Abstract
Background
Studies conducted mainly in high-income countries have shown that preterm births are associated with increased risk of behavioral problems and psychiatric disorders. The aim of this study was to assess the prevalence of behavioral problems from middle-childhood to early-adolescence according to gestational age at birth in a middle-income setting.
Methods
A population-based birth cohort (n = 4231) in Pelotas, Brazil, was followed-up in several occasions from birth to 11 years. Estimated GA was based on last menstrual period or, when unknown or inconsistent, on the Dubowitz method. Behavioral problems were assessed at 4 (Child Behavior Checklist - CBCL), and at 6 and 11 years (Development and Well-Being Assessment - DAWBA) tool. Maternal socio-economic characteristics and depression at 2, 4 and 6 years post-partum, child perinatal characteristics and breastfeeding duration were used as confounders. Analyses were run by linear and logistic regression.
Results
Three thousand two hundred four children had full information on gestational age, CBCL and DAWBA. At 4 years, mean total (42.9 ± 24.0) and mean externalizing (18.8 ± 9.1) CBCL scores were higher among preterm girls born at <34 weeks than among full term girls (33.2 ± 15.1 and 15.0 ± 6.6, respectively). After controlling for confounders the association was no longer significant. At the age of 6 years there was no association between gestational age and behavior, neither in crude nor in adjusted analyses. Odds ratio for any psychiatric disorders at 11 years was 60% (1.6; 1.1–2.1) higher among those born at 34–36 weeks than in full-term children, but the association disappeared in adjusted analyses.
Conclusion
At this large cohort, behavioral problems from middle-childhood to early-adolescence are more related to family socio-economic characteristics and to other child perinatal conditions than to gestational age at birth.
Similar content being viewed by others
Background
The effect of gestational age at birth, particularly the effect of prematurity (gestational age < 37 weeks) and early prematurity (< 34 weeks) has been subject of several studies worldwide. [1,2,3] Although the majority of preterm babies survive without impairment, studies have shown that preterm births are associated with increased risk of neonatal and infant mortality, [4,5,6] besides of predicting offspring morbidity across lifespan, including psychiatric disorders, academic problems, and social difficulties [7, 8].
Worldwide, the preterm birth rates range from 5% in high-income countries to 25% in low- and middle-income countries. [9] Since 1990, prematurity rates are increasing in all countries with reliable time trend data [10]. According to the World Health Organization estimates preterm rates are highest in general for low-income countries (11.8%), followed by lower middle-income countries (11.3%) and lowest for upper middle- and high-income countries (9.4 and 9.3%, respectively) [7]. Despite the fact that most of the preterm births take place in low- and middle-income countries, the available literature on the consequences of gestational age over behavioral problems later in life comes mainly from studies carried out in high-income countries and the results of the studies are inconsistent [1].
In Brazil, one of the top 10 countries with the highest numbers of preterm births worldwide, [7] the prevalence of psychiatric disorders in childhood, adolescence and adulthood is higher than in high-income countries, [11,12,13,14,15] turning it a suitable place to explore the association between prematurity and mental health. This study was planned to compare the prevalence of internalizing and externalizing symptoms at four, six and 11 years of age according to gestational age at birth among children from a population-based birth cohort.
Methods
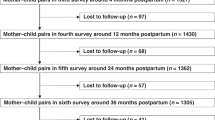
From January 1st to December 31st, 2004, all live births of mothers delivering at the maternity hospitals in Pelotas, a Southern Brazilian city, and residing at the urban area of the city were eligible to the Pelotas 2004 Birth Cohort. More than 99% of all deliveries took place in one of the five maternity hospitals available in the city. Mothers were interviewed soon after delivery regarding demographic, socio-economic, behavioral and biological characteristics, reproductive history, and health care services utilization. The non-response rate at recruitment was below 1%. A total of 4231 live births were enrolled in the cohort. Follow-ups were done at home at mean ages 3.0 ± 0.1, 11.9 ± 0.2, 23.9 ± 0.4 and 49.5 ± 1.7 months, and at a research clinic at 6.8 ± 0.3 and 10.9 ± 0.3 years, with follow-up rates between 86 and 96%. A detailed description of the methodology is given elsewhere [16].
