Abstract
Introduction
The occurrence of cardiovascular diseases and metabolic disorders steadily increases with the body mass index (BMI). Since the latter is not the best and earliest indicator of obesity and cardiovascular risk, the aim of the study was to evaluate some potential biological markers that would allow us to detect children and adolescents at higher risk at an early stage.
Methods
A sample of 330 children and adolescents were included in the study and divided into four groups: obese patients with hypertension, normal-weight patients with hypertension, patients with mildly elevated lipids and a control group of healthy children and adolescents. Some clinical parameters (age, body weight, body height, BMI, waist circumference, hip circumference, blood pressure), biochemical parameters (glucose, total cholesterol, triglycerides, HDL, LDL, apolipoprotein A1, homocysteine) and biological markers of obesity (ghrelin, adiponectin, leptin) were evaluated.
Results
Ghrelin and adiponectin were found to have a strong negative statistically significant correlation with BMI in all three observed groups (p < 0.001), but not in the control group (p = 0.053 and p = 0.316, respectively). In addition, leptin had a strong positive statistically significant correlation with BMI in all four groups (p < 0.001 for the research groups, p = 0.009 for the controls). In the group of obese patients with hypertension, statistically significant differences in all three markers of obesity were found in comparison to the control group (p < 0.001 for all markers). In the group of patients with mildly elevated lipids, ghrelin and leptin were significantly different (p = 0.002 and p < 0.001, respectively). In the group of normal-weight hypertensive patients, only values of ghrelin were different compared to the control group (p = 0.001).
Conclusion
In the research groups, significant differences were found in clinical, biochemical and biological parameters compared to the control group. The observed biological markers of obesity are useful early markers for identifying groups of patients that are at cardiovascular risk.
Similar content being viewed by others
Background
Obesity is a common disease in childhood that represents an epidemiological problem in some countries, including Slovenia [1, 2]. It is one of the significant cardiovascular risk factors associated with higher cardiovascular morbidity and other risk factors like hypertension and hyperlipidemia [1]. Moreover, it has been shown that obese children are more likely to stay overweight in adulthood and to experience cardiovascular diseases at an early age compared to their peers with normal weight [1]. Both hypertension and hyperlipidemia can also occur in children and are associated with the occurrence and cardiovascular outcomes in adulthood [3]. Numerous studies have found that cardiovascular morbidity and mortality increase with body mass index (BMI [2, 4]. Although BMI is used as a measure of obesity, it is not sensitive enough to detect early fat accumulation and early cardiovascular risk [5,6,7]. However, one of the crucial aims of preventive pediatrics is to detect children with higher cardiovascular risk at an early stage. Hence research is directed towards finding early markers of cardiovascular risk, including potential biological markers like leptin, ghrelin and adiponectin [4].
There has been a considerable amount of research on leptin, and less on adiponectin and ghrelin [8,9,10,11,12,13,14]. Obese children have high concentrations of leptin and low values of adiponectin, but their codependency has not yet been proven [8, 9]. In some studies, their correlations with anthropometrical parameters have been shown [8, 11]. Recently, the associations with metabolic syndrome have also been found, suggesting their potential for cardiovascular risk prediction [12]. In a few studies published on ghrelin, lower values have been revealed in obese children [10, 14]. In addition, its association with some cardio-metabolic factors has been shown [15].
The aim of the present study was to evaluate the potential role of some biological obesity markers as early cardiovascular risk factors. In addition, their correlations with BMI, a known marker of obesity, were investigated in three study groups (the hypertensive group, the obese hypertensive group, and the mild hyperlipidemia group).
