Abstract
Purpose
To evaluate the association of body stature with ocular biometrics and refraction in preschool children.
Methods
A cross-sectional, school-based study was conducted in Shenzhen, China. Preschool children aged 3 to 6 from 10 randomly-selected kindergartens were recruited. Ocular biometric parameters, including axial length (AL), anterior chamber depth (ACD), vitreous chamber depth (VCD), corneal radius curvature (CR), axial length to corneal radius ratio (AL-to-CR ratio) and lens thickness (LT) were measured using non-contact partial-coherence laser interferometry. Cycloplegic refractions were obtained by a desktop autorefractor. Body height and weight were measured using standard procedures. The association between body stature and ocular biometrics were analyzed with univariable and multivariable regression model.
Results
A total of 373 preschoolers were included. AL, ACD, VCD, CR, and AL-to-CR ratio, were positively associated with height and weight (p < 0.05), whereas LT was negatively associated with height and weight (p < 0.01). No association was observed between stature and central cornea thickness and refraction. After adjusted for age and gender in a multivariable regression model, AL had positive associations with height (p < 0.01) and weight (p < 0.01). However, refraction had no significant association with stature parameters.
Conclusion
Taller and heavier preschoolers had eyes with longer AL, deeper vitreous chamber, and flatter cornea. The significant associations between body stature and ocular biometric parameters reveal the driving influence of body development on the growth of eyeballs in preschoolers.
Similar content being viewed by others
Introduction
Myopia is a highly prevalent ocular disorder globally, especially in Asia [1]. Uncorrected visual acuity loss caused by myopia is the most common reason for visual impairment worldwide [2]. As the prevalence is yet increasing, it’s posing a major public health challenge.
Myopia occurs when there is a mismatch between the focal plane of the eye and the prolonged axial length (AL). During the postnatal eye growth, proportional changes in the ocular biometric parameters such as AL, anterior chamber depth (ACD), lens thickness (LT), corneal curvature (CR), and vitreous chamber depth (VCD) bring the eye to emmetropization and the disturbance of this highly coordinated process will lead to refractive errors [3]. Thus, a thorough understanding of the optical and structural development of the eye during emmetropization and its related factors helps to reveal the potential mechanism of myopia incidence.
It’s believed that a shared mechanism exists for ocular development and body stature since the eye grows at a time when body stature is also increasing. Previous studies have indicated that AL is associated with height, weight, and body mass index (BMI) and that longitudinal changes in AL and height are concomitant in children [4]. Twin study provided evidence that 89% of the phenotypic correlation of AL and height was due to shared genetic factors [5]. However, inconsistent results were observed [6,7,8,9,10,11]. For instance, the Anyang University Students Eye Study found a negative association between height and refraction [6], whereas Tien-Yin Wong et al. demonstrated no association between height and refraction [7]. Most previous studies have primarily included children older than seven years or adults, among which period myopia progression is susceptible to education and other confounding factors. A few studies have described the relationship between body stature and refraction, AL or CR in preschool children [12,13,14], but its relationship with other ocular biometrics was rarely discussed.
In this study, we aim to describe the distribution of refraction and comprehensive ocular biometrics including AL, central corneal thickness (CCT), ACD, LT, VCD, CR and AL-to-CR ratio, as well as to investigate their relationship with body stature (height, weight, BMI) in a preschool population from Shenzhen city, southern China.
Methods
Study population
This study is a school-based, cross-sectional study conducted in a group of preschoolers in Futian District, Shenzhen, Guangdong Province in southern China.
Participants were recruited from 10 randomly selected kindergartens with facilities and teaching staff of the same level. The study followed the tenets of the Declaration of Helsinki. Ethics approval was obtained from the Institutional Review Board of Shenzhen Maternity and Child Healthcare Hospital (SFYLS [2020] 042). The purpose and examination procedures of the study were explained to the parents or legal guardians at the ophthalmic clinic of Shenzhen Maternity and Child Healthcare Hospital, after which written informed consent was obtained.
