Abstract
Backgroud
The aim of this study was to investigate the associations between fluctuation in blood pressure (BP), ocular perfusion pressure (OPP) and visual field (VF) progression in normal-tension glaucoma (NTG).
Methods
This prospective, longitudinal study included 44 patients with NTG. Only newly diagnosed NTG patients who had not been treated with a glaucoma medication were included. Patients were examined every year for 7 years. Intraocular pressure (IOP), heart rate (HR), systolic BP (SBP), diastolic BP (DBP), ocular perfusion pressure (OPP), and diastolic ocular perfusion pressure (DOPP) were measured at the same time. Ophthalmic examinations, including perimetry, were performed also. Initial VF were compared with follow-up data after 7 years.
Results
After 7 years of follow-up, 9 of the 44 patients showed VF progression. The standard deviation (SD) of SBP and OPP were significantly associated with VF progression (P = 0.007, < 0.001, respectively). Multiple regression analysis showed that VF progression was significantly associated with SD of OPP (odds ratio, OR = 2.012, 95% CI = 1.016–3.985; P = 0.045).
Conclusions
Fluctuation in OPP was associated with VF progression in patients with NTG.
Similar content being viewed by others
Background
Intraocular pressure (IOP) is the most important causative risk factor for glaucoma [1, 2]. Previous studies have shown that lowering IOP slows visual field (VF) progression even in patients with normal-tension glaucoma (NTG) [1, 2]. However, several studies have shown that glaucoma often progressed, even when the IOP had been lowered [1, 3]. The investigators proposed that a combination of factors other than IOP was significantly associated with progression. Vascular factors have also been identified as risk factors [4,5,6].
Our previous population comprised of Korean adults revealed that patients with higher blood pressure (BP) variability developed primary open angle glaucoma significantly more frequently than did patients with lower BP variability [7]. Fluctuation of BP may trigger ischemic damage in small cerebral vessels, and repetitive peaks and troughs in BP cause endothelial dysfunction and breakdown of the blood–brain barrier [8]. Although vascular factors have been studied as risk factors in glaucoma, they are more related to the progression rather development of glaucoma [9].
However, to our knowledge, no previous report has evaluated the association between progression of glaucoma and long-term fluctuation of BP including ocular perfusion pressure (OPP). In the present study, we evaluated the associations of fluctuation in BP with OPP and VF progression in NTG patients.
Methods
We conducted a single-center, prospective, longitudinal study. Newly diagnosed NTG patients who had not been treated with a glaucoma medication were recruited from the glaucoma clinic of Seoul St. Mary’s Hospital. This research was approved by the St. Mary’s Hospital Institutional Review Board and all relevant principles of the Declaration of Helsinki were followed. All eligible patients who were willing to participate signed an informed consent form approved by an institutional review board.
The inclusion criteria for this study were as follows: (1) an age of 45 to 75 years, (2) best-corrected visual acuity ≥ 20/30, (3) untreated IOP < 22 mmHg, (4) open angle on gonioscopy, (5) glaucomatous optic disc (diffuse or localized rim thinning, vertical cup-to-disc ratio > 0.6, and/or notching in the neuroretinal rim), (4) VF loss consistent with glaucoma (≥ 3 adjacent points significant at P < 0.05 with one of these points being significant at P < 0.01, or a cluster of ≥ 2 adjacent points significant at P < 0.01), and (6) central corneal thickness ranging from 540 to 560 μm. If both eyes met these criteria, one eye was randomly selected for analysis.
The exclusion criteria were (1) systemic diseases such as hypertension, arrhythmia or cardiovascular disease which could affect BP or heart rate (HR), (2) other ocular disease, such as corneal abnormalities or retinal disease, and (3) a history of intraocular surgery, argon laser treatment, or laser trabeculoplasty.
Newly diagnosed NTG patients were examined at baseline (without medication), and they then started to use one anti-glaucoma eyedrop. Throughout the 7 year study period, the patients only ever used one eyedrop, and no patient underwent ocular surgery or laser treatment. All participants visited the hospital every 3 or 6 months according to the routine glaucoma treatment schedule and underwent ophthalomic examination including IOP measurement, VF examination using the Swedish interactive threshold algorithm Standard 24 − 2 (Humphrey; Carl Zeiss Meditec). All participants were specifically asked to visit the hospital at 4:00 P.M on ‘the study days’ at one-year intervals and were examined in terms of IOP, HR, systolic BP (SBP), and diastolic BP (DBP). Only test results measured on ‘the study days’ (8 times in total) were used in this study. Every IOP measurement was obtained by one blinded glaucoma specialist. The IOP values at each visit were the average of three consecutive measurements obtained using Goldmann applanation tonometry. The HR, SBP and DBP of the brachial artery were measured twice in the sitting position using a standard automated BP cuff. The average value of the two measurements was used.
OPP and diastolic OPP (DOPP) were calculated using the following formulae:
The standard deviation (SD) of SBP and DBP were calculated from the respective mean values at each visit. Fluctuations in IOP, BP, OPP, and DOPP were calculated as the SD over eight visits [7].