Materials and methods
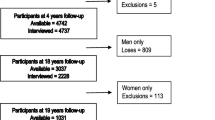
The study included 330 children and adolescents, aged from 8 months to 18 years, who were treated at our Department of Pediatrics. Patients were recruited prospectively, according to their risk factors. Body height and weight were measured to determine BMI. The Riva-Rocci method was used to measure blood pressure with appropriate cuff size (the bladder length covering 80%–100% of the circumference of the arm, the width at least 40%) and the first (phase I Korotkoff) and last (phase V Korotkoff) audible sounds to identify systolic and diastolic blood pressure, respectively. Fasting blood samples were used to assess leptin, adiponectin and ghrelin values. The levels of total adiponectin and leptin in the blood were measured using the quantitative sandwich enzyme immunoassay technique and the ghrelin level was measured using the sandwich ELISA method [16,17,18]. In addition, values of other biochemical cardiovascular risk factors were also measured from fasting blood serum using standard procedures (glucose − enzymatic hexokinase method, Siemens Dimension Vista; total cholesterol − cholesterol esterase enzymatic method, Siemens Dimension Vista; HDL and LDL cholesterol − homogenous direct method, Siemens Dimension Vista; triglycerides − enzymatic method, Siemens Dimension Vista; apolipoprotein A1 − nephelometric method, Siemens Healthineers Pro-Spec nephelometer; homocysteine − chemiluminiscent microparticle immunoassay, Abbott Architect 4000 SR) [19].
Children and adolescents were classified into four groups: obese patients with hypertension (92 patients), normal-weight patients with hypertension (104 patients), patients with mildly elevated lipids (99 patients) and a control group of 35 healthy children and adolescents. Obesity was defined as a BMI above the 95th percentile.
The data were statistically analyzed using IBM SPSS Statistics 22.0 with descriptive statistics (the mean values with the standard deviations), the Analysis of variance (ANOVA) tests with post hoc Bonferroni adjustment and bivariate correlations. The strength of correlation was defined by the Pearson coefficient (r), where a weak correlation ranged between 0 and 0.3, a moderate one with r between 0.3 and 0.7, and a strong correlation with r between 0.7 and 1. A significant statistical difference was defined as p < 0.05.
The research was approved by the institutional Ethical Committee.
Results
The characteristics of the four examined groups are shown in Table 1. Statistically significant differences according to the ANOVA post hoc Bonferroni adjusted tests between the control and the research groups are highlighted. Of note are the elevated values of both systolic and diastolic blood pressure that were also found in children with hyperlipidemia. There was no statistical difference in diastolic blood pressure in the other two research groups. In addition to children with elevated lipids, differences in some lipids were also found in the group of obese hypertensive children.
The correlations with BMI are displayed in Table 2, confirming correlations for all three research groups.
Correlations between BMI and all biomarkers in obese hypertensive patients are presented in Fig. 1.
In Table 3, the mean values of individual biological markers are highlighted and compared to the control group. Differences were found in all the study groups.
Correlation tests were made between researched biological markers (ghrelin, adiponectin, leptin) and other parameters in all the study groups (Table 4). Ghrelin and adiponectin significantly negatively correlated with age, anthropometric measurements including BMI, and systolic blood pressure in all three research groups. Diastolic blood pressure correlated negatively with both markers only in the group with mildly elevated lipids. Additionally, significant negative correlations were found between both markers and leptin in the group with mildly elevated lipids, between ghrelin and glucose, triglycerides and apolipoprotein A1 in the group with normal-weight hypertension, between both markers and homocysteine in both obesity-related hypertension and normal-weight hypertension. Ghrelin and adiponectin correlated positively with HDL-cholesterol in all three research groups. Furthermore, adiponectin correlated negatively with triglycerides and positively with both LDL-cholesterol and total cholesterol in the group with mildly elevated lipids. The positive correlation between adiponectin and both apolipoprotein A1 and ghrelin was also shown in all three groups.
The associations between leptin and researched parameters were less often significant. The positive correlations between leptin and all anthropometric parameters were found in both the obese hypertensive group and the mild hyperlipidemia group. In addition, leptin correlated positively with BMI, total cholesterol and triglycerides in the group with normal-weight hypertension, and with age, diastolic blood pressure, ghrelin and adiponectin in the mild hyperlipidemia group.
To emphasize, BMI was the only parameter that correlated significantly with all three biological markers, ghrelin, adiponectin and leptin, in all three research groups. Of note is the negative correlation found between systolic blood pressure and both ghrelin and adiponectin in all three research groups. For diastolic blood pressure, a correlation with all obesity markers was found only in the hyperlipidemia group. In addition, a positive correlation between ghrelin and adiponectin was shown in all the research groups.
In Figs. 2, 3 and 4, correlation factors between the biomarkers and other parameters are presented for all three research groups.
