Abstract
Background
To report a case of retinitis with multiple intraocular viral infections after second haematopoietic stem cell transplantation.
Case presentation
A 39-year-old female patient developed retinitis after a second haematopoietic stem cell transplant. Right eye was tested for three viral infections– cytomegalovirus, Epstein‒Barr virus and herpes simplex virus, while left was infected with cytomegalovirus. The patient was subsequently treated with vitreous cavity ganciclovir injections, and 1 week later both eyes tested negative for aqueous humour viruses.
Discussion and conclusion
CMV, EBV and HSV belong to the herpes virus family. They are all commonly observed in the body and represent opportunity infectious viruses. The retinitis they cause have different characteristics. But simultaneous infection of the eye by multiple viruses is quite rare. In this case, three viruses were detected in the patient’s eye, but whether the retina was caused by all three viruses at the same time could not be determined. A satisfactory outcome was achieved after treatment with vitreous cavity ganciclovir injection.
Similar content being viewed by others
Background
Acute lymphocytic leukaemia is a blood malignancy caused by malignant proliferation of lymphocytes in the blood and bone marrow [1]. The manifestations of acute lymphoblastic leukaemia is vary. Chemotherapy and haematopoietic stem cell transplantation(HSCT) are the common and very effective treatments [2]. Despite the effectiveness of haematopoietic stem cell transplantation in the treatment of acute lymphoblastic leukaemia, it continues to present many challenges. The origin of these problems is the immunosuppression that occurs during transplantation [3].
Opportunistic infections with intraocular viruses are often secondary conditions in immunosuppressed patients-such as individuals with acquired immunodeficiency syndrome(AIDS) and posthaematopoietic stem cell transplantation patients [4]. Cytomegalovirus(CMV) retinitis is the most common complication in these patients [5, 6]. CMV is a double-stranded DNA virus that is a member of the herpesvirus family [7]. Herpes viruses are usually divided into eight species. In addition to CMV, herpes simplex virus(HSV), varicella-zoster virus(VZV), and Epstein‒Barr virus(EBV) are also herpes viruses [6]. Retinitis caused by viruses other than CMV is uncommon in immunosuppressed patients, and mixed infections with multiple viruses are even rarer.
Within our limited knowledge, we have not seen reports of retinitis patients after haematopoietic stem cell transplantation who were coinfected by kinds of herpes viruses. In this case report, we describe a haematopoietic stem cell transplantation recipient who presented with retinitis caused by cytomegalovirus, Epstein‒Barr virus and herpes simplex virus.
Case presentation
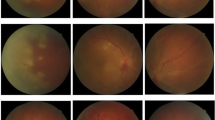
In April 2023, a 39-year-old Chinese woman presented to our hospital complaining of a black shadow in front of her right eye for 5 days. This patient had been diagnosed with acute lymphoblastic leukaemia in 2017 and received an autologous HSCT in 2018. Unfortunately, she suffered a relapse of leukaemia and underwent an allogeneic HSCT in October 2022. The patient developed ocular symptoms at 6 months after receiving the transplant. After the consultation, the patient received a series of tests including visual acuity, slit lamp, noncontact tonometer, ocular ultrasound, macular optical coherence tomography, and Optos fundus photography. The patient’s best corrected visual acuity was 20/20 in both eyes using the Snellen visual acuity chart. The intraocular pressure was within the normal range. Slit lamp examination revealed that the anterior segmental structures of both eyes were normal. Ultrasound of the eye suggested flocculent vitreous clouding in the lower part of the right eye (Fig. 1). Partial signal enhancement in the retina of the left eye was found, and part of the photoreceptor cell layer was missing on optical coherence tomography(OCT) (Fig. 1). Fundus photography revealed a yellowish-white exudate with haemorrhage in the peripheral retina of the right eye and a faint haemorrhage in the lower retina of the left eye (Fig. 2). Combining the medical history and relevant ophthalmic examination, we highly suspected that the patient had developed cytomegalovirus retinitis.
