Abstract
Background
Although poor complementary feeding is associated with poor child growth, nutrition interventions only have modest impact on child growth, due to high burden of infections. We aimed to assess the association of malaria with linear growth, hemoglobin, iron status, and development in children aged 6–18 months in a setting of high malaria and undernutrition prevalence.
Methods
Prospective cohort study, conducted in Mangochi district, Malawi. We enrolled six-months-old infants and collected weekly data for ‘presumed’ malaria, diarrhea, and acute respiratory infections (ARI) until age 18 months. Change in length-for-age z-scores (LAZ), stunting, hemoglobin, iron status, and development were assessed at age 18 months. We used ordinary least squares regression for continuous outcomes and modified Poisson regression for categorical outcomes.
Results
Of the 2723 children enrolled, 2016 (74.0%) had complete measurements. The mean (standard deviation) incidences of ‘presumed’ malaria, diarrhea, and ARI, respectively were: 1.4 (2.0), 4.6 (10.1), and 8.3 (5.0) episodes/child year. Prevalence of stunting increased from 27.4 to 41.5% from 6 to 18 months. ‘Presumed’ malaria incidence was associated with higher risk of stunting (risk ratio [RR] = 1.04, 95% confidence interval [CI] = 1.01 to 1.07, p = 0.023), anemia (RR = 1.02, 95%CI = 1.00 to 1.04, p = 0.014) and better socio-emotional scores (B = − 0.21, 95%CI = − 0.39 to − 0.03, p = 0.041), but not with change in LAZ, haemoglobin, iron status or other developmental outcomes. Diarrhea incidence was associated with change in LAZ (B = − 0.02; 95% CI = − 0.03 to − 0.01; p = 0.009), stunting (RR = 1.02; 95% CI = 1.01 to 1.03; p = 0.005), and slower motor development. ARI incidence was not associated with any outcome except for poorer socio-emotional scores.
Conclusion
In this population of young children living in a malaria-endemic setting, with active surveillance and treatment, ‘presumed’ malaria is not associated with change in LAZ, hemoglobin, or iron status, but could be associated with stunting and anemia. Diarrhea was more consistently associated with growth than was malaria or ARI. The findings may be different in contexts where active malaria surveillance and treatment is not provided.
Trial registration
NCT00945698 (July 24, 2009) and NCT01239693 (November 11, 2010).
Similar content being viewed by others
Introduction
Although poor complementary feeding is associated with poor child growth, many interventions designed to improve complementary foods only have modest impact on growth [1], possibly due to a high burden of infections in children [2, 3]. Studies in which morbidity treatment was integrated with a complementary feeding intervention demonstrated improved linear growth [4] and developmental outcomes in children [5, 6], suggesting the importance of reducing the burden of infections along with improved diet to promote child growth and development.
Longitudinal studies have reported a significant inverse association of diarrhea with growth [7,8,9]. However, studies on the association of malaria with growth and development have either reported inconsistent results or had cross-sectional designs, which makes it difficult to assess causality or directionality of association [10,11,12,13]. This has prevented the inclusion of malaria as a determinant of stunting in the Lives Saved Tool (LiST) model [14].
The International Lipid-based Nutrient Supplements (iLiNS) Project DOSE and DYAD-M studies were randomized controlled trials conducted in Malawi to study the impact of lipid-based nutrient supplements (LNS) on growth of children [15, 16]. The aim of this analysis was to assess the association of malaria with linear growth, hemoglobin, iron status, and child development. Our hypothesis was that linear growth, hemoglobin, iron status, and developmental outcomes at age 18 mo would be poorer in children with higher incidence of malaria from age 6 to 18 mo. We also analyzed the association of diarrhea and acute respiratory infections (ARI) with linear growth, hemoglobin, iron status, and developmental outcomes.
Methods
Study setting
The iLiNS-DOSE and iLiNS-DYAD-M studies were conducted in one public district hospital (Mangochi), one mission hospital (St Martins), and two rural public health centers (Lungwena and Namwera) in Mangochi District, Southern Malawi. The total catchment population of 180,000 largely subsisted on farming and fishing. In Malawian children aged < 5 years, the prevalence of reported fever (a proxy for malaria), diarrhea and ARI was 29, 22 and 5%, respectively, with seasonal fluctuations [17]. Malaria is endemic in Malawi and the study area has high malaria transmission with high temperature and frequent rainfall from October through April [18].
Study design and data collection
In the iLiNS-DOSE study, 6-mo old children were randomly allocated to one of five intervention groups provided with different doses or formulations of LNS or to a control group that did not receive LNS during the 12-mo study period, between November 2009 and May 2012. In the iLiNS-DYAD-M study, pregnant women < 20 weeks’ gestation were randomly allocated to one of three groups to receive iron and folic acid (IFA), multiple micronutrients (MMN) or a small-quantity (20 g) of LNS daily. After delivery, women in the IFA group received placebo tablets, while MMN and LNS supplementation was continued up to 6 mo postpartum. Children of mothers in the LNS group also received LNS 10 g twice daily from age 6 to 18 mo. This study was conducted from February 2011 to April 2015. Details of study design, randomization and enrolment for the two studies were explained in the main outcome papers [15, 16].
