Abstract
Background
Perinatal asphyxia is one of the leading causes of neonatal mortality and morbidity in Ethiopia. Understanding associated factors of perinatal asphyxia are important to identify vulnerable groups and to improve care during the perinatal period. Thus, this study aimed to assess the prevalence and associated factors of perinatal asphyxia among newborns admitted to NICU at the Gondar University Comprehensive Specialized Hospital Northwest Ethiopia, Ethiopia.
Method
Institutional based cross-sectional study was conducted on 364 newborns from November 2018 - August 2019. Data was collected using a structured and pre-tested questionnaire. It was then cleaned, coded, and entered using EPI INFO version 7, then analyzed with SPSS statistics version 20.0. Binary logistic regression analysis was used to identify variables with p < 0.2. An adjusted odds ratio (AOR) with a 95% CI and P-value of <0.05 was used to identify significantly associated variables with perinatal asphyxia.
Result
The prevalence of perinatal asphyxia in this study was 19.8, 95%CI (15.9, 24.2). Absence of maternal formal education (AOR = 4.09, 95%CI: 1.25, 13.38), pregnancy-induced hypertension (AOR = 4.07, 95%CI: 1.76, 9.40), antepartum hemorrhage (AOR = 6.35, 95%CI: 1.68, 23.97), prolonged duration of labor (AOR = 3.69, 95%CI: 1.68, 8.10), instrumental delivery (AOR = 3.17, 95%CI: 1.22, 8.21), and meconium-stained amniotic fluid (AOR = 4.50, 95%CI: 2.19, 9.26) were significantly associated with perinatal asphyxia.
Conclusion
The prevalence rate of perinatal asphyxia in this study was comparable to other resource poor countries. The absence of maternal formal education, pregnancy-induced hypertension, and Antepartum hemorrhage, prolonged duration of labor, Instrumental assisted delivery, and meconium-stained amniotic fluid was having significant association with perinatal asphyxia in this study.
Similar content being viewed by others
Background
Globally, perinatal asphyxia is the most serious public health problem and occurs due to impaired blood gas exchange leading to progressive hypoxia [1].
According to World Health Organization (WHO), perinatal asphyxia is defined as “failure to initiate and sustain breathing at birth” [2]. APGAR score is one of the indicators used to describe the wellbeing of the newborn at birth [3]. It is difficult to detect the timing of birth asphyxia in different inevitability [4] that is the reason the severity of birth asphyxia is widely evaluated by the Apgar score, at 1 and 5 min next to birth [5]. Apgar score consists of five components as appearance (color), heart rate, grimaces (reflexes), activity (muscle tone), and respiration each of which is given a score of 0, 1, or 2. Apgar score < 7 for longer than 5 min indicated perinatal asphyxia [6,7,8].
Perinatal asphyxia is one of the leading causes of neonatal morbidity and mortality globally, especially in developing countries [9], and also the central cause of long–term diseases like cerebral palsy, mental retardation, irreversible neurologic damage, and epilepsy leading to detrimental long-term consequences for both the child and family [10,11,12].
Globally, every year more than 2.5 million infants die within the first month of life and nearly all deaths of newborns were in developing countries with the highest number of deaths were observed in Sub-Saharan Africa [13] In low-income countries 23% of all neonatal deaths occurred due to perinatal asphyxia [14]. In Africa, perinatal asphyxia is one of the top three causes of newborn deaths next to infection and prematurity [15, 16]. Various studies indicated the prevalence of perinatal asphyxia in Columbia was 41% [17], Nigeria 21% [16], Jimma southwest Ethiopia 12.5% [18], and in Dire Dawa, Ethiopia 2.5% [19]. Evidence indicated that the neonatal mortality rate is 29/1000 live births in Ethiopia and 23% and a large proportion of these neonatal death occur within the first 48 h after delivery [20].
