Abstract
Background
The purpose of this project was to improve perinatal survival by introducing Moyo Fetal Heart Rate (FHR) Monitor coupled with neonatal resuscitation simulation training.
Methods
The implementation was done at three district hospitals. We assessed health care workers’ (HCW’s) skills and perinatal death trends during implementation. Baseline data were collected from the hospitals before implementation. Newborn resuscitation (NR) skills were assessed before and after simulation training. Assessment of perinatal outcomes was done over 2 years of implementation. We used descriptive analysis; a t-test (paired and independent two-sample) and a one-way Anova test to report the findings.
Results
A total of 107 HCW’s were trained on FHR monitoring using Moyo and NR knowledge and skills using NeoNatalie simulators. The knowledge increased post-training by 13.6% (p < 0.001). Skills score was increased by 25.5 and 38.2% for OSCE A and B respectively (p < 0.001). The overall fresh stillbirths rate dropped from 9 to 5 deaths per 1000 total births and early neonatal deaths at 7 days from 5 to 3 (p < 0.05) deaths per 1000 live births over 2 years of implementation.
Conclusion
There was a significant improvement of newborn resuscitation skills among HCW’s and neonatal survival at 2 years. Newborn resuscitation training coupling with Moyo FHR monitor has shown potential for improving perinatal survival. However, further evaluation is needed to explore the full potential of the package.
Similar content being viewed by others
Background
Perinatal deaths refer to a combination of fetal deaths (after 28 weeks) and live births with only brief survival (1 week) and are grouped on the assumption that similar factors are associated with these losses [1]. The majority of perinatal deaths occur in low-resource settings. A Meta-analysis study of demographic health surveys showed a perinatal mortality rate (PMR) of 34.7 across 21 countries in sub-Saharan Africa. In this analysis, the highest PMR was observed in Tanzania (39.5) [2].
In a hospital-based survey in Tanzania (2006–2015), neonatal mortality rates were reported to be increasing from 2.6 to 10.4 deaths per 1000 live births. Early neonates contributed 90% to these death rates constantly over time. In this survey, the leading cause of early neonatal deaths was birth asphyxia [3]. A facility-based case-control study in Zanzibar reported 59 stillbirths per 1000 total births, in which 52% had fetal heart rate (FHR) at admission [4].
Poor quality of intrapartum care contributes to perinatal mortality. An increased risk of intrapartum stillbirth when FHR is inadequately monitored is evident [5]. It is further reported that a shortage of FHR measurement devices is a barrier to FHR monitoring standards [6]. For the FHR monitoring to be effective, the device used must be reliable and convenient for both the HCW’ and pregnant women in labor. In high resource settings, FHR during labor is mostly monitored continuously using cardiotocography (CTG). In Tanzania, FHR is monitored intermittently mostly using Pinard fetoscope at lower health facilities or rarely by handheld Dopplers.
Doppler fetal monitors are becoming widely available and used in clinical practice in low-resource settings. These monitors use ultrasound technology to detect fetal heartbeats as early as 12 weeks [7]. One advantage of the Doppler fetal monitor is the electronic audio output, which allows users and laboring women to hear the fetal heartbeat. However, the dopplers carry some disadvantages including high cost, source of costly power (battery or electricity), and the need for technical maintenance. With further technological development, Doppler remains an important tool for the assessment of fetal well-being globally [7].
A recent systematic review study has shown that Doppler is superior at detecting abnormal intrapartum FHR compared to Pinard [8]. This review further shows that using Doppler on admission helps to accurately measure fetal deaths occurring after facility admission [8]. Trials conducted at referral teaching hospitals in Tanzania comparing the effectiveness of a novel Doppler FHR monitor (Moyo) compared with Pinard and classic Doppler have shown that Moyo is effective in detecting abnormal FHR [9, 10].
Moyo is a strap-on automatic multicrystal Doppler device (named Moyo, Laerdal Global Health) that has been recently introduced into clinical practice. Moyo is designed for both intermittent and continuous FHR monitoring. With a 9-crystal sensor, Moyo can accurately detect FHR within 5 s and can differentiate maternal and fetal heart rates. Moyo has 30 min histogram display of FHR trends which can be reviewed by the HCW to assess FHR. The device has an inbuilt audio-visual alarm if abnormal FHR is detected. Moyo is lightweight and portable and thus can allow a laboring woman to move around and choose the birth position.
Apart from the use of innovative devices, strengthening the knowledge and skills of health care workers (HCWs) to provide neonatal resuscitation (NR) is critical to reducing perinatal morbidity and mortality. American Academy of Pediatrics and its global partners created the Helping Babies Breathe (HBB) program, which teaches basic NR techniques to birth attendants in low-resource settings (LRSs).