In both studies, research assistants visited the children’s homes every week from age 6 to 18 mo to interview the guardians about the child’s health in the previous 7 days using a structured questionnaire. The information was complemented by a picture calendar filled out by the guardians daily to aid memory of their children’s morbidity status. The use of maternal interviews as a means of collecting data on child morbidity has been validated in previous studies [19, 20]. The research assistants referred all cases of ‘presumed’ malaria (presence of fever) to the nearby health facility for treatment with lumefantrine/artemether, the nationally recommended antimalarial drug. The children were followed throughout the year, covering periods of both high and low malaria transmission.
Anthropometric measurements were taken at age 6 mo and 18 mo. Study anthropometrists measured the infant’s length with a high-quality length board (Harpenden Infantometer; Holtain Limited) and recorded it to the nearest 1 mm. They weighed unclothed infants with electronic infant weighing scale (SECA 735; Seca GmbH & Co), recording to the nearest 10 g. The anthropometrists were trained and their measurement reliability was verified at the start of the study and at 6-mo intervals thereafter with methods adapted from the procedures used in the WHO Multicentre Growth Reference Study [21]. The anthropometrists calibrated all equipment with standard weights and length rods daily.
We assessed iron status at age 6 mo and 18 mo by measuring the zinc protoporphyrin (ZPP) concentration in unwashed venous blood sample using a hematofluorometer (206D, AVIV Biomedical Inc., Lakewood, NJ, USA). About 5–7 ml of blood was collected by venepuncture using a 23-gauge needle into 7.5 ml evacuated, trace element-free polyethylene tubes containing lithium heparin (Sarstedt AG & Co, Nümbrecht, Germany). The samples were kept covered in aluminium and away from light, in a refrigerator or on ice, and processed within 2 h of collection. We measured blood hemoglobin (Hb) concentration at age 6 mo and 18 mo from a drop of blood taken from a finger prick and collected in a microcuvette. Hb analysis was conducted on-site using a Hemo-Cue instrument (Hemocue 201+, HemoCue® AB, Ängelholm, Sweden).
We assessed fine and gross motor development at age 18 mo using the Kilifi Developmental Inventory (KDI) developed in Kenya [22]. Language development was assessed using a 100-word vocabulary checklist by maternal interview based on the MacArthur-Bates Communicative Development Inventory [23] adapted for the local languages, and 18-mo socio-emotional development was assessed using the Profile of Social and Emotional Development (PSED), also developed in Kenya. The child’s mood during the KDI assessment was rated as positive (smiling/laughing) or not positive (crying/inconsolable, changeable/mood swings, or no visible emotions). The child’s interaction with the assessor during the KDI was rated as positive (friendly) or not positive (avoidant and withdrawn, clings to family member, hesitant/when approached will accept reluctantly, difficult to engage in tasks, or inappropriate approaches to the assessor). The child’s activity level during the KDI was rated as positive (active and maintains interest) or not positive (unarousable, sleepy and can hardly be awakened, sleepy but easily awakened, does not spontaneously engage in activity, and awake but loses interest). The KDI, vocabulary, and PSED scores showed high inter-rater agreement and moderate to high test-retest reliability in this study setting [24, 25].
Definition of the predictors and the outcomes
We used a presumptive diagnosis of malaria derived from episodes of fever during the previous week, reported by the guardians. To ensure the diagnoses were mutually exclusive, we created an algorithm whereby any fever with a diarrhea episode (three or more loose stools in 24 h) was categorized as diarrhea; any fever in the presence of any respiratory symptoms (cough, rapid or difficult breathing and nasal discharge) was categorized as ARI. ‘Presumed’ malaria was defined as any fever episode in the absence of diarrhea and respiratory symptoms.
An episode of ‘presumed’ malaria, ARI or diarrhea was defined as the period starting from the day the child had the symptoms when preceded by at least 2 days of no symptoms or no data. The episode ended on the last day the child had the symptoms which was then followed by at least 2 symptom-free days. Incidence of ‘presumed’ malaria, ARI or diarrhea for each child from age 6 to 18 mo was calculated as total episodes / total follow up years at risk.
Longitudinal prevalences of common childhood symptoms (fever, diarrhea, and cough) from age 6 to 18 mo were defined as the number of days with the symptom divided by the total number of days of observation for each child [26].
We calculated age- and sex-standardized anthropometric indices [length-for-age z score (LAZ), weight-for-age z score (WAZ), and weight-for-length z score (WLZ)] based on the WHO Child Growth Standards [21] and considered values below – 2.0 indicative of underweight, stunting and wasting, respectively. Change in LAZ for each child was calculated as the difference between LAZ at age 18 mo and LAZ at age 6 mo.
Iron deficiency at age 6 mo and 18 mo was defined as whole blood ZPP > 70 μmol/mole heme [27]. Anemia at age 6 mo was defined as blood Hb concentration < 105 g/L [28] while anemia at age 18 mo was defined as blood Hb concentration < 110 g/L [29].
