Abstract
Background
Congenital central hypoventilation syndrome (CCHS) is a rare condition caused by mutations in the Paired-Like Homeobox 2B (PHOX2B) gene. It causes alveolar hypoventilation and autonomic dysregulation. This report aimed to raise awareness of this rare cause of neonatal apnea and hypoventilation as well as described the diagnostic work up to confirm the diagnosis in resource-limited setting where polysomnography for neonate is unavailable.
Case presentation
A late preterm female newborn born from a non-consanguineous primigravida 31-year-old mother had desaturation soon after birth followed by apnea and bradycardia. After becoming clinically stable, she still had extubation failure from apnea without hypercapnic ventilatory response which worsened during non-rapid eye movement (NREM) sleep. After exclusion of other etiologies, we suspected congenital central hypoventilation syndrome and sent genetic testing. The result showed a PHOX2B gene mutation which confirmed the diagnosis of CCHS. We gave the patient’s caregivers multidisciplinary home respiratory care training including tracheostomy care, basic life support, and simulation training for respiratory problem solving. Then, the patient was discharged and scheduled for follow-up surveillance for associated conditions.
Conclusion
Diagnosis of CCHS in neonates includes the main clue of the absence of hypercapnic ventilatory response which worsens during non-rapid eye movement (NREM) sleep after exclusion of other causes. Molecular testing for PHOX2B gene mutation was used to confirm the diagnosis.
Similar content being viewed by others
Background
Congenital central hypoventilation syndrome (CCHS) is a rare genetic disorder caused by mutations in the Paired-Like Homeobox 2B (PHOX2B) gene. It causes sleep-related hypoventilation and autonomic nervous system dysregulation [1, 2] which is associated with Hirschsprung disease and neural crest tumors such as neuroblastomas, ganglioneuromas and ganglioneuroblastomas [3, 4].
CCHS typically presents in the neonatal period usually shortly after birth. Presentation of CCHS in newborns were first reported in 1970 [5]. Some patients may also present in late childhood or adulthood (late-onset CCHS).
CCHS classically manifests as hypoventilation which is worsening in non-rapid eye movement (NREM) sleep, unusually it presents with hypoventilation during waking hours except for severe cases and rarely presents with apnea [6]. The main respiratory manifestation is the incapability of breathing regulation in response to abnormality of CO2 and O2 blood concentration, which is termed as hypercapnia and hypoxemia, respectively.
The most common cause for CCHS is identified as autosomal dominant inheritance in the PHOX2B gene [3, 4, 7]. Most PHOX2B gene mutations occur de novo (65–95%) [8]. Other familial PHOX2B gene mutations can be from somatic mutations in symptomatic parents (25%), asymptomatic parents (5–25%) with somatic mosaicism or germline mosaicism [7, 9, 10].
Most of CCHS cases (90–92%) are heterozygous for an abnormal expansion of polyalanine repeat sequence due to polyalanine repeat expansion mutations (PARM) in exon 3 of the PHOX2B gene, nevertheless, the rest (8–10%) are other non-polyalanine repeat expansion mutation (NPARM) in PHOX2B gene [3, 4, 7, 11].
Here we reported a unique case of a newborn with apnea and hypoventilation without hypercapnic ventilatory response which worsened during non-rapid eye movement (NREM) sleep, which was finally diagnosed as CCHS. We aim to raise awareness of this rare cause of neonatal apnea and hypoventilation, describe the diagnostic work up to exclude other etiologies, and confirm the diagnosis in resource-limited setting where polysomnography for neonate was unavailable.
Case presentation
A late preterm 36-week female neonate was born from a non-consanguineous primigravida 31-year-old mother who had regular antenatal care, no underlying disease, normal diabetic screening, no risk of major thalassemia, no history of smoking, illicit drug, or alcohol use. The mother’s serology was normal for hepatitis B virus, VDRL, and anti-HIV.
During pregnancy, she developed isolated idiopathic polyhydramnios with many episodes of fetal bradycardia and had placental angioedema. The mother came up with labor pain and the membrane was artificially ruptured. No systemic analgesia was given during delivery.