Systematic reviews have demonstrated significant improvement of HCW’s knowledge and skills after HBB simulation training [11]. However, it has been observed generally that the knowledge and skills gained fall off after initial training [12]. This is a barrier to HBB’s success. To improve skills retention among HCWs, several different HBB training approaches have been recommended [13,14,15].
The impact of HBB on perinatal outcomes has been evaluated with conflicting results. A pilot HBB study in eight hospitals in Tanzania between 2009 and 2011 resulted in a 47% reduction in hospital-based neonatal mortality within 24 h [16]. Several other studies in resource-limited settings have reported a positive impact of HBB training on intrapartum and early neonatal deaths. A study by KC et al. showed a change in intrapartum-related stillbirths from 9.0 to 3.2/1000 births after HBB implementation [17]. A systematic review study further showed the strongest decline in intrapartum-related stillbirths and one-day newborn deaths after HBB training [18]. However, frequent HBB training is necessary to sustain the impact on mortality. Mduma et al. showed significantly improved perinatal survival over 6 years of implementing low dose high frequency (LDHF) training of HBB [19].
Most countries in LRSs including Tanzania are far away from the recommended Sustainable Development Goals (SDGs) targets of 12 stillbirths per 1000 total births and 12 neonatal deaths per 1000 livebirths [20]. To reduce these deaths, there is an urgent need to develop and introduce tools/technologies and scale up these innovations to reach lower-level health facilities.
Beyond research to perinatal care improvement project was implemented to introduce Moyo Doppler device for FHR monitoring coupled with simulation HBB training at three district hospitals in northern Tanzania. This study aimed to assess the contribution of the project on HCW’s HBB skills and perinatal mortality over 2 years of implementation.
Materials and methods
Beyond research to perinatal care improvement project was implemented at three district hospitals namely Mbulu, Babati, and Hanang in northern Tanzania. The rate of perinatal mortality in northern Tanzania was 32 per 1000 pregnancies as per the last Demographic Health Survey (DHS) [21].
The district hospitals provide comprehensive emergency obstetric and newborn care services. They attend pregnant women direct from home and as referrals from dispensaries and health centers in the surrounding area. They refer complicated cases of pregnant women and newborns to referral hospitals in the surrounding.
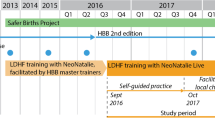
Haydom Lutheran Hospital was involved in the national HBB pilot project 2009, national HBB rollout program 2013–2015, and Moyo innovation (Safer Births sub-project) 2017. The hospital benefited in terms of staff capacity building including master trainers in HBB and FHR monitoring using Moyo Doppler. This project technical team comprised of an obstetrician, pediatrician, and four Moyo and HBB master trainer midwives experienced in labor care practices and use of Moyo devices.
The master trainers conducted a trainer of trainees (TOTs) course, four participants from each district hospital were involved. The TOTs training lasted for 2 days at HLH (1 day for HBB and 1 day for Moyo). The approach was hands-on, using a NeoNatalie simulator and upright bag-mask ventilator for HBB training. We further trained them on the use of Moyo for FHR monitoring and interpretation.
TOTs training was followed by training nurses/midwives and doctors working at maternity and theatre units of respective hospitals. The training was done at each district hospital setting by master trainers together with TOTs. HBB knowledge and skills for each participant were assessed by administering knowledge check questions and objective structured clinical evaluations (OSCE). This was done before and after training sessions. We used knowledge check questions, OSCE A and B available in HBB educational materials. We decided to use these evaluation tools because they have been validated and used elsewhere and they can be reproduced. Evaluations were supervised by the same master trainers in all training sessions.
Skills trained and evaluated include newborn assessment, drying, suction, stimulation, and bag-mask ventilation. We used curriculum and standard educational materials for HBB training as developed by the American Academy of Pediatrics (Second edition, English version). Participants were further trained on FHR monitoring, intermittent and continuous using the Moyo device. We used local guidelines that FHR to be reviewed every 30 min in the first stage and every 15 min in the second stage of labor and interpreted as normal when the rate is 110–160 and abnormal when the rate is below 110 or above 160 beats per minute.
After the training, facilities were provided with Moyo Doppler devices, NeoNataliae simulators, and upright bag-mask ventilators for self-practice and clinical care. Laerdal Foundation supported the project with training materials-Moyo Doppler, NeoNataliae simulators, upright bag-mask ventilators, and Penguin suction. Apart from the TOTs supervising ongoing practices at the hospitals to maintain and sustain skills, there were no other quality improvement activities related to maternal and newborn health at the district hospitals.
