Abstract
Background
The fat mass estimators waist-to-height ratio (WHtR) and relative fat mass—pediatric (RFMp) complement the widely accepted body mass index (BMI) in obesity evaluation. Aims of the Study: Conduct an easy appraisal of trunk fat and the cardiometabolic risk associated with pediatric obesity.
Methods
A total of 472 children (39% boys in the total sample) were classified as underweight, normal weight, overweight or obese (nutritional groups, NGs) according to BMI Z-score after initial anthropometric data were obtained and ad hoc exclusion criteria were applied. WHtR and RFMp (% of total fat) were calculated for each group, associations were assessed through multiple linear regression (MLR), and differences between sexes were evaluated (medians, IQR).
Results
The mean age (mean (95% CI)) was 10.8 y (10.1–11.1). The values in the total sample were as follows: WHtR, 0.5 (0.49–0.51) and RFMp%, 32.3 (31.7–33.0). In the overweight group, the values were as follows: WHtR, 0.51 (0.50–0.52) and RFMp(%), 34.2 (33.3–35.1). In the obese group, the values were as follows: WHtR, 0.56 (0.55–0.57) and RFMp(%), 37.8 (36.9–38.6). The associations were as follows (NG; independent variables): In the NG, adjusted R2 values were between 0.74 and 0.78. In the total sample, the beta coefficient was 3.36 (P < 0.001) for RFMp for girls; for waist circumference (WC), the beta coefficient was 2.97 (P < 0.001), and for WHtR the beta coefficients were − 0.01 (p < 0.001) and 0.03 (p < 0.001),for girls and for WC respectively.
The sex differences were as follows: BMI exhibited no differences in the NG (Mann-Whitney U). WHtR (median (IQR)) differed (M vs. F) in the total sample (0.49 (0.45–0.54) vs. 0.52 (0.45–0.56), p < 0.004); in the overweight group (0.51 (0.48–0.53) vs. 0.54 (0.51–0.55), p < 0.001); and in the obese group (0.55 (0.52–0.57) vs. 0.57 (0.54–0.60), p < 0.004). RFMp (%) differed in the total group (29.21 (24.27–32.92) vs. 36.63 (30.2–39.51), p < 0.001); in the overweight group (31.24 (28.35–32.35) vs. 37.95 (35.75–38.82), p < 0.001) and in the obese group (35.89 (32.05–36.15) vs. 40.63 (38.27–42.42), p < 0.001).
Conclusions
WHtR and RFMp are simple and reliable indices that do not require centile charts. Their values, including waist circumference, can be used to estimate the different trunk fat components in boys and girls better than BMI, especially if individuals are overweight or obese. RFMp proved to be more reliable as it considers sex. Both should be included in routine anthropometric readings.
Similar content being viewed by others
Introduction
Excessive abdominal fat deposition is associated with obesity-related comorbidities in adults [1–3] and children and adolescents [4, 5]. Among children and adolescents, the most common consequences are elevated blood pressure and subtle metabolic disturbances, among the numerous and coexistent clinical deviations that may appear inconspicuously at these early moments. Body mass index, whether expressed as a Z-score or percentage (BMI Zs, BMI %), is a widely accepted measure to identify malnutrition in pediatric groups, but BMI cannot indicate present or future cardiometabolic risks in overweight or obese children; in contrast, in adults, waist circumference readings are favored [6]. Body composition is different between children and adults and is modified by obesity; assessing these changes is complex. T G Lohman in 1989 [7] described that these quantitative fat differences can be estimated by anthropometry, body density and bioimpedance methodology; regarding the latter [8], bioimpedance was used to estimate the fat-free mass in children and in adults according to sex and ethnicity. Moreover, through air displacement plethysmography [9], a young population (< 19 years) was studied and was also assessed on the same day with dual X-ray absorptiometry (DXA). Ten years later, [10] as DXA gained precision in the assessment of body composition, the use of some previous methods (underwater weight) and devices (Omron) was decreasing. Positron emission tomography-computed tomography (PET-CT), particularly magnetic resonance imaging (MRI), allows also the assessment of bone and muscle in studies [11]. Currently, in addition to the heritability of body composition [12], the previously described methods for studying body composition are still in use, but improved methodology has made a selection of them available for use in both research and clinical settings. Therefore, interest in using simple tests based on waist circumference that have shown a reasonable association with cardiovascular risks in children [13] and adolescents [14] and have been associated with the mentioned accurate methods of estimation of fat mass percentage has been increasing [15].