From the child development data at age 18 mo, fine motor scores were calculated as the sum of 34 KDI fine motor items, each scored 0 or 1, gross motor scores were calculated as the sum of 35 KDI gross motor items, each scored 0 or 1 [22] and vocabulary score was the maternal-reported child expressive vocabulary out of the 100-word checklist. For these outcomes, moderate to severe delay was defined as the bottom 25% of the sample. The socio-emotional score was calculated as the sum of 19 PSED items. Moderate to severe delay was defined as the top 25% of our sample (a higher score indicates less advanced socio-emotional development).
Statistical analysis
We included in the analysis children who had outcomes measured at age 18 mo. For all continuous outcomes, we used ordinary least squares regression to assess the association between malaria incidence and each outcome; and for all binary outcomes, we used modified Poisson regression (with a robust variance estimator) [30].
We first assessed whether the relationship between the predictor and each outcome differed between the two studies. However, the interaction term was not statistically significant indicating that this relationship was not different between the two studies therefore we pooled data from the two cohorts. We then constructed multivariate models to determine which variables independently predicted the outcomes. We included all theoretically relevant variables, regardless of whether they were statistically significant or not after the bivariate analysis. The following variables collected at age 6 mo were included in the models: child sex, LAZ, WLZ, Hb, iron status, maternal education and household food insecurity access (HFIA) score generated by summing the value of responses to nine questions regarding food insecurity [31]. We also included in the models, from age 6 to 18 mo, the incidence of diarrhea and ARI, and whether the child received an intervention (LNS) or not. For the risk of stunting at age 18 mo, we included in the model stunting at age 6 mo (in place of LAZ). In addition, all developmental outcomes were adjusted for the child’s mood, activity level, age and interaction with the assessor.
We assessed collinearity among the variables (e.g. LAZ vs WLZ at age 6 mo). If the variables were highly collinear (> 0.5), we dropped the one that was less strongly associated with the outcomes. We accounted for intracluster correlation due to twins using generalised estimating equations [32].
We also performed exploratory analyses by using frequency of malaria episodes (from age 6 to 18 mo) as a categorical variable (no episode, one episode, and > 1 episodes groups). In addition, we conducted stratified analyses by stunting at age 6 mo. Although we performed bivariate analyses for each individual variable, we will only report the results from multivariate analysis.
We used Stata version 14 (StataCorp, Texas, USA) for all the analyses.
Results
Baseline characteristics and descriptive statistics
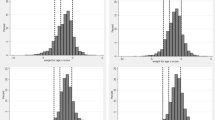
Of the 2723 children enrolled in the two study cohorts, 2016 (74.0%) had length measured both at age 6 mo and 18 mo (1417 children from the iLiNS DOSE study and 599 children from the iLiNS DYAD-M study). These were included in the final analysis (Fig. 1). The characteristics of these children at age 6 mo are summarized in Table 1.
The 2016 children included in the final analysis contributed 1647.9 child years of follow up, i.e. the mean (standard deviation) [SD] duration of follow up was 298 (61) days / child. A total of 24,024 morbidity episodes were reported during the home visits. Of these, 9.7% (2324/24024) were episodes of ‘presumed’ malaria. The rest of the morbidity episodes were due to: acute respiratory infections (ARI), 55.6% (13,360/24024); diarrhea, 33.6% (8083/24024); and minor conditions, 1.1% (257/24024).
Overall, the mean (SD) incidence of all illnesses combined was 14.8 (6.8) episodes per child year. The mean (SD) incidence of ‘presumed’ malaria was 1.4 (2.0) episodes per child year. The mean (SD) incidence of ARI was 8.3 (5.0) episodes per child year and the mean (SD) incidence of diarrhea was 4.6 (10.1) episodes per child year. The longitudinal prevalences of common childhood symptoms (fever, diarrhea, and cough) from age 6 to 18 mo were: 7.5%; 3.4%; and 11.7%, respectively.
During the 12-mo follow up period, 39.0% (787/2016) of the children did not report any episode of ‘presumed’ malaria, 30.3% (611/2016) reported one episode and 30.7% (618/2016) reported > 1 malaria episodes. The children who reported > 1 malaria episodes were responsible for 73.7% (1713/2324) of all ‘presumed’ malaria episodes reported in the two studies.
At age 18 mo, the mean (SD) length-for-age z-scores (LAZ), weight-for-age z-scores (WAZ) and weight-for-length (WLZ) scores were − 1.8 (1.1), − 1.0 (1.1) and − 0.2 (1.1) respectively. The proportions of children who were stunted, underweight and wasted were 41.5, 16.6 and 5.0%, respectively. The median (25th, 75th centile) zinc protoporphyrin (ZPP) concentration was 74 (51, 114) μmole/mole heme and the proportion with iron deficiency was 54.1%. The mean (SD) hemogobin (Hb) concentration was 108.5 (15.1) g/L and the proportion with anemia was 50.5%. The mean (SD) scores for fine motor, gross motor, language and Profile of Social and Emotional Development (PSED) were 20.9 (2.2), 17.3 (2.6), 26.2 (5.0) and 16.2 (5.4) respectively.
