Abstract
Objective
This study aimed to compare the one-year efficacy of myopia prevention and control using three optical intervention methods - single vision lens (SVL), high aspherical lenticule (HAL), and orthokeratology (OK) lens - in children with low myopia.
Methods
A cohort of 150 children aged 7–13 years with low myopia was recruited and divided into three groups: SVL (n = 50), HAL (n = 50), and OK lens group (n = 50), based on their preference for glasses. Follow-up assessments were carried out over one year, focusing on data from the right eye for statistical analysis. Baseline characteristics such as gender, age, axial length (AL), spherical equivalent refractive error (SER), flat keratometry (K1), steep keratometry (K2), anterior chamber depth (ACD), white-to-white corneal diameter (WTW), and non-contact tonometry (NCT) measurements were gathered and compared among the three groups before any intervention. Changes in AL growth after 1 year of intervention were assessed across the three groups. Subsequently, the AL growth control rates between the HAL and OK lens groups were compared, with the SVL group serving as the reference standard.
Results
The study found no statistically significant variances in baseline characteristics (gender, age, SER, AL, K1, K2, WTW, and NCT) among the SVL, HAL, and OK lens groups (all p > 0.05). Following a one-year intervention, AL growth rates were as follows: HAL group (0.163 ± 0.113 mm) < OK lens group (0.280 ± 0.170 mm) < SVL group (0.516 ± 0.190 mm), with statistically significant disparities (p < 0.05). The HAL group demonstrated a higher 1-year AL growth control rate (68.41%) compared to the OK lens group (45.74%) for children aged 7–13 with low myopia, with a statistically significant differences (p < 0.001). And there was significant difference in the SER change between SVL group and HAL group (p < 0.001).
Conclusion
Compared to SVL, HAL and OK lens are more effective in controlling axial growth in mild myopia. Specifically, HAL maybe shows superior outcomes in both preventive and corrective measures, also it needs to be supported by more studies from randomized controlled experiments.
Similar content being viewed by others
Background
Myopia is a significant global health issue, with projections suggesting that by 2050, 49.8% of the world’s population, totaling 4.758 billion individuals, will suffer from myopia, including 938 million with high myopia [1]. Low myopia is a transitional stage for children with varying degrees of myopia. Timely intervention at the onset of myopia could significantly reduce the prevalence of high myopia and its complications. Various strategies exist for preventing and managing myopia [2], including behavioral changes [3], environmental adjustments [4, 5], optical interventions [6, 7], pharmaceutical treatments like low-dose atropine [8, 9], and interventions such as repeated low-intensity red light (RLRL) exposure [10]. Optical interventions, such as single vision lenses (SVL), high aspherical lenticule (HAL), and orthokeratology (OK) lenses, are commonly used for children with myopia. This study aimed to compare the 1-year axial length (AL) growth differences in low myopia among three frequently used optical intervention methods: SVL, HAL, and OK lenses. The goal is to determine more suitable and effective optical interventions for preventing and managing low myopia in children, providing empirical evidence to support clinical strategies for myopia control.
Methods
Patients
A cohort of 150 children diagnosed with low myopia and receiving treatment at the Optometric Center of the First Affiliated Hospital of Guangxi University of Chinese Medicine during the period from May 1 to August 31, 2022, was included in the analysis. Inclusion criteria included: (1) children aged 7 to 13 years with myopia diagnosed in both eyes through astigmatism and optometry assessments; (2) individuals with a spherical equivalent refraction (SER) of -3.00D or higher and the difference between two eyes less than 1.50D; (3) those with a best corrected visual acuity of 0.8 or superior in both eyes. Exclusion criteria included: (1) participants who had utilized additional preventive measures, including RLRL, functional training, low-dose atropine eye drops, traditional Chinese medicine, etc., within the preceding six months apart from the prescribed intervention methods in this study; (2) individuals who were unable to consistently wear glasses or discontinue the use of OK lenses at their discretion during the intervention period; (3) intervention subjects with preexisting ocular conditions or those unsuitable for glasses or OK lenses, except for myopia, were not eligible for inclusion. This study was a prospective nonrandomized controlled study. All participants and their guardians provided written informed consent and provided permission for the results to be published anonymously. And the study adhered to the principles of the Helsinki Declaration, as approved by the Ethics Committee of Guangxi University of Traditional Chinese Medicine.
