Abstract
Background
Glycogen storage disease type III (GSD III) is a rare autosomal recessive glycogenolysis disorder due to AGL gene variants, characterized by hepatomegaly, fasting hypoglycemia, hyperlipidemia, elevated hepatic transaminases, growth retardation, progressive myopathy, and cardiomyopathy. However, it is not easy to make a definite diagnosis in early stage of disease only based on the clinical phenotype and imageology due to its clinical heterogeneity.
Case presentation
We report a two-year-old girl with GSD III from a nonconsanguineous Chinese family, who presented with hepatomegaly, fasting hypoglycemia, hyperlipidemia, elevated levels of transaminases. Accordingly, Sanger sequencing, whole‑exome sequencing of family trios, and qRT-PCR was performed, which revealed that the patient carried the compound heterogeneous variants, a novel frameshift mutation c.597delG (p. Q199Hfs*2) and a novel large gene fragment deletion of the entire exon 13 in AGL gene. The deletion of AGL was inherited from the proband’s father and the c.597delG variant was from the mother.
Conclusions
In this study, we identified two novel variants c.597delG (p. Q199Hfs*2) and deletion of the entire exon 13 in AGL in a Chinese GSD III patient. We extend the mutation spectrum of AGL. We suggest that high-throughput sequencing technology can detect and screen pathogenic variant, which is a scientific basis about genetic counseling and clinical diagnosis.
Similar content being viewed by others
Background
Glycogen storage disease type III(GSDIII; OMIM #232,400)also known as “limit dextrinosis”, “Cori” or “Forbes” disease, which was discovered by Barbara Illingworth and Gerty Cori1 in 1952, is a rare autosomal recessive glycogenolysis disorder with an incidence of 1:100,000 [1, 2]. Owing to the pathogenic variations in amyl glucosidase (AGL) gene (MIM #610,860), the glycogen debranching enzyme (GDE) is genetic deficiency or reduced activity, causing an accumulation of limit dextrin-like molecules in the cytoplasm of hepatocytes, myocytes, and other tissues [3].
The AGL gene has been isolated on chromosome 1p21 since 1991, and has been known as 85 kb in length with 35 exons encoding a 1532 amino acids protein(GDE) [4]. There are three important domains in AGL, the putative transferase catalytic residues, the putative glucosidase catalytic residues and the putative glycogen-binding domain (Fig. 1) [5]. Therefore, variants in these regions are more likely to influence the normal structure and function of AGL, resulting in the occurrence of GSD III. Due to alternative exon splicing and differential transcription of AGL, it has fix-transcript isoforms [6]. Isoform 1(NM_000642) is the major isoform, which consists of 34 exons and widely expresses in liver, muscle, kidney, and lymphoblastoid cells [7]. GDE is a 175-kD monomeric protein containing two independent catalytic domains, amylo-1-6-glucosidase (EC 3.2.1.33) and 1,4-α-D-glucan 4-α-D-glycosyltransferase (EC 2.4.1.25). It catalyzes one of the last steps in the conversion of glycogen to glucose-1-phosphate, playing an indispensable role in the glycogen degradation [5]. To date, over 180 different AGL gene pathogenic variants have been reported worldwide (Clinvar accessed in May 2021), reflecting a high degree of genetic heterogeneity. Among these variants, the majorities are nonsense variants followed by frameshift, splice site, and missense variants (https://www.ncbi.nlm.nih.gov/clinvar).
Schematic representation of the AGL gene comprising 35 exons. The variants in this study are written with black color. Blue boxes stand for exons considered encoding the putative transferase catalytic residues. Orange boxes stand for exons considered encoding the putative glucosidase catalytic residues and green ones stand for exons considered encoding putative glycogen-binding domain
Individuals with GSD III are characterized by progressive myopathy and liver disease. Based on differences in tissue expression level of the GDE, there are four subtypes of GSD, including GSD IIIa, IIIb, IIIc and IIId [8, 9]. GSD IIIa is the most common subtype, accounting for about 85% [3]. It mainly affects liver, skeletal, and cardiac muscle. Patients with GSD IIIb, which affects only the liver and account for about 15% of all GSD III patients [10]. It has been confirmed that selective loss of glucosidase activity or transferase activity is the pathogenic mechanism of GSD IIIc and GSD IIId, respectively [11]. Both GSD IIIc and GSD IIId are extremely rare. GSD III is usually developing in infancy and early childhood, presenting as hepatomegaly, growth retardation, fasting hypoglycemia, hyperlipidemia, elevated hepatic transaminases, progressive myopathy and cardiomyopathy [12, 13]. The hepatomegaly may disappear in adolescence and adulthood. Meanwhile, in patients without cirrhosis or myopathy, all symptoms usually improve during adolescence [14]. Muscle weakness is a slow progress, typically becoming prominent in the third to fourth decade [15]. Another common associated symptom is hypertrophic cardiomyopathy, which usually develops between most of the children with GSD IIIa. The clinical presentation is heterogeneous, ranging from asymptomatic to severe cardiac dysfunction, such as congestive heart failure and sudden death [16].