Discussion
In the current study, the potential role of some biological obesity markers as early cardiovascular risk factors was investigated in three groups of children and adolescents, patients with obesity-related hypertension, patients with mildly elevated lipids and patients with normal-weight hypertension. In all the research groups, their correlations with BMI, a known marker of obesity, were confirmed. The most promising biological marker was found to be ghrelin, proposed for early obesity and cardiovascular risk detection.
Comparison of individual groups with the control group of healthy children and adolescents showed no significant age differences, although there was a wide age range. In addition to significant differences in anthropometrical parameters in the obese hypertensive group, the results also showed differences in BMI as well as waist circumference in the other two research groups, indicating an impact of environmental factors [20]. Data from the group of patients with hypertension showed that they had mild hypertension, as the mean values of systolic blood pressure were 126.8 mmHg in normal-weight patients with hypertension and 128.3 mmHg in obese patients with hypertension. Similarly, the results of the lipid profile in the hyperlipidemia group showed that patients with mild metabolic disturbance were included. These are precisely the groups that require early markers of cardiovascular risk, indicating the importance of our results. Except for the group of patients with hypercholesterolemia, no statistically significant differences in diastolic blood pressure were found, confirming the findings in other studies investigating children with mild cardiovascular disturbances [21, 22].
Among biochemical parameters, the average values of total cholesterol, LDL cholesterol and triglycerides were higher in the groups of obese patients with hypertension and those with elevated lipids. HDL cholesterol was lowest in obese patients with hypertension. These parameters were therefore confirmed as significant risk factors in the obesity-related hypertension group, which is in agreement with previous studies [20, 23]. Glucose and homocysteine concentrations were comparable in all groups and did not differ from the control group.
All three investigated groups showed a statistically significant difference in the ghrelin concentration compared to the control group. In contrast, a statistically significant difference in the adiponectin concentration was found only in the group of obese patients with hypertension. The ghrelin concentration was lowest in obese patients with hypertension, which shows its negative correlation with obesity and obesity-related hypertension. This is in agreement with the results of previously published studies, proving a compensatory decrease in ghrelin when adipose tissue increases [14, 24]. However, some previous studies in children found no correlation between ghrelin and obesity-related hypertension, a correlation that was recently shown in adults [15, 25]. In addition, our finding of the role of ghrelin in normal weight hypertension has not been found in any previous studies in children. The concentration of adiponectin was highest in the healthy population and lowest in obese patients with hypertension, which has also been found in other studies [12, 26]. Leptin has been shown to be significantly different in the groups of obese patients with hypertension and patients with mildly elevated lipids. Therefore, we confirmed previous research proving its role in obesity [26, 27].
All the analyzed groups had a statistically significant positive correlation between leptin and BMI and a negative correlation between ghrelin and adiponectin and BMI, which are in accordance with earlier studies, thus confirming their potential for the determination of the obesity risk [8, 15, 26].
The codependent work of leptin and adiponectin has not yet been proven. Some studies found that the leptin/adiponectin ratio could be an important parameter in obesity [8]. However, other studies have shown that the parameters of children’s body structure are related to leptin, but not to adiponectin [13]. In the present study, their correlation was found only in the group of patients with hyperlipidemia. The same was found for the correlation of leptin and ghrelin. Some studies proposed that leptin affects blood ghrelin levels since it has an impact on satiation, thus inhibiting ghrelin secretion [10]. It has also been proven that fasting plasma ghrelin values in obese patients inversely correlate with plasma leptin concentrations [28, 29]. However, recent research has proposed that the two systems might work independently of each other, with different pathophysiological mechanisms [30]. Our finding of a correlation between adiponectin and ghrelin in all three research groups will require confirmation in other studies and further research.
Subgroup analysis of included patients revealed a moderate negative statistical correlation between ghrelin/adiponectin and a positive correlation between leptin and anthropometrical parameters in the group of obese children and adolescents with hypertension. These results show their good potential for assessing obesity, which was also confirmed by other studies [24, 31]. In the present study, their observed correlation with systolic blood pressure indicates their role in hypertension risk. Recently, leptin has been found to play a role in obesity-related hypertension [32, 33] as has adiponectin in adult men [34].