Association of malaria with linear growth
The mean (SD) change in LAZ from age 6 to 18 mo was − 0.44 (0.77). In multivariate analysis, there was no association between the incidence of ‘presumed’ malaria and change in LAZ from age 6 to 18 mo, adjusted for LAZ at age 6 mo (B = − 0.02, 95% CI = − 0.04 to 0.01, p = 0.069) (Table 2).
The proportion of children who were stunted increased from 27.4% at age 6 mo to 41.5% at age 18 mo. In multivariate analysis, the incidence of ‘presumed’ malaria was associated with higher risk of stunting at age 18 mo, adjusted for stunting at age 6 mo (RR = 1.04, 95% CI = 1.01 to 1.07, p = 0.023) (Table 2). When categorized by frequency of malaria episodes and adjusted for stunting at age 6 mo, children with > 1 malaria episodes from age 6 to 18 mo had higher risk of stunting at age 18 mo compared to children with zero malaria episodes (RR = 1.39, 95% CI = 1.13 to 1.70, p = 0.002).
Association of malaria with hemoglobin, anemia and iron status
The incidence of ‘presumed’ malaria from age 6 to 18 mo was associated with higher risk of anemia at age 18 mo, adjusted for hemoglobin at age 6 mo (RR = − 0.12; 95% CI = − 0.20 to − 0.04; p = 0.002) but not with hemoglobin or iron deficiency at age 18 mo (Table 3).
Association of malaria with child development
The association of incidence of ‘presumed’ malaria from age 6 to 18 mo with child development was significant for PSED scores (B = − 0.21; 95% CI = 0.39 to − 0.03; p = 0.041), but not for the other domains of child development, adjusted for the covariates listed in the footnotes to Tables 4 and 5.
Association of diarrhea and ARI with linear growth, hemoglobin, iron status, and developmental outcomes
In multivariate analysis, incidence of diarrhea from age 6 to 18 mo was associated with change in LAZ from age 6 to 18 mo (B = − 0.02; 95% CI = − 0.03 to − 0.01; p = 0.009), higher risk of stunting at age 18 mo (RR = 1.02; 95% CI = 1.01 to 1.03; p = 0.005) (Table 2), lower gross motor scores at age 18 mo (B = − 0.02; 95% CI = − 0.03 to − 0.01; p < 0.001), and higher risk of gross motor delay (RR = 1.01; 95% CI = 1.00 to 1.02; p < 0.001) and fine motor delay (RR = 1.01; 95% CI = 1.00 to 1.02; p = 0.011) at age 18 mo (Tables 4 and 5).
The incidence of ARI from age 6 to 18 mo was not significantly associated with growth or other outcomes except for PSED scores (B = 0.08; 95% CI = 0.03 to 0.14; p = 0.004), and PSED delay (RR = 1.02; 95% CI = 1.00 to 1.04; p = 0.025) (Tables 4 and 5).
Discussion
We tested the hypothesis that the linear growth, hemoglobin, iron status, and developmental outcomes at age 18 mo would be poorer in children with higher incidence of ‘presumed’ malaria. In a sample of 2016 Malawian children aged 6–18 mo, we found that malaria was not associated with change in LAZ, fine motor scores, gross motor scores, language development, iron status or hemoglobin concentration. Higher incidence of ‘presumed’ malaria was associated with higher risk of stunting and anemia (i.e: one additional episode of ‘presumed’ malaria per year was associated with 4 and 2% higher risk of stunting and anemia, respectively). Higher incidence of ‘presumed’ malaria was also associated with lower socio-emotional scores (i.e: one additional episode of ‘presumed’ malaria per year was associated with a reduction in PSED scores by 0.21), suggesting that children with higher malaria incidence tended to have fewer socio-emotional problems, possibly because malaria causes lethargy and inactivity which may manifest as fewer behavioral problems.
Our study had several strengths: the weekly home morbidity data collection for 1 year provided comprehensive data covering periods of both high and low malaria transmission; the longitudinal design made it possible to correlate the malaria exposure with the outcomes and interpret the directionality of association; and pooling of data from two studies helped us draw conclusions from a large sample. Although we did not calculate post-hoc power for this analysis, with a large sample size of 2016 children and narrow confidence intervals obtained for most of the morbidity outcomes, we believe the study was powered to detect clinically meaningful associations.
Our results should be interpreted with caution because we excluded children who did not have the outcomes measured at age 18 mo (26% of the sample), resulting in possible survival bias. However, this attrition rate is similar to that of other studies with a long follow up period [9, 10]. Moreover, we expect that the children lost to follow up may have had worse outcomes, which probably would have increased the strength of association in our findings.