The prevalence of abdominal obesity is not very well known in pediatric groups because different methods (and names) are used to assessing abdominal obesity; the most common method is likely, dual X-ray absorptiometry (DXA) (central fat’ or ‘trunk fat’). Computed tomography and magnetic resonance imaging are considered the gold standard for quantitative measurement of abdominal adipose tissue compartments (visceral subcutaneous, etc.), although they are less frequently used due to minimal but significant radiation exposure and cost. Anthropometry is considered the basic and straightforward method, and pure waist circumference, apart from the far more commonly assessed BMI, is measured at each visit. Furthermore, abdominal fat increases as the child grows. After extensive research in adults [16, 17] evidencing an association of abdominal obesity with and/or predictive capacity for cardiometabolic conditions, waist circumference percentiles [18, 19] and diverse derived equations appeared in the pediatric obesity preventive literature. Of these, the waist-to-height ratio (WHtR) and relative fat mass—pediatric (RFMp) were selected for assessment in the present study. A WHtR [20] greater than 0.5 is associated with most health risks occurring in obese adults, even in subjects identified as normal weight. A value ≥0.5 has also been accepted for children and adolescents for the estimation of abdominal obesity. In the context of relative fat mass (RFM), obesity risks depend on an elevated ratio of adipose tissue mass to total body weight. Therefore, precise estimation of body fat percentage is relevant. RFM better predicts whole-body fat percentage measured by DXA in males and females. RFM was developed in a large study on adults [21] RFM—pediatric (RFMp) has been developed also [22]. RFMp is also an estimator of fat mass percentage based on the height/waist ratio with the presumed advantage of considering sexes separately and has exhibited close agreement with DXA measurements. Therefore, RFMp can quickly provide an idea of fat content not only at initial diagnosis but also over the course of long-term obesity follow-up.
Our hypothesis was as follows: because the correlations of trunk fat estimators with matched DXA data have been established, we hypothesize that WHtR and RFMp are elevated in pediatric overweight and obese individuals, thus signaling cardiometabolic risk in both sexes.
The aim of this study was to determine whether these clinically matched estimators can provide information about the (trunk) fat content in addition to the information provided by globally recognized BMI in children with different nutritional statuses (underweight, normal weight, overweight and obese), especially signaling fat difference thresholds by sex.
Methods
Study design
Secondary analysis of exclusively initial diagnostic measures of patients attending the Pediatric Institute for Nutrition, Growth and Metabolism Clinical Unit of the University Hospital was conducted. Participants: A total of 472 (185 boys) children and adolescents aged 10.8 years (95% CI 10.1–11.1) were classified into nutritional groups according to their BMI Z scores as underweight (UW, < − 1 SD), normal weight (NW, − 1 to + 1 SD), overweight (OW, + 1 to + 2 SD) and obese (OB, > 2 SD). Age and sex subgroups were also studied. These baseline data came from patients attending the unit between 2014 and 2018. All of the participants were followed and cared for under the direction of this unit. Children with incomplete somatic data, low school performance, atypical social status and chronic conditions were excluded (n = 27).
Intervention
According to the established rules of the unit, the following anthropometric measures were taken by specialized and specific personnel: height (Harpenden stadiometer, Holtain Limited, Harpenden UK), weight (electronic scales), waist circumference (inextensible tape) and blood pressure (GE Carescape tm, V100, Dinamap Technology, Freiburg, Germany, two pressure cuffs). For waist circumference (WC), we followed the recommendations of the WHO [23] but with pediatric precautions as follows: the child was in a standing position, and the tape was horizontally placed at the midpoint between the lower costal margin and upper anterior iliac apophysis. The tape was not too tight or too loose and reading to the nearest 0.1 cm at the end of exhalation was obtained, but before recording the result, changes in the centimeter readings were assessed (left to right) with respiratory movements. All measures were taken in an acclimatized room where children were in light underwear and barefoot, always in the morning and after a light continental breakfast. For height and WC, all readings were in centimeters and centiles, and Z scores were obtained through the anthropometric program based on IOTF standards. BMI % was also assessed according to the Poskitt definition [24]. Target height ([25] Molineri 1984) was assessed as midparental height ± 6.5 cm for both boys and girls. WHtR is a unitless ratio. RFMp was calculated according to pediatric equations [26], and the results express the estimated percentage (%) of total body fat:
RFMp (for 8 to 14 years) = 74 – (22 x height/waist) + (5 x sex);
RFMp (for 15 to 19 years) = 64 – (20 x height/waist) + (12 x sex).
Note that for both equations, sex implies male 0 and female 1, and the results are given [26] as percentages. Because there is no definition of obesity based on body fat percentage, we used NHANES data matched to DXA as a reference (22), where figures greater than 29% for boys and 41% girls would indicate high body fat percentage. In our sample, values very close to the nutritional groups defining limits were obtained (Table 1), indicating the association of overweight with greater abdominal adiposity (trunk fat).
BMI Z scores were selected as a general and widely accepted model but did not include waist circumference, whereas WHtR and RFMp provided an idea of trunk fat.
Ethics
The applied procedures were conducted in accordance with the standards of the institutional Ethics Committee and with the Declaration of Helsinki (1964; 2000). The study was approved by our Institution Ethics Committee.
Statistical analysis
A descriptive analysis was performed, and the mean and standard deviation or 95% confidence interval or median and interquartile ranges (IQRs) are provided for quantitative variables according to the previous results of a normality test. For categorical data, absolute values and percentages were applied. A univariate analysis by the Mann–Whitney U test to assess sex differences in estimated fat percentages was also applied to dependent and independent variables, as shown below. Correlation studies were conducted to assess the linear relationship among the dependent and continuous covariates. A multivariate study was conducted to assess the relationships of covariates (sex, BMI Zs, waist circumference (WC Zs), birth weight (BW Zs), systolic and diastolic blood pressure) with dependent variables (WHtR and RFMp). Next, the B (Beta) coefficient was obtained for each dependent variable in five models, four according to every BMI group and the fifth comprising all participants without any stratification. Stata Biostatistical Program, SSS version 15, 2017, was used, and a P value < 0.05 was considered significant. The findings of this study should be considered exploratory and/or descriptive.