The neonate was delivered vaginally, weighted 2,700 g and had an Apgar score of 6 in the 1st minute, 7 in the 5th minute, and 10 in the 10th minute. She then had bradypnea (respiratory rate 30 breaths/min) and oxygen desaturation down to 80% at 10 min of age. After putting on an oxygen hood at 10 L per min (LPM), oxygen saturation was increased up to 95–100%. At that time, her respiratory rate was 30 breaths/min. She received antibiotics because neonatal sepsis was suspected. Two hours after delivery, the neonate had an apneic episode with bradypnea and oxygen desaturation down to 49%. The patient was then put on a nasal continuous positive airway pressure (nCPAP) and transferred to the neonatal intensive care unit (NICU). Her chest radiograph showed only perihilar streaking.
During hospitalization, the patient had multiple episodes of bradycardia, apnea and underwent endotracheal intubation at the age of 3 days. Multiple investigations were performed to find the cause. A chest radiography (CXR) showed no abnormal finding. An electrocardiogram (EKG) showed sinus bradycardia which was suspected from respiratory impairment. An electroencephalogram (EEG) didn’t show electroclinical seizure. A brain MRI showed no abnormality of the brain stem. A diaphragmatic ultrasonography showed symmetrical diaphragmatic motion without paradoxical movement. The patient’s complete blood count (CBC), electrolyte and serum glucose levels were normal. The septic workups which included a hemoculture as well as a cerebrospinal fluid (CSF) analysis and culture were also normal. Thus, apnea of prematurity (AOP), though, unlikely to occur with such severity at her birth gestational age, was suspected at that time and intravenous aminophylline was initiated as a treatment.
At 5 days of age, the patient had delayed passing meconium. A physical examination showed abdominal distension. There was bile content on orogastric tube. The barium enema was performed and showed relatively small caliber and abnormal contraction of the rectum without definite transition zone. Therefore, Hirschsprung disease couldn’t be totally excluded. The patient did not undergo rectal biopsy for a definitive diagnosis at that time because she could pass stools well after rectal irrigations.
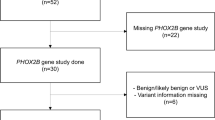
The patient could breathe with ventilator support and her respiratory rate was 40–60 breaths/min. During sleep, the respiratory rate usually dropped to 40 breaths/min without spontaneous breath. However, blood gases and end tidal CO2 levels were normal. The first 2 extubation attempts at the age of 18 and 37 days failed because the patient became drowsy, had stridor and desaturation. Fiberoptic laryngoscopy and bronchoscopy were performed and revealed only erythema and swelling of the arytenoid without laryngomalacia or other airway abnormalities. The results of our investigation are summarized in Table 1. The third extubation to nasal CPAP was performed at the age of 50 days (post-conceptual age of 43 weeks). Intravenous dexamethasone was administered to reduce airway swelling before the extubation. After the extubation the patient had no stridor nor other signs of respiratory distress, but her monitor tracing showed bradypnea, desaturation, and hypoventilation without hypercapnic ventilatory response to respiratory acidosis. Her capillary blood gas confirmed severe respiratory acidosis (pH 7.11, PCO2 89 mmHg). We strongly suspected a diagnosis of congenital central hypoventilation syndrome and sent genetic testing of the PHOX2B gene mutation. The result showed heterozygous expansion of polyalanine, caused by GCG 20/25 repeat expansion (Fig. 1). Unfortunately, we couldn’t do a full attended polysomnography because small size equipment for neonates was unavailable.
The patient was discharged at 3 months of age after a tracheostomy insertion. We gave multidisciplinary home respiratory care training including tracheostomy care, basic life support, simulation training for respiratory problem solving, and provided home visits. We changed the tracheostomy tube every 6 weeks and did follow-up surveillance including neurocognitive development.
At 3 years of age, the child presented with abdominal distension and a repeat barium enema was suggestive of Hirschsprung disease. She underwent trans anal anorectal pull-through surgery. A biopsy of the sigmoid colon revealed aganglionosis at proximal end and throughout the entire length of specimen confirming Hirschsprung disease.
Until now, the child was well managed on home ventilator support. Although the parents took good care of her, she had two episodes of pneumonia. She gradually caught up with her growth and development. Her mother can perform home respiratory care proficiently and we hope that she can be decannulated in the future.
