Abstract
Purpose
The objective of this study was to evaluate anterior segment parameters across various phenotypes of polycystic ovary syndrome (PCOS), considering body mass index (BMI), serum estradiol and testosterone levels.
Materials and Methods
This prospective study included 116 women with PCOS, with each of the four distinct phenotype comprising 29 women. Additionally, 29 healthy women were included in the control group. All participants underwent comprehensive ophthalmologic examinations, including intraocular pressure (IOP) measurements. Anterior segment parameters, such as central corneal thickness (CCT), axial length (AL), aqueous depth (AD), anterior chamber depth (ACD), and lens thickness (LT) were measured using optic biometry. Endothelial cell density (ECD) was assessed using non-contact specular microscopy. The BMI was calculated, and serum levels of estradiol and testosterone were noted.
Results
IOP was found to be significantly higher (p = 0.003) and CCT was significantly thicker (p = 0.004) in all phenotypes of PCOS compared to the control group. BMI, serum estradiol and free testosterone were found to correlate with both IOP and CCT. AL, AD, ACD and LT values showed no significant differences compared to the control group. Although ECD tend to be higher in the PCOS phenotypes, this difference was not statistically significant (p > 0.05).
Conclusion
Given our findings that CCT and IOP are significantly elevated in PCOS phenotypes. PCOS should be considered as an important factor when evaluating female patients for anterior segment diseases and glaucoma.
Similar content being viewed by others
Introductıon
Polycystic ovary syndrome (PCOS) is the most prevalent endocrinopathies affecting women of reproductive age and stands as one of the leading causes of infertility [1]. It is a diverse endocrine disorder characterized by irregular or absent menstrual periods, elevated androgen levels, and the presence of numerous small cystic follicles beneath the ovarian capsule, as identified through ultrasonography [2]. PCOS is recognized as a risk factor for obesity, insulin resistance, metabolic disorders, and cardiovascular issues; it often involves insulin resistance and hyperinsulinemia, which contribute to increased androgen production and reduced sex hormone-binding globulin levels, playing a critical role in the development of hyperandrogenism [3].The NIH 2012 Evidence-Based Methodology Workshop on PCOS recommended classifying PCOS into four distinct phenotypes, adapting and broading the Rotterdam 2003 criteria. This approach aims to refine the characterization of PCOS, elucidate associated risk factors, maximize clinical care and delineate peripheral effects [4].
Recent research showed that estrogen, progesterone, and androgens affect various eye structures such as the cornea, lens, iris, ciliary body, retina, lacrimal glands, and meibomian glands [5,6,7]. These hormones are believed to influence blood-retinal barrier regulation, neuroprotection, vascular regulation, and intraocular pressure (IOP) modification at the eye level, suggesting potential roles in the pathogenesis of various ocular disorders [8]. Recent advancements in ocular imaging techniques enable researchers to obtain high-quality images of anterior segment structures and assist in detecting changes across various systemic disease processes.
In the current study, we aimed to compare IOP, anterior segment parameters, including axial length (AL), aqueous depth (AD), anterior chamber depth (ACD), and lens thickness (LT), specular microscopy findings, and central corneal thickness (CCT) between patients with distinct PCOS phenotypes and healthy individuals. Additionally, we evaluated the relationships between these findings and body mass index (BMI), serum estradiol and testosterone levels.
Materıals and methods
This prospective case control study was conducted at the outpatient ophthalmology clinic in ophthalmology and Obstetrics and Gynecology Clinics department of Recep Tayyip Erdogan University from August 2020 to July 2021 and was approved by the local human research ethics committee (2020/243). All patients included in this study gave their informed consent, which adhered to the tenets of the Declaration of Helsinki, and written informed consent was obtained from all subjects.
Our study enrolled 116 women diagnosed with PCOS and differentiated by sub-phenotypes, at the Obstetrics and Gynecology Clinics between August 2020 and July 2021. Additionally, we recruited 29 healthy volunteer women with regular menstrual cycles and normal ovarian morphology, employed at our hospital. None of the participants were pregnant. Detailed medical data and personal medical history were obtained from all participants.
PCOS diagnosis followed the Rotterdam 2003 Criteria, encompassing oligomenorrhea (defined as more than 35 days between menses or experiencing eight or fewer menses per year), clinical and/or biochemical evidence of hyperandrogenism (evidenced by clinical symptoms such as hirsutism, acne, androgenic alopecia, or laboratory findings such as elevated serum total and free testosterone levels), and ultrasonographic evidence of polycystic ovaries (characterized by the presence of 12 or more follicles measuring 2–9 mm in diameter and/or increased ovarian volume exceeding 10 mL). A single ovary meeting these criteria was deemed sufficient for a PCOS diagnosis.