Another possible cause of bias is the presumptive diagnosis of malaria, which could lead to misclassification. There is overlap in the symptoms of malaria, diarrhea and ARI [33] which may affect the sensitivity and specificity of presumptive malaria diagnosis depending on the intensity of malaria transmission. For example, presumptive malaria diagnosis usually has higher sensitivity and lower specificity in areas of high malaria transmission compared to areas of low transmission [34, 35]. With the global decline in malaria incidence and availability of malaria Rapid Diagnostic Tests (mRDTs), the WHO in 2010 recommended antimalarial treatment be provided when there is evidence of a positive malaria test result [36]. However, at the time of conducting our study, mRDTs had not been rolled out nationwide, hence presumptive malaria diagnosis was used not only in this study but also in national prevalence surveys [18, 37], according to the practice of Integrated Management of Childhood Illness (IMCI) [38, 39]. Furthermore, in exploratory analysis using hospital diagnosed malaria (confirmed by mRDT, albeit with a lot of missing data), the direction of the associations was similar, suggesting that our findings are still valid (data not shown).
Our research assistants referred the children suspected of malaria to a clinic for treatment; the active surveillance and early treatment may have helped improve the study outcomes, which may have resulted in underestimation of the associations.
It is also possible that the association of malaria with stunting, anemia, and PSED scores was significant by chance due to multiple testing [40]. However, we believe the chance finding was less likely for the significant associations of diarrhoea and ARI with the outcomes because these associations were relatively strong based on p-values.
The available evidence on the association of malaria with growth and other outcomes is inconclusive. Some studies have reported significant associations of malaria with stunting, hemoglobin concentration, iron status and child development [11, 12, 41,42,43,44]. Children living in settings where infectious diseases are frequent and complementary food is of poor quality often fail to achieve catch up growth after illness episodes [45], hence frequent malaria could be associated with growth faltering. Earlier evidence suggested that anorexia, vomiting, and a catabolic state are responsible for the poor growth associated with febrile illnesses in children [46]. However, other studies have reported no association of malaria with growth outcomes [47,48,49,50]. Similar to our study, most of these studies provided active malaria diagnosis and treatment, which may have attenuated the strength of the association.
In the studies cited above, different exposure and outcome measures were used, which may also explain the inconsistency in the findings. For example, we defined linear growth as change in LAZ and stunting. Change in LAZ indicates the growth rate between two time-points and therefore provides more information about linear growth faltering than stunting status assessed at one time-point [51, 52]. Therefore, it is possible that there is no association between malaria and linear growth (based on change in LAZ), hemoglobin or iron status, or the association is very weak. It is also possible that the association between malaria and these outcomes is only seen in children in the left end of the curve (i.e. LAZ < − 2 or hemoglobin < 110 g/L), hence the significant association of malaria with stunting and anemia but not change in LAZ or hemoglobin concentration. In contrast, diarrhea incidence was associated with an entire leftward shift in LAZ and gross motor scores in this population. A leftward shift in mean LAZ for a population is associated with increased risk of mortality [53].
The association of diarrhea with growth has been reported in previous studies [7,8,9]. Frequent diarrhea episodes result in persistent loss of nutrients necessary for growth through malabsorption, changes in gut microbiota, continuous immune system activation, increased metabolism and anorexia resulting in growth suppression. In our study, the magnitude of the significant associations of malaria and diarrhea with the outcomes were small, consistent with other studies [7, 42, 44, 54,55,56]. This could be partly attributable to the active surveillance and treatment provided to all children, or unmeasured confounding [44], or that perhaps other conditions such as chronic inflammation and environmental enteric dysfunction may be more important determinants of child growth in developing countries [57, 58]. Nevertheless, in a study combining nutrition intervention with treatment of malaria and diarrhea there was greater growth velocity, a 25% reduction in prevalence of stunting and improved developmental outcomes at age 18 months [4], suggesting that interventions that combine improved nutrition with control of infections may have significant impact.
Conclusions
We conclude that in this population of children aged 6–18 mo living in a malaria-endemic setting, with active surveillance and early treatment, ‘presumed’ malaria is not associated with change in LAZ, hemoglobin or iron status, but could be associated with stunting and anemia. In this population, diarrhoea was more consistently associated with growth than was malaria or ARI. These findings may be different in contexts where there is no active case finding and treatment for malaria is not promptly administered.
Abbreviations
- ARI:
-
Acute respiratory infection
- CI:
-
Confidence interval
- Hb:
-
Hemoglobin
- HFIA:
-
Household food insecurity access
- IFA:
-
Iron and folic acid
- IMCI:
-
Integrated Management of Childhood Illness
- KDI:
-
Kilifi Developmental Inventory
- LAZ:
-
Length-for-age z-scores
- LNS:
-
Lipid-based nutrient supplements
- MMN:
-
Multiple micronutrients
- mRDT:
-
Malaria Rapid Diagnostic Test
- PSED:
-
Profile of Social and Emotional Development
- RR:
-
Risk ratio
- SD:
-
Standard deviation
- WAZ:
-
Weight-for-age z-scores
- WHO:
-
World Health Organization
- WLZ:
-
Weight-for-length z-scores
- ZPP:
-
Zinc protoporphyrin
References
Dewey KG, Adu-Afarwuah S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Maternal and Child Nutrition. 2008;4:24–85.