Here, we reported a patient whose clinical diagnosis was considered as glycogen storage disease III. Whole exome sequencing (WES), Sanger sequencing, and quantitative real time polymerase chain reaction (qRT-PCR) was performed on the proband and her parents to make an accurate diagnosis. Our findings provide a wider range of AGL gene variants spectrum in patients with GSD III in the Chinese population.
Case presentation
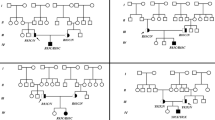
A two-old-girl was admitted to Tianjin Children’s Hospital due to progressive enlargement of the abdomen resulting from hepatomegaly. The parents of the patient are non-consanguineous. The pedigree of the family is depicted in Fig. 2. Laboratory examinations revealed nocturnal fasting hypoglycemia, hyperlipidemia, significantly elevated levels of transaminases. Hepatomegaly was confirmed with abdominal ultrasound and abdominal computed tomography enhanced scan. These clinical phenotypes suggested GSD III. However, electromyography excluded myopathy, cardiomyopathy was ruled out by electrocardiogram and echocardiography, and physical examination showed no obvious growth retardation.
Pedigree of the GSD III family with the variants of exon 5 and exon 13. Here, the circles indicate female individuals and rectangles indicate males. The patient of the study is indicated by a black circle. The patient (II-2) contains two variations in AGL gene, the c.597delG(p.Q199Hfs※2)in exon 5 is inherited from the mother (I-2) and the deletion of exon 13 is inherited from the father(I-1)
Biochemical, imaging, clinical and diet therapy data at baseline, 8 days and 20 days are shown in Table 1.
To make a definite diagnosis, the peripheral blood of the patient and parents were sent to MyGenostics company (Beijing, China) for whole-exome sequencing (WES), Sanger sequencing, and qRT-PCR. Genetic analysis revealed a biallelic novel pathogenic variants in AGL gene. Sanger sequencing identified a previously unreported heterozygous variant in exon 5 of the AGL gene: c.597delG (p. Q199Hfs*2) (NM_000642), which inherited from the mother (I-2) (Fig. 3). This variant causes the glutamine at position 199 is changed to histidine, leading to the insertion of a stop codon at position 200. Furthermore, the heterozygous deletion of exon 13 found by WES was also a previously unreported variant, which inherited from the father(I-1). The results of qRT-PCR showed that the relative copy number of exon 13 in the control and the patient’s mother were normal, while the proband and his father were half of the normal, confirming the absence of exon 13 (Fig. 4). The deletion of exon 13 causes deletions of amino acid from position 538 to 578, leading to the termination transcription at the 540th amino acid. Both variants could cause the early termination of gene transcription. The patient (II-2) inherited both variants and was therefore a compound heterozygote. The sister (II-1) had no symptoms of GSD III, who did not performed WES.
Gene deletion and duplication analysis map. A Multiplex Ligation-dependent Probe Amplification (MLPA) of the patient and her parents; B shows qRT-PCR results of exon 13 in AGL gene: the relative copy number in the control and the patient’s mother was normal, and the proband and his father were half of the normal; C shows qRT-PCR results of exon 9: the relative copy number in four groups were normal. All these indicates the proband has a heterozygous deletion in AGL gene (exon13), and shows the deletion was inherited from the proband’s father. The Red circle shows the region of fragment deletion, ** means P < 0.01, ‘ns’ means P > 0.05
Discussion and conclusions
In our study, we reported a two-year-old girl (Fig. 2, II-2) from the region of China. She came to hospital for treatment mainly because of hepatomegaly. All examinations performed that she had hepatomegaly, nocturnal fasting hypoglycemia, hyperlipidemia, significantly elevated levels of transaminases, and midface hypoplasia with a depressed nasal bridge. However, she did not have any symptoms or exam evidence of myopathy or cardiomyopathy.