Discussion and conclusion
Congenital central hypoventilation syndrome (CCHS) is a rare condition, first reported in 1970 [5]. It may be underdiagnosed. At that time, there were about 20 case reports of idiopathic central hypoventilation syndrome in adults. In 1999, The American Thoracic Society indicated there were roughly 160–180 cases of CCHS around the world [12]. Until 2003, the PHOX2B gene mutations, located on chromosome 4q12, were considered responsible for CCHS leading to diagnosis of more cases [4]. In 2005, the French CCHS working group reported an estimated incidence of 1: 200,000 live births in France [13]. In 2009, about 1,000 cases were confirmed by molecular studies [14]. Since then, more than 1000 cases of CCHS have been reported worldwide [8].
The clinical presentation of CCHS is variable from shallow breathing during sleep, neonatal cyanosis, central apnea during wakefulness to sudden death [15, 16]. In our patient, the first manifestation was neonatal apnea and bradycardia. The diagnosis of CCHS in preterm infants (gestational age < 37 weeks) could be challenging and significantly delayed, especially in early or extremely premature infants (gestational age < 28 weeks), because they commonly have AOP which has similar presentation as that of CCHS. Unlike CCHS, apnea in AOP frequently occurred in rapid eye movement (REM) sleep and almost all infants eventually outgrow AOP at post-conceptual age of 36 to 40 weeks. However, in extremely premature infants AOP could exist beyond 38 to 40 weeks [17]. Without the aid of polysomnography, the diagnosis of CCHS was suspected even with its rarity in our patient because apnea and bradypnea still persist at post-conceptual age of 43 weeks and other causes including cardiopulmonary, neuromuscular, and metabolic causes had been ruled out. The unusually severe and frequent apnea requiring endotracheal intubation in late preterm infants could be another important clue to the diagnosis of CCHS.
During ventilator support, our patient still had hypoventilation during non-rapid eye movement (NREM) sleep. After other causes had been ruled out, the diagnosis of CCHS was suspected even with the rareness of the disease.
The diagnosis of CCHS was supported by polysomnography and confirmed by molecular testing for PHOX2B gene mutation, the disease defining gene [4, 7]. Her genetic testing results was heterozygous of polyalanine expansion 20/25. The polyalanine repeat mutation (PARM) is found in over 90% of CCHS. The genotype of PARM coding ranges from 20/24 to 20/33 (The normal genotype is 20/20). The 20/25 genotype, as in our patient, is one of the most common mutations of PHOX2B gene [8, 14].
The respiratory severity of CCHS is related to the number of repeats in PARM. Her genotype mutation is 20/25 which has the mildest form of respiratory symptom. A patient with this type of mutation has a variety of symptom severities. Most patients do not require 24 h of ventilatory support while they grow up [8]. Moreover, the PARM length is also associated with several autonomic dysregulation-related symptoms such as arrhythmia, abnormal sweating and GI symptoms [7]. In our patient, she had only bradycardia and constipation as the autonomic symptom.
Constipation in CCHS patients could be from autonomic dysfunction or Hirschsprung disease [3]. Hirschsprung disease occurs among 20% of CCHS patients. It was reported in 87 to 100% of NPARMs in contrast to 13 to 20% of PARMs. There was no report in 20/25 genotype before. At 3 years of age, this child was finally diagnosed Hirschsprung disease and was the first case in 20/25 genotype to the best of our knowledge.
All CCHS patients should be evaluated for 3 main issues which are breathing physiology during asleep and awake, autonomic nervous system function, and comorbidities screening. All evaluations and screening processes will be individualized to each patient who has different forms of mutations on the PHOX2B gene [8]. For 20/25 mutations as in this patient, the guideline suggests annual in-hospital comprehensive physiologic testing, neurocognitive assessment, and 72 h Holter monitoring.
There are many ways of assisting ventilation such as invasive ventilation, noninvasive positive pressure ventilation, and diaphragmatic pacing. Invasive ventilation with a tracheostomy tube is suitable for the infant period as in the case of this patient. Noninvasive positive pressure ventilation is usually used in school-aged patients during sleep. Diaphragmatic pacing can also be considered in some severe cases who depend on mechanical ventilator during daytime but it is costly and needs to be performed by experienced tertiary care centers [18].