Perinatal asphyxia can be affected by different factors. For example, obstetric complications [18], duration of labor [19, 21], maternal educational status, [19], lack of antenatal care, caesarian section, and weight of the fetus [21] can have an impact on the outcome of the newborn. Maternal, obstetrical, and fetal factors which result in decreased blood flow and oxygenation to the tissues can cause hypoxia in the fetus and asphyxia in the newborn [22]. Perinatal asphyxia is highly prevalent in developing countries as well as in Ethiopia. It is one of the top three causes of neonatal death. Therefore, this study aimed to investigate the prevalence of perinatal asphyxia and its associated factors among newborns admitted to the Neonatal Intensive Care Unit (NICU) at the University of Gondar Comprehensive Specialized Hospital Northwest Ethiopia, Ethiopia,
Methods
Study design and period
The institution-based cross-sectional study design was conducted at the University Gondar Comprehensive Specialized Hospital, from November 1st/2018 - August 31st/2019.
Study area/setting
This study was conducted at the University of Gondar Comprehensive Specialized Hospital. It is located in Gondar city, Amhara National Region State, Northwest Ethiopia. It is the only comprehensive specialized teaching and referral hospital in the area with a total of 641 beds, 130 beds on the pediatrics side including the neonatal ward. It is the only hospital with NICU in the area.
NICU has 36 beds, 14 incubators, and 4 radiant warmers. The staff is composed of senior pediatricians, residents, interns, and BSc nurses. According to the hospital monthly mortality and morbidity report, there are about 150 neonatal admissions per month which give about 1800 admissions annually.
Population and sample
The source population in this study was all new-born who were ever admitted to NICU at the University of Gondar Comprehensive Specialized Hospital and the study population was new-born who were admitted to NICU during the study period. The data was collected in this hospital from November 1st/2018 - August 31st/2019. By using systematic random sampling technique newborns with birth weight ≥ 1000 g or gestational age ≥ 28 weeks were included in the study.
The sample size was determined by using single population proportion formula assuming a 16.6% proportion from a previous study conducted at the University of Gondar referral hospital in 2014 [23], 95% confidence interval, and 4% marginal error.
With Z of 1.96 at 95% confidence interval, the margin of error of 4%, and by adding a 10% non-response rate then the final sample size was 365.
Variable of the study
The dependent variable was perinatal asphyxia, whereas the independent variables were socio-demographic characteristics (maternal age, marital status, educational status, and place of residence), antepartum factors (previous obstetrics history, ANC visits, obstetrics, and medical complications), Intrapartum factors (membrane rupture, duration of labor, obstructed labor, meconium-stained amniotic fluid, fetal presentation, mode and place of delivery), and fetal factors (Gestational age at birth, Apgar score, birth weight, sex of the newborn).
Newborns with birth weight ≥ 1000 g or gestational age ≥ 28 weeks were included in the study. Fifth minute Apgar score < 7 or requirement of positive pressure ventilation immediately after delivery with neurologic manifestations (hypo or hypertonia, irritability) was used to define perinatal asphyxia among the study participants [6,7,8]. Whereas, Newborns with major congenital anomalies incompatible with life such as hydrops, Neural tube defects, cyanotic congenital heart diseases, or chromosomal anomalies were excluded from the study. Newborns with opium or anesthesia-related low Apgar score were also excluded from this study.
Data collection procedure and quality control
The data were collected by 4 intern doctors and 2 BSc nurses using a standardized pretested questionnaire. One day theoretical and practical training was given for the data collectors about the objective of the study. For each newborn, we have collected data regarding pregnancy, delivery, and neonatal admission characteristics. Socio-demographic data and medical history were taken by interview. Apgar score and diagnosis were filled by chart review. To ensure the quality of data, the questionnaire was pre-tested for consistency of understanding and completeness of data items on 10% of newborns at Obstetrics Labor Ward. The data collection process was closely monitored by the principal investigator throughout the data collection period. Completed questionnaires were checked regularly for completeness of the information and any gaps identified were immediately communicated to the data collectors.