Inclusion and exclusion criteria
Four hundred and nineteen preschoolers aged 3 to 6 years were enumerated and have given informed consent for participation. Children were excluded as they had congenital diseases, developmental disabilities, systemic diseases, eye diseases, and other diseases that would affect the development of stature or ocular biometry. Those failed to finish all the examinations were also excluded. As a result, three hundred and seventy-three preschoolers were included into final analysis.
Examinations
Ocular examinations were conducted at the ophthalmic clinic of Shenzhen Maternity and Child Healthcare Hospital from September to October, 2020. Ocular biometrics, including AL, ACD and LT were measured before pupil dilation with a non-contact partial-coherence laser interferometry (IOL Master; Carl Zeiss Meditec, Oberkochen, Germany). After intraocular pressure measurement with a non-contact tonometer (CT-1, Topcon, Japan), 1% cyclopentolate drops were administered to participants with normal intraocular pressure to induce cycloplegia. After the pupils were fully dilated, refraction examinations were taken using a desktop autorefractor (KR8800; Topcon Corp., Tokyo, Japan). Height and weight were measured without shoes in a standardized manner.
Definitions
Spherical equivalent refraction (SER) was calculated as spherical diopters (D) plus one-half cylindrical diopters using data extracted from the autorefractor. Corneal radius (CR) was calculated as the mean of the greatest CR and the lowest one. Vitreous chamber depth (VCD) was calculated as the AL minus ACD and LT. The AL-to-CR ratio was computed as AL in millimeters divided by CR in millimeters. BMI was computed using the formula BMI = weight(kg)/height(m)2.
Statistics
The distribution of ocular biometrics, including AL, ACD, LT, VCD, CR, AL-to-CR ratio, refraction presented as SER, and stature parameters, including height, weight, and BMI, were presented and compared by gender using t-tests. As the ocular biometrics and refraction of both eyes are highly correlated (Pearson’s correlation coefficient for AL, 0.98; CCT, 0.98; ACD, 0.98; LT, 0.99; VCD, 0.97; CR, 0.97; AL-to-CR ratio, 0.96, and SER, 0.89), only the data of the right eyes were presented and analyzed. Mean, standard deviation and the range of body stature, ocular biometrics, and refraction were presented. Trend analysis of ocular biometrics and refraction was performed by height, weight, and BMI quartiles to detect a significant difference. Univariable analyses were performed to determine the associations of height, weight, and BMI with different ocular biometric components and refraction. Multivariable regression analyses adjusted by age and gender were performed to assess the effects of height, weight, and BMI on ocular biometrics and refraction. In the regression model, individual refraction or ocular biometric components were analyzed as the dependent variables, and height, weight, or BMI were the independent variables. A two-sided P value of 0.05 or less was considered statistically significant. All analyses were performed using the Stata Statistical Software (version 16.0; Stata Corp, College Station, TX). All confidence intervals (CIs) are 95%.
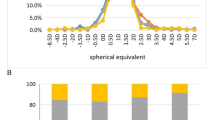
Results
A total of 373 children were enrolled in the analysis, with a mean age of 4.91 ± 0.79 years without statistically significant gender difference (t = 1.62, p = 0.11). In general, girls were shorter (109.26 ± 7.11 cm vs. 111.71 ± 6.74 cm, t = 3.41, p < 0.01) and lighter (18.32 ± 3.16 kg vs. 19.32 ± 2.81 kg, t = 3.23, p < 0.01) than boys (Table 1). The average SER of the population was 1.33 ± 0.79D, and greater hyperopia was observed in girls (1.48 ± 0.84, t=-3.71, p < 0.01) with shorter AL (21.97 mm vs. 22.57 mm, t = 9.35, p < 0.01), smaller CCT (0.54 mm vs. 0.55 mm, t = 3.54, p < 0.01) and CR (7.71 mm vs., 7.83 mm, t = 5.15, p < 0.01), shallower ACD (3.43 mm vs. 3.56 mm, t = 6.29, p < 0.01), smaller VCD (14.44 mm vs. 14.94 mm, t = 8.01, p < 0.01) and thicker LT (3.56 mm vs. 3.52 mm, t=-2.95, p < 0.01).