Results
Table 1 shows the values for the main clinical data of the total sample and the following nutritional status groups: underweight, normal weight, overweight and obese. The total sample was considered because of the potential association of estimators with a wider range of BMIs. All nutritional groups included both sexes, and their clinical values are shown according to BMI nutritional categories. It is worth noting the narrow 95% confidence interval for all values. RFMp varied from 22.3% in the underweight group to 37.8% in the obese group, and WHtR and waist circumference Z scores also exhibited narrow ranges in agreement to their nutritional status.
Because of the higher values of body fat percentage in females, Table 2 shows the different degrees of association of sex with fat estimators in the analyzed groups. As expected, no sex difference appeared for the BMI Z value, as it was used as a primary categorizer for underweight, overweight and obesity among the total sample of children with a mean age of 10.8 years (95% CI 10.5–11.1), but these Z score values (Table 1) provide baseline data related to fat mass differences. WC Z scores were higher and exhibited significant levels in girls in all groups, even in the underweight group (p < 0.004). Concerning (trunk) fat mass estimators, WHtR was greater in girls than in boys in the total sample (p < 0.004), specifically in the overweight (p < 0.001) and obese groups (p < 0.004). RFMp showed differences in the total sample and the normal weight, overweight and obese groups, with higher values in females (p < 0.001). All these sex differences were observed with no differences in BMI within the groups, suggesting it is worth considering that fat plays a role in body weight in addition to other components.
The associations of trunk fat estimators (WHtR and RFMp) with the groups and with the main independent variables in these groups are shown in Table 3. This was evaluated in two ways. First, the adjusted coefficient of determination (aR2, table first column in both estimators) was considered. In the case of WHtR, the aR2 values explained its association with the BMIs that characterize each group, ranging from 0.88 in the total sample to 0.007 in the underweight group. When considering aR2 for RFMp, the association in all studied groups ranged from 0.87 in the total sample to 0.57 in the underweight group, signaling a certain advantage of this latter estimator; both estimators explained nearly 88% of the outcomes. Second, in the multivariate study (subsequent columns in Table 3), regarding the B coefficient, as clearly appears in the case of WHtR values, the associations with the six variables analyzed in each nutritional status group were weaker, indicating a weaker association with some variables, especially birth weight and systolic and diastolic blood pressure. As expected for RFMp, the B coefficient had high values for sex in the four nutritional groups and the total sample, ranging from 3.77 in the obese group to 4.58 in the underweight group and 3.36 in the total sample, signaling greater values for girls regardless of nutritional group to which they belonged, thus indicating a significant association with trunk fat.
Standard correlation matrix: In the normal weight group, BMI was correlated with trunk fat estimators; the strongest association was found for WHtR (r = 0.63; p < 0.001) and RFMp (r = 0.58, P < 0.001). These trends were maintained in the overweight and obese groups. The correlation matrix values did not show any further remarkable findings.
Discussion
The main findings of this study are as follows: 1) Waist circumference (WC), waist-to-height ratio (WHtR) and relative fat mass—pediatric (RFMp) can be used to estimate truncal fat because the models used indicate that their change is associated with the six analyzed independent variables (Table 3); this association was moderately stronger in the total sample, consequently adding valuable information to the BMI estimative capacity of body fat content. 2) The estimators exhibited differences between boys and girls in all nutritional groups, whereas BMI did not exhibit differences. The nonstatistical significance, in the case of BMI according to one of the statistical principles [27], cannot be interpreted as equality, as this was a primary idea in this study. 3) Mean values and uncertainty ranges of estimators were obtained in each nutritional group.
The risk associated with excessive trunk fat was described in the mid-1900s in adults [28], stressing the importance of the body shape of the individuals. These risks were shown later in the context of a wide range of comorbidities. Paradigmatic examples are the associations with type 2 diabetes [29, 30], hyperuricemia [31], elevation of free T3 and MRI-assessed abdominal fat distribution [32], heart failure mid-range ejection fraction [33], and even prevalent or previous metabolic syndrome. These relationships were established by means of different waist circumference-derived indices [34]. It is worth referring to the conclusions of Baton Rouge [35] regarding the analysis of these various equations; although the waist circumference index is preferred, capacity of indices for evaluating an individual person’s health risks were considered. To improve feasibility, other waist-height indices may be useful [36] and have already been tested in different geographic areas in children as cardiometabolic risk factors [37]. More specifically and due to the simplicity and reliability of measures, WHtR was chosen for assessing central adiposity in children in a remote South Pacific archipelago [38]. With the present-day understanding of pediatric obesity risks, it is worth considering that these elevated trunk fat markers are associated with the main biochemical markers of insulin resistance and inflammatory and metabolic abnormalities [39]. The clinical approach of analyzing trunk fat has led to the assessment of 17,000 participants with BMI < 25 kg/m2 but with excessive body fat [40]. In children and young people, the estimation of trunk fat by proxy methods has been slow due to the varied charts for waist circumference despite the publications of McCarthy [41, 42] facilitating Z score calculation. More recent publications [18, 43] included international centile cutoffs, but nevertheless, truncal assessment has not reached the accepted level of BMI in a clinical setting. Waist circumference is still considered a reliable measure for assessing abdominal obesity [44], especially in countries with uneven care distribution, and in others with better conditions, its evaluation is the first or preliminary step prior to subsequent more precise tests [45].