Phenotyping was conducted subsequent to PCOS diagnosis, identifying four distinct phenotypes: A, B, C, and D [4]. Phenotype A fulfilled all three criteria (menstrual irregularity, hyperandrogenism, and PCO appearance on ultrasound), Phenotype B presented with menstrual irregularity and hyperandrogenism without ultrasound evidence, Phenotype C exhibited hyperandrogenism and PCO appearance on ultrasound, and Phenotype D demonstrated only menstrual irregularity and PCO appearance on ultrasound without hyperandrogenism. Patients were categorized into one of these four groups based on phenotypic criteria, and their information was recorded accordingly.
Following diagnosis at the Obstetrics and Gynecology Clinics, patients underwent necessary ultrasound and laboratory assessments. Venous blood samples were collected from women during the early follicular phase of their menstrual cycle (days 3–5), either after the onset of spontaneous menstruation or progesterone-induced bleeding. These samples were obtained from the antecubital veins between 08:00 and 09:00 in the morning, following a 12-h fast. Luteinizing hormone (LH), follicle stimulating hormone (FSH), estradiol, and total/free testosterone levels were measured.
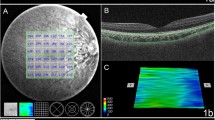
Subsequently, patients included in the study were referred to the ophthalmology clinic, with no specific phenotype notified. Each patient was provided with a comprehensive ophthalmological examination, encompassing a fundus examination, biomicroscopy, tonometry and determination of optimal visual acuity. IOP was measured using Goldman applanation tonometry (Nikon, Japan) in the morning between 9:00 and 11:00 A.M. Ocular biometric parameters, including AL, AD, ACD, LT, and CCT were measured using non-contact ocular biometry, Lenstar LS 900 (Haag-Streit, Inc., Koeniz, Switzerland). One sample image is shared in Fig. 1. ECD was assessed using non-contact specular microscopy Tomey EM-4000 (Tomey Corporation, Japan). An experienced ophthalmic technician took five readings for each eye. The mean of the remaining three readings was utilized for analysis after excluding the highest and lowest values. Data from right eyes were used for the evaluation.
Subjects with hormonal drug use or congenital or acquired endocrine disorders were excluded from the study. Furthermore, the study excluded participants with a history of contact lens use, glaucoma, ocular surgery, trauma, keratorefractive surgery, refractive errors greater than 2 diopters, or any anomalies related to the cornea, lens, or ocular surface.
Statistical analysis
Data were analysed with IBM SPSS programme. Compliance with normal distribution within and between groups was analysed by Kolmogorov-Smirnow and Shapiro Wilk tests. Mann Whitney U test was used to compare non-normally distributed data according to binary groups. Normally distributed data were analysed by one-way analysis of variance and non-normally distributed data were analysed by Kruskall Wallis H test. Fisher's exact test was used to investigate categorical data according to groups, and multiple comparisons were analysed by Z test with Bonferroni correction. The relationships between quantitative characteristics that were not normally distributed were analysed with Spearman's rho correlation coefficient. The results of the analyses were presented as mean ± standard deviation, median (minimum—maximum) for quantitative data and frequency (percentage) for categorical data. Significance level was taken as p < 0.05.
Results
The study comprised a total of 116 patients in the PCOS group, with each phenotype consisting of 29 patients, and 29 healthy women in the control group. The mean age was 22.02 ± 11 years (ranging from 17 to 28) in the PCOS group and 24.05 ± 08 years (ranging from 20 to 27) in the control group, with no significant difference in terms of age between the groups. There was no statistically significant difference in age between the phenotypes and when compared with the control group. BMI, serum estradiol and free testosterone levels were compared between the groups. BMI and serum estradiol levels were significantly higher in PCOS phenotypes compared to the control group (p < 0.001). Free testosterone levels were significantly higher in PCOS phenotypes except for phenotype D compared to the control group. (p < 0.001).Serum estradiol and free testosterone levels were compared between phenotypes, phenotype A was found to have a statistically significant difference (p = 0.002, p = 0.001).BMI levels were compared, phenotype A had the highest value among phenotypes, but this did not cause a statistically significant difference between phenotypes (p > 0.05). Although free testosterone levels were higher in phenotype D than in the control group, this was not statistically significant (p > 0.05). These results are summarized in Table 1.