Sample size estimation
Bao J et al. [11]. have shown that the mean AL change was 0.36 ± 0.02 mm in the SVL group, 0.13 ± 0.02 mm in the HAL group, and 0.24 ± 0.17 mm in the OK lens group. Following formula was used to calculate the appropriate sample size for this study. σ was 0.17 and δ was 0.12. A test level α = 0.05 was adopted. The statistical power is set at 0.90. Zα was 1.96 and Zβ was 1.28. The minimum sample size required for this study was calculated to be 46, including the 10% of study participants who might be lost to follow-up. Each group in this study was 50 cases, which met the minimum sample size requirement for the study.
Interventions
SVL group: Subjects triedon the glasses according to the optometry prescription and mild adjustments were made based on the subjects’ subjective perception of wearing the glasses in order to obtain the final spherical equivalent refraction. The glasses were adjusted using the lowest negative spherical lens to optimize visual acuity. Refusing to wear glasses during activities like sleeping, eating, bathing, or engaging in strenuous exercise was recommended. Spectacles could be worn during meals if it didn’t affect the quality of vision and if the subject feltthat it didn’t affect vision. Nonetheless, they should be worn at all other times, with a daily minimum wear time of 8 h.
HAL group: The application of HAL with complete correction was mandated following the optometry principles and wearing time guidelines established for the SVL group. Stellest of Esssilor were employed in this investigation.
OK lens group: For optimal outcomes, wearing the night-wear OK lenses was imperative without interruption for at least 8 h overnight. The CRT OK lens utilized in this investigation was individualized with a 6.0 base curve.
Acquisition of specific parameters
Age was calculated as full age, for example, 9.1 to 9.9 years old would be counted as 9 years of age. Spherical equivalent refraction (SER = spherical + 1/2 cylindrical) was determined using 0.5% tropicamide eye drops (0.4/tube, Shenyang Xingqi Eye Medicine Co., Ltd., Liaoning, China) to induce ciliary muscle paralysis. Three drops were administered every 5 min, followed by a 30-minute waiting period. Refraction was assessed using an automatic computer refractometer (AR-310 A, Nidek, Japan), with three measurements taken and averaged. AL, flat keratometry (K1), steep keratometry (K2), anterior chamber depth (ACD), and white-to-white distance (WTW) were measured using IOL master (IOL master-500, Zeiss, Germany). Non-contact tonometry (NCT) values were obtained with a tonometer (NT-510, Nidec, Japan), with three measurements taken and averaged. All procedures were performed by the same trained personnel. The analysis focused on the specific indicators of the right eye in all study participants.
Statistical analysis
SPSS Statistics 24.0 software was used to analyze the data obtained in the study statistically. The normal distribution of numerical data was evaluated with the Shapiro-Wilk test. For all statistical analysis, data were expressed as mean ± standard deviation (SD) (x̅ ± s). One-way ANOVA tests were conducted to compare age, baseline AL, baseline SER, AL, K1, K2, ACD, WTW, and AL growth across three groups, with bonferroni test used for pairwise comparisons. Gender distribution and AL growth control rates between HAL and OK lens groups were evaluated through a four-grid chi-square test at a significance level of α = 0.05. Linear regression analysis was used to adjust for the effects of age and gender on 1-year AL growth. P value less than 0.05 was considered as statistical significant.
Results
Baseline comparison results revealed no statistically significant differences in gender, age, BCVA, SER, AL, NCT, ACD, corneal curvature, and corneal size among the SVL group, HAL group, and OK lens group (all p > 0.05) (Table 1).