Waist-to-height ratio
WHtR in adults was proposed in 1995 in Japan by SD Hsieh and almost simultaneously in the UK by M Ashwell [20], demonstrating that ratios > 0.5 were strongly associated with myocardial ischemia and metabolic risk factors (T2D). This association has also been described in children and adolescents elsewhere [46, 47]. Other variants of this ratio [48] are not widely used. In adolescents in the AVON longitudinal study [14] that included nearly 3000 children followed over 8 years, ratios > 0.5 were associated with elevated fasting blood lipids, glucose, insulin and blood pressure in boys (OR 6.8; 95% CI 4.4–10.6) and girls (OR 3.8; 95% CI 2.3–6.3), and the associations of this ratio once established were highly specific compared to those of BMI. Similar results were shown in a systematic review and meta-analysis [49]. Consequently, WHtR could be considered a simple and reliable first step in risk assessment.
Relative fat mass—pediatric (RFMp)
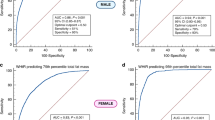
As mentioned, Woolcott and Bergman [21] derived an equation from adult height/waist for estimation of whole-body fat percentage and later developed an equation for children and adolescents [22], which was assessed according to DXA values. The novelty of this estimator is the sex consideration, which decreases the rate of misclassification of relative fat mass due to a more precise diagnosis of obesity/adiposity in females. This equation has been tested in other parts of the world [50, 51] in adult populations and in adolescents [52]. In our study, the initial correlation with BMI as the major standard criterion for overweight and obesity classification was significant in the whole sample and normal weight groups, but in the overweight and obese groups, the degree of correlation slightly decreased, which was in agreement with the next multiple regression finding. This fact is interesting because waist circumference does not intervene in the measurement of BMI and would be more related to body or trunk fat than BMI. The normal distribution and density of RFMp in this study could provide adequate conditions for future analyses (Fig. 1).
Multiple linear regression
The high aR2 values are indicative of the appropriateness of the estimators used, but since they are below 90% (predictive capacity), they should be considered indicative of association mainly for females and waist circumference and, to a lesser extent, BMI Z scores. Specific analyses of nutritional statuses revealed that in the total sample, among individuals with greater fat deposit (obese) and the lowest fat deposit (underweight), an association between sex and RFMp was found; the regression B coefficients implied that girls have an RFMp 3.36 units higher than boys, or in the case of WC Z scores, each unit of increment implies an increase of 2.97 in the RFMp. This associative trend was very similar and regular in the normal weight, overweight and obese groups. All of these findings indicate greater precision than that of BMI Z score, basically because BMI does not consider waist circumference, which is also manifested through its lower coefficients (Table 3). For WHtR, these associations remain at a lower level but maintained their p values; therefore, the simplicity of its calculation (ratio waist/height) and its well-proven threshold of 0.5 make it an efficacious screening tool.
In the underweight group (7.4% of the total sample), all children were discreetly affected (BMI Zs − 1.35 SD; 95% CI − 1.46 to − 1.24), with a minor reduction in target height (− 0.05 SD; 95% CI − 0.23 to 0.25) in 20 instances where both progenitors were measured, suggesting potential familial undernutrition; furthermore, their social level could not be considered as of lower class. Inclusion in the study was motivated to assess the estimators’ behavior on the opposite side of the spectrum of overweight.
Regarding sex, in all nutritional groups, BMI did not show differences between sexes; conversely, the estimators clearly did, as weight apart from fat comprises nonfat body components that veil adiposity. This would justify the increasing values of RFMp in the normal, overweight and obese groups; again, this no difference occurs with BMI Z scores in both boys and girls. The median RFMp was significantly higher in girls than in boys, sharing the same classificatory BMI range in all groups (regardless of the BMI category), which is probably in agreement with the higher fat content in girls at this age [22], consequently giving an idea of abdominal fat.
Furthermore, DXA studies revealed a greater proportion of fat in girls, particularly when they reach puberty [53, 54]. This association with DXA was already studied by us [55] in 142 overweight and obese individuals with an average age (mean, 95% CI) of 11.5 (10.3–11.8) years, with no differences between boys and girls in age or BMI Z score; furthermore, in that study, we found a relationship between %trunk fat and sex—42.2% (40.3–44.1) in boys versus 45.8% (43.7–47.8) in girls (p = 0.001)—and for waist circumference (WC) Z score—1.9 (1.7–2.2) in boys versus 2.4 (2.1–2.8) in girls (p = 0.001); the regression analysis between WC and %trunk fat revealed a regression coefficient of β = 2.9 for WC (P = 0.001). Thus, there is a need to study sexes separately in pediatric obesity studies.