The comparison of anterior segment parameters of the subjects with different phenotypes of PCOS and control group are shown in Table 2. The CCT was found to be significantly thicker in all phenotypes of PCOS compared to the control group (p = 0.004). When phenotypes were compared among themselves, no statistically significant difference was found although CCT was higher in phenotype A (p > 0.05). Additionally, IOP was observed to be significantly higher across all phenotypes of PCOS in comparison to the control group (p = 0.003). When phenotypes were compared among themselves, IOP was found to be higher in phenotype A compared to other phenotypes, but this was not statistically significant (p > 0.05). The mean ECD measured in PCOS phenotypes was 2745 ± 78.5, while in the control group it was 2693.4 ± 69.01. Although higher in the PCOS phenotypes, this difference was not statistically significant (p > 0.05). Furthermore, the differences in AL, AD, ACD, and LT between groups were not statistically significant.
Table 3 demonstrates the correlation between IOP and CCT with BMI, serum estradiol, and free testosterone in patients with PCOS. BMI, serum estradiol and free testosterone were found to correlate with both IOP (p < 0.001; r = 0.234, r = 0.198, r = 326, respectively) and CCT (p < 0.01; r = 169, r = 204, r = 258, respectively).
Dıscussıon
In the current study, we investigated the differences in anterior segment parameters in subjects with various phenotypes of PCOS. Our observations revealed that both CCT and IOP are significantly elevated in subjects with PCOS phenotypes, directly correlating with increasing levels of sex hormones. The differences in AL, AD, ACD, and LT between groups were not statistically significant.
Hyperandrogenism, a key feature of PCOS, contributes to exacerbating inflammation and oxidative stress, thereby significantly affecting cellular processes such as proliferation and differentiation [3]. The presence of sex steroid receptor mRNA has been observed in various ocular tissues, including the lens, retina, cornea, iris, ciliary body, lacrimal and meibomian glands, eyelid, conjunctiva, and cornea, as demonstrated by Wickham et al. [9]. While the precise impact of sex hormones on the cornea remains unclear, reports suggest that corneal epithelial and stromal fibroblasts express sex steroid receptors, and the cornea responds to fluctuations in serum levels of androgens and estrogens [10]. Changes in corneal thickness and biomechanical properties during menstrual cycle have been reported in previous studies. Kiely et al. observed that corneal thickening occurs on the second day of the menstrual cycle and around the time of ovulation. This thickening is followed by thinning and a subsequent slight thickening on day 21. They suggested that these variations in corneal thickness are associated with fluctuations in estrogen levels [11]. Goldich et al. reported that corneal hysteresis and corneal resistance factor were temporarily reduced during ovulation. The cornea was thinnest at the start of the cycle and became thicker during ovulation and at the cycle's end [12]. Cengiz Ozturk et al. evaluated corneal topography and densitometry characteristics in patients with PCOS and reported an intensification of corneal densitometry values and alterations in keratometry data that suggest corneal ectasia [13].
Several studies have previously reported that patients with PCOS exhibit increased CCT [14, 15]. Hyperandrogenism and hyperinsulinemia, two primary components of PCOS, lead to dysregulation of the insulin-like growth factor-1 (IGF-1) system. This dysregulation stimulates and promotes the proliferation of corneal cells [16]. Researchers found that an elevated IGF-1 and insulin levels were associated with increased CCT in women with PCOS [17]. They attributed the increased CCT values to the chronic low-grade inflammation and the modulation of keratocytes and the synthesis of the corneal stromal extracellular matrix. Additionally, they suggested that elevated levels of IGF-1 inhibit the corneal endothelial pump, increase endothelial permeability, and subsequently increase stromal swelling pressure [17]. Furthermore it is well-known that hormonal disorders affect the tear film and ocular surface, subsequently resulting in dry eye disease. The tear film is essential for the lubrication, protection and metabolism of the cornea. Dysregulation in the tear film and ocular surface components may also lead to structural and biomechanical changes at the cornea level [8]. In our study, we observed that CCT was greater and correlated with increasing levels of serum estradiol and free testosterone across all phenotypes of PCOS, with these effects being most prominent in Phenotype A. The androgen level in Phenotype A was statistically higher than in the other phenotypes (p = 0.001) and this was positively correlated with CCT elevation. Additionally, we found that the mean ECD was higher in the PCOS phenotypes compared to the control group, although this difference was not statistically significant. Balıkçı et al. reported that ECD values were lower in the PCOS group, while Dağ et al. reported that the hexagonal cell ratio in the corneal endothelium of PCOS patients was higher than in healthy controls, without reaching statistical significance [18, 19].