(A) Ultrasound of the eye indicates significant clouding of the vitreous humour below the right eye (The white arrow). (B) There is no significant abnormality in the ultrasound of the left eye. (C) OCT suggested enhanced signal in part of the retina of the right eye, with partial absence of the photoreceptor cell layer
(A) A yellowish-white exudate with hemorrhage was seen in the peripheral part of the retina in the direction of 9 o’clock (White rectangle). (B) Inferior vitreous opacity was evident, and the lower portion of the retina could not be seen (White rectangle). (C) Multiple small degenerations were observed in the retina of the left eye (White rectangle)
Therefore, we performed anterior atrial puncture and extracted aqueous humour from the patient for viral testing on 23, April. We further refined FFA + ICGA on April 25. Surprisingly, utilizing broad-spectrum high-throughput sequencing, it was found that the aqueous humour of her right eye tested positive for three viral DNAs-CMV, EBV, and HSV (Fig. 3). Internal markings and no template control were added to rule out a false detection of both herpes viruses during the high-throughput sequencing. The left eye was positive for CMV only. The FFA + ICGA findings indicated a small amount of retinal exudate in the patient’s right eye, and a large area of obscured fluorescence in the subnasal and inferior choroid (Fig. 4). The patient was then treated with bilateral vitreous cavity ganciclovir injections. Viral DNA was retested one week later and no virus was detected in the aqueous humour of either eye by quantitative polymerase chain reaction(QPCR). The test was negative for viral DNA. OCT and fundus photography indicated no significant changes in the fundus. The patients underwent weekly serum cytomegalovirus and EBV testing after the second stem cell transplant. She was cytomegalovirus positive only between November 15, 2022 and January 14, 2023, with viral copy numbers ranging from 1.02 × 102 to 2.37 × 104 during this period. Each test was negative for EBV. The patient was treated with systemic antiviral therapy in the hematology department since February, 2023. As of May 22, 2023, her fundal lesions all remained stable.
(A) A small amount of fluorescence leakage is seen in the retinal FFA of the right eye. (B) ICGA shows extensive fluorescence obscuration in the subnasal and inferior choroid of the right eye. (C) No significant abnormalities were seen in the FFA of the left eye. (D) Multiple small patches of obscured fluorescence were seen in the ICGA of the left eye
Discussion and conclusion
Cytomegalovirus infections are common in posttransplant patients, especially in the graft-versus-host disease (GVHD) and immunosuppressed patients. Even serum positivity for CMV is as high as 92.2% [8]. In half of the patients, prior to the onset of ocular symptoms, patients develop other systemic CMV infection signs, most commonly including gastrointestinal disorders and interstitial pneumonitis. It has been otherwise reported in the literature that CMV retinitis is usually diagnosed within 106–365 days after transplantation, with a median of 251 days [9]. This timeframe appears to be the window of high incidence of CMV retinitis. The patient in this case was diagnosed approximately six months after transplantation. However, a thorough examination of the patient’s internal medicine findings did not reveal the presence of chronic GVHD in the individual, and in contrast to typical CMV retinitis, three distinct viruses were detected in her ocular region.
CMV, HSV and EBV infections are opportunistic infections [10]. They are fairly common in the body, and EBV is lifelong in 90% of people [11]. Moreover, these viruses have been implicated in the aetiology of ARN [12]. The evidence of CMV and EBV causing ARN is not robust enough [13]. Retinitis caused by various viruses in the herpesvirus family has its own characteristics; patients with retinitis caused by HSV are usually immunocompetent, while CMV is more common in immunodeficient individuals [14]. The most critical feature of ARN is necrotizing retinitis involving the peripheral retina [13]. In combination with a positive PCR for HSV or VZV in the aqueous humour or vitreous specimen and a characteristic clinical picture including– (a) ring or fusion retinitis, and (b) retinal vascular sheaths and/or occlusions, and (c) vitritis of more than mild severity, the diagnosis of ARN is confirmed [13]. PCR is the best way to detect HSV. ARN progresses quickly, and treatment typically does not need to be postponed until the return of PCR results. Indeed, the earlier the treatment, the better the prognosis for vision [15, 16]. EBV retinitis is very rare. EBV retinitis tends to result in the chronic uveitis which is characterized by vitreous strands and snowball-shaped lower portions, optic disc oedema, massive retinitis and retinal haemorrhages, and diffuse macular oedema [17]. And EBV tends to cause severe retinitis, which is difficult to treat with various treatments [17, 18]. While CMV retinitis is quite common in immunodeficient patients. The extent of retinal damage in our patient was mild and no evidence of ARN was detected. Despite the three viruses identified in the patient’s aqueous humour, we still considered CMV to be the cause of the retinitis. Although these three viruses are often detected in inflammatory ophthalmologic lesions [19], coinfection with multiple herpes viruses is rare due to their different infection characteristics of these viruses.