Blood pressure
Only a weak relationship of diastolic blood pressure with RFMp (r = 0 .206, p < 0.001) appeared in the total sample. Despite well-established policies for BP measurement in the clinical area of this unit with an elevated blood pressure section [56], the results are not as consistent as those of other clinical parameters, and doubts about BP screening [57, 58] probably not only apply to these data but also lead to reconsidering these policies.
Present techniques allow abdominal fat to be measured separately from subcutaneous fat in children [59, 60], but this may not be an available method for evaluation of the growing double burden of malnutrition in low- and middle-income countries (LMICs), so it is important to look for proxy estimators. Furthermore, proxy measures are useful even when DXA is available but cannot be justified at every follow-up visit. Therefore, and after firm association of estimators based on waist circumference and trunk fat, we recommend that the studied estimators be used because of their safety, simplicity [61], known low variability [62] and good correlation with CT and MRI [63] when assessing metabolically unhealthy fat accumulation [3, 64] and furthermore to increase precision by considering sex [55] and age if assessing a diverse sample [65, 66, 67].
Limitations
Using accurate standardized anthropometric data, we assessed the potential advantages of WHtR and RFMp without a specific design for child obesity studies [68]. As females were predominant (286/472, 60.6%), the subsequent higher proportion in the study groups could be a confounding factor, and it was not possible to perform validation [69]. Therefore, another weak point is the lack of a precise comparison, such as DXA, but in this case, the aim was to assess diagnostic performance of anthropometry for nutritional deviations, some of them not requiring more complex techniques with side effects.
Conclusions
The calculation of WHtR is a very simple and reliable method that does not require reference growth centile charts; consequently, it should be the first step in screening, while RFMp gives an idea of the body (and trunk) fat content in both sexes. Both could indicate cardiometabolic consequences that are already present or that could occur in the near future, especially if the values increase during the follow-up. At present, BMI Z score is considered the most widely used marker for overweight and obesity (while BMI percentage is better understood by patients and their families); hence, to increase clinical accuracy, both estimators should be added as routine anthropometric measurements in primary health care settings and in specific surveys.
Availability of data and materials
The generated dataset is available from the corresponding author on reasonable request.
Abbreviations
- BMI%:
-
Relative body mass index
- MLR:
-
Multiple linear regression
- NGs:
-
Nutritional groups
- OB:
-
Obese
- OW:
-
Overweight
- RFMp:
-
Relative fat mass index—pediatric
- WC:
-
Waist circumference
- WHtR:
-
Waist-to-height ratio
References
Centre for Disease Control and Prevention. More than a third of adults estimated to have prediabetes. http://www.cdc.gov/media/releases/2011/p0126_diabetes.html
Gupta P, Lanca C, Gan ATL, Soh P, Thakur S, Tao Y. The association between body composition using dual energy X-ray absorptiometry and type 2 diabetes: a systematic review and meta-analysis of observational studies. Sci Rep. 2019;9(1):12634. https://doi.org/10.1038/s41598-019-49162-5.
Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes & Endocrinol. 2020;8(7):616–27.
Kim G, Divers J, Fino NF, Dabelea D, Lawrence JM, Reynolds K. Trends in prevalence of cardiovascular risk factors from 2002 to 2012 among youth early in the course of type 1 and type 2diabetes. The SEARCH for diabetes in youth study. Pediatr Diabetes. 2019;20(6):893–701.
Hwang J, Kim JY. Nonalcoholic fatty liver and abdominal fat accumulation according to vitamin D status in patients with type 2 diabetes. J Obes Metab Syndr. 2018;27:125–7.
Ross R, Neeland IJ, Yamashita S, Shai I, Seidel J, Magni P. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nature Reviews Endocrinology 04 Feb 2020, doi: https://doi.org/10.1037/s41574-019-0310-7.
Lohman TG. Assessment of body composition in children. Pediatr Exerc Sci. 1989;1:19–30.
Heyward VH. Practical body composition assessment for children, adults and older adults. Int J Sport Nutr Exerc Metabolism. 1998;8(3):285–307. https://doi.org/10.1123/ijsn.3.285.
Nuñez C, Kovera AJ, Pietrobelli A, Heshka S, Horlick M, Kehayias JJ. Body composition in children and adults by air displacement plethysmography. Eur J Clin Nutr. 1999;53(5):382–7. https://doi.org/10.1038/sj.ejcn.1600735.
Jensky-Squires NE, Dieli-Conwright CM, Rossuello A, Erceg DN, McCauley S, Schroeder ET. Validity and reliability of body composition analysers in children and adults. British J Nutrition. 2008;100:859–65.
Dr W, Leonard MB, Zemel BS. Body composition analysis in the pediatric population. Pediatr Endocrinol Rev. 2012;10(1):130–9.
Brener A, Waksman Y, Rosenfeld T, Levy S, Peleg I, Raviv A. The heritability of body composition. BMC Pediatr. 2021;21(225). https://doi.org/10.1186/s12887-021-02695-z.