Iannotti LL, Jean S, Dulience L, Green J, Joseph S, Franc J, et al. Linear growth increased in young children in an urban slum of Haiti : a randomized controlled trial of a lipid-based nutrient supplement 1–3. Am J Clin Nutr. 2014;99:198–208.
Hadi H, Dibley MJ, West KP. Complex interactions with infection and diet may explain seasonal growth responses to vitamin a in preschool aged Indonesian children. Eur J Clin Nutr. 2004;58(7):990–9.
Hess SY, Abbeddou S, Jimenez EY, Somé JW, Vosti SA, Ouédraogo ZP, et al. Small-Quantity Lipid-Based Nutrient Supplements, Regardless of Their Zinc Content, Increase Growth and Reduce the Prevalence of Stunting and Wasting in Young Burkinabe Children: A Cluster-Randomized Trial. PLoS One. 2015;10(3):e0122242 Available from: http://dx.plos.org/10.1371/journal.pone.0122242.
Prado EL, Abbeddou S, Yakes Jimenez E, Some JW, Ouedraogo ZP, Vosti SA, et al. Lipid-based nutrient supplements plus malaria and diarrhea treatment increase infant development scores in a cluster-randomized trial in Burkina Faso. J Nutr. 2016;146(4):814–22 Available from: http://jn.nutrition.org/cgi/doi/10.3945/jn.115.225524.
Taylor C, Sarma R, Parker R, Reinke W, Faruqee R, Kielmann A. Child and maternal health Services in Rural India: the Narangwal experiment, volume 1: integrated nutrition and health care. Vol. 2, integrated family planning and health care. Baltimore and London: The Johns Hopkins University Press; 1983.
Richard SA, Black RE, Gilman RH, Guerrant RL, Kang G, Lanata CF, et al. Diarrhea in early childhood: short-term association with weight and long-term association with length. Am J Epidemiol. 2013;178(7):1129–38 Available from: http://aje.oxfordjournals.org/cgi/doi/10.1093/aje/kwt094.
Checkley W, Buckley G, Gilman RH, Assis AM, Guerrant RL, Morris SS et al. Multi-country analysis of the effects of diarrhoea on childhood stunting. International Journal of Epidemiology. 2008;37(4):816-830. https://doi.org/10.1093/ije/dyn099.
Checkley W, Epstein LD, Gilman RH, Black RE, Cabrera L, Sterling CR. Effects of Cryptosporidium parvum infection in Peruvian children: growth faltering and subsequent catch-up growth. Am J Epidemiol. 1998;148(5):497–506.
Alexandre MAA, Benzecry SG, Siqueira AM, Vitor-Silva S, Melo GC, Monteiro WM, et al. The association between nutritional status and malaria in children from a rural Community in the Amazonian Region: a longitudinal study. PLoS Negl Trop Dis. 2015;9(4):e0003743.
Fink G, Olgiati A, Hawela M, Miller JM, Matafwali B. Association between early childhood exposure to malaria and children’s pre-school development: evidence from the Zambia early childhood development project. Malar J. 2013;12(1):1–9.
Lee G, Yori P, Olortegui MP, Pan W, Caulfield L, Gilman RH, et al. Comparative effects of vivax malaria, fever and diarrhoea on child growth. Int J Epidemiol. 2012;41(2):531–9.
Williams TN, Maitland K, Phelps L, Bennett S, Peto TEA, Viji J, et al. Plasmodium vivax: a cause of malnutrition in young children. QJM. 1997;90(12):751–7 Available from: http://www.ncbi.nlm.nih.gov/pubmed/9536339.
Jackson BD, Black RE. A Literature Review of the Effect of Malaria on Stunting. J Nutr. 2017:jn242289 Available from: https://academic.oup.com/jn/article/147/11/2163S-2168S/4743207.
Maleta KM, Phuka J, Alho L, Cheung YB, Dewey KG, Ashorn U, et al. Provision of 10–40 g/d lipid-based nutrient supplements from 6 to 18 months of age does not prevent linear growth faltering in Malawi. J Nutr. 2015;145(8):1909–15.
Ashorn P, Alho L, Ashorn U, Cheung YB, Dewey KG, Gondwe A, et al. Supplementation of maternal diets during pregnancy and for 6 months postpartum and infant diets thereafter with Small-quantity lipid-based nutrient supplements does not promote child growth by 18 months of age in rural Malawi: a randomized controlled Tria. J Nutr. 2015;145(6):1345–53 Available from: http://jn.nutrition.org/cgi/doi/10.3945/jn.114.207225.
National Statistical Office (NSO) [Malawi] and ICF. Malawi Demographic and Health Survey 2015–16. Zomba, Malawi, Rockville: NSO and ICF; 2017.
National Malaria Control Programme (NMCP) [Malawi] and ICF International. Malawi Malaria Indicator Survey (MIS) 2012. Lilongwe, Malawi, and Calverton, Maryland, USA: NMCP and ICF International; 2012.
Rousham EK, Northrop-Clewes CA, Lunn PG. Maternal reports of child illness and the biochemical status of the child: the use of morbidity interviews in rural Bangladesh. Br J Nutr. 1998;80(5):451–6.