Data processing and analysis
Data were coded and entered into Epi info version 7.0 then exported to SPSS version 20 for cleaning and analysis. Summary statistics were carried out. Multicollinearity and model fitness was checked using Hosmer Lemeshow. Both Bi-variable and multivariable logistic regression analyses were used to identify associated factors of perinatal asphyxia. Variables with a P-value ≤ of 0.2 in the bi-variable logistic regression were entered into the multivariable logistic regression analysis. Adjusted odds ratio (AOR) with 95% confidence interval (CI) was computed. Variables with a p-value <0.05 in the multivariable logistic regression analysis were considered as significantly associated with perinatal asphyxia.
Results
Maternal socio-demographic characteristics
A total of 364 study participants were included in this study with a response rate of 99.7%. The majority of mothers 141(38.7%) were aged 25-29 years. Regarding marital status, 357(98.1%) of the mothers were married at the moment. Nearly one-third of the mothers (29.9%) had no formal education. Among the total study participants, 207(56.9%) were rural dwellers (Table 1).
Antepartum related characteristics
Among the study participants, 211(58%) were multiparous. About 346 (95.1%) mothers had a history of at least one ANC follow-up during the current pregnancy. Based on the previous obstetrics history of mothers 20 (5.5%) had an abortion, 18 (4.9%) had intrauterine death and 16(4.4%) had neonatal death. Twenty-one (8.5%) mothers had antepartum hemorrhage during pregnancy. In about 56(15.4%) mothers pregnancy-induced hypertension was diagnosed (Table 2).
Intrapartum related characteristics
Out of the total participants, 336(92.3%) mothers had spontaneous onset of labor and in about 67(18.4%) mothers’ labor duration was more than 18 h. Nearly two-thirds (65.7%) of mothers had spontaneous vertex deliveries (SVD). In our study, inborn babies were more than outborn babies accounting for 257(70.6%) and 107(29.4%), respectively. In about 82(22.5%) mothers the amniotic fluid was meconium stained (Table 3).
Neonatal related characteristics
Out of the total newborns, 213(58.5%) were male. Three-quarters (76.92%) of the newborn was a term. Three-fourth (73.1%) of the newborns had normal birth weight. There were 27(7.42%) twins among the study participants (Table 4).
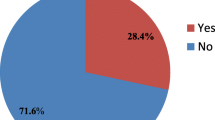
Prevalence of perinatal asphyxia
The prevalence of perinatal asphyxia in newborns admitted to NICU at the University of Gondar Comprehensive Specialized Hospital was 19.8% with 95%CI (15.9, 24.2).
Predictors of perinatal asphyxia
The bi-variable logistic regression analysis showed that maternal education, place of residence, parity, pregnancy-induced hypertension, antepartum hemorrhage, premature rupture of membrane, prolonged duration of labor, mode of delivery, place of delivery, fetal presentation, obstructed labor, meconium-stained amniotic fluid, gestational age, and birth weight were associated with perinatal asphyxia with p-value <0.2. However, the multivariable logistic regression analysis identified that absence of maternal formal education, pregnancy-induced hypertension, antepartum hemorrhage, duration of labor ≥18 h, instrumental delivery, and meconium-stained amniotic fluid were significantly associated with perinatal asphyxia.
The likelihood of developing perinatal asphyxia among neonates born from mothers who had not to attend formal education was 4 times (AOR = 4.09, 95%CI: 1.25, 13.38) higher compared with educated one. Neonates born from mothers with pregnancy-induced hypertension were 4.07 times (AOR = 4.07, 95%CI: 1.76, 9.40) more likely to develop perinatal asphyxia compared with their counterparts. Neonates born from mothers with Antepartum Hemorrhage had 6.4 times (AOR = 6.35, 95%CI: 1.68, 23.97) higher risk of developing perinatal asphyxia as compared to their counterparts. Mothers who had prolonged labor were 3.7 times (AOR = 3.69, 95%CI: 1.68, 8.10) more likely to have asphyxiated newborns than those who had a normal duration of labor. Regarding the mode of delivery, those newborns born through instrumental assisted were 3.2 times (AOR = 3.17, 95%CI: 1.22, 8.21) more likely to develop perinatal asphyxia than newborns delivered through spontaneous vaginal delivery. Neonates born with meconium-stained amniotic fluid were 4.5 times (AOR = 4.50, 95%CI: 2.19, 9.26) as likely to have perinatal asphyxia (Table 5).