We hypothesized that the HBB skills score of the HCW’s at district hospitals before the training was 65%. We planned to increase the skills score to 90% after the training. To achieve that we needed to train 102 HCW’s in all three district hospitals. To increase the strength of the study we added 20%, therefore 120 HCW’s were planned to be trained.
Training data was obtained by recording test scores before and after training sessions. To obtain data on clinical outcome assessment, we collected baseline information from the district hospitals for the year 2017 before we implemented the project in 2018 and 2019. Data on total deliveries, live births, fresh stillbirths, and early neonatal deaths were gathered from each hospital. After 2 years of implementation, we collected the same clinical data from the same source. The main source of clinical outcomes data was District Health Information Software (DHIS2). The DHIS2 compiles and presents electronic routine health services information collected through the Health Management Information System.
Information from DHIS2 was collected using a structured data collection form. To ensure data quality, validation of data was done by an investigator in cooperation with data focal persons at the district hospitals. Double data entry was performed by the data clerk and discrepancies were resolved.
Data analysis was performed using R 3.6.2(Foundation for Statistical Computing, Vienna, Austria). We used descriptive analysis (mean, standard deviation, count, and percent), paired t-test was used to assess the significant differences between the overall mean scores of pre-tests and post-test of each skills question and knowledge. An Independent two-sample t-test was used to assess the significant differences of skills gained among the binary demographic variables. One-way analysis of variance was used to assess the comparison of skills and knowledge gain among the demographic variable with multiple levels and significant differences between perinatal outcomes among the years before and during implementation. Tukey honest significant differences were used as a post hoc test for comparing significant differences between the means of the levels of a factor. The level of significance was set at 0.05.
Results
A total of 107 HCWs were trained on FHR monitoring using Moyo Doppler and HBB using NeoNatalie simulators. The distribution of HCWs was highest in Babati hospital (40%) and lowest in Mbulu hospital (27%). More than two-thirds were female and about three quarter were nurses. About 60% had age below 40 years and half of them had less than 10 years of working experience (Table 1).
HBB skills were assessed using OSCE tests pre-and post-training. Skill gain was 25.5 and 38.2% for OSCE A and B respectively with significant differences between pre-test and post-test scores. Significant differences in skills gained were only observed between the sites in OSCE B, where Hanang was observed to have a high level of skills gained about 50.9% and Babati was observed to have a low level of skills gain of 31.6% (Table 2).
An average score of knowledge gain was 13.6%, with a significant difference between pre-test score and post-test score, where the highest average score of knowledge gain was observed Babati with 15.9% and Hanang had the lowest score gained 10.3% with no significant difference between sites (Table 2).
An overall FSB rate was around 9 cases per 1000 births in 2017 and dropped to 5 cases per 1000 births in 2019, where the rates vary from site to site. The early neonatal death rate within 24 h and 7 days has dropped from 4 cases and 5 cases per 1000 live births respectively in 2017 to 2 cases and 3 cases per 1000 live births in 2019 (Table 3).
The significant differences between the average rates of perinatal mortality among the years before and during the implementation were observed on early neonatal death at 24 h and 7 days, where the year 2019 had a lower early neonatal death rate compared to the year 2017 and their comparison is significant (Table 4).
Generally, the perinatal outcomes (FSB and neonatal death within 7 days) seem to be decreasing over implementation years, though in some of the sites the decline is not smooth. For FSB, Hanang was observed to have high FSB in all years compared to other sites, whereas small differences were observed in early neonatal death rates at 7 days between the sites among all years (Fig. 1).
Discussion
In this project, we were able to increase NR skills significantly through simulation training of HCWs and introduce novel FHR monitoring Doppler at district hospitals. The availability of essential medical devices and strategic training of HCWs is central to reducing perinatal morbidity and mortality. In LRSs, innovative medical devices are rarely available at lower health facilities, including the Moyo Doppler device for FHR monitoring. In this project, we rolled out this innovative device coupled with HBB training. Previous studies have demonstrated the effectiveness of this device in FHR monitoring [9, 10] and its acceptability among midwives and laboring women [22]. To our understanding, this is the first scale-up project to roll out an innovative novel FHR monitor (Moyo) coupled with HBB training at lower health facilities in Tanzania.
Training on maternal and newborn HCW’s is a crucial intervention to improve perinatal survival. This project has achieved significant HBB knowledge and skills gain after the training by 13 and 31% respectively. The difference of gain in knowledge and skills might be explained by the fact that the majority of participants were nurses from the labor ward who have experience with NR skills in their routine work hence easy to learn skills during the training.