The cardinal clinical features of GSD III are hepatomegaly, fasting hypoglycemia, elevated serum concentrations of transaminases and CK [17]. The diagnosis is established by identification of biallelic pathogenic variants in AGL gene using molecular genetic testing such as single-gene testing or whole exome sequencing [18]. Liver or muscle biopsy can certify deficient glycogen debranching enzyme activity and accumulation of limit dextrin-like molecules in either liver or muscle biopsy specimen, so they are always used to distinguish different subtypes [19]. However, biopsy is more invasiveness and not required to make the diagnosis of GSD III, it is rarely performed. In our case, due to the typical clinical symptoms, the patient shown high clinical suspicion of GSD III. To make clear diagnosis, we performed genetic analysis technology on the proband and her parents. The result laid out that the proband had a biallelic likely pathogenicity variants in AGL gene. Thus, the patient was diagnosed as GSD III.
Unfortunately, due to the invasive of biopsy the patient’s family disagreed with the operation, and no further detection of liver or muscle branch enzyme activity was carried out. Hence, the clinical subtype of the patient could not be confirmed. Since there was no obvious growth retardation in the patient, no further evaluation was undertaken, such as imaging examination of the skeletal system, etc. Therefore, follow-up in the later stage is very necessary.
To date, there are over 180 different AGL gene pathogenic variants registered in the Clinvar database (https://www.ncbi.nlm.nih.gov/clinvar). It includes all variant types: missense, nonsense, splice site, frameshift, and large gene fragment deletions and duplications. The majorities are frameshift (39.0%), nonsense (36.2%), and splice-site (10.4%) variants. Depending on ethnic groups, the prevalent mutations of AGL vary in GSD III. Information on the spectrum of AGL variants will improve molecular diagnosis of GSD III in these populations and genetic counseling. For example, the most frequent variant among Italian patients is splice-site variant (c.2681 + 1G > A), the common nonsense variant in the Faroe Islands is p.R408X, and the prevalent variants in the United States are p.R864X and c.3964delT [20]. In Asian, c.1735 + 1G > T shows the highest frequency in Japanese, Korean and Chinese patients [20]. The common variant in Turkish patients is p. W1327X [21]. Despite these, there is still high heterogeneity of AGL variants worldwide and pathogenic variants scattered throughout the gene [22]. In our case, the patient carries two compound-heterozygous variants (c.597delG and deletion of exon 13) in AGL. According to the ACMG standards and guidelines for the interpretation of sequence variants [23], the maternal frameshift variant c.597delG is a 1 bp deletion encompassed in exon 5, which causes a shift in the open reading frame and insertion of a premature termination codon (p. Q199Hfs*2), resulting in a truncating protein. This will lead to the loss of protein function and the occurrence of GSD III (PVS1). The variant is absent from controls in Exome Sequencing Project, 1000 Genomes or ExAC (PM2). Therefore, variant c.597delG is considered a likely pathogenic variant. Otherwise, the large gene fragment deletion in AGL gene with a paternal origin is a 124 bp deletion of the entire exon 13. It results in a premature truncation of the protein, leading to the loss of protein function (PVS1). The variant is absent from controls in Exome Sequencing Project, 1000 Genomes or ExAC (PM2). Thus, variant deletion of exon 13 is classified as likely pathogenic variant of AGL. Those two variants are novel and no registered in the Clinvar or the HGMD. The patient was diagnosed with GSD III according to the typical clinical features of liver disease hepatomegaly, nocturnal fasting hypoglycemia, hyperlipidemia, significantly elevated levels of transaminases. Those are consistent with the result of genetic analysis a biallelic novel pathogenic variants in AGL gene.
