Abstract
Upper eyelid surgeries, such as blepharoplasty and ptosis correction, are commonly performed procedures worldwide. This review examines the effects of these surgeries on ocular properties and visual function. A search of the PubMed and Google Scholar databases was conducted to identify relevant articles published after 2000. The results demonstrate that the ocular and adnexal organs function as a unified visual system, with changes in one component affecting the functions of others. Eyelid surgery can alter ocular properties and functions by modifying retinal lighting and ocular optics. These alterations can affect intraocular pressure estimation, corneal curvature, corneal epithelial thickness, refractive power of the cornea, and intraocular lens calculation. Additionally, eyelid surgery can exacerbate dry eye symptoms and impact contrast sensitivity, which is a significant factor in visual quality. Therefore, understanding these interactions is crucial before performing eyelid surgery and during follow-up. This review summarizes recent literature on the effects of upper eyelid surgery on corneal properties and visual function, emphasizing the importance of considering these factors when planning or undergoing such procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Eyelid surgeries, including blepharoplasty and ptosis repair, are among the most performed orbital and cosmetic procedures worldwide. In the United States alone, over 200,000 blepharoplasties are conducted annually [1]. Patients with heavy and structurally lax eyelids may experience increased pressure on the globe, which can affect various ocular measurements such as anterior corneal curvature and epithelial thickness, corneal refractive power, and intraocular lens (IOL) calculations [2,3,4,5,6,7]. For instance, severe ptosis correction has been found to induce significant changes in corneal spherical and cylindrical power, corneal aberrations, and contrast sensitivity, among other factors [2, 3, 8, 9]. Furthermore, upper eyelid blepharoplasty and blepharoptosis repair can lead to varying degrees of dry eye that may persist for several months after surgery [10, 11]. The impact of these factors on other ocular and orbital therapeutic and cosmetic procedures can be decisive. As such, it may be advisable to perform orbital and cosmetic surgery prior to intraocular surgery to achieve more predictable outcomes with minimal manipulation. However, it is important to note that some surgeons often delay eyelid surgery until after intraocular surgery because the use of an eyelid speculum can stretch the eyelids and orbicularis and cause ptosis.
Given the increasing number of orbital and cosmetic procedures being performed worldwide as well as a growing body of literature examining their effects on visual function, it is imperative that we review existing research to better understand how these surgeries impact ocular surface characteristics, corneal properties, and visual function while also identifying areas where further investigation is needed.
Methods
We conducted a comprehensive literature search using the PubMed and Google Scholar databases. Our search strategy included these keywords: blepharoplasty, blepharoptosis, ptosis, cornea, corneal topography, dry eye, astigmatism, and tear. We limited our search to English articles published after the year 2000 and carefully selected relevant studies for inclusion in this narrative review. Our search yielded a total of forty original articles, one review article, and one case report. The data extracted from these sources were meticulously analyzed and presented in two tables (Table 1 and Table 2), organized according to the type of surgery performed.
Main Text
Corneal optics
The cornea plays a crucial role in visual acuity due to its contribution of approximately two-thirds of the eye’s total optical power. The anterior surface curvature of the cornea is primarily responsible for corneal refraction. Given that this surface is in direct contact with the eyelids, alterations in eyelid shape and function can result in changes to corneal refraction, steep and flat corneal meridians, refractive error, and corneal astigmatism.
Gullstrand’s hypothesis suggests that induced corneal astigmatism is caused by pressure from the eyelid on the vertical meridian, resulting in with-the-rule (WTR) astigmatism [37]. This pressure flattens the corneal periphery while steepening the central region [30, 31, 36]. Consequently, elevating the eyelid causes central flattening and peripheral steepening. Assadi et al. reported significant flattening of the inferior cornea six months after levator resection or sling surgery on 27 eyes with congenital ptosis [33]. Zinkernagel et al. found that all patients showed significant changes in corneal astigmatism within a central 5-mm zone after ptosis correction with a mean change of 0.72 D [14]. Pressure exerted by the eyelid on the periphery of a ptotic eye’s cornea causes a flat periphery and steep center resulting in astigmatism. Ptosis surgery corrects this condition, with the greatest effect being observed at the center of the cornea [14]. Preoperative ptosis severity predicts postoperative corneal astigmatism alteration. Severe ptosis causes steepening of the inferior meridian, which subsequently experiences the greatest flattening after surgery [33]. Conversely, mild ptosis causes steepening of the superior meridian, which then undergoes the most significant flattening postoperatively [29]. Aydemir and Aydemir investigated the impact of ptosis on IOL power calculation. The results indicated that only patients with ptosis greater than 4 mm experienced significant reduction in corneal curvature and astigmatism following surgery [5]. Therefore, for patients with severe eyelid ptosis and cataracts, it is crucial to account for potential changes in IOL power calculation after ptosis surgery.