In the group of children and adolescents with elevated lipids, a moderate negative statistical correlation was found between ghrelin and adiponectin and anthropometrical parameters as well as systolic and diastolic blood pressure, indicating their good predictive value in this group of patients. Leptin was found to have a moderate positive correlation with anthropometrical parameters as well as with diastolic blood pressure. Some previously published studies have found a correlation between lipid fractions and biological markers of obesity [27, 35]. To our knowledge, the correlation with blood pressure in such children has not been evaluated.
In the group of children and adolescents with normal-weight hypertension, the correlation between ghrelin, leptin and adiponectin and anthropometrical parameters has also been found. In a recent study, leptin was shown to correlate with blood pressure, but this was not confirmed in our study [32]. However, ghrelin and adiponectin have been confirmed as cardiovascular markers in normal-weight hypertensive patients, which has not been proven in children until now, although this correlation has been found in adult patients [36]. Interestingly, the finding of correlations between both ghrelin and adiponectin and homocysteine in patients with hypertension, obese and normal-weight, needs further investigations. In addition, their potential mechanisms of action, including inflammation [37] and other biological effects [38], have to be determined.
Conclusion
Our study showed that biological markers of obesity have the potential to be used as early cardiovascular risk factors. It seems that the parameters are especially helpful in the obese population with hypertension. Ghrelin has been found to be a valid marker for all investigated groups and we recommend its use for the determination of cardiovascular risk. We have also confirmed that biological markers of obesity correlate with BMI, ghrelin and adiponectin negatively and leptin positively.
What this paper adds:
- 1.
Biological markers of obesity are useful not only as markers of obesity but also as early cardiovascular risk markers.
- 2.
Along with the large impact of leptin, ghrelin and adiponectin also play significant roles, with potential codependency.
- 3.
The most promising biological marker in all three groups of children was found to be ghrelin, which we propose for the determination of cardiovascular risk.
Availability of data and materials
All data generated or analyzed during this study are included in this published article, except the correlations of the biological markers with other investigated parameters, presented as the Table 4.
Abbreviations
- ANOVA:
-
Analysis of variance
- BMI:
-
Body mass index
- N:
-
Nonsignificant
- SD:
-
Standard deviation
References
Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: causes and consequences. J Family Med Prim Care. 2015;4:187–92. https://doi.org/10.4103/2249-4863.154628.
Gabrijelčič Blenkuš M, Robnik M. Overweight and obesity in children and adolescents in Slovenia II. Ljubljana: National Institute for Public Health; 2016.
Theodore RF, Broadbent J, Nagin D, Ambler A, Hogan S, Ramrakha S, et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertens. 2015;66:1108–15. https://doi.org/10.1161/HYPERTENSIONAHA.115.05831.
Centers for disease control and prevention. Childhood obesity facts. 2017. https://www.cdc.gov/healthyschools/obesity/facts.htm. Accessed 30 Jan 2017.
Wickramasinghe VP, Cleghorn GJ, Edmiston KA, Murphy AJ, Abbott RA, Davies PS. Validity of BMI as a measure of obesity in Australian white Caucasian and Australian Sri Lankan children. Ann Hum Biol. 2005;32:60–71.
Bauer KW, Marcus MD, El ghormli L, Ogden CL, Foster GD. Cardio-metabolic risk screening among adolescents: understanding the utility of body mass index, waist circumference and waist to height ratio. Pediatr Obes. 2015;10:329–37. https://doi.org/10.1111/ijpo.267.
Simmonds M, Burch J, Llewellyn A, Griffiths C, Yang H, Owen C, et al. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: a systematic review and meta-analysis. Health Technol Assess. 2015;19:1–336. https://doi.org/10.3310/hta19430.
Zhang M, Cheng H, Zhao X, Hou D, Yan Y, Cianflone K, et al. Leptin and leptin-to-adiponectin ratio predict adiposity gain in nonobese children over a six-year period. Child Obes. 2017;13:213–21. https://doi.org/10.1089/chi.2016.0273.
Bjornstad P, Truong U, Dorosz JL, Cree-Green M, Baumgartner A, Coe G, et al. Cardiopulmonary dysfunction and adiponectin in adolescents with type 2 diabetes. J Am Heart Assoc. 2016;5:e002804. https://doi.org/10.1161/JAHA.115.002804.