There is poor correlation between the genotype and phenotype of GSD III. Moderate to severe disease (GSD IIIa) associated with homozygosity for loss of function variants [24]. Frameshift, nonsense, and splices site variants are possible significant association with elevated CK and TC, suggesting that these variants were associated with severe phenotype [5, 20]. To evaluate genotype–phenotype relationships in GSD III with similar milder phenotype, we compared clinical features among patients with AGL-variants published to date (Table 2). In earlier reports, variants of exon 3, such as c.16 C > T and c.18_19delGA, along with a second mutation elsewhere in the AGL gene were reported to be associated with GSD IIIb [9]. This is consistent with our observation [24,25,26,27]. Otherwise, we observed milder phenotype has been found to be associated with IVS32–12 A > G homozygosity variant in intron 32 of the AGL gene [28, 29]. As is evident from Table 2, typical clinical features of mild GSD III are liver disease hepatomegaly, fasting hypoglycemia, hyperlipidemia, significantly elevated levels of transaminases, with or without elevated serum concentrations of CK. The increased serum CK is a suggestive and nonspecific marker of muscle breakdown. There are correlations between premature termination codon (PTC) variants and elevated serum CK value. Otherwise, the missense and small in-frame deletion mutations are associated with a normal serum CK level in GSD III [20]. However skeletal muscle and cardiologic complications were usually minimal during childhood, progressive myopathy can develop after the third or fourth decade of life [30]. In our study, the patient manifests as liver damage, and has no evidence for myopathy or cardiomyopathy up to now, which may associate with the age at diagnosis, disease classification or heterozygous variants of AGL. We considerate the patient probably GSD IIIb (though not confirmed) as clinical and biochemical data of the patient presented here rule out muscular manifestations. So, if there is no muscle damage in the patient during the late follow-up or confirmed by muscle biopsy as GSD IIIb, our report and the previous report [29] provide evidence that variants in exons other than exon 3 could be responsible for the GSD IIIb phenotype. Hyperlipidemia may relate to frameshift variant (c.597delG). Although previous reports suggest that PTC is associated with elevated levels of serum CK, our study shows a normal serum CK level, which may due to the patient’s age or measurement in resting state [7]. These differences indicate the vary widely heterogeneity of phenotype. The follow-up date and further research is needed to clarify the relationship between PTC and CK. It also helps to understand the disease development and guide treatment in the future.
The treatment of GSD III is still controversial, and the recognized mainstay treatment is dietary management to maintain euglycemia, including uncooked cornstarch therapy with a nocturnal high-protein supplementation [33]. Recently, high fat diet has been confirmed a benefit effect to the progress of cardiomyopathy and myopathy [34]. In the past few years, significant progress has been made in gene therapy, which is expected to be more effective in the future for the treatment with GSD III [35]. In this research, the patient was treated with uncooked cornstarch 1-2 g/kg/d after being diagnosed with GSD III 8 days later. After a period of dietary control, her nocturnal fasting blood glucose returned to normal. 20 days after admission, compared to the situation at the time of admission, there was no retraction in the size of the liver by abdominal ultrasonography, but the transaminase decreased.
In summary, we identified two novel variants c.597delG (p. Q199Hfs*2) and deletion of the entire exon 13 in AGL in a Chinese GSD III patient. We extend the mutation spectrum of AGL in Chinese patients with GSD III and point out to the heterogenous genetic background of the disease, providing theoretical guidance for genetic counseling and precision therapy. Our results suggest the need for complete AGL gene sequencing to diagnose the disease based on a suggestive clinical feature and provide genetic counseling for young families. However, it is limited to hypothesize on the correlation between genotype and phenotype just based on this patient only. In the future, we will continue to collect cases for cohort studies in order to expand the basic information of the disease and establish genotype-phenotype correlation.
Availability of data and materials
The raw datasets used and analysed during the current study are not deposited in publicly available repositories because of considerations about the privacy or security of human. However, the datasets can be available from the corresponding author on reasonable request.
Abbreviations
- ALG :
-
Amyl glucosidase gene
- GSDIII:
-
Glycogen storage disease type III
- GDE:
-
Glycogen debranching enzyme
- WES:
-
Whole exome sequencing
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CK:
-
Creatine kinase
- PTC:
-
Premature termination codon
References
Kishnani PS, Austin SL, Arn P, Bali DS, Boney A, Case LE, Chung WK, Desai DM, El-Gharbawy A, Haller R, et al. Glycogen storage disease type III diagnosis and management guidelines. Genet Med. 2010;12(7):446–63.
Dagli A, Sentner CP, Weinstein DA. Glycogen Storage Disease Type III. In: GeneReviews(®). edn. Edited by Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, Amemiya A. Seattle (WA): University of Washington, Seattle Copyright © 1993–2020, University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved.; 1993.
Sentner CP, Hoogeveen IJ, Weinstein DA, Santer R, Murphy E, McKiernan PJ, Steuerwald U, Beauchamp NJ, Taybert J, Laforet P, et al. Glycogen storage disease type III: diagnosis, genotype, management, clinical course and outcome. J Inherit Metab Dis. 2016;39(5):697–704.