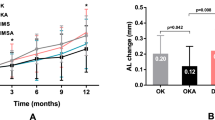
After a 1-year intervention, Table 2 displays the specific values for the three groups of study participants. The AL growth in the SVL group was 0.516 ± 0.190 mm; in the HAL group, it was 0.163 ± 0.113 mm, and in the OK lens group, it was 0.280 ± 0.170 mm. The sequence of AL growth was HAL group < OK lens group < SVL group, with statistically significant differences (Bonferroni test shows all p values < 0.05). The HAL group exhibited a 1-year AL growth control rate of 68.41% for children aged 7–13 with low myopia, in contrast to 45.74% in the OK lens group. The HAL group significantly surpassed the OK lens group (p < 0.001). The SER progression was reported in the SVL and HAL groups. The SER change in the SVL group was − 1.225 ± 0.467 mm, in the HAL group, it was − 0.304 ± 0.249 mm. And there was significant difference in the SER change between the two groups (p < 0.001).
Bonferroni test was utilized to conduct pairwise comparisons among three groups. Following a one-year intervention, the comparison of AL growth revealed statistically significant differences between the groups. After one year of intervention, the HAL group presented less growth compared to the OK lens group, and the OK lens group demonstrated less growth compared to the SVL group (Bonferroni test indicates that all p < 0.05).
Correlation analyses examined the relationship between age and AL growth across distinct groups. A significant negative correlation was observed between age and AL growth in the SVL group (r = -0.567, p < 0.001). Conversely, no statistically significant correlations were evident in the HAL group (r = -0.214, p = 0.135) or the OK lens group (r = -0.188, p = 0.191). These associations are visually depicted in Fig. 1.
In the linear regression analysis, age and gender were adjusted in Table 3. The results showed that compared with the SVL group, the HAL group showed a decrease of 0.357 (95% CI: -0.417, -0.297) in 1-year AL growth, while the OK lens group showed a decrease of 0.247 (95% CI: -0.307, -0.187) in 1-year AL growth. The differences were statistically significant (p < 0.001), when the reference group was set as the SVL group. For one year increase in age, the AL growth decreased by 0.036 (95% CI:-0.051, -0.020), and there was statistically significant (p < 0.001). However, there was no statistical difference in AL growth between female and male (p = 0.518).
Discussion
The age range of 7–13 years is a critical period in children’s growth and development, marked by the rapid progression of myopia [11, 12]. In China, myopia is categorized into low, moderate, and high myopia according to refractive error, low myopia ( < − 3.00D), moderate myopia (− 3.00 to − 6.00D), and high myopia (> -6.00D) [13, 14]. Low myopia is a significant transitional phase towards high myopia, playing a crucial role in myopia prevention and management. Optical interventions are commonly used to manage myopia in children. This study aims to evaluate and compare the effectiveness of three common optical interventions - SVL, HAL, and OK lenses - in controlling AL growth in children aged 7–13 years. The goal is to objectively distinguish the varying impacts of these optical interventions, providing empirical evidence to guide clinical practice.
Our study has demonstrated the efficacy of HAL and OK lens in preventing and managing myopia. The annual AL growth is significantly reduced with HAL (0.163 ± 0.113 mm) and OK lens (0.280 ± 0.170 mm) compared to SVL (0.516 ± 0.190 mm). HAL act as specialized defocusing lenses. These results indicate that after one year of intervention using three optical methods, both HAL and OK lenses were more successful in controlling AL growth in children with low myopia compared to SVL group. Among these, HAL, followed by OK lenses, demonstrated the most effective control.