The patient’s aqueous humour was positive for CMV, HSV and EBV DNA, but her blood was negative for CMV and EBV at the time of ocular symptoms. The patient’s blood has never been positive for EBV since her initiation of EBV testing. Although EBV virus is not detected in the blood, the virus is likely to be latent in the body. It has been reported in the literature that EBV virus can be detected in about 20% of cadaveric eye tissues [20]. This may have contributed to the phenomenon. The literature has previously reported a number of patients with dual viral infections [21,22,23]. Such cases are extremely rare. We believe that the eye is a relatively independent organ due to the presence of multiple barriers, resulting in viruses in the blood being relatively independent of viruses in the eye. Therefore, the situation of the viruses in the blood does not reflect the situation of the intraocular viruses, which is likely the reason for the different results of aqueous humour and blood virus tests. We have never been clear as to why three viruses were detected in the patient’s aqueous humour. Indeed, we have not seen any similar reports in the past. Thus, we hypothesize that these three viruses coincidentally entered the eye successively within a short period of time while the patient was in an immunocompromised state, and at the same time the viruses escaped the surveillance of immune cells in the eye but could not enter the bloodstream due to the presence of multiple blood-eye barriers in the eye. Eventually, the three viruses simultaneously infected in the eye. Of course, although three viruses were detected in the patient’s eye, this does not mean that all three viruses caused retinitis. In particular, whether EBV can cause retinitis in immunodeficient patients remains highly controversial. The vitreous cavity injection of ganciclovir treatment was effective essentially ruling out the possibility of EBV retinitis. Therefore, the final and most likely diagnosis for this patient remains CMV retinitis. However, the evidence of simultaneous intraocular infection by all three viruses is clear. As the concomitant detection of all three viruses in the same patient’s eye is still quite rare, this case has certain research value.
Fortunately, all three viruses were disappeared after vitreous cavity injections of ganciclovir. With only one vitreous cavity injection, the patient’s aqueous humour screen was negative for virual infection. The fundal condition of the patient also remained stable for the time being.
Through this case, we were still able to recognize that it is still quite necessary to perform aqueous humour testing in such immunodeficient patients once they present with ocular symptoms. This is because (1) blood virus testing is hardly a true reflection of the viral situation in the eye, and (2) CMV infection is most common in this type of patient, but other viruses are also present with the possibility of infection, especially those usually thought to be present in immunocompetent individuals.
Although we currently do not know why patients are infected with these viruses at the same time, we hope to conduct further research to avoid multiple infections as much as possible and to be able to protect the vision of these unfortunate patients to the greatest extent achievable.
Data availability
Supporting data for the results of this study are available from the authors upon request. The e-mail address is 21718142@zju.edu.cn.
Abbreviations
- AIDS:
-
Acquired immunodeficiency syndrome
- CMV:
-
Cytomegalovirus
- HSV:
-
Herpes simplex virus. VZV:varicella-zoster virus
- EBV:
-
Epstein-Barr virus
- HSCT:
-
Hematopoietic stem cell transplant
- OCT:
-
Optical coherence tomography
- FFA:
-
Fundus fluorescein angiography
- ICGA:
-
Indocyanine green angiography
- QPCR:
-
Quantitative Polymerase Chain Reaction
References
Gao C, MA X, Zhang Z, et al. Asparaginase erwinia chrysanthemi for acute lymphoblastic leukemia and lymphoblastic lymphoma[J]. Drugs Today (Barc). 2022;58(6):261–71.
