Abstract
Background
Retinopathy of prematurity (ROP) is a major cause of visual impairment in premature infants, often requiring surgical interventions in advanced stages. This retrospective case series study investigates non-surgical management for Stage 4A ROP, specifically the use of combined laser therapy and intravitreal anti-vascular endothelial growth factor (VEGF) injections.
Methods
Ten eyes from five infants with Stage 4A ROP were treated with a combined laser and anti-VEGF approach. Comprehensive follow-up examinations were conducted to evaluate the treatment outcomes.
Results
The study demonstrated successful retinal attachment without complications, showcasing the efficacy and safety of this non-surgical method. A comparison with surgical interventions highlighted the potential benefits in terms of reduced adverse effects.
Discussion
This combined treatment emerges as a promising first-choice option for Stage 4A ROP, offering rapid regression without surgical intervention, particularly in early stages. However, larger randomized clinical trials are necessary to validate these findings and establish definitive guidelines for managing this complex condition.
Conclusion
Combined laser and anti-VEGF therapy proved to be an effective and safe non-surgical approach for Stage 4A ROP, with the potential to reduce the need for surgery, especially in its early presentation. Further research is required to confirm these findings and provide comprehensive recommendations for clinical practice.
Similar content being viewed by others
Background
Retinopathy of prematurity (ROP) stands as the primary cause of visual impairment among infants globally [1]. This vasoproliferative disorder primarily impacts preterm and underweight newborns [2]. ROP stage 4 was defined by International Classification of Retinopathy of Prematurity (ICROP) as ROP with extrafoveal (4A) or foveal (4B) partial retinal detachment (RD) [3]. Moreover, the amount of VEGF in the vitreous body is high in ROP stage 4 [4]. Several studies reported good anatomical and visual outcomes for intravitreal anti-VEGFs in ROP stage 4 [4, 5]. The conventional treatment for high-risk pre-threshold retinopathy of prematurity (ROP) involves traditional laser therapy targeting the non-vascularized retina, eliminating cells producing Vascular Endothelial Growth Factor (VEGF) [6]. However, there is a recent shift towards adopting anti-VEGF agents [6]. Laser photocoagulation has a success rate of 80–85%, aiming to stop disease progression [7, 8]. Surgical intervention is essential for stages 4B and 5, with lens sparing vitrectomy (LSV) showing promise. Despite advancements, surgical interventions, including LSV, have complications [9]. Treating stage 4A aims to prevent progression to stage 4B or 5, requiring timely interventions for disease control and vision preservation [6]. In this study, we focus on patients who had ROP stage 4a but were managed using non-surgical methods including combined laser and intravitreal anti-VEGF.
Materials and methods
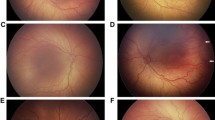
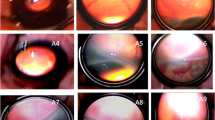
This is a retrospective case series study. All medical records of patients with ROP stage 4a were evaluated. The research protocol received approval from the institutional ethics committee and adhered to the principles of the Declaration of Helsinki. In this study, a total of 10 eyes from 5 infants with stage 4 ROP who referred to Poostchi Eye Clinic were enrolled in 2023. All patients initially presented as primary referrals without any prior therapeutic interventions. In the examination, we observed arterial tortuosity and venous dilation of the posterior vessels, as well as a ridge in the peripheral retina with associated retinal detachment. Fortunately, the macula remains attached (Fig. 1A, B, C). Subsequently, all of them underwent simultaneous laser photocoagulation and intravitreal anti-VEGF injections by vitreoretinal fellowship. All steps and procedures were comprehensively elucidated in the procedure section. Follow-up examinations were done on days 1, 3, 5, and 7 after treatment and then every week for 1 month, followed by every 2 weeks until confirmed attachment of the retina and no active ROP, thereafter every 4 weeks till 1 year. During the follow-up assessments, it was observed that the retinas of all patients remained attached (Fig. 1D, E), and there was no need for vitrectomy. Demographic and medical Data, age at treatment, stage and location of ROP and the width of partial retinal detachment as clock hour were recorded.
