong KS, Huang JL, Tasi MH, Lin TY, Hsieh SY. Proinflammatory cytokines, fibrinolytic systemenzymes, and biochemical indices in children with infectious para-pneumonic effusions. Pediatr Infect Dis J. 2008;27:699–703.
Acknowledgements
Mr Vikas Patwa ( NurseNurse AIIMS Jodhpur) , AIIMS Bhubaneswar Ms Jyotshnarani Sahoo, Ms Manaswini Biswal, KIMS Vedasree and Gayatri, Dr Prakash Wari ,HoDPediatrics, Director, Principal ,Medical superintendent ,KIMS,Hubballi, Umaisa Zehra (research nurse). Saba (data entry operator)
Accordance
I confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Funding
This work was supported by Bill and Melinda Gates Foundation through The INCLEN Trust International (Grant number: OPP1084307). The funding source had no contribution in study design, implementation, collection and interpretation of data and report writing.
Author information
Authors and Affiliations
Contributions
VR,AM,RL,SKK:Concept and designed the study, analysed data and drafted.PP,RRD,JPG,JIB,BV,KRJ;Collected the data,supervised at site,analysed and interpreted the data. DS,PK,KS,SM,BAC: Collected the data and helped in data analysis.All authors reviewed the systematic review and revised the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from Ethics Committee of KIMS,Hubballi and other five study sites. Written informed consent was obtained from legal guardians/parents of participants. A copy of consent form was given to parents/ guardian. Personal information (paper and electronic registers) were stored in an appropriate manner so as to ensure full confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ratageri, V.H., Panigatti, P., Mukherjee, A. et al. Role of procalcitonin in diagnosis of community acquired pneumonia in Children. BMC Pediatr 22, 217 (2022). https://doi.org/10.1186/s12887-022-03286-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03286-2