Cao XY, LI JJ, LU PH, et al. Efficacy and safety of cd19 car-t cell therapy for acute lymphoblastic leukemia patients relapsed after allogeneic hematopoietic stem cell transplantation[J]. Int J Hematol. 2022;116(3):315–29.
MA R, Liu XT, Chang YJ. Allogeneic hematopoietic stem cell transplantation for acute lymphoblastic leukemia: current status and future directions mainly focusing on a Chinese perspective[J]. Expert Rev Hematol. 2022;15(9):789–803.
Liu M, HE H, LU Q, et al. Cmv retinitis and subsequent acute cystoid macular oedema after treatment with vitreous ganciclovir injection: a case report[J]. BMC Ophthalmol. 2022;22(1):284.
Huang EJ, Wang CP, Lai CH, et al. Rapid regression of cystoid macular edema associated with cytomegalovirus retinitis in adult acute myeloid leukemia by intravitreal methotrexate combined with oral valganciclovir: a case report with comparison of binocular outcome[J]. Taiwan J Ophthalmol. 2016;6(3):145–9.
Steve RJ, Mammen S, Selvaraj K, et al. Comparison of a chemiluminescence immunoassay and an enzyme immunoassay for detection of igm antibodies against measles, mumps, rubella, cytomegalovirus (cmv), Epstein Barr virus (ebv), and human herpes virus (hhv) -1 and– 2 infections[J]. Indian J Med Microbiol. 2022;40(3):354–8.
Carmichael A. Cytomegalovirus and the eye[J]. Eye (Lond). 2012;26(2):237–40.
YI ES, Lee JW, Kim YJ, et al. Risk factors and outcomes of cytomegalovirus infection in children post cord blood transplantation with focus on impact of graft-versus-host disease and immunosuppressants[J]. Ann Hematol. 2022;101(2):409–19.
Crippa F, Corey L, Chuang EL, et al. Virological, clinical, and ophthalmologic features of cytomegalovirus retinitis after hematopoietic stem cell transplantation[J]. Clin Infect Dis. 2001;32(2):214–9.
Reusser P, Fisher LD, Buckner CD, et al. Cytomegalovirus infection after autologous bone marrow transplantation: occurrence of cytomegalovirus disease and effect on engraftment[J]. Blood. 1990;75(9):1888–94.
James JA, KAufman KM, Farris AD, et al. An increased prevalence of epstein-barr virus infection in young patients suggests a possible etiology for systemic lupus erythematosus[J]. J Clin Invest. 1997;100(12):3019–26.
Bonfioli AA, Eller AW. Acute retinal necrosis[J]. Semin Ophthalmol. 2005;20(3):155–60.
Classification criteria for. Acute retinal necrosis syndrome[J]. Am J Ophthalmol. 2021;228:237–44.
Madhavan HN, Priya K, Biswas J. Current perspectives of herpesviral retinitis and choroiditis[J]. Indian J Pathol Microbiol. 2004;47(4):453–68.
Schoenberger SD, Kim SJ, Thorne JE, et al. Diagnosis and treatment of acute retinal necrosis: a report by the American academy of ophthalmology[J]. Ophthalmology. 2017;124(3):382–92.
Aksu-Ceylan N, Güner ME, Cebeci Z, et al. Association between prognosis of acute retinal necrosis and retinal involvement[J]. Turk J Ophthalmol. 2022;52(6):405–11.
Cho J, Bhavsar AR, Cho DH, et al. Successful treatment of epstein-barr virus-induced necrotizing retinitis with intravitreous ganciclovir, foscarnet, and methotrexate[J]. Case Rep Ophthalmol. 2022;13(1):116–23.
Mushiga Y, Komoto T, Nagai N, et al. Effects of intraocular treatments for epstein-barr virus (ebv) retinitis: a case report[J]. Med (Baltim). 2021;100(48):e28101.