Discussion
Perinatal asphyxia is one of the major causes of neonatal death during the neonatal period. Therefore, this study aimed to assess the prevalence and associated factors of perinatal asphyxia in newborns admitted to NICU at the University of Gondar Comprehensive Specialized Hospital with level III NICU care.
In this study, the prevalence of perinatal asphyxia was found to be 19.8% (15.9, 24.2). This study is in line with other studies done in Nigeria (21.1%) [16], Tigray Ayder hospital with level IV NICU care (18%) [21], and higher than the previous report from the University of Gondar Referral Hospital in 2013 (13.8%) [24]. This might be due to increased referral cases from time to time in different primary hospitals and health centers either after detecting obstetrics complications or attending deliveries of asphyxiated babies because the University of Gondar Comprehensive Specialized Hospital is the only specialized hospital in the catchment area with Neonatal Intensive Care Unit. On the other hand, the prevalence rate obtained in this study was lower than what has been observed in Dilla University Referral Hospital with level III NICU care (32.8%) [25]. In Dilla, low birth weight was a significant risk factor of perinatal asphyxia and there was a high proportion of low birth weight in Dilla as compared to Gondar, this may increase the prevalence of perinatal asphyxia.
In this study, there was a statistically significant association between perinatal asphyxia and maternal educational status. Neonates born from mothers who had not attend formal education were four times more likely to develop perinatal asphyxia. This finding is consistent with studies done in Ethiopia in Dilchora Referral Hospital with level II NICU care, Kenya kaka mega county referral hospital, Ghana, Tanzania, and Pakistan [19, 26,27,28,29]. This may be due to women without formal education might have a lack of awareness about maternal health care services like antenatal care visits. Maternal illiteracy is a very broad indicator of poor socio-economic conditions associated with malnutrition, frequent pregnancies, and delay in care-seeking during the antepartum and intrapartum period.
Pregnancy-induced hypertension was also observed as a significant risk factor of perinatal asphyxia in our study. Neonates born from mothers with pregnancy-induced hypertension were four times more likely to develop perinatal asphyxia compared with their counterparts. This study is consistent with studies conducted in Jimma, India, Cameroon, and Pakistan [6, 18, 30, 31]. Pregnancy-induced hypertension can result in a decrease in placental blood flow and loss of placental integrity which can lead to an inadequate fetoplacental blood flow causing intrauterine growth retardation and perinatal asphyxia [32].
Prolonged duration of labor was another risk factor of perinatal asphyxia. Newborns delivered from mothers who spent more than 18 h in labor were 3.7 times more likely to develop perinatal asphyxia as compared to their counterparts. This result is consistent with previous studies done at the University of Gondar Referral Hospital [24], in Dilchora referral Hospital [19], Cameroon, Kenya, Nigeria, and Sweden [6, 16, 26, 33]. Prolonged labor is likely to occur if the women have a narrow pelvis, poor uterine contraction, or slow cervical effacement. If the labor does not progress normally, there may be serious complications such as uterine rupture, hemorrhage, maternal infection, neonatal infection, and fetal distress. All of these complications can lead to perinatal asphyxia. Furthermore, the child experience prolonged or arrested labor may start to experience birth asphyxia due to umbilical cord problems or the stress of too many contractions [34].