In a one-year randomized double-blind controlled trial by Bao et al. [15], involving individuals aged around 10.4 years with moderate to low myopia, the group using HAL exhibited an AL growth of 0.13 ± 0.02 mm, resulting in an AL growth control rate of 64%, whereas the single lens group showed an AL growth of 0.36 ± 0.02 mm. In this study, the one-year AL growth in the SVL group was higher than that of Bao et al., the growth in the HAL group was similar, and the AL control rate (68.41%) was slightly higher than that in the their study. This may be related to the fact that the subjects in this study were low myopia and the mean age was different from subjects of the Bao J et al. ( < − 3.00D vs. between − 0.75 D and − 4.75 D; 9.6 years old vs. 10.4 years old). Children who present with myopia at a very young age tend to show faster myopia progression [14, 15]. Myopia typically begins to develop from about 6 years old and exhibits faster rates of progression below 10 years old [16]. As reported in studies on children and adolescents with low and moderate myopia, the prevention and control effect of defocus-incorporated multiple segment lenses (DIMS) are basically the same as that of OK lens [16, 17]. However, for children with low myopia, the results of this study show that HAL, a kind of defocus-incorporated multiple segment lens, may be slightly better than OK lens in preventing and controlling myopia, this finding highlights the unique aspect of this study. It has to be recognized that the small sample size included in this study may have had some impact on the results. Subsequent research by Bao et al. over 2 to 3 years further supported the effectiveness of HAL in controlling myopia [18, 19]. This study also investigated the impact of gender and age on AL growth with HAL and OK lens, finding no gender differences or significant age-related correlations. In contrast, wearing SVL is associated with a negative correlation between age and AL growth, suggesting that older individuals experience slower AL growth. These results indicates that wearing HAL and OK lens within 1 year is not much associated with age. But this correlation analysis did not account for the effects of other factors, so a linear regression analysis is used for further analysis. These results also suggest that HAL can effectively manage myopia progression in children aged 7 to 13 with low myopia, irrespective of gender. However, for children of different ages, for each year increase in age, AL growth decreased by 0.036(95% CI:-0.051, -0.020), and there were statistical differences. However, confirming this conclusion would require larger sample sizes and longer study durations.
The OK lens, a rigid, high-oxygen-permeable contact lens with an anti-geometric design, is commonly utilized for myopia management in children and adolescents. Extensive clinical studies [20, 21] have validated its safety and efficacy. A recent investigation by the research team led by Xiaomei Qu [22] examined 249 children using OK lenses, noting an annual AL growth of 0.21 ± 0.15 mm, slightly lower than the results of our study (0.280 ± 0.170 mm). This may be because they studied children with moderate to low myopia, with a baseline SER of -3.03 ± 1.11 diopter (D), as opposed to the low myopia in our study, with a baseline SER of -1.717 ± 0.524 diopter. Similarly, a study on children aged 8–12 with myopia conducted by Shengsong Xu et al. [23]. reported a 1-year AL increase of 0.24 ± 0.17 mm in participants with moderate to low myopia. The findings of previous studies [24, 25] have demonstrated a consistent trend of an annual increase in AL ranging from 0.20 to 0.25 mm, regardless of lens eccentricity. This pattern is consistently observed across multiple research investigations [26]. However, limited research exists on the therapeutic effects of OK lenses on low myopia. This study seeks to address this gap by comparing the efficacy of OK lenses with other optical interventions to determine the optimal optical strategies for managing low myopia in children.
This study employed a HAL obtained from Stellest of Esssilor Lens Company, characterized by an optical center of 9 mm surrounded by 11 rings. The lens design allows a gradient defocusing range from + 3.50D to + 5.50D across the rings [27]. The HAL group demonstrated an AL growth control rate of 68.41% compared to the 45.74% rate observed in the OK lens group. This discrepancy may be attributed to the more pronounced and consistent peripheral defocus induced by the HAL in cases of low myopia. Nevertheless, further investigation is necessary to confirm this finding.
There are some limitations of this study. Firstly, the number of cases in each group of 50 cases is small, which is prone to selection bias, although it has met the minimum sample size requirements. The more patients are enrolled in the group, the more credible the results will be. Secondly, the observation period is not long enough. If the observation period is longer, it will be able to evaluate the long-term prevention and control effect of the three myopia preventions and control methods on low myopia. Finally, there is the limitation of non-randomized enrollment. Because the subjects had to purchase the lenses at their own expense, complete randomization could not be achieved. If there is sufficient funding in the future, the lenses can be purchased uniformly to achieve the goal of randomized enrollment.