Klok MD, Jakobsdottir S, Drent ML. The role of leptin and ghrelin in the regulation of food intake and body weight in humans. Obesity Rev. 2007;8:21–34.
Jain V, Kumar A, Agarwala A, Vikram N, Ramakrishnan L. Adiponectin, interleukin-6 and high-sensitivity C-reactive protein levels in overweight/obese Indian children. Indian Pediatr. 2017;54:848–50.
Stroescu RF, Mărginean O, Bizerea T, Gafencu M, Voicu A, Doroș G. Adiponectin, leptin and high sensitivity C-reactive protein values in obese children − important markers for metabolic syndrome? J Pediatr Endocrinol Metab. 2019;32:27–31. https://doi.org/10.1515/jpem-2018-0378.
Ambroszkiewicz J, Gajewska J, Szamotulska K, Rowicka G, Klemarczyk W, Chełchowska M. Comparison of body composition and adipokine levels between thin and normal-weight prepubertal children. J Pediatr (Rio J). 2017;93:428–35. https://doi.org/10.1016/j.jped.2016.11.004.
Önnerfält J, Erlanson-Albertsson C, Montelius C, Thorngren-Jerneck K. Obese children aged 4−6 displayed decreased fasting and postprandial ghrelin levels in response to a test meal. Acta Paediatr. 2018;107:523–8. https://doi.org/10.1111/apa.14165.
Heshmat R, Shafiee G, Qorbani M, Azizi-Soleiman F, Djalalinia S, Esmaeil Motlagh M, et al. Association of ghrelin with cardiometabolic risk factors in Iranian adolescents: the CASPIAN-III study. J Cardiovasc Thorac Res. 2016;8:107–12.
R&D Systems. Quantikine ELISA. Human leptin, vol. 3. Minneapolis: R&D systems; 2009. p. 3.
R&D Systems. Quantikine ELISA. Human total adiponectin/Arcp30. Minneapolis: R&D systems; 2012. p. 2.
EMD Millipore Corporation. Human ghrelin (total). EMD Missouri: Millipore Corporation; 2009. p. 2.
University Medical Center Maribor. Department of laboratory diagnostics. 2017. https://www.ukc-mb.si/oddelki-službe-enote/skupni-medicinski-oddelki/oddelek-za-laboratorijsko-diagnostiko/seznam-preiskav/. Accessed 14 Jan 2020.
Dalla Valle M, Laatikainen T, Kalliokoski T, Nykänen P, Jääskeläinen J. Childhood obesity in specialist care − searching for a healthy obese child. Ann Med. 2015;47:639–54. https://doi.org/10.3109/07853890.2015.1083118.
Zampetti S, Campagna G, Lucantoni F, Marandola L, D'Onofrio L, Chiesa C, et al. Wrist circumference is associated with increased systolic blood pressure in children with overweight/obesity. Hypertens Res. 2018;41:193–7. https://doi.org/10.1038/s41440-017-0006-0.
Stelcar A, Homsak E, Marcun VN. Assessment of early cardiovascular risk in children and adolescents with essential hypertension. Klin Pediatr. 2017;229:1–7. https://doi.org/10.1055/s-0043-104220.
Elmaoğulları S, Tepe D, Uçaktürk SA, Karaca Kara F, Demirel F. Prevalence of dyslipidemia and associated factors in obese children and adolescents. J Clin Res Pediatr Endocrinol. 2015;7:228–34. https://doi.org/10.4274/jcrpe.1867.
Wali P, King J, He Z, Tonb D, Horvath K. Ghrelin and obestatin levels in children with failure to thrive and obesity. J Pediatr Gastroenterol Nutr. 2014;58:376–81. https://doi.org/10.1097/MPG.0000000000000223.
Wang WM, Li SM, Du FM, Zhu ZC, Zhang JC, Li YX. Ghrelin and obestatin levels in hypertensive obese patients. J Int Med Res. 2014;42:1202–8. https://doi.org/10.1177/0300060514543040.
Pires A, Martins P, Pereira AM, Marinho J, Vaz Silva P, Marques M, et al. Pro-inflammatory triggers in childhood obesity: correlation between leptin, adiponectin and high-sensitivity C-reactive protein in a group of obese Portuguese children. Rev Port Cardiol. 2014;33:691–7. https://doi.org/10.1016/j.repc.2014.04.004.