This achievement is consistent with what has been reported in other studies underlining that HBB increased the acquisition rate of knowledge and skills of basic NR [11]. The nature of HBB simulation training – curriculum design, educational materials, and experienced master trainers may have contributed to the gained knowledge and skills. The acquired HBB knowledge and skills serve as important professional capacity building among involved health care workers to improve perinatal care.
The scale-up of Moyo coupled with HBB through this project was associated with improvement in clinical outcomes. The data indicates the reduction of stillbirths, 24 h and 7 days neonatal deaths. Previous studies using Moyo alone didn’t show a reduction in perinatal deaths as they were not coupled with newborn resuscitation training. In this study, FHRs of women who are in active labor was monitored using Moyo regardless of risk status. FHR monitoring followed the local guideline of measuring FHR after every 30 min for the first stage of labor and every 15 min for the second stage of labor for low-risk labors. For high-risk labors, Moyo was strapped on and FHR monitored continuously throughout.
Moyo Doppler has been reported to increase detection of abnormal FHR, which is a predictor of perinatal death. The risk of stillbirth is likely to decline when detection of abnormal FHR is coupled with recommended interventions such as intrauterine resuscitation or emergency delivery. The involved district hospitals are capable of providing emergency delivery services in case abnormal FHR is detected. Hence, proper utilization of the newly introduced device is probably going to further improve the birth outcomes.
Results of innovations in health services have a greater and more rapid impact on improving health when scaled up to reach facilities and communities. In addition, sustainability and local ownership are key principles of scale-up success [23]. In this project, local Trainers of Trainees (TOTs) were trained to support the use of Moyo for FHR monitoring and ongoing HBB practices at the facilities to sustain knowledge and skills. Materials for training and clinical care use were supplied to respective hospitals.
Addressing the perinatal death challenge by combining innovative tools (Moyo Doppler) and training modality (simulation) is the main strength of this project. Limitations include few HCWs with previous HBB training, this might have affected training skills scores. Some trained HCWs were shifted to other departments and some retired during implementation hence their gained knowledge and skills were not fully exploited. The results seen may have been affected by other unrecognized competing factors.
Conclusion
Implementation of this project has resulted in an increased HBB knowledge and skills and is associated with an improvement in perinatal survival. An implementation approach combining Moyo and HBB at a large scale is recommended to further evaluate the impact on perinatal mortality.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DHIS:
-
District health information system
- FHR:
-
Fetal heart rate
- FSB:
-
Fresh stillbirth
- HBB:
-
Helping babies breathe
- HCW:
-
Health care workers
- OSCE:
-
Objective structured clinical evaluation
- TOT:
-
Trainer of trainees
- NR:
-
Newborn resuscitations
- LRSs:
-
Low resource settings
References
Barfield WD, AAP COMMITTEE ON FETUS AND NEWBORN. Standard terminology for fetal, infant, and perinatal deaths. Pediatrics. 2016;137(5):e20160551.
Akombi BJ, Renzaho AM. Perinatal mortality in sub-Saharan Africa : a Meta-analysis of demographic and health surveys. Ann Glob Heal. 2019;85:106.
Mangu CD, Rumisha SF, Lyimo EP, Mremi IR, Massawe IS, Bwana VM, et al. Trends, patterns and cause-specific neonatal mortality in Tanzania: a hospital-based retrospective survey. Int Health. 2021;13(4):334–43.
Maaløe N, Housseine N, Bygbjerg IC, Meguid T, Khamis RS, Mohamed AG, et al. Stillbirths and quality of care during labor at the low resource referral hospital of Zanzibar: a case-control study. BMC Pregnancy Childbirth. 2016;16:351.
Ashish KC, Johan W, Robert B, Uwe EMM. Inadequate fetal heart rate monitoring and poor use of partogram associated with intrapartum stillbirth : a case-referent study in Nepal. BMC Pregnancy Childbirth. 2016;16:233.
Ayebare E, Jonas W, Ndeezi G, et al. Fetal heart rate monitoring practices at a public hospital in northern Uganda–what health workers document, do, and say. Glob Health Action. 2020;13:1711618.
Hamelmann P, Vullings R, Kolen FA, et al. Doppler ultrasound Technology for Fetal Heart Rate Monitoring: a review. IEEE Trans Ultrason Ferroelectr Freq Control. 2020;67:226–38.
Plotkin M, Kamala B, Ricca J, et al. Systematic review of Doppler for detecting intrapartum fetal heart abnormalities and measuring perinatal mortality in low- and middle-income countries. Int J Gynecol Obstet. 2020;148:145–56.