Conclusion
In conclusion, the one-year comparative study analysis suggests that HAL and OK lenses are more effective than SVL in managing AL growth in children with low myopia. No statistically significant correlation was found between gender. Both interventions prove to be successful in the prevention and control of myopia progression. Notably, HAL demonstrates superior efficacy in controlling AL growth, positioning them as a top-tier optical intervention for managing low myopia in pediatric clinical practice.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- SVL:
-
Single vision lens
- HAL:
-
High aspherical lenticule
- OK:
-
Orthokeratology
- SER:
-
Spherical equivalent refraction
- D:
-
Diopter
- AL:
-
Axial length
- K1:
-
Flat keratometry
- K2:
-
Steep keratometry
- ACD:
-
Anterior chamber depth
- WTW:
-
White-to-white distance
- NCT:
-
Non-contact tonometry
- LRL:
-
low-intensity red light
- SD:
-
Standard deviation
- DIMS:
-
Defocus-incorporated multiple segment lenses
References
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–42.
Russo A, Boldini A, Romano D, Mazza G, Bignotti S, Morescalchi F, Semeraro F. Myopia: Mechanisms and Strategies to Slow Down Its Progression. J Ophthalmol 2022, 2022:1004977.
He X, Sankaridurg P, Wang J, Chen J, Naduvilath T, He M, Zhu Z, Li W, Morgan IG, Xiong S, et al. Time outdoors in reducing myopia: a School-based Cluster Randomized Trial with Objective Monitoring of Outdoor Time and Light Intensity. Ophthalmology. 2022;129(11):1245–54.
Li X, Li L, Qin W, Cao Q, Mu X, Liu T, Li Z, Zhang W. Urban Living Environment and Myopia in Children. JAMA Netw Open. 2023;6(12):e2346999.
Biswas S, El Kareh A, Qureshi M, Lee DMX, Sun CH, Lam JSH, Saw SM, Najjar RP. The influence of the environment and lifestyle on myopia. J Physiol Anthropol. 2024;43(1):7.
Liu YL, Lin KK, Cheng LS, Lin CW, Lee JS, Hou CH, Tsai TH. Efficacy of multifocal soft contact lenses in reducing myopia progression among Taiwanese schoolchildren: a Randomized Paired-Eye Clinical Trial. Ophthalmol Ther. 2024;13(2):541–52.
Garcia-Del Valle AM, Blazquez V, Gros-Otero J, Infante M, Culebras A, Verdejo A, Sebastian J, Garcia M, Bueno S, Pinero DP. Efficacy and safety of a soft contact lens to control myopia progression. Clin Exp Optom. 2021;104(1):14–21.
Yam JC, Zhang XJ, Zhang Y, Yip BHK, Tang F, Wong ES, Bui CHT, Kam KW, Ng MPH, Ko ST, et al. Effect of low-concentration atropine eyedrops vs Placebo on Myopia incidence in children: the LAMP2 Randomized Clinical Trial. JAMA. 2023;329(6):472–81.
Ha A, Kim SJ, Shim SR, Kim YK, Jung JH. Efficacy and safety of 8 atropine concentrations for Myopia Control in Children: A Network Meta-Analysis. Ophthalmology. 2022;129(3):322–33.
Jiang Y, Zhu Z, Tan X, Kong X, Zhong H, Zhang J, Xiong R, Yuan Y, Zeng J, Morgan IG, et al. Effect of repeated low-level Red-Light Therapy for Myopia Control in children: a Multicenter Randomized Controlled Trial. Ophthalmology. 2022;129(5):509–19.
McCullough S, Adamson G, Breslin KMM, McClelland JF, Doyle L, Saunders KJ. Axial growth and refractive change in white European children and young adults: predictive factors for myopia. Sci Rep. 2020;10(1):15189.
Tideman JWL, Polling JR, Vingerling JR, Jaddoe VWV, Williams C, Guggenheim JA, Klaver CCW. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018;96(3):301–9.
Xi L, Zhang C, He Y. Single-step transepithelial photorefractive keratectomy in the treatment of mild, moderate, and high myopia: six month results. BMC Ophthalmol. 2018;18(1):209.