The correlations of height, weight, and BMI, with ocular biometric parameters and SER, are shown in Table 2. Only height was correlated with SER (r=-0.12, p < 0.05). Both height and weight were positively and significantly correlated with AL (r = 0.36 and 0.34), ACD (r = 0.18 and 0.19), VCD (r = 0.39 and 0.34), CR (r = 0.12 and 0.17), and AL-to-CR ratio (r = 0.31 and 0.21) but negatively correlated with LT (r=-0.32 and − 0.23, specifically). BMI had no correlation with refraction and biometrics except for CR (r = 0.12, p < 0.05). There was no significant correlation between body stature and CCT (all r < 0.1 and p > 0.05 ).
The mean values of refraction and ocular biometrics of the children, categorized by quartiles of height, weight, and BMI, are shown in Table 3. Height and weight quartiles were significantly associated with ocular biometrics except for CCT. Generally, higher and heavier children tended to have longer eyes, deeper ACD, thinner lenses, deeper VCD, flatter cornea and larger AL-to-CR ratio (all p < 0.05). By contrast, refraction didn’t change significantly with increasing height and weight. Children with higher BMI values tended to have flatter cornea, while other ocular biometrics changed insignificantly when BMI increased. Unlike other biometrics, no significant tendency was observed in SER and CCT across quartiles of height, weight and BMI.
Table 4 shows the coefficients in linear regression models where the individual refraction or ocular biometric components as the dependent variables and height, weight, or BMI as the independent variables. In the univariable regression model, an increase in height and weight significantly affected ocular biometric growth, except for CCT. After adjusting for age and gender, both height and weight were significantly and positively associated with AL. The adjusted R2 of the model was approximately 0.28, indicating that 28% of the variance in AL could be attributed to difference in height or weight. Height and weight were also significantly correlated with VCD, with adjusted R2 values of 0.26. Although the correlation between height and weight with CR were significant, but only 7–8% of the variance of CR could be explained by the variance of height or weight, BMI showed marginal positive associations with CR, with an adjusted R2 of 0.07.
Discussion
This study provides evidence on the association between body stature with ocular biometrics in preschoolers in southern China. We found taller and heavier preschool children had eyes with longer AL, deeper vitreous chamber, and flatter cornea. However, no association between body stature and refraction was observed when adjusted for age and gender.
As most of the juvenile myopia is axial myopia, AL elongation is considered the most crucial determinant of myopia incidence [15]. Previous studies have found that AL and height were associated and concomitant both in children and adults. After adjusting for age and gender, an increase of 10 cm in body height was associated with an elongation in AL for about 0.28 mm in Chinese adults in Singapore [7], 0.33 mm in young adults in northern China [6], and 0.27 mm in Australian children [11]. In our study, every increase of 10 cm in height results in 0.20 mm difference of AL elongation (the β between AL and height was 0.02 in the adjusted linear model), which was less than previous reports. The discrepancies in results among studies may be mainly attributed to the enrolled population. On one hand, axial length elongation may be mainly driven by physical growth in preschoolers, but more affected by environmental factors such as education and near work activities after entering schools [16]. The GUSTO birth cohort study has found no evidence of environmental factors influencing early-onset myopia. Taller children at birth and at 12, 24, and 36 months were found to have longer AL in 3 years old [17]. Another birth cohort study also reveals that taller and heavier neonates had longer AL at 6 years of age and growth during pregnancy and 2 years postnatally is the most important period underlying this association [18]. Thus, the relation between height and AL might be age-specific.