Antepartum hemorrhage is another risk factor of perinatal asphyxia. Newborns delivered from mothers with antepartum hemorrhage were 6.4 times more likely to develop perinatal asphyxia. This finding is similar to a study conducted in Pakistan and Indonesia [19, 24]. During antepartum bleeding, there will be decreased blood flow from the mother to the fetus which can lead to perinatal asphyxia if maternal transfusion or delivery is delayed.
Regarding the mode of delivery, newborns delivered with instrumental assisted delivery were 3.2 times more likely to develop perinatal asphyxia. This finding is similar to a study conducted in Dilchora referral Hospital, Ethiopia, and India [19, 30]. This finding might be because either most of the mothers came with possible complications or the decision to assist with the instrument might be delayed till they develop a complication. Most of the indications for instrumental delivery can compromise adequate oxygen supply to the fetus, which might result in fetal distress and perinatal asphyxia. In general in developing countries including Ethiopia mothers and neonates were prone to morbidity and mortality due to instrumental delivery [35].
Neonates born from mothers with a history of meconium-stained amniotic fluid were four and half times more likely to develop perinatal asphyxia. This is consistent with previous studies conducted at the University of Gondar Referral Hospital [24], Jimma public Hospitals [18], Cameroon [30], Pakistan [31], India [6], and Nigeria [16]. This might be explained by meconium aspiration syndrome leading to airway obstruction and subsequent hypoxia. The possible reason could be intrapartum inhalation of meconium-stained amniotic fluid resulted in chemical pneumonitis with the inflammation of pulmonary tissues, the aspiration syndrome leading to airway obstruction, and pulmonary air leak, this in turn to hypoxia that is prenatal asphyxia [36].
Even though, there is a standard guideline for neonatal resuscitation; the death of neonatal mortality due to perinatal asphyxia is increasing in Ethiopia. This means perinatal asphyxia is a common problem in our country so every stakeholder better use different strategies to reduce the burden of perinatal asphyxia by taking the appropriate action on the determinants.
The limitation of this study was some potential predictors for the low Apgar score were not considered like placental factors, maternal anemia, and intrauterine infections.
Conclusion
The prevalence rate of perinatal asphyxia in this study was comparable to other poor rescores countries. The absence of maternal education, pregnancy-induced hypertension, antepartum hemorrhage, prolonged duration of labor, instrumental assisted delivery, and meconium-stained amniotic fluid was found to be predictors of perinatal asphyxia. Therefore, to reduce the burden of perinatal asphyxia better to improve the quality of intrapartum care by implementing different strategies to prevent prolonged labor, identify obstetrics complications, ascertain and make a strict follow up of mothers with meconium-stained amniotic fluid. Addressing and identifying determinants of perinatal asphyxia may improve the application of the WHO standard guideline effectively and consistently.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality but are available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Ante-Natal Care
- APGAR:
-
Appearance, Pulse rate, Grimace, Activity, Respiration rate
- C/S:
-
Cesarean section
- GA:
-
Gestational age
- UOGCSH:
-
University of Gondar Comprehensive Specialized Hospital
- NICU:
-
Neonatal Intensive Care Unit
- COR:
-
Crude odds ratio
- AOR:
-
Adjusted odds ratio
- PNA:
-
Perinatal Asphyxia
- PROM:
-
Premature Rupture of Membrane
- SPSS:
-
Statistical Package for Social Science
- SVD:
-
Spontaneous Vertex delivery
- WHO:
-
World Health Organization
References
Antonucci R, Porcella A, Pilloni MD. Perinatal asphyxia in the term newborn. J Pediatr Neonatal Individualized Med (JPNIM). 2014;3(2):e030269.
Technical Working Group WHO. Postpartum care of the mother and newborn: a practical guide. Birth. 1999;26(4):255–8.
Ruth VJ, Raivio KO. Perinatal brain damage: predictive value of metabolic acidosis and the Apgar score. Br Med J. 1988;297(6640):24–7.