Kroeger A. Health interview surveys in developing countries: a review of the methods and results. Int J Epidemiol. 1983;12(4):465–81.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85 Available from: http://www.ncbi.nlm.nih.gov/pubmed/16817681.
Abubakar A, Holding P, van Baar A, Newton CRJC, van de Vijver FJR. Monitoring psychomotor development in a resource-limited setting: an evaluation of the Kilifi developmental inventory. Ann Trop Paediatr. 2008;28(3):217–26.
Fenson L, Marchman VA, Thal DJ, Dale PS, Steven Reznick J, Bates E. The MacArthur-bates communicative development inventories User’s guide and technical manual. Baltimore: Paul H. Brookes Publishing Co; 2006.
Prado EL, Phuka J, Maleta K, Ashorn P, Ashorn U, Vosti SA, et al. Provision of lipid-based nutrient supplements from age 6 to 18 months does not affect infant development scores in a randomized trial in Malawi. Matern Child Health J. 2016;20(10):2199–208.
Prado EL, Maleta K, Ashorn P, Ashorn U, Vosti SA, Sadalaki J, et al. Effects of maternal and child lipid-based nutrient supplements on infant development: a randomized trial in Malawi. Am J Clin Nutr [Internet]. 2016;103(3):784–93 Available from: http://ajcn.nutrition.org/cgi/doi/10.3945/ajcn.115.114579.
Morris SS, Cousens SN, Kirkwood BR, Arthur P, Ross DA. Is prevalence of diarrhea a better predictor of subsequent mortality and weight gain than diarrhea incidence? Am J Epidemiol. 1996;144(6):582–8.
Beard JL. Indicators of iron status of populations: free erythrocyte protoporphyrin and zinc protoporphyrin; serum and plasma iron, total iron binding capacity and transferrin receptor; and serum transferrin receptor. In: WHO, CDC, editor. Assessing the iron status of populations. Geneva: World Health Organization; 2007.
Dewey KG, Domellöf M, Cohen RJ, Landa Rivera L, Hernell O, Lönnerdal B. Iron supplementation affects growth and morbidity of breast-fed infants: results of a randomized trial in Sweden and Honduras. J Nutr. 2002;132(11):3249–55.
World Health Organization. Nutritional anaemias: tools for effective prevention and control. Geneva: World Health Organization; 2017.
Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6.
Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide, vol. 3. Washington, D.C: Food and Nutrition Technical Assistance Project, Academy for Educational Development; 2007.
Yelland LN, Sullivan TR, Makrides M. Accounting for multiple births in randomised trials: a systematic review. Arch Dis Child - Fetal Neonatal Ed. 2015;100(2):F116–20 Available from: http://fn.bmj.com/lookup/doi/10.1136/archdischild-2014-306239.
World Health Organization. Programme of Acute Respiratory Infections., World Health Organization. Malaria Control Unit. The Overlap in the clinical presentation and treatment of malaria and pneumonia in children : report of a meeting (Geneva, 8 April 1991). 1992.
Luxemburger C, Nosten F, Kyle DE, Kiricharoen L, Chongsuphajaisiddhi T, White NJ. Clinical features cannot predict a diagnosis of malaria or differentiate the infecting species in children living in an area of low transmission. Trans R Soc Trop Med Hyg. 1998;92(1):45–9.
Bojang KA, Obaro S, Morison LA, Greenwood BM. A prospective evaluation of a clinical algorithm for the diagnosis of malaria in Gambian children. Trop Med Int Heal. 2000;5(4):231–6 Available from: http://doi.wiley.com/10.1046/j.1365-3156.2000.00538.x.
World Health Organization. Treatment of Severe Malaria, Guidel Treat Malar; 2015. p. 71–88.
National Statistical Office (NSO) and ICF Macro. Malawi Demographic and Health Survey 2010. Zomba, Malawi, and Calverton, Maryland, USA: NSO and ICF Macro; 2011
Chandramohan D, Jaffar S, Greenwood B. Use of clinical algorithms for diagnosing malaria. Trop Med Int Heal. 2002;7(1):45–52.
World Health Organization. IMCI chart booklet: WHO. World Health Organization; 2014. [cited 7 Nov 2018]. Available from: https://www.who.int/maternal_child_adolescent/documents/IMCI_chartbooklet/en/
Streiner DL. Best (but oft-forgotten) practices: the multiple problems of multiplicity-whether and how to correct for many statistical tests. Am J Clin Nutr. 2015;102(4):721–8.
Gone T, Lemango F, Eliso E, Yohannes S, Yohannes T. The association between malaria and malnutrition among under-five children in Shashogo District, southern Ethiopia: a case-control study. Infect Dis Poverty. 2017;6(1):4–11. https://doi.org/10.1186/s40249-016-0221-y.
Hautvast JLA, Tolboom JJM, Willems JL, Mwela CM, Monnens LAH. Consequences of infections for three-month length increment in young children in rural Zambia. Acta Paediatr. 2000;89(3):296–301.