A, B, C Color fundus photographs before treatment with intravitreal injections and laser, showed arterial tortuosity and venous dilation of the posterior vessels, there was a ridge with retinal detachment in the peripheral retina and attached macula. D, E Color fundus photographs after treatment showed 360º degrees laser in the peripheral retina and attached retina
Procedure
After pupillary dilatation with 1% tropicamide, indirect retinal laser photocoagulation with near confluent laser spots was performed. Subsequently, preparation of the eyelids and conjunctiva was conducted using 10% povidone iodine, followed by the placement of a lid speculum. After a 3-min interval, a dosage of 0.625 mg (0.025 ml) of bevacizumab was administered into the vitreous cavity utilizing a 30-gauge needle. The needle was inserted through the supratemporal quadrant of the pars plana, positioned 1.5mm posterior to the limbus. The affected eye was treated with topical antibiotics, including gentamicin ophthalmic drops (3mg/ml) three times daily, and betamethasone ophthalmic drops (0.10%) four times daily.
Evaluation of surgical outcomes
The evaluation of anatomical results was performed. This assessment involved binocular ophthalmoscopy and the capture of fundus photographs using phoenix digital fundus camera during subsequent follow-up appointments. During follow-up, changes in retinal detachment, stage and extent of ROP, retinal vessels, plus disease and macular contour were monitored. Inadequate regression after treatment was defined as persistent ROP. Retinal vascularization arrest with new demarcation line, ridge, or RD was defined as recurrent ROP [10]. In patients with persistent ROP or recurrent ROP, retreatment with either intravitreal injection of anti-VEGFs or surgery including lens sparing core vitrectomy for removing traction may be considered. In addition, visual and refractive outcomes and ocular alignment were evaluated. Intravitreal complications including endophthalmitis, cataract, vitreous hemorrhage, and also major systemic conditions were recorded.
Results
The baseline characteristics of all patients are summarized in Table 1.
In this study, we had 5 infants, 4 of whom were female and 1 was male. Among them, one was a twin. Except for one infant who developed sepsis and received blood transfusion, the others had no specific past medical history. All patients were in stage 4a zone2 except one who was in stage 4a zone1 (Table 2).
Neonatal Demographics and Medical Parameters Dataset of all patients are shown in Table 3.
The study variables included birth weight (1399g, 1220.82), age (30.6 weeks, 0.94), NICU stay (32.6 days, 31.34), O2 usage (22 days, 20.21), and laser/injection age (39.4 weeks, 3.24. No infant experienced complications after the surgery, and all infants’ retinas were successfully attached and inactive. No reactivation or retreatment was reported. Macula of all patients was normal without any dragging or distortion after 1 year. No ocular side effects including cataract, endophthalmitis, vitreous hemorrhage was reported. One year after laser and anti-VEGF injections, patients underwent refraction. Table 4 uniformly reports their refraction and visual acuity, all recorded as CSM.