Estimates of gestational age were based on the last menstrual period (LMP) providing they were consistent with predicted birth weight, length, and head circumference, based on the normal curves for these parameters for each week of gestational age. [17] If LMP-based gestational age was unknown or inconsistent, the clinical maturity estimate based on the Dubowitz method, [18] which was performed on almost all newborns, was adopted. Gestational age was categorized as extremely preterm (< 28 weeks), very preterm (28–31 weeks), moderate preterm (32–33 weeks), late preterm (34–36 weeks of gestations), and full term newborns (≥ 37 weeks) [19].
Adverse behavioral outcomes were assessed at four, six and 11 years of age. At the four-year follow-up children were assessed for the presence of behavioral/emotional problems by the application of the Child Behavioral Checklist (CBCL) to mothers or caregivers. [20] The instrument provides scores on eight scales: withdrawn, somatic complaints, anxious/depressed, social problems, thought problems, attention problems, aggressive behavior and rule-breaking behavior. Data from these scales were summed to provide an overall score (total problems) and two broad dimensions (internalizing and externalizing problems). The CBCL was validated among Brazilian children [21].
At the six and 11-year follow-ups children were assessed using the Development and Well-Being Assessment (DAWBA) tool, [22] an instrument designed to assess psychiatric disorders according to The International Classification of Diseases-Tenth Revision (ICD-10), The Diagnostic and Statistical Manual of Mental Disorders-4th Edition, and The Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition criteria for ages 5–17 years. [23, 24] The instrument was validated in the Brazilian population. [25] Trained psychologists administered the DAWBA to mothers or caregivers. A computerized algorithm provided the probability of a child having any psychiatric disorder based on responses to the structured questions, but clinical Raters (two experienced child psychiatrists) provided the final evaluation. The Raters reviewed the symptoms and the negative impact of symptoms over the child relationship within the family and with persons from the social environment, as well as all the qualitative information in their own assessment [26]. Externalizing disorders included oppositional defiant disorder, conduct disorder and any Attention Deficit Hyperactivity Disorder (ADHD), including hyperactive, inattentive and combined sub-types and ADHD not otherwise specified. Internalizing disorders included diagnoses of anxiety and depression. For comparability, in the present analyses the ICD-10 criteria were used.
Information on family income in the month prior to delivery; maternal schooling, age, skin color, living with a partner, parity, smoking during pregnancy, depression (assessed at 2-, 4- and 6-year follow-ups and defined as probable when the Edinburgh Post-natal Depression Score was ≥13), [27] and type of delivery were collected. At birth, child sex, low birth weight (birth weight < 2500 g), Apgar score at 1st and 5th minutes, and need of intensive care were recorded. Information on hospital admissions in the first year and breastfeeding duration (<12, 12–23.9 and ≥24 months) was gathered.
Only single births were included in the analyses. Due to the small number of children born at <34 weeks, the extremely, very and moderate preterm births were grouped into <34 weeks for the analyses. The CBCL scores were analyzed as continuous outcome in original score units (a higher score reflects greater problems). To assess the association between gestational age and CBCL scores ANOVA analysis was conducted. Multivariate linear regression was used to estimate the effect of gestational age at birth over total, internalizing and externalizing problems at age 4 years adjusting for potential confounding factors in separate models. Potential confounders were grouped and included in the adjusted analysis using a backward strategy selection. If the significance level was below 0.20 the variable remained in the model as a potential confounder for the next level [28].
Psychiatric disorders at six and 11 years (any psychiatric disorder, internalizing and externalizing disorders) were analyzed as dichotomous outcomes. Pearson X 2 tests were used to assess the association between gestational age and the outcomes. Crude and adjusted analyses were carried out with logistic regression. Because there was no effect modification by child sex, the adjusted linear and logistic regression analyses were carried out with the whole sample, having child sex as a confounding variable.
Results
A total of 3204 children were followed-up from birth to 11 years of age and had full information on gestational age at birth, CBCL at four years and DAWBA at six and 11 years of age. Among them, 416 (12.9%) were preterm. Prevalence of late preterm (34–36 weeks) and preterms <34 weeks was 10.6 and 2.3%, respectively.
Tables 1 and 2 show that gestational age groups were different in regard to several background characteristics. Preterm births were more prevalent among low-income families and among non-white, adolescent mothers with lower level of formal education (Table 1). In Table 2, prevalence of low Apgar at 1st and 5th minutes and low birth weight were higher among preterm newborns that also required intensive care more frequently than the full-term newborns. Breastfeeding was interrupted earlier and hospitalizations during infancy were more frequent among preterm than among term infants. There was no difference in prevalence of maternal depression at 24 months and at 6 years after delivery between the different gestational ages, whereas depression was higher among mothers of preterm born children at the 48-month follow-up.