Bao Y, Dawson TL Jr, Chen YT. Human glycogen debranching enzyme gene (AGL): complete structural organization and characterization of the 5’ flanking region. Genomics. 1996;38(2):155–65.
Perveen S, Gupta N, Kumar M, Kaur P, Chowdhury MR, Kabra M. Spectrum of amyloglucosidase mutations in Asian Indian patients with Glycogen storage disease type III. Am J Med Genet A. 2020;182(5):1190–200.
Shen JJ, Chen YT. Molecular characterization of glycogen storage disease type III. Curr Mol Med. 2002;2(2):167–75.
Dagli ASC, Weinstein DA. Glycogen Storage Disease Type III. 2010 Mar 9 [Updated 2016 Dec 29]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK26372/: Glycogen Storage Disease Type III.
Endo Y, Horinishi A, Vorgerd M, Aoyama Y, Ebara T, Murase T, Odawara M, Podskarbi T, Shin YS, Okubo M. Molecular analysis of the AGL gene: heterogeneity of mutations in patients with glycogen storage disease type III from Germany, Canada, Afghanistan, Iran, and Turkey. J Hum Genet. 2006;51(11):958–63.
Goldstein JL, Austin SL, Boyette K, Kanaly A, Veerapandiyan A, Rehder C, Kishnani PS, Bali DS. Molecular analysis of the AGL gene: identification of 25 novel mutations and evidence of genetic heterogeneity in patients with Glycogen Storage Disease Type III. Genet Med. 2010;12(7):424–30.
Zobeiri M. Liver Transplantation in a Myopathic Patient with Glycogen Storage Disease Type IIIa and Decompensated Cirrhosis. Int J Organ Transplant Med. 2017;8(4):217–20.
Ozen H. Glycogen storage diseases: new perspectives. World J Gastroenterol. 2007;13(18):2541–53.
Verbeek RJ, Sentner CP, Smit GP, Maurits NM, Derks TG, van der Hoeven JH, Sival DA. Muscle Ultrasound in Patients with Glycogen Storage Disease Types I and III. Ultrasound Med Biol. 2016;42(1):133–42.
Elpeleg ON. The molecular background of glycogen metabolism disorders. J Pediatr Endocrinol Metab. 1999;12(3):363–79.
Halaby CA, Young SP, Austin S, Stefanescu E, Bali D, Clinton LK, Smith B, Pendyal S, Upadia J, Schooler GR, et al. Liver fibrosis during clinical ascertainment of glycogen storage disease type III: a need for improved and systematic monitoring. Genet Med. 2019;21(12):2686–94.
Lucchiari S, Santoro D, Pagliarani S, Comi GP. Clinical, biochemical and genetic features of glycogen debranching enzyme deficiency. Acta Myol. 2007;26(1):72–4.
Austin SL, Proia AD, Spencer-Manzon MJ, Butany J, Wechsler SB, Kishnani PS. Cardiac Pathology in Glycogen Storage Disease Type III. JIMD Rep. 2012;6:65–72.
Seigel J, Weinstein DA, Hillman R, Colbert B, Matthews B, Bachrach B. Glycogen Storage Disease Type Ilia Presenting as Non-Ketotic Hypoglycemia: Use of a Newly Approved Commercially Available Mutation Analysis to Non-Invasively Confirm the Diagnosis. J Pediatr Endocrinol Metab. 2020;21(6):587–90.
Burda P, Hochuli M. Hepatic glycogen storage disorders: what have we learned in recent years? Curr Opin Clin Nutr Metab Care. 2015;18(4):415–21.
Bao Y, Yang BZ, Dawson TL Jr, Chen YT. Isolation and nucleotide sequence of human liver glycogen debranching enzyme mRNA: identification of multiple tissue-specific isoforms. Gene. 1997;197(1–2):389–98.
Lu C, Qiu Z, Sun M, Wang W, Wei M, Zhang X. Spectrum of AGL mutations in Chinese patients with glycogen storage disease type III: identification of 31 novel mutations. J Hum Genet. 2016;61(7):641–5.
Çakar NE, Gezdirici A, Topuz H, Önal H. Novel variants in Turkish patients with glycogen storage disease. Pediatr Int. 2020;62(10):1145–50.
Berling É, Laforêt P, Wahbi K, Labrune P, Petit F, Ronzitti G, O'Brien A. Narrative review of glycogen storage disorder type III with a focus on neuromuscular, cardiac and therapeutic aspects. J Inherit Metab Dis. 2021;44(3):521–33.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24.