Olney DK, Kariger PK, Stoltzfus RJ, Khalfan SS, Ali NS, Tielsch JM, et al. Development of nutritionally at-risk young children is predicted by malaria, anemia, and stunting in Pemba, Zanzibar. J Nutr. 2009;139(4):763–72 Available from: http://www.ncbi.nlm.nih.gov/pubmed/19225131.
Kang H, Kreuels B, Adjei O, Krumkamp R, May J, Small DSDS. The causal effect of malaria on stunting: a Mendelian randomization and matching approach. Int J Epidemiol. 2013;42(5):1390–8.
Victora CG, Barros F, Kirkwood B, Vaughan J. Pneumonia, diarrhea, and growth in the first 4 y of life: a longitudinal study of 5914 urban Brazilian children. Am J Clin Nutr. 1990;52(2):391–6.
Solomons NW, Mazariegos M, Brown KH, Klasing K. The underprivileged, developing country child: environmental contamination and growth failure revisited. Nutr Rev. 1993;51(11):327–32.
Nyakeriga AM, Troye-Blomberg M, Chemtai AK, Marsh K, Williams TN. Malaria and nutritional status in children living on the coast of Kenya. Am J Clin Nutr. 2004;190(3):1604–10.
Rowland MG, Cole TJ, Whitehead RG. A quantitative study into the role of infection in determining nutritional status in Gambian village children. Br J Nutr. 1977;37(3):441–50 Available from: http://www.ncbi.nlm.nih.gov/pubmed/861194.
Boivin MJ, Sikorskii A, Familiar-Lopez I, Ruiseñor-Escudero H, Muhindo M, Kapisi J, et al. Malaria illness mediated by anaemia lessens cognitive development in younger Ugandan children. Malar J. 2016;15(1):1–12.
Das BS, Thurnham DI, Das DB. Influence of malaria on markers of iron status in children: implications for interpreting iron status in malaria-endemic communities. Br J Nutr. 1997;78(5):751–60.
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500–24. Avalable from: https://www.ncbi.nlm.nih.gov/pubmed/25046751.
Perumal N, Bassani DG, Roth DE. Use and misuse of stunting as a measure of child health. J Nutr. 2018;148(3):311–5 Available from: https://academic.oup.com/jn/article/148/3/311/4930811.
Olofin I, McDonald CM, Ezzati M, Flaxman S, Black REFW. Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: a pooled analysis of ten prospective studies. PLoS one. 2013;8(5) Available from: https://doi.org/10.1371/journal.pone.0064636.
Poskitt EME, Cole TJ, Whitehead RG. Less diarrhoea but no change in growth: 15 years’ data from three Gambian villages. Arch Dis Child. 1999;80(2):115–20.
Moy R, CMTF D, Choto R, McNeish A, Booth I. Diarrhoea and growth faltering in rural Zimbabwe. Eur J Clin Nutr. 1994;11(48):810–21.
Briend A, Hasan K, Aziz K, Hoque B. Are diarrhoea control programmes likely to reduce childhood malnutrition? Observations from rural Bangladesh. Lancet. 1989;2:319–22.
Dewey KG, Mayers DR. Early child growth: how do nutrition and infection interact? Matern Child Nutr. 2011;7(SUPPL. 3):129–42.
Mbuya MNN, Humphrey JH. Preventing environmental enteric dysfunction through improved water, sanitation and hygiene: an opportunity for stunting reduction in developing countries. Matern Child Nutr. 2016;12:106–20.
Acknowledgements
The authors thank the study participants, the local communities of Mangochi, the health service staff and their research personnel at the study sites as well as members of the trial’s data safety and monitoring board, the iLiNS extended research team and the iLiNS-Project Steering Committee for their contributions in all stages of the study.
Funding
This publication is funded by a grant to the University of California, Davis from the Bill & Melinda Gates Foundation. The findings and conclusions contained within the article are those of the authors and do not necessarily reflect positions or policies of the Bill & Melinda Gates Foundation. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of this manuscript.
Availability of data and materials
The datasets used and analysed during this study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows: KM, JP, KGD, YBC, UA, and PA designed the study; JB, NP, JM, CM, LH, JP, YBC, UA, ELP, KGD, PA, and KM conducted the study; JB analysed the data and wrote the paper, with critical input and comments from all other authors; JB and KM had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed according to International Conference of Harmonization–Good Clinical Practice (ICH-GCP) guidelines and the ethical standards of the Helsinki Declaration. The protocol was reviewed and approved by the Institutional Review Boards of the University of Malawi, College of Medicine (IRB reference number P.01/09/722) and the Pirkanmaa Hospital District, Finland (IRB reference number R09130). At least one guardian signed or thumb-printed an informed consent form before enrolment of each participant. An independent data safety and monitoring board monitored the incidence of suspected SAE during the trial.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bendabenda, J., Patson, N., Hallamaa, L. et al. The association of malaria morbidity with linear growth, hemoglobin, iron status, and development in young Malawian children: a prospective cohort study. BMC Pediatr 18, 396 (2018). https://doi.org/10.1186/s12887-018-1378-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-018-1378-2