Associations between refraction and height were inconsistent in different studies [6, 7, 9,10,11, 19, 20]. Negative associations between refraction and stature i.e., taller and heavier persons with less hyperopic eyes, were observed in different ethnicities and regions [11, 19]. However, some studies found no association between height and refraction in preschoolers [17, 21, 22],which is consistent with our study. It can be easily understood that taller and heavier children have longer AL but flatter cornea, thus resulting in a slight difference in refraction in this study. Similar phenomenon has been observed that AL grows significantly with minimal changes in refraction in preschool children [23], suggesting body stature has limited potential in predicting refraction in preschoolers.
Similar to the previous studies [13, 18], taller and heavier children had deeper vitreous chambers and flatter corneas in our study. One possible explanation is that, not only AL elongation but also other ocular biometrics growth were concurrent with and driven by physical development in preschool children. Besides the genetic correlation between stature and AL [5], common determinant genes controlling body size and other ocular component dimensions such as cornea and lens were found in chickens [24]. The genetic height and birth weight risk scores were both significantly associated with ocular biometry in children [18]. Another possible reason is that the change of VCD and cornea are secondary to AL elongation. The secondary changes result from the physical stretching of eyeball as well as biological regulation to match optical power with the focal plane. Longitudinal and experimental evidence are needed to confirm these hypotheses.
AL-to-CR ratio was found to have a stronger association with refraction than AL in previous studies [25,26,27]. However, earlier reports of the association between body stature and AL-to-CR ratio were controversial in adults or school children [6]. A cross-sectional study conducted in 3-year-old preschoolers in China found no association between body stature and AL-to-CR ratio after adjusting for gender [28]. Similarly, we didn’t find a significant association between AL-to-CR ratio and height or weight in preschool children neither. On one hand, the AL-to-CR ratio in preschooler is relatively stable given the concurrent increase of AL and CR during emmetropization. Different ages, refractive error situations, and the lack of control for confounding variables may also result in conflicting results.
Reports on the relationship of BMI with ocular biometrics and refraction did not agree with each other. The Anyang University Students Eye Study found that BMI was significantly related to CR and ACD. Wu et al. found a strong association between BMI, AL, and CR after adjusting for age and gender [9]. But Wong et al. found that BMI was not related to those ocular biometric parameters [7]. We found no association between BMI and ocular biometrics and refraction in this study, indicating obesity may not influence the eye growth and refraction development. Supportive evidence has been found in the data from a total of 6855 ethnically-diverse Americans that body metrics nor nutritional factors (serum Vitamin D, glucose levels and caffeine intake) were associated with refractive error or myopia status [29].
The current study enrolled preschool children who were free from education pressure and mostly emmetropia, which enables us to investigate the direct relationship between body stature and ocular biometrics during emmetropization. Body statures have significant relationships with AL, VCD and CR, but not with refraction, revealing that taller and heavier preschool children have higher risk of myopia when compared to their emmetropia counterparts. Potential limitations of this study should be mentioned. Firstly, we did not include risk factors such as lifestyle, diet habits, environmental factors, and parental characteristics that would affect ocular biometrics development. Therefore, the impact of height and weight on ocular biometrics consists not only genetic effects but also underlying familial environmental influence. Secondly, the enrollment of preschoolers who were mostly emmetropia and less affected by education pressure enables us to investigate the impact of body stature on emmetropization process, but the small proportion of already myopic children may bias the results. Thirdly, this study is a cross-sectional study. The relationship between longitudinal change of body stature and ocular biometrics needs further investigations.
Conclusion
In conclusion, stature parameters were associated with ocular biometrics in preschoolers but not with refraction. Height and weight both have a positive impact on the growth of axial length and vitreous chamber, whereas BMI does not. Height, weight and BMI do not influence CCT, ACD, LT and AL-to-CR ratio. However, they do have a significant but limited influence on CR. The growth of eyeball in preschoolers may be driven by physical development, whereas longitudinal shreds of evidence are still needed.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42.