Early diagnosis and multidisciplinary management can help when predicting disease outcomes and long-term survival. Two-thirds to 80% of patients are able to breathe on their own during waking hours after infancy while the rest need to use a mechanical ventilator all the time. Effective ventilation support can reduce mortality [19]. While there are all kinds of complications, severe pneumonia is the most common cause of death with CCHS patients. Continuing abnormalities in breathing require lifelong ventilatory support [20]. Neurologic complications including learning disabilities and attention deficit hyperactivity disorder may result from affected brain development as a consequence of chronic hypoxia [21]. Although CCHS is a lifelong disorder and there are many life-threatening complications, many CCHS patients eventually have a good quality of life and normal social functioning.
In conclusion, the absence of a hypercapnic ventilatory response which worsens during non-rapid eye movement (NREM) sleep, after exclusion of other causes, is the main clue to the diagnosis of CCHS in neonates. Molecular testing for PHOX2B gene mutation was used to confirm the diagnosis.
Availability of data and materials
This data is available from the authors upon reasonable request and with the permission of the institution.
Abbreviations
- CCHS:
-
Congenital central hypoventilation syndrome
- PHOX2B:
-
Paired-Like Homeobox 2B
- NREM:
-
Non-rapid eye movement
- PARM:
-
Polyalanine repeat expansion mutation
- NPARM:
-
Non-polyalanine repeat expansion mutation
- LPM:
-
Liter per min
- nCPAP:
-
Nasal continuous positive airway pressure
- NICU:
-
Neonatal intensive care unit
References
Weese-Mayer DE, Silvestri JM, Huffman AD, Smok-Pearsall SM, Kowal MH, Maher BS, Cooper ME, Marazita ML. Case/control family study of autonomic nervous system dysfunction in idiopathic congenital central hypoventilation syndrome. Am J Med Genet. 2001;100(3):237–45.
Marazita ML, Maher BS, Cooper ME, Silvestri JM, Huffman AD, Smok-Pearsall SM, Kowal MH, Weese-Mayer DE. Genetic segregation analysis of autonomic nervous system dysfunction in families of probands with idiopathic congenital central hypoventilation syndrome. Am J Med Genet. 2001;100(3):229–36.
Berry-Kravis EM, Zhou L, Rand CM, Weese-Mayer DE. Congenital central hypoventilation syndrome: PHOX2B mutations and phenotype. Am J Respir Crit Care Med. 2006;174(10):1139–44.
Amiel J, Laudier B, Attie-Bitach T, Trang H, de Pontual L, Gener B, Trochet D, Etchevers H, Ray P, Simonneau M, Vekemans M, Munnich A, Gaultier C, Lyonnet S. Polyalanine expansion and frameshift mutations of the paired-like homeobox gene PHOX2B in congenital central hypoventilation syndrome. Nat Genet. 2003;33(4):459–61.
Mellins RB, Balfour HH Jr, Turino GM, Winters RW. Failure of automatic control of ventilation (Ondine’s curse). Report of an infant born with this syndrome and review of the literature. Med (Baltim). 1970;49(6):487–504.
Carroll MS, Patwari PP, Kenny AS, Brogadir CD, Stewart TM, Weese-Mayer DE. Residual chemosensitivity to ventilatory challenges in genotyped congenital central hypoventilation syndrome. J Appl Physiol (1985). 2014;116(4):439–50.
Weese-Mayer DE, Berry-Kravis EM, Zhou L, Maher BS, Silvestri JM, Curran ME, Marazita ML. Idiopathic congenital central hypoventilation syndrome: analysis of genes pertinent to early autonomic nervous system embryologic development and identification of mutations in PHOX2b. Am J Med Genet A. 2003;123a(3):267–78.
Weese-Mayer DE, Berry-Kravis EM, Ceccherini I, Keens TG, Loghmanee DA, Trang H. An official ATS clinical policy statement: Congenital central hypoventilation syndrome: genetic basis, diagnosis, and management. Am J Respir Crit Care Med. 2010;181(6):626–44.