Keenan WJ, Udaeta E, López M, Niermeyer S. Delivery and immediate neonatal care. pediatric education in disasters manual american academy of pediatrics, Buenos Aires, Argentina; 2009. p. 217–37.
Ryan S, Gregg J, Patel L. Core paediatrics: a problem-solving approach. Arnold; 2003.
Chiabi A, Nguefack S, Evelyne M, Nodem S, Mbuagbaw L, Mbonda E, et al. Risk factors for birth asphyxia in an urban health facility in Cameroon. Iran J Child Neurol. 2013;7(3):46.
Chandra S, Ramji S, Thirupuram S. Perinatal asphyxia: multivariate analysis of risk factors in hospital births. Indian Pediatr. 1997;34(3):206–12.
Yelamali B, Panigatti P, Pol R, Talawar K, Naik S, Badakali A. Outcome of newborn with birth asphyxia in tertiary care hospital-a retrospective study. Medica Innovatica. 2014;3(2):59–64.
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–57.
Low JA, Pickersgill H, Killen H, Derrick EJ. The prediction and prevention of intrapartum fetal asphyxia in term pregnancies. Am J Obstet Gynecol. 2001;184(4):724–30.
Van Lerberghe W. The World Health Report 2005: Make every mother and child count: World Health Organization; 2005.
Wallander JL, McClure E, Biasini F, Goudar SS, Pasha O, Chomba E, et al. Brain research to ameliorate impaired neurodevelopment-home-based intervention trial (BRAIN-HIT). BMC Pediatr. 2010;10(1):27.
UNICEF. For every child, reimagine: UNICEF annual report 2019. UNICEF; 2020.
Shireen N, Nahar N, Mollah A. Risk factors and short-term outcome of birth asphyxiated babies in Dhaka medical college hospital. Bangladesh J Child Health. 2009;33(3):83–9.
Lawn J, Mongi P, Cousens S. Africa’s newborns-counting them and making them count. In: Opportunities for Africa’s newborns: practical data, policy and programmatic support for newborn care in Africa; 2006.
Ilah BG, Aminu MS, Musa A, Adelakun MB, Adeniji AO, Kolawole T. Prevalence and risk factors for perinatal asphyxia as seen at a specialist hospital in Gusau, Nigeria. Sub-Saharan Afr J Med. 2015;2(2):64.
Torres-Muñoz J, Rojas C, Mendoza-Urbano D, Marín-Cuero D, Orobio S, Echandía C. Risk factors associated with the development of perinatal asphyxia in neonates at the Hospital Universitario del Valle, Cali, Colombia, 2010-2011. Biomédica. 2017;37:51–6.
Wayessa Z, Belachew T, Joseph J. Birth asphyxia and associated factors among newborns delivered in Jimma zone public hospitals, Southwest Ethiopia: a cross-sectional study. J Midwifery Reprod Health. 2018;6(2):1289–95.
Ibrahim N, Muhye A, Abdulie S. Prevalence of birth asphyxia and associated factors among neonates delivered in Dilchora Referral Hospital. Dire Dawa, Eastern Ethiopia. Clin Mother Child Health. 2017;14(279):2.
Ethiopia. Ethiopia Demographic and Health Survey, 2016: ICF International, c entral Statistical Agency, uly 2017. 2012.
Gebregziabher GT, Hadgu FB, Abebe HT. Prevalence and associated factors of perinatal asphyxia in neonates admitted to ayder comprehensive specialized hospital, Northern Ethiopia: a cross-sectional study. Int J Pediatr. 2020;2020.
Berglund S, Grunewald C, Pettersson H, Cnattingius S. Risk factors for asphyxia associated with substandard care during labor. Acta Obstet Gynecol Scand. 2010;89(1):39–48.
Kokeb M, Desta T. Institution based prospective cross-sectional study on patterns of neonatal morbidity at Gondar University hospital neonatal unit, North-West Ethiopia. Ethiop J Health Sci. 2016;26(1):73–9.