Uğurbaş and Zilelioğlu found a significantly increased rate of astigmatism in ptotic eyes compared to normal control eyelids in their study on 44 eyes of 22 patients with congenital ptosis. These ptotic eyes typically exhibited a bow-tie pattern on topographic maps [8]. Another cross-sectional study by Kim and Lee on 33,103 Korean individuals reported a hyperopic shift and increased against-the-rule (ATR) astigmatism in ptotic eyelids [3].
A study by Kim and colleagues found that 6 weeks after levator resection surgery, corneal power increased and astigmatism decreased in half of the cases [18]. However, after blepharoplasty surgery, corneal power and astigmatism remained unchanged in most patients. The lower changes in corneal power and astigmatism are attributed to a relatively smaller change in lid position following blepharoplasty surgery. Brown et al. reported average dioptric changes of approximately 0.60 D and 0.55 D after ptosis repair and blepharoplasty surgeries [23]. Nearly 30% of ptosis repair patients exhibited transient astigmatic changes exceeding 1.00 D, compared to only 11% of blepharoplasty patients. The patient may need to change their spectacle or contact lens correction after surgery. Dogan et al. evaluated the corneal parameters using Scheimpflug imaging for patients who underwent upper blepharoplasty [16]. The study found that the steepest keratometry significantly increased in patients with margin reflex distance 1 (MRD1) less than 2.5 mm. However, no significant changes were observed in visual acuity and astigmatic power vectors (J0 and J45). Sommer et al. performed skin-only blepharoplasty on 42 eyes, resulting in a 0.4 D increase in the Kmax after 4 weeks [4]. However, the difference between the inferior-superior (I-S) value decreased by 0.22 D. These changes in corneal curvature did not result in significant changes to the BCVA. Simsek et al. also observed a small mean increase of 0.15 D in corneal astigmatism among 60% of their participants one month after blepharoplasty surgery [9]. However, this increase was only borderline significant three months thereafter. In a study by Zinkernagel and coworkers, 82 eyes were assessed before and 3 months after blepharoplasty or ptosis correction surgery [14]. The authors observed that ptosis correction and blepharoplasty with removal of pre-aponeurotic fat pads caused alterations of 0.25 D and 0.21 D in total corneal astigmatism, respectively. Blepharoplasty without resection of pre-aponeurotic fat pads caused an insignificant change of 0.09 D in corneal astigmatism. This may be due to the lower gravitational effect on the cornea of skin-only blepharoplasty. Interestingly, ptotic patients with deep superior sulcus may experience greater reduction in cylindrical power than others following blepharoptosis surgery due to more structurally rigid eyelids in patients with deepening of the upper eyelid sulcus [32].
Some studies report no significant change in topographic corneal parameters following ptosis correction surgery [28, 35], but these may be limited by small sample sizes or short follow-up periods. Interestingly, Youssef et al. reported a decrease of 0.5 D and 0.9 D in corneal astigmatism and corneal power, respectively, three months after surgery despite finding no significant alteration one month postoperatively [30]. Older studies have reported an increase in corneal astigmatism following ptosis correction surgery, but these primarily used keratometric measurements which do not directly measure corneal curvature. Other studies also reported a reversal of this increase after resolution of temporary post-operative eyelid edema [38]. As post-operative eyelid edema can persist for up to two months following blepharoplasty surgery [39], it is recommended to repeat corneal topography and refraction three months postoperatively before making further decisions.
Mongkolareepong et al. identified pre-operative corneal astigmatism as a key predictor of postoperative change in corneal astigmatism [34]. Specifically, 72.2% of patients with preoperative corneal astigmatism greater than 1.5 D experienced a decrease of 0.65 D following ptosis surgery, while patients with less than 1.5 D corneal astigmatism did not experience significant changes.