Kamala B, Kidanto H, Dalen I, et al. Effectiveness of a novel continuous doppler (Moyo) versus intermittent doppler in intrapartum detection of abnormal fetal heart rate: a randomized controlled study in Tanzania. Int J Environ Res Public Health. 2019;16:315.
Mdoe PF, Ersdal HL, Mduma E, et al. Randomized controlled trial of continuous Doppler versus intermittent fetoscope fetal heart rate monitoring in a resource setting. Int J Gynecol Obstet. 2018;143(3):344–50.
Reisman J, Arlington L, Jensen L, Louis H, Suarez-Rebling D, Nelson BD. Newborn resuscitation training in resource-limited settings: a systematic literature review. Pediatrics. 2016;138:e20154490.
Bang A, Patel A, Bellad R, et al. Helping babies breathe ( HBB ) training : what happens to knowledge and skills over time ? BMC Pregnancy Childbirth. 2016;16:364.
Drake M, Bishanga DR, Temu A, et al. Structured on-the-job training to improve retention of newborn resuscitation skills : a national cohort helping babies breathe study in Tanzania. BMC Pediatr. 2019;19:51.
Tabangin ME, Josyula S, Taylor KK, Vasquez JC, Kamath-rayne BD. Resuscitation skills after Helping Babies Breathe training : a comparison of varying practice frequency and impact on retention of skills in different types of providers. Int Heal. 2018;10(3):163–71.
Eblovi D, Kelly P, Afua G, Agyapong S, Dante SPM. Retention and use of newborn resuscitation skills following a series of helping babies breathe training for midwives in rural Ghana. Glob Health Action. 2017;10:1387985.
Msemo G, Massawe A, Mmbando D, et al. Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training. Pediatrics. 2013;131:e353–60.
Ashish KC, Wrammert J, Clark RB, et al. Reducing perinatal mortality in Nepal using helping babies breathe. Pediatrics. 2016;137:e20150117.
Versantvoort JMD, Kleinhout MY, Ockhuijsen HDL, Bloemenkamp K, De Vries WB, Van Den Hoogen A. Helping babies breathe and its effects on intrapartum-related stillbirths and neonatal mortality in low-resource settings: a systematic review. Arch Dis Child. 2020;105:127–33.
Mduma E, Kvaloy JT, Soreide E, et al. Frequent refresher training on newborn resuscitation and potential impact on perinatal outcome over time in a rural Tanzanian hospital : an observational study. BMJ Open. 2019;9:e030572.
WHO & UNICEF. The every new born action plan. Ending preventable newborn deaths and stillbirths by 2030. 2020. Available from: https://www.unicef.org/media/77166/file/Ending-preventable-newborn-deaths-and-stillbirths-by-2030-universal-health-coverage-in-2020–2025.
Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF. Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS-MIS) 2015-16. Dar es Salaam and Rockville: MoHCDGEC, MoH, NBS, OCGS, and ICF; 2016.
Lafontan SR, Sundby J, Ersdal HL, Abeid M, Kidanto HL, Mbekenga CK. “I was relieved to know that my baby was safe”: Women’s attitudes and perceptions on using a new electronic fetal heart rate monitor during labor in Tanzania. Int J Environ Res Public Health. 2018;15:302.
Michael J, De G-j J, Zyaee P, Ricca J, Fullerton J. Scaling up high-impact interventions : how is it done ? Int J Gynecol Obstet. 2015;130:S4–10.
Acknowledgments
We acknowledge support from involved district authorities, participated staff, master trainers, and funding agency.
Funding
Funding for this project was received from Laerdal Foundation.
Author information
Authors and Affiliations
Contributions
YM – study conduct, analysis, manuscript writing, JG – conduct, and data collection, AY – data collection, manuscript writing, GG – analysis and manuscript writing, EM – study conception and manuscript writing, PM- study conception and manuscript writing. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Permission to conduct this study was obtained from the Hospitals administration, District Medical Officers of respective districts, and the Regional Medical Officer. Ethical approval was obtained from ethical committee at the National Institute of Medical Research (NIMR) Tanzania certificate reference number NIMR/HQ/R.8a/vol. ix/2864. Written informed consent for participation was obtained from all study participants. Permission to use DHIS2 data was obtained from hospital administration. Data was handled confidentially and used for study purposes only. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
Authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Munyaw, Y., Gidabayda, J., Yeconia, A. et al. Beyond research: improved perinatal care through scale-up of a Moyo fetal heart rate monitor coupled with simulation training in northern Tanzania for helping babies breathe. BMC Pediatr 22, 191 (2022). https://doi.org/10.1186/s12887-022-03249-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03249-7