Naidoo KS, Leasher J, Bourne RR, Flaxman SR, Jonas JB, Keeffe J, Limburg H, Pesudovs K, Price H, White RA. Global vision impairment and blindness due to uncorrected refractive error, 1990–2010. Optom Vis Sci. 2016;93:227–34.
Siegwart JT Jr, Norton TT. Perspective: how might emmetropization and genetic factors produce myopia in normal eyes? Optometry Vis Science: Official Publication Am Acad Optometry. 2011;88:E365.
Wang D, Ding X, Liu B, Zhang J, He M. Longitudinal changes of axial length and height are associated and concomitant in children. Investig Ophthalmol Vis Sci. 2011;52:7949–53.
Zhang J, Hur YM, Huang W, Ding X, Feng K, He M. Shared genetic determinants of axial length and height in children: the Guangzhou twin eye study. Arch Ophthalmol. 2011;129:63–8.
Wei S, Sun Y, Li S-M, Hu J-P, Cao K, An W, Guo J-Y, Li H, Wang N. Effect of body stature on refraction and ocular biometry in Chinese young adults: the Anyang University Students Eye Study. Clin Experimental Optometry. 2021;104:201–6.
Wong TY, Foster PJ, Johnson GJ, Klein BEK, Seah SKL. The relationship between ocular dimensions and refraction with adult stature: the Tanjong Pagar survey. Investig Ophthalmol Vis Sci. 2001;42:1237–42.
Gessesse GW, Debela AS, Anbesse DH. Ocular biometry and their correlations with ocular and anthropometric measurements among Ethiopian adults. Clin Ophthalmol. 2020;14:3363–9.
Wu HM, Gupta A, Newland HS, Selva D, Aung T, Casson RJ. Association between stature, ocular biometry and refraction in an adult population in rural Myanmar: the Meiktila eye study. Clin Exp Ophthalmol. 2007;35:834–9.
Lee KE, Klein BE, Klein R, Quandt Z, Wong TY. Association of age, stature, and education with ocular dimensions in an older white population. Arch Ophthalmol. 2009;127:88–93.
Ojaimi E, Morgan IG, Robaei D, Rose KA, Smith W, Rochtchina E, Mitchell P. Effect of stature and other anthropometric parameters on eye size and refraction in a population-based study of Australian children. Investig Ophthalmol Vis Sci. 2005;46:4424–9.
Low W, Dirani M, Gazzard G, Chan YH, Zhou HJ, Selvaraj P, Au Eong KG, Young TL, Mitchell P, Wong TY, Saw SM. Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br J Ophthalmol. 2010;94:1012–6.
Northstone K, Guggenheim JA, Howe LD, Tilling K, Paternoster L, Kemp JP, McMahon G, Williams C. Body stature growth trajectories during childhood and the development of myopia. Ophthalmology. 2013;120:1064–73e1.
Li T, Zhou X, Chen X, Qi H, Gao Q. Refractive error in Chinese Preschool children: the Shanghai Study. Eye Contact Lens. 2019;45:182–7.
Meng W, Butterworth J, Malecaze F, Calvas P. Axial length of myopia: a review of current research. Ophthalmologica. 2011;225:127–34.
Morgan IG, Wu PC, Ostrin LA, Tideman JWL, Yam JC, Lan W, Baraas RC, He X, Sankaridurg P, Saw SM, French AN, Rose KA, Guggenheim JA. IMI Risk factors for myopia. Invest Ophthalmol Vis Sci. 2021;62:3.
Chua SY, Ikram MK, Tan CS, Lee YS, Ni Y, Shirong C, Gluckman PD, Chong YS, Yap F, Wong TY, Ngo CS, Saw SM. Growing up in Singapore towards Healthy outcomes Study G. relative contribution of risk factors for early-onset myopia in young Asian children. Invest Ophthalmol Vis Sci. 2015;56:8101–7.