In Table 3, mean CBCL total score was higher among girls born at <34 weeks (42.9 ± 24.0) and at 34–36 weeks (35.7 ± 17.9) than among girls born full term (33.5 ± 15.9) (p = 0.001). Mean externalizing scores were also higher among preterm than among full-term girls. Among boys, mean internalizing problems score was higher among those born at 34–36 weeks (6.8 ± 4.7) in comparison to those born at term (6.1 ± 4.3) (p = 0.045).
In Table 4, after allowing for family income, maternal marital status, skin color, schooling, age, parity, and smoking during pregnancy, type of delivery, child sex, low birth weight, Apgar at 1st and 5th minutes, and intensive care hospitalization at birth, the association between gestational age and total CBCL score at age 4 years disappeared. In the same way, the association between preterm birth and internalizing and externalizing problems at 4 years observed in crude analyses, disappeared after adjusting to family income, and maternal marital status, skin color and schooling.
Two girls and three boys born at <34 weeks of gestation presented any psychiatric disorder at the age of 6 years (Table 5). At 11 years, three girls and seven boys born at <34 weeks presented any psychiatric disorder. Prevalence of any psychiatric disorder among late preterm girls and boys at 6 years was 12.7 and 15.9%, respectively. At 11 years, late preterm girls and boys had a prevalence of any psychiatric disorders of 12.7 and 17.6%, respectively. There was no difference in prevalence of behavior problems at six and 11 years according to gestational age.
No association was observed between gestational age and psychiatric disorders neither in crude nor in adjusted analyses (Table 6) at the age of 6 years. At 11 years, the odds ratio for any psychiatric disorder was 60% (1.6; 1.1–2.1) higher among late preterms in comparison to full-term children. At the full adjusted model (Model 5) the highest odds for any psychiatric disorder was seen for late preterm children at 11 years (OR = 1.5; 1.0–2.1), but the confidence interval of the estimate overlapped the null value (Table 6).
Discussion
After controlling for a number of critical confounders, this study found no association between preterm birth and increased risk of behavioral problems at the age of four, 6 and 11 years. The lack of association of gestational age with behavioral problems and psychiatric disorders at three different ages of the same cohort participants reinforces the finding of no association between them.
This finding is in line with results of other studies. [29, 30] In the United States, healthy late-preterm infants were compared with their full-term counterparts from age four through 15 years for numerous standard cognitive, achievement, socio-emotional, and behavioral outcomes. [29] No differences were found between late-preterm and full-term children. Through age 15 years, the mean difference of most of the outcomes hovered around 0.
Also, in a large nationally representative Australian cohort of 5000 children, aged 0 to 1, 2 to 3, and 4 to 5 years of age, children born at 33–36 weeks were compared with healthy-term peers. Child mental health was measured by mother-report on the Strengths and Difficulties Questionnaire. [31] There were small increases in emotional symptoms and total difficulties for the preterm group at age four to 5 years. After adjusting for maternal and socio-demographic factors, preterm birth continued to predict emotional symptoms but not total difficulties at age four to 5 years [30].
Other studies, most of them conducted in high-income countries, have reported higher risks for internalizing and externalizing problems and psychiatric morbidity among the preterm children. [1,2,3, 32] Contextual factors may play a role at the observed difference between the studies. For instance, an analysis comparing single-born children from the Pelotas 2004 birth cohort at the age of 6 years with children of similar age from the Avon Longitudinal Study of Parents and Children, in the United Kingdom, to investigate whether birth exposures play a causal role in the development of childhood attention problems, showed that whereas Attention Deficit Hyperactivity Disorder (as assessed by means of DAWBA) was associated with preterm birth among children from the British cohort (OR = 2.33, 95% CI 1.23–4.42), there was no association with gestational age in the Pelotas cohort. [33] Compared to gestational age at birth, social, health and economic factors may play a greater role in the development of behavioral problems in middle-income than in high-income settings.
A higher social risk, represented by low parental educational level, younger maternal age, and low socio-economic status, is strongly associated with increased behavior problems. [1, 34,35,36] Maternal clinical depression and anxiety have a negative influence on mother-infant interaction and this in turn affects the behavioral outcome of the children. [37,38,39] All these risk factors are more prevalent in low and middle-income settings. Such characteristics of the confounding structure were controlled for in the current study.