Ningli Wang JG, Li X, Yao K. Xinghuai Sun: Ophthalmology. In: The third edition. Volume 17. Beijing: The peoples medical publishing house; 2015: 410.
Bao J, Yang A, Huang Y, Li X, Pan Y, Ding C, Lim EW, Zheng J, Spiegel DP, Drobe B, et al. One-year myopia control efficacy of spectacle lenses with aspherical lenslets. Br J Ophthalmol. 2022;106(8):1171–6.
Zhang W, Tan X. Effects of Orthokeratology Lens Compared to Defocus Incorporated Multiple Segments Lens for adolescent myopia and factors related to corneal Injury. Altern Ther Health Med; 2024.
Lu W, Ji R, Jiang D, Shi L, Ding W, Tian Y, Zhao C, Leng L. Different efficacy in myopia control: comparison between orthokeratology and defocus-incorporated multiple segment lenses. Cont Lens Anterior Eye. 2024;47(2):102122.
Chen J, Zhuo R, Chen J, Yang A, Lim EW, Bao J, Drobe B, Spiegel DP, Chen H, Hou L. Spectacle lenses with slightly aspherical lenslets for myopia control: clinical trial design and baseline data. BMC Ophthalmol. 2022;22(1):345.
Li X, Huang Y, Yin Z, Liu C, Zhang S, Yang A, Drobe B, Chen H, Bao J. Myopia control efficacy of spectacle lenses with Aspherical Lenslets: results of a 3-Year Follow-Up study. Am J Ophthalmol. 2023;253:160–8.
Singh K, Bhattacharyya M, Goel A, Arora R, Gotmare N, Aggarwal H. Orthokeratology in Moderate Myopia: a study of predictability and safety. J Ophthalmic Vis Res. 2020;15(2):210–7.
Bullimore MA, Johnson LA. Overnight orthokeratology. Cont Lens Anterior Eye. 2020;43(4):322–32.
Wang B, Naidu RK, Qu X. Factors related to axial length elongation and myopia progression in orthokeratology practice. PLoS ONE. 2017;12(4):e0175913.
Xu S, Li Z, Zhao W, Zheng B, Jiang J, Ye G, Feng Z, Long W, He L, He M, et al. Effect of atropine, orthokeratology and combined treatments for myopia control: a 2-year stratified randomised clinical trial. Br J Ophthalmol. 2023;107(12):1812–7.
Chen Z, Zhou J, Xue F, Qu X, Zhou X. Two-year add-on effect of using low concentration atropine in poor responders of orthokeratology in myopic children. Br J Ophthalmol. 2022;106(8):1069–72.
Kinoshita N, Konno Y, Hamada N, Kanda Y, Shimmura-Tomita M, Kaburaki T, Kakehashi A. Efficacy of combined orthokeratology and 0.01% atropine solution for slowing axial elongation in children with myopia: a 2-year randomised trial. Sci Rep. 2020;10(1):12750.
Sun L, Li ZX, Chen Y, He ZQ, Song HX. The effect of orthokeratology treatment zone decentration on myopia progression. BMC Ophthalmol. 2022;22(1):76.
Erdinest N, London N, Lavy I, Berkow D, Landau D, Morad Y, Levinger N. Peripheral Defocus and Myopia Management: a Mini-review. Korean J Ophthalmol. 2023;37(1):70–81.
Acknowledgements
None.
Funding
The study was supported by Guangxi Key Research and Development Plan (No. GuikeAB20238029), Fund Project of Guangxi University of Chinese Medicine Introduced Doctoral Scientific Research (No. 2022BS027).
Author information
Authors and Affiliations
Contributions
XW designed research; WL and CD conducted research and wrote the paper; WL performed statistical analysis; YZ and YJ collected data and conducted follow-up visits; HL had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Guangxi University of Traditional Chinese Medicine, China. All participants and their guardians provided written informed consent and provided permission for the results to be published anonymously.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lai, W., Diao, C., Li, H. et al. Three optical intervention methods for low myopia control in children: a one-year follow-up study. BMC Ophthalmol 24, 319 (2024). https://doi.org/10.1186/s12886-024-03598-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03598-0