Tideman JWL, Polling JR, Jaddoe VWV, Vingerling JR, Klaver CCW. Growth in foetal life, infancy, and early childhood and the association with ocular biometry. Ophthalmic Physiol Opt. 2019;39:245–52.
Xie XW, Xu L, Wang YX, Jonas JB. Body height and ocular diseases. The Beijing Eye Study. Graefes Arch Clin Exp Ophthalmol. 2009;247:1651–7.
Eysteinsson T, Jonasson F, Arnarsson A, Sasaki H, Sasaki K. Relationships between ocular dimensions and adult stature among participants in the Reykjavik Eye Study. Acta Ophthalmol Scand. 2005;83:734–8.
Lim LS, Chua S, Tan PT, Cai S, Chong YS, Kwek K, Gluckman PD, Fortier MV, Ngo C, Qiu A, Saw SM. Eye size and shape in newborn children and their relation to axial length and refraction at 3 years. Ophthalmic Physiol Opt. 2015;35:414–23.
Liu L, Li R, Huang D, Lin X, Zhu H, Wang Y, Zhao X, Zhang X, Liu H. Prediction of premyopia and myopia in Chinese preschool children: a longitudinal cohort. BMC Ophthalmol. 2021;21:283.
Guo X, Fu M, Ding X, Morgan IG, Zeng Y, He M. Significant Axial elongation with minimal change in refraction in 3- to 6-Year-old Chinese preschoolers: the Shenzhen Kindergarten Eye Study. Ophthalmology. 2017;124:1826–38.
Prashar A, Hocking PM, Erichsen JT, Fan Q, Saw SM, Guggenheim JA. Common determinants of body size and eye size in chickens from an advanced intercross line. Exp Eye Res. 2009;89:42–8.
Ojaimi E, Rose KA, Morgan IG, Smith W, Martin FJ, Kifley A, Robaei D, Mitchell P. Distribution of ocular biometric parameters and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci. 2005;46:2748–54.
Iyamu E, Iyamu J, Obiakor CI. The role of axial length-corneal radius of curvature ratio in refractive state categorization in a nigerian population. ISRN Ophthalmol 2011; 2011: 138941.
He X, Zou H, Lu L, Zhao R, Zhao H, Li Q, Zhu J. Axial length/corneal radius ratio: association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS ONE. 2015;10:e0111766.
Huang D, Chen X, Gong Q, Yuan C, Ding H, Bai J, Zhu H, Fu Z, Yu R, Liu H. Ocular biometric parameters among 3-year-old Chinese children: testability, distribution and association with anthropometric parameters. Sci Rep. 2016;6:29577.
Harb EN, Wildsoet CF. Nutritional factors and myopia: An Analysis of National Health and Nutrition Examination Survey Data. Optom Vis Sci. 2021;98:458–68.
Acknowledgements
Not applicable.
Funding
This research was supported by the National Natural Science Foundation of China (Grant Number: 81271037); No additional external funding was received. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Min Fu and Decai Wang conceived and planned the research study. Linling Li wrote the manuscript, carried out data collection in the research area. Chimei Liao helped by supervising the project, review of the manuscript, and worked on approval of the version for publication. Xiaojuan Zhang, Juan Lu and Yangfa Zeng analyzed, interpreted and produced the preliminary report. All the authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval and permission to conduct the study were obtained from the Institutional Review Board of Shenzhen Maternity and Child Healthcare Hospital (SFYLS [2020] 042) and were carried out in accordance with the tenets of the Declaration of Helsinki. Parents, guardians, or both were informed of the purpose of the study and had to give their informed consent before the child was enrolled.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, L., Liao, C., Zhang, X. et al. Association between body stature with ocular biometrics and refraction among Chinese preschoolers. BMC Ophthalmol 24, 107 (2024). https://doi.org/10.1186/s12886-024-03372-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03372-2