In this study, VF progression was defined using the Early Manifest Glaucoma Trial criteria [9, 12]. In the Early Manifest Glaucoma Trial, tentative VF progression was defined as three or more indicators of progression at the same location on three consecutive tests. Participants who showed tentative progression at their last visit 7 years later were reexamined 1 month thereafter to confirm VF progression. At the re-examination visit, only the VF test was performed. Patients were assigned to VF progression and non-progression groups.
The Mann-Whitney U test was used to compare the non-grogression and progression groups, because progression group is small samples (n = 9). To identify factors associated with progression, univariate and multivariate logistic regression analyses were performed. Variables significant at P < 0.05 in the univariate analysis were included in the multivariate model. We used Spearman correlation analysis to evaluate the relationships between VF progression and other variables. P values < 0.05 were considered to indicate statistical significance. All statistical analyses were performed using SPSS for Windows software (ver. 18.0; SPSS Inc., Chicago, IL, USA).
Results
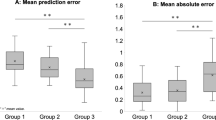
In total, 44 patients with NTG were enrolled in the study. Table 1 summarizes the demographic and clinical characteristics of the participants. Of the 44 patients, 9 demonstrated progression. Age, gender, IOP, refraction, baseline mean deviation, pattern SD, central corneal thickness, SBP, DBP, OPP, and DOPP showed no significant differences between the groups (Table 2). However, the visit-to-visit variability in SBP and OPP (defined on the basis of the SDs) differed significantly between the patients with and without progression ( P = 0.007 and P < 0.001 respectively; Table 2). The relationships between risk factors and VF progression were evaluated by logistic regression analysis. In the univariate analysis, progression was associated with the SD of SBP (odds ratio [OR] = 1.239; 95% confidence interval [CI] = 1.036–1.482; P = 0.019) and the SD of OPP (OR = 2.165; 95% CI = 1.205–3.891; P = 0.010; Table 3). In a subsequent multiple regression analysis, including progression as the dependent parameter and variables with P values < 0.05 in the univariate analysis as independent variables, progression was significantly associated with the SD of OPP (OR = 2.012, 95% CI = 1.016–3.985; P = 0.045; Table 3).
The relationship between the variables and VF progression were analyzed using Spearman correlation analysis. VF progression correlated significantly with the SD of SBP (ρ = 0.404, P = 0.007), SD of DBP (ρ = 0.300, P = 0.048), and SD of OPP (ρ = 0.522, P < 0.001). However, no significant correlation was detected between VF progression and gender, age, IOP, mean deviation, pattern SD, SBP, DBP, OPP, DOPP, the SD of IOP, or the SD of DOPP (Table 4).
Discussion
Elevated IOP is considered a major risk factor for glaucoma, and several vascular risk factors have also been identified [4, 13, 14]. Such vascular factors can lead to hypoperfusion of the optic disc and may contributes significantly to the progression of glaucoma [15,16,17,18,19,20].
Long-term repetitive fluctuation of BP may damage the vasculature [8]. Impaired vascular autoregulation affects the stability of ocular perfusion, and repeated ischemic/reperfusion injury triggers glaucomatous optic neuropathy [17, 21, 22].
Our previous study showed that patients with greater long-term BP variability developed primary open angle glaucoma significantly more frequently than did patients less variability (P < 0.001) in a large population-based cohort [7]. In the current study, long-term fluctuation of SBP and OPP were significantly associated with VF progression (P = 0.007 and P < 0.001, respectively). Multiple regression analysis showed that VF progression was significantly associated with the SD of OPP (OR = 2.012, 95% CI = 1.016–3.985; P = 0.045). In conclusion, BP fluctuation was associated with the progression of glaucoma in both studies.
Previously, Sung et al. showed that patients with NTG in the highest tertile of mean OPP fluctuation over 24 h were at greater risk of progressive VF loss than patients in the lowest fluctuation tertile [23]. They showed that short-term fluctuation of mean OPP was associated with VF progression in NTG patients. We measured visit-to-visit BP and showed that long-term fluctuation of OPP was associated with VF progression in patients with NTG. To our knowledge, this is the first report on a relationship between VF progression and long-term fluctuation of OPP in NTG patients.
A limitation of this prospective, longitudinal study should be acknowledged: the multivariate analysis had a relatively small sample size. However included participants who underwent full ophthalmic and systemic evaluation and checked BP at the same time during the follow-up period. In addition, the participants did not develop new systemic diseases and did not take systemic drug during the total observation period, which enhances the reliability of the study.
In summary, we found that long-term fluctuation of OPP was associated with VF progression in patients with NTG. Currently, interest in glaucoma treatment concerns not only IOP lowering but also vascular factors. This study highlights the risk of cardiovascular instability in association with glaucoma progression and suggests another way to manage glaucoma. Further studies are needed to more comprehensively investigate the role of vascular factors in VF progression in NTG patients.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Collaborative normal-tension Glaucoma Study Group. Am J Ophthalmol. 1998;126:487–97.
The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Collaborative normal-tension Glaucoma Study Group. Am J Ophthalmol. 1998;126:498–505.