Hardy LL, Xu J, Guo CZ, Garnett SP. 30-year cross-sectional trends in waist-to-height ratio in Australian school age children: 1985to 2015. Acta Pediatr. 2019;108(4):707–11.
Graves L, Garnett SP, Cowell CT, Baur LA, Ness A, Sattar N. Waist-to-height ratio and cardiometabolic risk factors in adolescence: findings from a prospective birth cohort. Pediatric Obesity. 2013;9:327–38.
Sijtsma A, Bocca G. L’Abée C, Liem ET, Sauer PJJ. Waist-to-height ratio, waist circumference and BMI as indicators of percentage fat mass and cardiometabolic risk factors in children aged 3-7 years. Clin Nutr 2014; 33: 311–315.
Zhang L, Wang Z, Wang X, Chen Z, Shao L, Dong Y. Prevalence of abdominal obesity in China: Results from a cross-sectional study of nearly half million participants. Obesity 24 Sep 2019 doi: https://doi.org/10.1002/obby.22620.
Sedlmeier AM, Baumeister SE, Weber A, Fisher B, Thorand B, Ittermann T, et al. Relation of body fat mass and fat-free mass to total mortality: results from 7 prospective cohort studies. Am J Clin Nutr. 2021;113:639–46.
Xi B, Zong X, Kelishadi R, Litwin M, Hong YM, Poh BK. International waist circumference percentile cut-offs for central obesity in children and adolescents aged 6–18 years. JCEM 14 Nov 2019, doi: https://doi.org/10.1210/clinem/dgz195.
Shah M, Radia D, McCarthy HD. Waist circumference centiles for UK South Asian children. Arch Dis Child 2018; 105(1), doi: https://doi.org/10.1136/archdischild-2018-315722.
Ashwell M, Gibson S. A proposal for a primary screening tool: ‘keep your waist circumference to less than half your height. BMC Med. 2014;12:207–12.
Woolcott OO, Bergman RN. Relative fat mass (RFM) as a new estimator of whole-body fat percentage—A cross-sectional study in American adult individuals. Scientific Reports 20 Jul 2018; 8: 10980, doi: https://doi.org/10.1038/s41598-018-29362-1.
Woolcott OO, Bergman RN. Relative fat mass as an estimator of whole-body fat percentage among children and adolescents: a cross-sectional study using NHANES. Sci Rep. 2019;9:15279. https://doi.org/10.1038/s41598-019-51701-z.
World Health Organization. Waist circumference and waist-hip ratio: report of a WHO expert consultation. Geneva, 8–11 Dec 2008. Publication date 2011.
Poskitt EME. Practical pediatric nutrition. Tiptree: Butterworth & Co; 1988. p. 254.
Molineri L, Largo RH, Prader A. Target Height and Secular Trend in the Swiss Population. In Borms J, Hauspie R, Sand EA (eds). Human Growth and Development 1984 Springer Boston MA (p 193); doi: https://doi.org/10.1007/978-1-4757-0743-4_21
Woolcott OO, Bergman RN. Defining cutoffs to diagnose obesity using the relative fat mass (RFM): association with mortality in NHANES 1999-014. Int J Obes. 2020. https://doi.org/10.1038/s41366-010-0516-8.
Young PJ, Nickson CP, Perner A. When should clinicians act on non-statistically significant results from clinical trials? JAMA online may 8; 2020. https://doi.org/10.1001/jama.2020.3608.
Vague J. The degree of masculine differentiation of obesities: A factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. 1956. Obes Res. 1996;4(2):204–12.
Fan Y, Wang R, Ding L, Meng Z, Zhang Q, Shen Y. Waist circumference and its changes are more strongly associated with the risk of type 2 diabetes than body mass index and changes in body weight in Chinese adults. J Nutrition. 2020;150(5):1259–65.
Elizalde-Barrera CI, Rubio-Guerra AF, Lozano-Nuevo JJ, Olvera-Gomez JL. Triglycerides and waist to height ratio are more accurate than visceral adiposity and body adiposity index to predict impaired fasting glucose. Diabetes Res Clin Pract. 2019;153:49–54.
Huang Z, Huang B, Zhang H, Zhu M, Zhu H. Waist-to-height ratio is a better predictor of hyperuricemia than body mass index and waist circumference in Chinese. Ann Nutr Metab. 2019. https://doi.org/10.1159/000504282.
Nie X, Xu Y, Ma X, Xiao Y, Wang Y, Bao Y. Association between abdominal fat distribution and free triiodothyronine in a euthyroid population. Obesity Facts June 5 2020, doi: https://doi.org/10.1159/000507709.
Gao F, Wan J, Xu B, Wang X, Lin X, Wang P. Trajectories of waist-to-hip ratio and adverse outcomes in heart failure with mid-range ejection fraction. Obesity Facts. 2020. https://doi.org/10.1159/000507708.