Discussion
Although vitrectomy or scleral buckling is suggested for stage 4 ROP, these treatments may have many adverse effects including endophthalmitis, iatrogenic retinal break, cataract, and delayed-onset intraocular pressure elevation after vitrectomy [11,12,13] and anisometropia, high myopia, and the need for removal of the buckle after scleral buckling [14, 15]. According to the ETROP study, vitrectomy in ROP stage 4a is not as successful as other case series [12]. Regression rate in patients with stage 4a ROP who were treated with laser alone was 55.6% and 76.9% in those who were treated with anti-VEGF intravitreal injection alone [9]. Therefore, combined laser and anti-VEGF intravitreal injection might have more effects, similar to our study. A meta-analysis study reported no statistically significant differences between anti-VEGF treatment and laser treatment in the regression rate. However, anti-VEGF treatment had a higher recurrence and retreatment rate. In addition, safety outcomes were similar between the two treatments. IVB was associated with fewer surgical interventions and better refractive outcomes [16]. Even if vitrectomy is required, anti-VEGFs could reduce intraoperative bleeding, surgery time, endodiathermy during surgery, postoperative complications and increase percentage of lens preservation, anatomical reattachment and vision recovery [17]. However, anti-VEGFs may increase the risk of proliferative membrane contraction and consequently may exacerbate retinal detachment [18,19,20]. In addition, laser photocoagulation does not take effect immediately as Paulus YM. Et al study represented that retinal scar stabilizes about 1 month after laser at about 35% of the initial lesion size and at the same moment retinal gliosis occurs in all retinal layers, therefore in the meantime retinal detachment may be aggravated [21]. However, laser and bevacizumab combination therapy is safe and contributes to more rapid regression compared with laser monotherapy [22]. This method decreases rate of retinal detachment compared with anti-VEGF monotherapy. Over all it seems to be more beneficial in stage 4a ROP, like our study, than laser or intravitreal anti-VEGF monotherapy. As mentioned in Sukgen et al.’s study [9], Cases with less than 6 clock hours in stage 4a are more responsive to non-surgical treatments, similar to our cases. Combined laser and anti-VEGF injection seems to be the best first choice treatment in ROP stage 4a. In the follow-up, if any progression was seen, treatment was immediately converted to surgical treatment. If no progression was seen, follow-up continued till complete regression of ROP.
The present study is subject to several limitations, encompassing its retrospective design, a relatively modest sample size, a truncated follow-up period, and the absence of a control group. To address and enhance these limitations, it is recommended that future investigations adopt a prospective approach, encompassing a larger cohort, implementation of a control group, and an extended follow-up duration.
Conclusion
This study demonstrates the efficacy of combined treatment in effectively controlling enrolled cases, resulting in stable conditions after 1 year of close follow-up. These findings suggest that the combined treatment method is effective for stage 4A ROP cases. However, it should be noted that this study had a limited sample size and a relatively short follow-up period. Therefore, further analysis is warranted to increase the number of cases, extend the duration of follow-up, or even include similar cases from different institutions to enhance the reliability of the study conclusions.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Darlow BA, Gilbert C. Retinopathy of prematurity – a world update. Semin Perinatol. 2019;43(6):315–6.
Hellström A, Smith LE, Dammann O. Retinopathy of prematurity. Lancet. 2013;382(9902):1445–57. PubMed PMID: 23782686. Pubmed Central PMCID: PMC4389630. Epub 20130617. eng.
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Chan RP, Berrocal A, et al. International classification of retinopathy of prematurity. Ophthalmology. 2021;128(10):e51–68.
Hartnett ME. Retinopathy of prematurity: evolving treatment with Anti-Vascular endothelial growth factor. Am J Ophthalmol. 2020;218:208–13.
Taher NO, Ghaddaf AA, Al-Ghamdi SA, Homsi JJ, Al-Harbi BJ, Alomari LK, et al. Intravitreal anti-vascular endothelial growth factor injection for retinopathy of prematurity: a systematic review and meta-analysis. Front Med. 2022;9:884608.
Narnaware SH, Bawankule PK. Role of LASERS in stage 4A retinopathy of prematurity (ROP). Lasers Med Sci. 2021;36(5):989–93.
Mueller B, Salchow DJ, Waffenschmidt E, Joussen AM, Schmalisch G, Czernik C, et al. Treatment of type I ROP with intravitreal bevacizumab or laser photocoagulation according to retinal zone. Br J Ophthalmol. 2017;101(3):365–70. PubMed PMID: 27301450. Epub 20160614. eng.
Hwang CK, Hubbard GB, Hutchinson AK, Lambert SR. Outcomes after intravitreal bevacizumab versus laser photocoagulation for retinopathy of prematurity: a 5-year retrospective analysis. Ophthalmology. 2015;122(5):1008–15. PubMed PMID: 25687024. Pubmed Central PMCID: PMC4414677. Epub 20150214. eng.
Sukgen EA, Koçluk Y. Treatment for stage 4A retinopathy of prematurity: laser and/or ranibizumab. Graefes Arch Clin Exp Ophthalmol. 2017;255(2):263–9. PubMed PMID: 27495302. Epub 20160806. eng.