In addition to CCT being an indicator of corneal rigidity and significantly influencing the accuracy of IOP measurements obtained through applanation tonometry, numerous human studies have found evidence that sex hormones affect IOP. Estrogens have been shown to have neuroprotective effects, reduce IOP, and increase ocular blood flow. Newman-Casey et al. concluded that estrogen-containing hormone replacement therapy may reduce the risk of primary open-angle glaucoma (OAG) in postmenopausal women [20]. Although the mechanisms by which changes in sex hormones in PCOS modulate IOP are not fully understood, hyperandrogenism is primarily considered to play a role in elevated IOP. Alpogan et al. reported that supraphysiological doses of testosterone led to an increase in IOP in female-to-male transgender individuals [21]. Toker et al. observed that higher serum testosterone levels were correlated with increased IOP in menopausal women [22]. Researchers reported that higher testosterone levels were linked with increased risk for OAG [23]. The mechanism by which testosterone increases IOP is believed to involve the reduction of eNOS activity in the trabecular meshwork and the suppression of aqueous humor outflow [24]. Since insulin resistance and obesity are contributors to PCOS, a higher BMI is a significant confounding factor in elevated IOP. According to a recent comprehensive review, there appears to be a noteworthy correlation between elevated IOP levels and excess body weight [25]. Zainab et al. observed that patients with PCOS had significantly higher BMI and exhibited higher IOP and CCT compared to age-matched females [26]. In our study, consistent with the literature, testosterone levels, BMI, and IOP were significantly higher in the PCOS group, with the most pronounced differences observed in phenotype A. We also investigated ocular biometric parameters including, AL, AD, ACD and LT; however, the differences in these parameters were not statistically significant between PCOS patients and the control group.
The strength of this study lies in its evaluation of PCOS patients according to four distinct phenotypes within a prospective, single-center framework. However, limitations include a relatively small population size, not considering the disease duration and the fact that ocular examinations were conducted at the same time of day, preventing the assessment of the effects of the circadian 24-h CCT rhythm on IOP. Additionally, examinations were conducted with a single device, and measurements were not confirmed with another device.
In conclusion, the current study observed thicker CCT and elevated IOP in young women with PCOS, correlating with increasing levels of sex hormones. Ophthalmologists should be aware of the potential changes in anterior segment structures, particularly when planning refractive surgery, fitting contact lenses, or conducting glaucoma and keratoconus follow-up in patients with PCOS.
Availability of data and materials
The data can be used at any time by obtaining permission from the authors.
Abbreviations
- AD:
-
Aqueous depth
- ACD:
-
Anterior chamber depth
- AL:
-
Axial length
- BMI:
-
Body mass index
- CCT:
-
Central corneal thickness
- ECD:
-
Endothelial cell density
- FSH:
-
Follicle stimulating hormone
- IGF-1:
-
Insulin-like growth factor-1
- IOP:
-
Intraocular pressure
- LH:
-
Luteinizing hormone
- LT:
-
Lens thickness
- OAG:
-
Open-angle glaucoma
- PCOS:
-
Polycystic ovary syndrome
References
Sirmans SM, Pate KA. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin Epidemiol. 2013;6:1–13.
Sadeghi HM, et al. Polycystic ovary syndrome: a comprehensive review of pathogenesis, management, and drug repurposing. Int J Mol Sci. 2022;23(2):583.
Hajam YA, et al. A review on critical appraisal and pathogenesis of polycystic ovarian syndrome. Endocr Metabol Sci. 2024;14:100162.
Mumusoglu S, Yildiz BO. Polycystic ovary syndrome phenotypes and prevalence: Differential impact of diagnostic criteria and clinical versus unselected population. Curr Opin Endocr Metab Res. 2020;12:66–71.
Gupta PD, et al. Sex hormone receptors in the human eye. Surv Ophthalmol. 2005;50(3):274–84.
Icoz M, Yuzbasıoglu S. Evaluation of choroidal thickness and choroidal vascular index in patients using combined oral contraceptive pills. Cutan Ocul Toxicol. 2023;42(4):232–6.
Icoz M, Gurturk-Icoz SG, Kolsuz-Koldamca H. Effect of oral contraceptive pills on the retinal microvascular structure: An optical coherence tomography angiography study. Photodiagnosis Photodyn Ther. 2023;42: 103635.
Nuzzi R, Caselgrandi P. Sex hormones and their effects on ocular disorders and pathophysiology: current aspects and our experience. Int J Mol Sci. 2022;23(6).