Rico-Martin S, Calderon-Garcia JF, Sanchez-Rey P, Franco-Antonio C, Martinez-Alvarez M, Sanchez Muñoz-Terrero JF. Effectiveness of body roundness index in predicting metabolic syndrome: A systematic review and meta-analysis. Obesity Reviews 08 Apr 2020, doi: https://doi.org/10.1111/obr.13023.
Hwaung P, Heo M, Kennedy S, Hong S, Thomas DM, Shepherd J. Optimun waist circumference-height indices for evaluating adult adiposity: An analytic review. Obes Rev Jan 21 2020, doi:https://doi.org/10.1111/obr.12947.
Hwaung P, Heo M, Kennedy S, Thomas D, Shepherd, Heymsfield S. Adjusting waist circumference for stature: Perspective on Ashwell and Gibson comments. Obesity Reviews 09 June 2020, doi: https://doi.org/10.1111/obr.13072.
Ejtahed HS, Kelishadi R, Hasani-Ranjbar S, Angoorani P, Motlagh ME, Shafiee G, et al. Discriminatory ability of visceral adiposity index as an indicator for modeling cardio-metabolic risk factors in pediatric population: the CASPIAN- V study. J Cardiovasc Thorac Res. 2019;11(4):280–6.
Dancause KN, Vilar M, Chan C, DeHuff C, Wilson M, Soloway LE. Patterns of childhood and adolescent overweight and obesity during health transition in Vanuatu. Public Health Nutr. 2011;15(1):158–66.
Higgins V, Omidi A, Tahmasebi H, Asgari S, Gordanifar K, Nieuwesteeg M, et al. Marked influence of adiposity on laboratory biomarkers in a healthy cohort of children and adolescents. J Clin Endocrinol Metab. 2020;105(4). https://doi.org/10.1210/clinem/dgz161.
Ohlsson B, Manjer J. Sociodemographic and lifestyle factors in relation to overweight defined by BMI and ‘Normal-weight obesity’. J Obesity. 2020. https://doi.org/10.1155/2020/2070297.
McCarthy HD, Jarret KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0-16.9 y. Eur J Clin Nutr. 2001;55:902–7.
McCarthy HD, Ellis SM, Cole TJ. Central overweight and obesity in British youth aged 11-16 years: cross sectional surveys of waist circumference. BMJ. 2003;326. https://doi.org/10.1136/bmj326.7390.624.
Hassapidou M, Tzotzas T, Makri E, Paglos I, Kaklamanos I, Kapantais E, et al. Prevalence and geographic variation of abdominal obesity in 7- and 9-year-old children in Greece; World Health Organization childhood obesity surveillance initiative 2010. BMC Public Health. 2017;17:126–40.
Kryst L, Woronkowicz A, Kowal M, Pilecki MW, Sobiecki J. Abdominal obesity screening tools in the aspects of secular trend. Anthropol Anz. 2016;73(4):295–312.
Palmieri VJ, Henshaw MH, Carter J, Chowdhury SM. Assessing truncal obesity in predicting cardiometabolic risk in children: clinical measures versus dual-energy X-ray absorptiometry. Acta Pediatrica. 2018;107:1065–9.
Frayon S, Cavaloc Y, Wattelez G, Cerrier S, Lerrant Y, Ashwell M. Potential for waist-to-height ratio to detect overfat adolescents from a Pacific Island even those within the normal BMI range. Obes Res Clin Pract. 2018;12(4):351–7.
Fredriksen M, Skär A, Mamen A. Waist circumference in 6-12-year-old children: the health oriented pedagogical project (HOPP). Scand J Public Health. 2018;46(21 suppl):12–20.
Hwaung P, Heo M, Kennedy S, Hong S, Thomas DM, Shepherd J, et al. Optimum waist circumference-height indices for evaluating adult adiposity: An analytic review. Obesity Reviews. 2019. https://doi.org/10.1111/obr.12947.
Alves CA Jr, Mocellin MC, ECA G, Silva DA, Trindade EB. Anthropometric indicators as body fat discriminators in children and adolescents: a systematic review and meta-analysis. Adv Nutr. 2017;8(5):718–27.
Paek JK, Kim J, Kim K, Lee SY. Usefulness of relative fat mass in estimating body adiposity in Korean adult population. Endocr J. 2019;66(8):723–9.
Guzman-Leon AE, Velarde AG, Vidal-Salas M, Urquijo-Ruiz LG, Caraveo-Gutierrez LA, Valencia ME. External validation of the relative fat mass (RFM) index in adults from north-West Mexico using different reference methods. PLoS One. 2019;14(12):e0226767.
Ripka WL, Orsso CE, Haqq AM, Prado CM, Ulbricht L, Leite N. Validity and accuracy of body fat prediction equations using anthropometrics measurements in adolescents. Eat Weight Disord 19 May 2020, doi: https://doi.org/10.1007/s405119-020-00918-3
Guo B, Wu Q, Gong J, Xiao Z, Tang Y, Shang Y et al. Gender difference in body fat for healthy Chinese children and adolescents. Childhood Obesity 23 Mar 2016, doi: https://doi.org/10.1089/chi.2015.0139.