Drance S, Anderson DR, Schulzer M. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. Am J Ophthalmol. 2001;131:699–708.
Sommer A. Intraocular pressure and glaucoma. Am J Ophthalmol. 1989;107:186–8.
Flammer J, Orgül S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21:359–93.
Gupta N, Ly T, Zhang Q, Kaufman PL, Weinreb RN, Yücel YH. Chronic ocular hypertension induces dendrite pathology in the lateral geniculate nucleus of the brain. Exp Eye Res. 2007;84:176–84.
Lee NY, Jung Y, Han K, Park CK. Fluctuation in systolic blood pressure is a major systemic risk factor for development of primary open-angle glaucoma. Sci Rep. 2017;7:43734.
Wardlaw JM, Farrall A, Armitage PA, Carpenter T, Chappell F, Doubal F, et al. Changes in background blood-brain barrier integrity between lacunar and cortical ischemic stroke subtypes. Stroke. 2008;39:1327–32.
Lee NY, Kim MH, Park CK. Visual field progression is Associated with systemic concentration of macrophage chemoattractant Protein-1 in Normal-Tension Glaucoma. Curr Eye Res. 2017;42:1002–6.
Costagliola C, Parmeggiani F, Virgili G, Lamberti G, Incorvaia C, Perri P, et al. Circadian changes of intraocular pressure and ocular perfusion pressure after timolol or latanoprost in caucasians with normal-tension glaucoma. Graefes Arch Clin Exp Ophthalmol. 2008;246:389–96.
Quaranta L, Gandolfo F, Turano R, Rovida F, Pizzolante T, Musig A, Gandolfo E. Effects of topical hypotensive drugs on circadian IOP, blood pressure, and calculated diastolic ocular perfusion pressure in patients with glaucoma. Invest Ophthalmol Vis Sci. 2006;47:2917–23.
Miglior S, Torri V, Zeyen T, Pfeiffer N, Vaz JC, Adamsons I. Intercurrent factors associated with the development of open-angle glaucoma in the European glaucoma prevention study. Am J Ophthalmol. 2007;144:266–75.
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP et al. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:701– 13; discussion 829– 30.
Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt J, Singh K. Relationship between intraocular pressure and primary open angle glaucoma among white and black americans. Baltim Eye Surv Arch Ophthalmol. 1991;109:1090–5.
Phelps CD, Corbett JJ. Migraine and low-tension glaucoma. A case-control study. Invest Ophthalmol Vis Sci. 1985;26:1105–8.
Hayreh SS. Factors influencing blood flow in the optic nerve head. J Glaucoma. 1997;6:412–25.
Anderson DR. Introductory comments on blood flow autoregulation in the optic nerve head and vascular risk factors in glaucoma. Surv Ophthalmol. 1999;43(Suppl 1):S5–9.
Drance S. Chronic open angle glaucoma: risk factors in addition to intraocular pressure. Acta Ophthalmol Scand. 2001;79:545.
Huck A, Harris A, Siesky B, Kim N, Muchnik M, Kanakamedala P, et al. Vascular considerations in glaucoma patients of African and European descent. Acta Ophthalmol. 2014;92:e336–40.
Chung HJ, Hwang HB, Lee NY. The Association between Primary Open-Angle Glaucoma and blood pressure: two aspects of hypertension and hypotension. Biomed Res Int. 2015;2015:827516.
Lee NY, Park HY, Park CK, Ahn MD. Analysis of systemic endothelin-1, matrix metalloproteinase-9, macrophage chemoattractant protein-1, and high-sensitivity C-reactive protein in normal-tension glaucoma. Curr Eye Res. 2012;37:1121–6.
Pillunat LE, Stodtmeister R, Wilmanns I, Christ T. Autoregulation of ocular blood flow during changes in intraocular pressure. Preliminary results. Graefes Arch Clin Exp Ophthalmol. 1985;223:219–23.
Sung KR, Lee S, Park SB, Choi J, Kim ST, Yun SC, et al. Twenty-four hour ocular perfusion pressure fluctuation and risk of normal-tension glaucoma progression. Invest Ophthalmol Vis Sci. 2009;50:5266–74.
Acknowledgements
We thank Michael Irvine, PhD, from Edanz (www.edanz.com/ac) for editing a draft of this manuscript.
Funding
The author(s) wish(es) to acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2023.
Author information
Authors and Affiliations
Contributions
Study concept and design: CKP; data collection NYL; analysis and interpretation of the data: DYS and NYL; writing the manuscript: DYS and NYL; critical revision of the manuscript: DYS and NYL; statistical expertise: DYS and NYL; administrative, technical, or material support: CKP; supervision: CKP.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the St. Mary’s Hospital Institutional Review Board and all relevant principles of the Declaration of Helsinki were followed. All eligible patients who were willing to participate signed informed consent from approved by an institutional review board.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, N.Y., Shin, D.Y. & Park, C.K. Associations of long-term fluctuation in blood pressure and ocular perfusion pressure with visual field progression in normal-tension glaucoma. BMC Ophthalmol 24, 209 (2024). https://doi.org/10.1186/s12886-024-03454-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03454-1