Jois A, Navarro P, Ortega-Senovilla H, Gavela-Pérez T, Soriano-Guillén L, Garcés C. Relationship of high leptin levels with an adverse lipid and insulin profile in 6−8 year-old children in Spain. Nutr Metab Cardiovasc Dis. 2015;25:1111–6. https://doi.org/10.1016/j.numecd.2015.09.005.
Soriano-Guillén L, Ortega L, Navarro P, Riestra P, Gavela-Pérez T, Garcés C. Sex-related differences in the association of ghrelin levels with obesity in adolescents. Clin Chem Lab Med. 2016;54:1371–6. https://doi.org/10.1515/cclm-2015-0555.
Kyrgios I, Galli-Tsinopoulou A, Stylianou C. Ghrelin-leptin network influences serum chitinase 3-like protein 1 (YKL-40) levels in obese prepubertal children. Regul Pept. 2013;183:69–73. https://doi.org/10.1016/j.regpep.2013.03.022.
Rodríguez A. Novel molecular aspects of ghrelin and leptin in the control of adipobiology and the cardiovascular system. Obes Facts. 2014;7:82–95. https://doi.org/10.1159/000360837.
Ochiai H, Shirasawa T, Nishimura R, Nanri H, Ohtsu T, Hoshino H, et al. Abdominal obesity and serum adiponectin complexes among population-based elementary school children in Japan: a cross-sectional study. BMC Pediatr. 2014;14:81. https://doi.org/10.1186/1471-2431-14-81.
Jędzura A, Adamczyk P, Bjanid O, Świętochowska E, Roszkowska-Bjanid D, Baraniecka A, et al. Non-dipping status and selected adipokines concentration in children with primary arterial hypertension. Clin Exp Hypertens. 2017;39:718–25. https://doi.org/10.1080/10641963.2017.1324474.
Fujita Y, Kouda K, Ohara K, Nakamura H, Iki M. Leptin mediates the relationship between fat mass and blood pressure: the Hamamatsu school-based health study. Med (Baltimore). 2019;98:e14934. https://doi.org/10.1097/MD.0000000000014934.
Yang YD, Zheng CJ, Dong YH, Zou ZY, Lv Y, Wang ZH, et al. Sex difference in the mediation roles of an inflammatory factor (hsCRP) and adipokines on the relationship between adiposity and blood pressure. Hypertens Res. 2019;42:903–11. https://doi.org/10.1038/s41440-019-0222-x.
Winer JC, Zern TL, Taksali SE, Dziura J, Cali AM, Wollschlager M, et al. Adiponectin in childhood and adolescent obesity and its association with inflammatory markers and components of the metabolic syndrome. J Clin Endocrinol Metab. 2006;91:4415–23.
Peri-Okonny PA, Ayers C, Maalouf N, Das SR, de Lemos JA, Berry JD, et al. Adiponectin protects against incident hypertension independent of body fat distribution: observations from the Dallas Heart Study. Diabetes Metab Res Rev. 2017;33(2). https://doi.org/10.1002/dmrr.2840.
Bando M, Iwakura H, Ueda Y, Ariyasu H, Inaba H, Furukawa Y, et al. IL-1β directly suppress ghrelin mRNA expression in ghrelin-producing cells. Mol Cell Endocrinol. 2017;447:45–51. https://doi.org/10.1016/j.mce.2017.02.032.
Tokudome T, Otani K, Miyazato M, Kangawa K. Ghrelin and the heart. Peptides. 2019;1:42–6. https://doi.org/10.1016/j.peptides.2018.05.006.
Funding
This research has received no specific grant or funding from any funding source in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NMV conceived the study and its design, supervised data collection and the statistical analysis, and wrote the main part of the manuscript. LO performed data collection, statistical analysis and helped draft the manuscript. MM participated in data collection and analysis and helped draft the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethics approval from the institutional Ethical Committee at the University Medical Center Maribor. Written informed consent was obtained from the parents of children and adolescents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Varda, N.M., Medved, M. & Ojsteršek, L. The associations between some biological markers, obesity, and cardiovascular risk in Slovenian children and adolescents. BMC Pediatr 20, 81 (2020). https://doi.org/10.1186/s12887-020-1978-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-020-1978-5