Wickham LA, Gao J, Toda I, et al. Identification of androgen, estrogen and progesterone receptor mRNAs in the eye. Acta Ophthalmol Scand. 2000;78(2):146–53. https://doi.org/10.1034/J.1600-0420.2000.078002146.X.
McKay TB, Priyadarsini S, Karamichos D. Sex hormones, growth hormone, and the cornea. Cells. 2022;11(2).
Kiely PM, Carney LG, Smith G. Menstrual cycle variations of corneal topography and thickness. Am J Optom Physiol Opt. 1983;60(10):822–9.
Goldich Y, et al. Variations in corneal biomechanical parameters and central corneal thickness during the menstrual cycle. J Cataract Refract Surg. 2011;37(8):1507–11.
Cengiz Ozturk TG, Akcam HT, Ellibes Kaya A. Pentacam corneal topography and densitometry features of PCOS patients. BMC Ophthalmol. 2023;23(1):5.
Puthiyedath R, et al. A comparative study on ocular manifestations in patients with polycystic ovary syndrome and healthy volunteers. Kerala J Ophthalmol. 2022;34(3):250–5.
Karaca Adıyeke S, et al. Anterior segment findings in women with polycystic ovary syndrome. Turk J Ophthalmol. 2017;47(1):24–7.
Feldman ST, et al. Stimulation of DNA synthesis and c-fos expression in corneal endothelium by insulin or insulin-like growth factor-I. Invest Ophthalmol Vis Sci. 1993;34(6):2105–11.
Kebapcilar AG, et al. Cornea in PCOS patients as a possible target of IGF-1 action and insulin resistance. Arch Gynecol Obstet. 2014;290(6):1255–63.
Balıkçı AT, Ulutaş HG, Özgen GA. Evaluation of meibomian gland morphology and anterior segment parameters by Sirius topography systems in polycystic ovary syndrome. Indian J Ophthalmol. 2022;70(8):2922–8.
Dağ ZÖ, Örnek N, Örnek K. Corneal endothelial cell density and morphology in patients with polycystic ovary syndrome. Turkiye Klinikleri J Ophthalmol. 2018;27(2):129–34.
Newman-Casey PA, et al. The potential association between postmenopausal hormone use and primary open-angle glaucoma. JAMA Ophthalmology. 2014;132(3):298–303.
Alpogan O, et al. Effects of testosterone on intraocular pressure, thicknesses of retinal nerve fiber layer, ganglion cell complex, macula and on ocular blood flow in female-to-male transgender persons. Int Ophthalmol. 2021;41:3651–61.
Toker E, Yenice O, Temel A. Influence of serum levels of sex hormones on intraocular pressure in menopausal women. J Glaucoma. 2003;12(5):436–40.
Vergroesen JE, et al. Higher testosterone is associated with open-angle glaucoma in women: a genetic predisposition? Biol Sex Differ. 2023;14(1):27.
Lee JS, et al. Cross sectional study among intraocular pressure, mean arterial blood pressure, and serum testosterone according to the anthropometric obesity indices in Korean men. World J Mens Health. 2021;39(4):697–704.
Waspodo N, et al. Role of excessive weight in intraocular pressure: a systematic review and meta-analysis. BMJ Open Ophthalmol. 2023;8(1):e001355.
Zainab Ali Mezher A, Mudhher Ghani A, Alaa Sabree Fakree A. The relation between intraocular pressure level and polycystic ovarian disease. Eurasian Med Res Period. 2022;13:114–9.
Acknowledgements
The authors would like to thank Mine Kaya for the statistical analysis of the study. Also, thanks to native speaker Mr. Jerremy Huggsfor editing the English of the article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
FS and BG. have constructed/constructed the main idea and hypothesis of the study. FS, BG, FU and EY developed the theory and arranged/edited the material and method section. FS has done the evaluation of the data in the Results section. Discussion section of the article. Written by FS.FU and MGA, SC, HA reviewed, corrected and approved. In addition, all authors discussed the entire study and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the local human research ethics committee from Recep Tayyip Erdogan University. Protocol number and date 2020/243 and 24.12.2020. All patients included in this study gave their informed consent, which adhered to the tenets of the Declaration of Helsinki, and written informed consent was obtained from all subjects. Consent was obtained from the patients. Consent was also obtained from our institution.
Consent for publication
Consent was obtained from the patients. Consent was also obtained from our institution.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sumer, F., Gurlek, B., Yildiz, E. et al. Variations in anterior segment parameters among different phenotypes of polycystic ovary syndrome. BMC Ophthalmol 24, 419 (2024). https://doi.org/10.1186/s12886-024-03676-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03676-3