Hu J, Blair MP, Shapiro MJ, Lichtenstein SJ, Galasso JM, Kapur R. Reactivation of retinopathy of prematurity after bevacizumab injection. Arch Ophthalmol. 2012;130(8):1000–6. PubMed PMID: 22491394. eng.
Kychenthal A, Dorta P. 25-gauge lens-sparing vitrectomy for stage 4A retinopathy of prematurity. Retina. 2008;28(3):S65–8.
Iwahashi-Shima C, Miki A, Hamasaki T, Otori Y, Matsushita K, Kiuchi Y, et al. Intraocular pressure elevation is a delayed-onset complication after successful vitrectomy for stages 4 and 5 retinopathy of prematurity. Retina. 2012;32(8):1636–42.
El Rayes EN, Vinekar A, Capone A Jr. Three-year anatomic and visual outcomes after vitrectomy for stage 4B retinopathy of prematurity. Retina. 2008;28(4):568–72.
Hinz BJ, de Juan JE, Repka MX. Scleral buckling surgery for active stage 4A retinopathy of prematurity. Ophthalmology. 1998;105(10):1827–30.
Chow DR, Ferrone PJ, Trese MT. Refractive changes associated with scleral buckling and division in retinopathy of prematurity. Arch Ophthalmol. 1998;116(11):1446–8.
Houston SK, Wykoff CC, Berrocal AM, Hess DJ, Murray TG. Laser treatment for retinopathy of prematurity. Lasers Med Sci. 2013;28:683–92.
Xu Y, Zhang Q, Kang X, Zhu Y, Li J, Chen Y, et al. Early vitreoretinal surgery on vascularly active stage 4 retinopathy of prematurity through the preoperative intravitreal bevacizumab injection. Acta Ophthalmol. 2013;91(4):e304-10. PubMed PMID: 23647944. Epub 20130507. eng.
Honda S, Hirabayashi H, Tsukahara Y, Negi A. Acute contraction of the proliferative membrane after an intravitreal injection of bevacizumab for advanced retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 2008;246(7):1061–3. PubMed PMID: 18320201. Epub 20080305. eng.
Zepeda-Romero LC, Liera-Garcia JA, Gutiérrez-Padilla JA, Valtierra-Santiago CI, Avila-Gómez CD. Paradoxical vascular-fibrotic reaction after intravitreal bevacizumab for retinopathy of prematurity. Eye (Lond). 2010;24(5):931–3. PubMed PMID: 19557020. Epub 20090626. eng.
Arevalo JF, Maia M, Flynn HW Jr, Saravia M, Avery RL, Wu L, et al. Tractional retinal detachment following intravitreal bevacizumab (Avastin) in patients with severe proliferative diabetic retinopathy. Br J Ophthalmol. 2008;92(2):213–6. PubMed PMID: 17965108. Epub 20071026. eng.
Paulus YM, Jain A, Gariano RF, Stanzel BV, Marmor M, Blumenkranz MS, et al. Healing of retinal photocoagulation lesions. Invest Ophthalmol Vis Sci. 2008;49(12):5540–5. PubMed PMID: 18757510. Epub 20080829. eng.
Namvar E, Bolkheir A, Emadi Z, Johari M, Nowroozzadeh MH. Outcomes of near confluent laser versus combined less dense laser and bevacizumab treatment of prethreshold ROP Type 1 Zone 2: a randomized controlled trial. BMC Ophthalmol. 2022;22(1):1–6.
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
EN and AA responsible for the writing, data gathering, data analysis, interpretation, and critical review of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional review board of the Shiraz University of Medical Sciences approved the study and the tenets of the declaration of Helsinki and its later amendments were followed. All participants signed the informed consent form. This study has been approved by the ethics committee at Shiraz university of Medical Sciences (IR.SUMS.MED.REC.1402.326).
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Namvar, E., Attar, A. Non-surgical treatment of stage 4A retinopathy of prematurity. BMC Ophthalmol 24, 180 (2024). https://doi.org/10.1186/s12886-024-03434-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03434-5