Gudayu TW. Proportion and factors associated with low fifth minute Apgar score among singleton newborn babies in Gondar University Referral Hospital; North West Ethiopia. Afr Health Sci. 2017;17(1):1–6.
Alemu A, Melaku G, Abera GB, Damte A. Prevalence and associated factors of perinatal asphyxia among newborns in Dilla University referral hospital, Southern Ethiopia–2017. Pediatr Health Med Ther. 2019;10:69.
Kibai EK. Perinatal factors associated with birth asphyxia among neonates in maternity ward kakamega county refferal hospital, kenya; 2017.
Bouwhuis SA, Davis MD. Contribution of sexually transmitted diseases and socioeconomic factors to perinatal mortality in rural Ghana. Int J Dermatol. 2004;43(1):27–30.
Sepeku A, Kohi T. Treatment outcomes of neonatal asphyxia at a national hospital in Dar es Salaam, Tanzania. Afr J Nurs Midwifery. 2011;13(2):43–56.
Tabassum F, Rizvi A, Ariff S, Soofi S, Bhutta ZA. Risk factors associated with birth asphyxia in rural district Matiari, Pakistan: a case control study. Int J Clin Med. 2014;5(21):1430.
Gane B, Bhat V, Rao R. Antenatal and intrapartum risk factors for perinatal asphyxia: A case control study. Curr Pediatr Res. 2013.
Aslam HM, Saleem S, Afzal R, Iqbal U, Saleem SM, Shaikh MWA, et al. Risk factors of birth asphyxia. Ital J Pediatr. 2014;40(1):94.
Malhotra A, Allison BJ, Castillo-Melendez M, Jenkin G, Polglase GR, Miller SL. Neonatal morbidities of fetal growth restriction: pathophysiology and impact. Front Endocrinol. 2019;10:55.
Altman M, Sandström A, Petersson G, Frisell T, Cnattingius S, Stephansson O. Prolonged second stage of labor is associated with low Apgar score. Eur J Epidemiol. 2015;30(11):1209–15.
Qureshi AM, ur Rehman A, Siddiqi TS. Hypoxic ischemic encephalopathy in neonates. J Ayub Med Coll Abbottabad. 2010;22(4):190–3.
Singh A, Rathore P. A comparative study of feto-maternal outcome in instrumental vaginal delivery. J Obstet Gynecol India. 2011;61(6):663–6.
Yurdakök M. Meconium aspiration syndrome: do we know? Turk J Pediatr. 2011;53(2):121.
Acknowledgment
We would like to acknowledge the University of Gondar College of medicine and health sciences and data collectors.
Funding
The author received funding for this specific research article from University of Gondar, Gondar, Ethiopia.
Author information
Authors and Affiliations
Contributions
Data curation, formal analysis, resources, software, validation, and visualization: Addisu Ginbu Dubie, Mehretie Kokeb, Abraham Tarkegn Mersha, Chilot Desta Agegnehu. The investigation, Methodology, supervision, conceptualization, analysis, and interpretation writing a detailed review, editing, and preparing manuscript: Addisu Ginbu Dubie, Mehretie Kokeb, Abraham Tarkegn Mersha, Chilot Desta Agegnehu. Finally, all the authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional review board of the college of medicine and health science, University of Gondar. Permission of a written letter was obtained from University of Gondar Comprehensive Specialized Hospital administrators. Informed consent was taken from the parent or legal guardian. The data collected was kept confidential and only used for the study purpose. All methods were carried out following relevant guidelines and regulations.
Consent for publication
It is not applicable.
Competing interests
All authors declare that they have no competing interest final content of the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dubie, A.G., Kokeb, M., Mersha, A.T. et al. Prevalence and associated factors of perinatal asphyxia in newborns admitted to neonatal intensive care unit at the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia, Ethiopia. BMC Pediatr 21, 525 (2021). https://doi.org/10.1186/s12887-021-03019-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-021-03019-x