Denker M, Danielson A, Karlsson MK, Wollmer P, Andersen LB, Thorsson O. Total body fat, abdominal fat, body fat distribution and surrogate markers for health related to adipocyte fatty acid-binding protein (FABP$) in children. J Pediatr Endocrinol Metab. 2017;30(4):375–82.
Moya M, Juste M, Caturla J. Changes in adiposity estimated by dual energy x-ray attenuation (dxa) in obese pediatric patients. In: Sepiashvili R. Editor. Advances in allergy, asthma & immunology. From basic science to clinical management. World Forum of Pediatrics. Bologna (Italy), MEDIMOND. Moduzzi editore. 2010 p 179–184.
Bosch VM, Moya M, Espejo MP, Gutierrez J, Meca J. Blood pressure in schoolchildren and adolescents and its variation according to nutritional status evaluation: an early preventive key for obesity comorbidities. Obes Control Ther. 2015;2(2):1–6. https://doi.org/10.1526/2374-8354/2/2/00118.
US Preventive Services Task Force (USPSTF). Screening for High Blood Pressure in Children and Adolescents. US Preventive Services Task Force Recommendation Statement. JAMA 2020; 324(18): 1878–1883, doi: https://doi.org/10.1001/jama.2020.20122
Hanevold CD, Faino AV, Flynn JF. Use of automated office blood pressure measurement in the evaluation of elevated blood pressure in children and adolescents. J Pediatr Jul 4 2020, doi:https://doi.org/10.1016/j.jpeds2020.06.059.
Sadananthan SA, Tint MT, Michael N, Aris IM, Loy SL, Lee KJ, et al. Association between early life weight gain and abdominal fat partitioning at 4.5 years is sex, ethnicity, and age dependent. Obesity (Silver Spring). 2019;27(3):470–8.
Jaesche L, Steinbrecher A, Hansen G, Sommer S, Adler C, Janke J. Association of body surface scanner-based abdominal volume with parameters of the Metabolic Syndrome and comparison with manually measured waist circumference. Scientific Reports 2020; 10: art n° 9324.
Klipstein-Grobusch K, Boeing GH. Interviewer variability in anthropometric measurements and estimates of body composition. Int J Epidemiol. 1997;26(suppl 1):s174–80.
Danquah I, Addo J, Boateng D, Klipstein-Grobush K, Meeks V, Galbete C, et al. Early-life factors are associated with waist circumference and type 2 diabetes among Ghanaian adults: The RODAM Study. Scientific Reports. 2019. https://doi.org/10.1038/s41598-019-47169-6.
Hocking S, Samocha-Bonet D, Milner KL, Greenfield JR, Chisholm DJ. Adiposity and insulin resistance in humans: the role of the different tissue and cellular lipid depots. Endocr Rev. 2013;34:463–500.
Mauvais-Jarvis F, Merz NB, Barnes PJ, Brinton RD, Carrero JJ, DeMeo DL. Sex and gender: modifiers of health, disease, and medicine. Lancet. 2020;396:565–82.
Moya M. An update in prevention and treatment of pediatric obesity. World J Pediatr. 2008;4(3):173–85.
Moller G, Ritz C, Kjolbaek L, Vuholm S, Kellebjerg Korndal S, Meinert Larsen T, et al. Sagittal abdominal diameter and waist circumference appear to be equally good as identifiers of cardiometabolic risk. Nutr Metab Cardiovasc Dis. 2021;31(2):518–27.
Braunerová RT, Kunesová M, Heinen MM, Rutter H, Hassapidou M, Duleva V. et al. Waist circumference and waist-to-height ratio in 7-year-old children—WHO Childhood Obesity Surveillance Initiative. Obesity Reviews. 2021:e13208. https://doi.org/10.1111/obr.13208.
Brown AW, Altman DG, Baranowski T, Bland JM, Dawson JA, Dhurandhar NV, et al. Childhood obesity intervention studies: A narrative review and guide for investigators, authors, editors, reviewers, journalists and readers to guard against exaggerated effectiveness claims. Obesity Reviews. 19 Aug 2019. https://doi.org/10.1111/obr.12923.
Frongillo EA, Baranowski T, Subar AF, Tooze JA, Kirpatrick SI. Establishing validity and cross-context equivalence of measures and indicators. J Acad Nutr Dietetics. 22 Nov 2018. https://doi.org/10.1016/jand.2018.09.005.
Acknowledgments
Not applicable
Funding
None was received.
Author information
Authors and Affiliations
Contributions
MM designed the study, performed the data analysis and drafted the article. VP also performed the data and statistical analyses. Both authors thoroughly revised the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee for Research of the Hospital Universitario of San Juan de Alicante according to 1964 Declaration of Helsinki (Approval 10 March 2018). Because of the retrospective nature of the study, the requirement for informed consent was waived by the Ethics Committee because all retrieved data came from children’s medical records that were fully anonymized.
Consent for publication
Not applicable.
Competing interests
No financial or nonfinancial benefits have been received or will be received from any source or party.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Moya, M., Pérez-Fernandez, V. Estimating trunk fat in children according to sex using basic somatic readings: an opportunity for improving evaluation among girls. BMC Pediatr 21, 446 (2021). https://doi.org/10.1186/s12887-021-02918-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-021-02918-3