Bachetti T, Parodi S, Di Duca M, Santamaria G, Ravazzolo R, Ceccherini I. Low amounts of PHOX2B expanded alleles in asymptomatic parents suggest unsuspected recurrence risk in congenital central hypoventilation syndrome. J Mol Med (Berl). 2011;89(5):505–13.
Rand CM, Yu M, Jennings LJ, Panesar K, Berry-Kravis EM, Zhou L, Weese-Mayer DE. Germline mosaicism of PHOX2B mutation accounts for familial recurrence of congenital central hypoventilation syndrome (CCHS). Am J Med Genet A. 2012;158a(9):2297–301.
Weese-Mayer DE, Marazita ML, Rand CM, Berry-Kravis EM, et al. Congenital Central Hypoventilation Syndrome. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, et al., editors. GeneReviews is a registered trademark of the University of Washington, Seattle. Seattle: University of Washington, Seattle University of Washington, Seattle; 1993. All rights reserved.
Idiopathic congenital central. hypoventilation syndrome: diagnosis and management. American Thoracic Society. Am J Respir Crit Care Med. 1999;160(1):368–73.
Trang H, Dehan M, Beaufils F, Zaccaria I, Amiel J, Gaultier C. The French Congenital Central Hypoventilation Syndrome Registry: general data, phenotype, and genotype. Chest. 2005;127(1):72–9.
Weese-Mayer DE, Rand CM, Berry-Kravis EM, Jennings LJ, Loghmanee DA, Patwari PP, Ceccherini I. Congenital central hypoventilation syndrome from past to future: model for translational and transitional autonomic medicine. Pediatr Pulmonol. 2009;44(6):521–35.
Fleming PJ, Cade D, Bryan MH, Bryan AC. Congenital central hypoventilation and sleep state. Pediatrics. 1980;66(3):425–8.
Weese-Mayer DE, Silvestri JM, Menzies LJ, Morrow-Kenny AS, Hunt CE, Hauptman SA. Congenital central hypoventilation syndrome: diagnosis, management, and long-term outcome in thirty-two children. J Pediatr. 1992;120(3):381–7.
Zhao J, Gonzalez F, Mu D. Apnea of prematurity: from cause to treatment. Eur J Pediatr. 2011;170(9):1097–105.
Verkaeren E, Brion A, Hurbault A, Chenivesse C, Morelot-Panzini C, Gonzalez-Bermejo J, Attali V, Similowski T, Straus C. Health-related quality of life in young adults with congenital central hypoventilation syndrome due to PHOX2B mutations: a cross-sectional study. Respir Res. 2015;16:80.
Grigg-Damberger M, Wells A. Central congenital hypoventilation syndrome: changing face of a less mysterious but more complex genetic disorder. Semin Respir Crit Care Med. 2009;30(3):262–74.
Ruof H, Hammer J, Tillmann B, Ghelfi D, Weber P. Neuropsychological, behavioral, and adaptive functioning of Swiss children with congenital central hypoventilation syndrome. J Child Neurol. 2008;23(11):1254–9.
Vanderlaan M, Holbrook CR, Wang M, Tuell A, Gozal D. Epidemiologic survey of 196 patients with congenital central hypoventilation syndrome. Pediatr Pulmonol. 2004;37(3):217–29.
Acknowledgements
The authors would like to thank the patient’s family for their consent to publish this case report. We also would like to express gratitude to all neonatologists and pediatric surgeons at Siriraj Hospital, Mahidol University for their contribution to patient care. We are grateful to Martin C. Nicholson for English editing, Siriraj Medical Research Center (SiMR) for publication support, and Division of Medical Genetics, Department of Pediatrics, Faculty of Medicine Ramathibodi Hospital, Mahidol University for the patient’s genetic testing.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
PT, KR, and NK drafted the manuscript and reviewed the literature. PK, MC, and BY contributed to patient care and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The case report was performed according to the Declaration of Helsinki. Written informed consent was obtained from the patient’s parents for the publication of this case report.
Consent for publication
Written informed consent for publication of this case report was obtained from the parents of the patients.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tovichien, P., Rattananont, K., Kulthamrongsri, N. et al. Rare cause of neonatal apnea from congenital central hypoventilation syndrome. BMC Pediatr 22, 105 (2022). https://doi.org/10.1186/s12887-022-03167-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03167-8