Crushell E, Treacy EP, Dawe J, Durkie M, Beauchamp NJ. Glycogen storage disease type III in the Irish population. J Inherit Metab Dis. 2010;33(Suppl 3):215–8.
Lee TM, Berman-Rosenzweig ES, Slonim AE, Chung WK. Two Cases of Pulmonary Hypertension Associated with Type III Glycogen Storage Disease. JIMD Rep. 2011;1:79–82.
Sentner CP, Vos YJ, Niezen-Koning KN, Mol B, Smit GP. Mutation Analysis in Glycogen Storage Disease Type III Patients in the Netherlands: Novel Genotype-Phenotype Relationships and Five Novel Mutations in the AGL Gene. JIMD Rep. 2013;7:19–26.
Oterdoom LH, Verweij KE, Biermann K, Langeveld M, van Buuren HR. Hepatocellular Adenomas and Carcinoma in Asymptomatic, Non-Cirrhotic Type III Glycogen Storage Disease. J Gastrointestin Liver Dis. 2015;24(4):515–8.
Mili A, Ben Charfeddine I, Mamaï O, Abdelhak S, Adala L, Amara A, Pagliarani S, Lucchiarri S, Ayadi A, Tebib N, et al. Molecular and biochemical characterization of Tunisian patients with glycogen storage disease type III. J Hum Genet. 2012;57(3):170–5.
Basit S, Malibari O, Al Balwi AM, Abdusamad F, Abu Ismail F. A founder splice site mutation underlies glycogen storage disease type 3 in consanguineous Saudi families. Ann Saudi Med. 2014;34(5):390–5.
Ko JS, Moon JS, Seo JK, Yang HR, Chang JY, Park SS. A mutation analysis of the AGL gene in Korean patients with glycogen storage disease type III. J Hum Genet. 2014;59(1):42–5.
Minen F, Cont G, De Cunto A, Martelossi S, Ventura A, Maggiore G, et al. Delayed diagnosis of glycogen storage disease type III. J Pediatr Gastroenterol Nutr. 2012;54(1):122-4.
Ben Rhouma F, Azzouz H, Petit FM, Khelifa MB, Chehida AB, Nasrallah F, et al. Molecular and biochemical characterization of a novel intronic single point mutation in a Tunisian family with glycogen storage disease type III. Mol Biol Rep. 2013;40(7):4197–202.
Dagli AI, Zori RT, McCune H, Ivsic T, Maisenbacher MK, Weinstein DA. Reversal of glycogen storage disease type IIIa-related cardiomyopathy with modification of diet. J Inherit Metab Dis. 2009;32(Suppl 1):103–6.
Rossi A, Hoogeveen IJ, Bastek VB, de Boer F, Montanari C, Meyer U, Maiorana A, Bordugo A, Dianin A, Campana C, et al. Dietary lipids in glycogen storage disease type III: A systematic literature study, case studies, and future recommendations. J Inherit Metab Dis. 2020;43(4):770–7.
Kishnani PS, Sun B, Koeberl DD. Gene therapy for glycogen storage diseases. Hum Mol Genet. 2019;28(R1):R31–41.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National Natural Science Foundation of China (grant number 81771589), the Project of Tianjin Health Science and Technology (grant number ZC20120), and the Public Health and Technology project of Tianjin (grant number TJWJ2021ZD007). These fundings had an important role in the collection, analysis and interpretation of genetic data, but it did not have any role in the design of the study and writing the manuscript.
Author information
Authors and Affiliations
Contributions
J W was involved in the collection and critical analysis of clinical data. YP Y drafted of the manuscript. CQ C contributed to the designing the study, supervision, and critical review of the manuscript. XF Z and Y Z contributed to the supervision and critical analysis of laboratory data, including the interpretation of NGS results. Y Z and JB S confirmed the authenticity of all the raw data and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient (or the parent) and the study was approved by the ethics committee of Tianjin Children’s Hospital (Tianjin, China).
Consent for publication
Written informed consent was obtained from the patient’s parents for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal. Written informed consent was obtained from the patient’s parents for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, J., Yu, Y., Cai, C. et al. The biallelic novel pathogenic variants in AGL gene in a chinese patient with glycogen storage disease type III. BMC Pediatr 22, 284 (2022). https://doi.org/10.1186/s12887-022-03252-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03252-y