Ergazaki M, Xinarianos G, Giannoudis A, et al. Detection of hsv, cmv and ebv by the polymerase chain-reaction technique in patients with inflammatory eye-diseases[J]. Oncol Rep. 1994;1(6):1207–10.
Alvarez-Guzman C, Ortiz-Morales G, Ruiz-Lozano R et al. Simultaneous amplification of herpes simplex virus type 2 and epstein–barr virus in an immunocompetent host with acute retinal necrosis[J]. Pan-American J Ophthalmol. 2021;3(1).
Lopez J, Hua HU, Toy BC. A case of herpes simplex virus and cytomegalovirus retinitis coinfection[J]. Retin Cases Brief Rep; 2023.
Samanta R, Puthalath AS, Sood G et al. Macular dual retinitis with herpes simplex and cytomegalovirus following periocular corticosteroid in a patient of pemphigus vulgaris[J]. Eur J Ophthalmol. 2021:11206721211052847.
Sato T, Kitamura R, Kaburaki T, et al. Retinitis associated with double infection of epstein-barr virus and varicella-zoster virus: a case report[J]. Med (Baltim). 2018;97(31):e11663.
Acknowledgements
We thank the Affiliated People’s Hospital of Ningbo University for providing the case and the comprehensive examination.
Funding
Science and Technology Innovation 2025 Major Project of Ningbo, China (2021Z054) for data collection. Ningbo Clinical Research Center for Ophthalmology and the Project of NINGBO Leading Medical&Health Disipline (2016-S05) for medical history analysis. Ningbo Public Welfare Science and Technology Plan Project (2022S054) for a portion of the patient’s treatment and exams. Zhejiang Medical and Health Science and Technology Plan Project (2023KY300、2023KY301). Ningbo Natural Science Foundation (2023J385). Zhejiang Medical and Health Science and Technology Plan Project(2024KY372). Ningbo Natural Science Foundation(2023J170). Zhejiang Provincial Natural Science Foundation of China (LQ23H120001). Science and Technology Program of Traditional Chinese Medicine in Zhejiang Province (2024ZL920). Ningbo Clinical Research Center for Ophthalmology (2022L003). Ningbo Key Laboratory for neuroretinopathy medical research.
Author information
Authors and Affiliations
Contributions
All the authors of this article have read and approved the manuscript. MYL, first author, completed the first draft of the article and extensive revisions. HQH, one coauthor, played an extremely important role in revising and embellishing the article. JTZ, second coauthor, revised and improved the whole article. SHX, third author, provided information on the disease and helped to analyze the possible scenarios of the case. QKL, fourth author, provide funding and technical analysis. LFZ, fifth author, fund the article. WNR, corresponding author, provided all data and images of the case and participated in the review and revision of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of clinical data and/or images. Each author reviewed the final manuscript. All consented to the publication of the article and signed the written consent form.
Competing interests
All the authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
QPCR probes and primers
Virus | Forward primer | Reverse primer | Probe |
|---|---|---|---|
CMV | CCAACAGGATCATCGACCTCA | GAATCTCCTCGAGAATATGCTTGATTT | ACCCGGTGTTCAACAAGCTCC |
VZV | TTGAACTGGATCTGTAGAGCAAC | CCTCTAAATCACATAACAGGTCACT | CAGACCGCGATGTAAGCCGAA |
HSV | GCATCGCGGTGGTCTTCA | GAGTAGCGGTGGCCGAA | TCAAGGCCACCATGTACTACAAAGAC |
EBV | CCCGGATAGACCTGGATGAC | CCCAAATTAAATAGTGATGCCAAAGAC | ATGCGTGTGATGATGACCTACCT |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, M., He, H., Zhang, J. et al. Retinitis after haematopoietic stem cell transplantation with multiple intraocular viral infections (cytomegalovirus, Epstein‒Barr virus and herpes simplex virus)- a case report. BMC Ophthalmol 24, 38 (2024). https://doi.org/10.1186/s12886-024-03300-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03300-4