Medical factors, such as the length of stay in a neonatal intensive care unit, a prolonged need for artificial ventilation and postnatal corticosteroid exposure may negatively affect behavioral outcome. [1] The access to full intensive care technology and the survival rate after intensive care management are higher among preterm children born in high-income than among those born in low and middle-income settings. Lack of adjustment for such characteristics may positively confound the association between age at birth and behavioral outcomes of the children.
Preterm children that were included in the current analyses are a subsample of all preterm babies that belonged to the cohort. The neonatal mortality rate during the year of 2004 in Pelotas was of 12.7‰ live births [40] (three times higher than that for high-income countries in that year - 4‰). [41] The majority of deaths was due to preterm-related complications. [40] Single babies born at <34 weeks represented 22.3% (125/561) of all preterm births and more than one fifth of them (22%) (28/125) died at the neonatal period whereas 77% (75/97) of the survivors were entered in the current analysis. Moreover, more than half of those born at <28 weeks died in the first week of life (16/25; 64%). The high neonatal and post-neonatal mortality rates among preterm newborns in the present study may have excluded from the analyses the most severely impaired children.
Among the strengths of this study is the large population-based birth cohort with a small rate of losses and refusals in all the waves of follow-up. The instruments employed to measure the outcome (CBCL and DAWBA) were validated for use in the Brazilian population. A number of critical co-variables, including maternal depression and family environmental characteristics, were entered in the adjusted analyses, so minimizing the likelihood of residual confounding that can spuriously lead to associations that are biased due to the lack of control for important confounders.
On the other hand, a limitation is that the study relied only on the mother or the caregiver perspective for the assessment of the children behavioral functioning (the CBCL and DAWBA versions for teachers were not applied). Teachers and parents tend to notice different kinds of behavior problems. [42] At the age of 6 years, many of the cohort children were not yet attending the school and the remaining were at the beginning of the school life. Even so, information on teachers’ complaints regarding the child behavior was gathered from the mother during the six-year and 11-year interview and was used by the Rater when judging for the presence of emotional problem. Additionally, children with different risks may have been inappropriately pooled into the <34 weeks group thus impairing the study capacity of assessing their behavioral outcomes [43].
Conclusion
There was no association between gestational age and behavioral problems at four, six and 11 years of age among children enrolled in the Pelotas 2004 Birth Cohort and followed-up from birth to 11 years in a middle-income setting. Behavioral problems from middle-childhood to early-adolescence were more related to family socio-economic characteristics than to GA age at birth. This study highlights the importance of targeting children from families with less favorable socio-economic conditions, a risk factor that co-occur with preterm birth in low and middle-income settings, with the aim of preventing behavioral problems in childhood and adolescence.
Abbreviations
- ADHD:
-
Attention Deficit Hyperactivity Disorder
- ANOVA:
-
Analysis of variance
- CBCL:
-
Child Behavioral Checklist
- DAWBA:
-
Development and Well-Being Assessment
- ICD-10:
-
International Classification of Diseases-Tenth Revision
- LMP:
-
Last menstrual period
- SDQ:
-
Strengths and Difficulties Questionnaire
References
Arpi E, Ferrari F. Preterm birth and behaviour problems in infants and preschool-age children: a review of the recent literature. Dev Med Child Neurol. 2013;55(9):788–96.
Johnson S, Marlow N. Preterm birth and childhood psychiatric disorders. Pediatr Res. 2011;69(5 Pt 2):11R–8R.
Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics. 2009;124(2):717–28.
Lawn JE, Kinney MV, Black RE, Pitt C, Cousens S, Kerber K, Corbett E, Moran AC, Morrissey CS, Oestergaard MZ. Newborn survival: a multi-country analysis of a decade of change. Health Policy Plan. 2012;27(Suppl 3):iii6–28.
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61.
Santos IS, Matijasevich A, Silveira MF, Sclowitz IK, Barros AJ, Victora CG, Barros FC. Associated factors and consequences of late preterm births: results from the 2004 Pelotas birth cohort. Paediatr Perinat Epidemiol. 2008;22(4):350–9.
Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller AB, Kinney M, Lawn J. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013;10(Suppl 1):S2.
McGowan JE, Alderdice FA, Holmes VA, Johnston L. Early childhood development of late-preterm infants: a systematic review. Pediatrics. 2011;127(6):1111–24.
Lawn JE, Gravett MG, Nunes TM, Rubens CE, Stanton C, Group. GR: GLobal report on preterm birth and stillbirth (1 of 7): definitions, description of the burden and opportunities to improve data. BMC Pregnancy Childbirth 2010, 10 (Suppl 1):S1.
Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, Adler A, Vera Garcia C, Rohde S, Say L, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379(9832):2162–72.
Matijasevich A, Murray E, Stein A, Anselmi L, Menezes AM, Santos IS, Barros AJ, Gigante DP, Barros FC, Victora CG. Increase in child behavior problems among urban Brazilian 4-year olds: 1993 and 2004 Pelotas birth cohorts. J Child Psychol Psychiatry. 2014;55(10):1125–34.
Anselmi L, Fleitlich-Bilyk B, Menezes AM, Araujo CL, Rohde LA. Prevalence of psychiatric disorders in a Brazilian birth cohort of 11-year-olds. Soc Psychiatry Psychiatr Epidemiol. 2010;45(1):135–42.
Anselmi L, Barros FC, Minten GC, Gigante DP, Horta BL. Victora CG. [prevalence and early determinants of common mental disorders in the 1982 birth cohort, Pelotas, southern Brazil]. Rev Saude Publica. 2008;42(Suppl 2):26–33.
Murray J, Anselmi L, Gallo EA, Fleitlich-Bilyk B, Bordin IA. Epidemiology of childhood conduct problems in Brazil: systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2013;48(10):1527–38.
Murray J, Maughan B, Menezes AM, Hickman M, MacLeod J, Matijasevich A, Goncalves H, Anselmi L, Gallo EA, Barros FC. Perinatal and sociodemographic factors at birth predicting conduct problems and violence to age 18 years: comparison of Brazilian and British birth cohorts. J Child Psychol Psychiatry. 2015;56(8):914–22.
Santos IS, Barros AJ, Matijasevich A, Zanini R, Chrestani Cesar MA, Camargo-Figuera FA, Oliveira IO, Barros FC, Victora CG. Cohort profile update: 2004 Pelotas (Brazil) birth cohort study. Body composition, mental health and genetic assessment at the 6 years follow-up. Int J Epidemiol. 2014;43(5):1437–1437a-f.
Fenton TR. A new growth chart for preterm babies: Babson and Benda's chart updated with recent data and a new format. BMC Pediatr. 2003;3:13.
Dubowitz LM, Dubowitz V, Goldberg C. Clinical assessment of gestational age in the newborn infant. J Pediatr. 1970;77(1):1–10.
WHO. Recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14 , 1976. Acta Obstet Gynecol Scand. 1977;56(3):247–53.
Achenbach T. Manual for the child behavior checklist/4–18 and 1991 profile. Burlington: Department of Psychiatry, University of Vermont; 1991.
Bordin I, Mari J, Caeiro M. Validação da versão brasileira do Child Behavioral Checklist CBCL-Inventário de Comportamentos da Infância e Adolescência: dados preliminares. Rev Bras Psiquiatr. 1995;17:55–66.
Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The development and well-being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry. 2000;41(5):645–55.
WHO. The ICD-10 classification of mental and behavioral disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993.
APA. Diagnostic and statistical manual of mental disorder (DSM-IV-fourth version). Washington: American Psychiatric Association; 1994.
Fleitlich-Bilyk B, Goodman R. Prevalence of child and adolescent psychiatric disorders in southeast Brazil. J Am Acad Child Adolesc Psychiatry. 2004;43(6):727–34.
Ford T, Last A, Henley W, Norman S, Guglani S, Kelesidi K, Martin AM, Moran P, Latham-Cork H, Goodman R. Can standardized diagnostic assessment be a useful adjunct to clinical assessment in child mental health services? A randomized controlled trial of disclosure of the development and well-being assessment to practitioners. Soc Psychiatry Psychiatr Epidemiol. 2013;48(4):583–93.
Santos IS, Matijasevich A, Tavares BF, Barros AJ, Botelho IP, Lapolli C, Magalhaes PV, Barbosa AP, Barros FC. Validation of the Edinburgh postnatal depression scale (EPDS) in a sample of mothers from the 2004 Pelotas birth cohort study. Cad Saude Publica. 2007;23(11):2577–88.
Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138(11):923–36.
Gurka MJ, LoCasale-Crouch J, Blackman JA. Long-term cognition, achievement, socioemotional, and behavioral development of healthy late-preterm infants. Arch Pediatr Adolesc Med. 2010;164(6):525–32.
Westrupp EM, Mensah FK, Giallo R, Cooklin A, Nicholson JM. Mental health in low-to-moderate risk preterm, low birth weight, and small for gestational age children at 4 to 5 years: the role of early maternal parenting. J Am Acad Child Adolesc Psychiatry. 2012;51(3):313–23.
Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. 1997;38(5):581–6.
Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA. 2002;288(6):728–37.
Murray E, Pearson R, Fernandes M, Santos IS, Barros FC, Victora CG, Stein A, Matijasevich A. Are fetal growth impairment and preterm birth causally related to child attention problems and ADHD? Evidence from a comparison between high-income and middle-income cohorts. J Epidemiol Community Health. 2016;70(7):704–9.
de Laat SA, Essink-Bot ML, van Wassenaer-Leemhuis AG, Vrijkotte TG. Effect of socioeconomic status on psychosocial problems in 5- to 6-year-old preterm- and term-born children: the ABCD study. Eur Child Adolesc Psychiatry. 2016;25(7):757–67.
Potijk MR, de Winter AF, Bos AF, Kerstjens JM, Reijneveld SA. Behavioural and emotional problems in moderately preterm children with low socioeconomic status: a population-based study. Eur Child Adolesc Psychiatry. 2015;24(7):787–95.
Potharst ES, van Wassenaer AG, Houtzager BA, van Hus JW, Last BF, Kok JH. High incidence of multi-domain disabilities in very preterm children at five years of age. J Pediatr. 2011;159(1):79–85.
Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: a sensitive period? J Am Acad Child Adolesc Psychiatry. 2010;49(7):699–707.
Loomans EM, van der Stelt O, van Eijsden M, Gemke RJ, Vrijkotte T, den Bergh BR. Antenatal maternal anxiety is associated with problem behaviour at age five. Early Hum Dev. 2011;87(8):565–70.
Feldman R, Bamberger E, Kanat-Maymon Y. Parent-specific reciprocity from infancy to adolescence shapes children's social competence and dialogical skills. Attach Hum Dev. 2013;15(4):407–23.
Barros AJ, Matijasevich A, Santos IS, Albernaz EP, Victora CG. Neonatal mortality: description and effect of hospital of birth after risk adjustment. Rev Saude Publica. 2008;42(1):1–9.
Save the Children. State of the world’s newborns. 2001: A report from saving newborn’s lives. Washington; 2001.
Konold TR, Pianta RC. The influence of informants’ on ratings of children’s behavioral functioning: a latent variable approach. J Psychoeduc Assess. 2007;25(3):222–36.
Richards JL, Drews-Botsch C, Sales JM, Flanders WD, Kramer MR. Describing the shape of the relationship between gestational age at birth and cognitive development in a nationally representative U.S. Birth Cohort. 2016;30(6):571–82.
Acknowledgements
Not applicable
Funding
This article is based on data from the study “Pelotas Birth Cohort, 2004” conducted by Postgraduate Program in Epidemiology at Universidade Federal de Pelotas, with the collaboration of the Brazilian Public Health Association (ABRASCO). From 2009 to 2013, the Wellcome Trust supported the 2004 birth cohort study (Grant number 086974/Z/08/Z). The World Health Organization (Process number 03014HNI), National Support Program for Centers of Excellence (PRONEX) (Process number 04/0882.7), Brazilian National Research Council (CNPq) (Process numbers 481,012–2009-5; 484,077–2010-4; 470,965–2010-0; and 481,141–2007-3), Brazilian Ministry of Health (Process number 4589–04), and Children’s Pastorate supported previous phases of the study. Iná S. Santos, Fernando C. Barros and Alicia Matijasevich receive support from the National Council for Scientific and Technological Development (CNPq), Brazil. The study sponsors had no involvement in study design; the collection, analysis, and interpretation of data; the writing of the report; nor in the decision to submit the paper for publication. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
ISS and AM conceived the work, conducted the analyses and draft the first version of the manuscript. TNM made substantial contributions to acquisition and interpretation of data. FCB revised the manuscript critically and contributed with interpretation of the findings. All authors gave final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Medical Ethics Committee of the Federal University of Pelotas approved the study protocol and all follow-ups of the Pelotas 2004 Birth Cohort Study. Mothers signed a consent form on behalf of them and their children at each follow-up, after being informed of the study objectives. At the 11-year follow-up, the cohort participants aged 11 years or more also signed an informed consent form.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Santos, I.S., Barros, F.C., Munhoz, T. et al. Gestational age at birth and behavioral problems from four to 11 years of age: birth cohort study. BMC Pediatr 17, 184 (2017). https://doi.org/10.1186/s12887-017-0936-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-017-0936-3