Gandhi et al. observed a decrease of 0.47 D in corneal astigmatism following frontalis suspension surgery, with a more pronounced reduction in patients aged 5–10 years [31]. The authors suggested that performing surgery for severe ptosis at a younger age may be more beneficial due to increased corneal flaccidity of children. Another study also documented a significant change of 0.43 diopters in corneal astigmatism three months after ptosis correction surgery in patients aged 4–12 years [40].
Sussenbach et al. described a noteworthy case in which high corneal astigmatism was concealed by the stenopic effect of a ptotic eyelid with a narrow palpebral fissure, resulting in good vision for the patient [41]. However, following surgical elevation of the eyelid, the underlying keratoconus was revealed, and the patient reported a decreased vision.
The factors that influence changes in corneal astigmatism following eyelid surgery can be summarized as follows:
-
Type of surgery: Ptosis correction has a greater impact than upper eyelid blepharoplasty, and fat removal during upper blepharoplasty has a greater effect than skin removal alone [10, 11].
-
Severity of preoperative ptosis: The more severe the ptosis, the greater the change in corneal astigmatism following surgery [5, 35].
-
Preoperative corneal astigmatism: If above 1.5 D, it will have a greater effect in reducing astigmatism after ptosis correction surgery [29].
-
Patient age: Younger patients tend to experience a greater reduction in corneal astigmatism following ptosis surgery [18, 23].
-
Duration of patient follow-up: Changes in astigmatism become more stable over time after eyelid surgery, particularly after 6 months [9, 14, 30, 33].
Studies have generally shown a mild increase in corneal dioptric power following ptosis repair surgeries. Changes greater than 0.5 D may induce visually significant alterations and should be discussed with the patient prior to surgery [42]. However, other studies have demonstrated that changes in corneal refraction and keratometry six months after levator resection surgery in adults are not statistically significant. Brief subjective visual symptoms may be attributed by changes in the eyelid position or age-related changes in the lens and cataract formation [43].
Corneal biomechanics
Corneal biomechanics encompasses the properties of the cornea that dictate its response to external forces. The properties are characterized by parameters such as corneal hysteresis and corneal resistance factors. Corneal hysteresis refers to the difference between the air pressure on the cornea during deflation and inflation, while corneal thickness plays a crucial role in determining corneal resistance factors [44]. The impact of ptosis and dermatochalasis on corneal biomechanics is an emerging area of research that has recently garnered attention from several authors. Given that these conditions can affect patients across all age groups, their influence on corneal biomechanics may significantly alter outcomes for various corneal pathologies and treatments, including keratoconus, cataract surgery, and refractive surgery. As such, it is imperative to elucidate the effect of ptosis and dermatochalasis on corneal biomechanics.
In one study conducted by Sommer and colleagues, minimal increases in both corneal hysteresis and corneal resistance factor were observed four weeks following skin-only blepharoplasty surgery; however, these increases were not statistically significant [4]. In another study conducted by Li et al., corneal biomechanical parameters were assessed by Corvis ST tonometry. The results indicated that these parameters differed minimally but significantly between ptotic eyes and normal eyes [7]. Furthermore, these differences remained unchanged six months post-surgery. The authors concluded that ptotic eyes have thicker corneas and exhibit less flexibility in response to external forces. However, further research is necessary to elucidate the potential effects of ptosis and dermatochalasis, as well as their corrective surgeries, on corneal biomechanics.
In brief, it is important to consider that alterations in eyelid position following eyelid surgery may result in significant changes in corneal biomechanical properties. These changes are particularly relevant in corneas with intrinsic pathology or abnormal thickness.
Contrast sensitivity and higher-order aberrations
Contrast sensitivity is defined as the ability to distinguish an object from its background. This visual ability differs from visual acuity, which measures the clarity of vision at distance. As such, two individuals with identical visual acuity may exhibit different contrast sensitivities that determine their visual performance, particularly in dimly lit environments [45].
Higher-order aberration (HOA) is a significant factor in contrast sensitivity and refers to the distortion acquired by a wavefront of light when it encounters an eye with imperfections in its refractive components. When subjects narrow their palpebral fissures, both HOA and lower-order aberration (LOA) increase [46]. In a study by Han et al., the authors assessed the squeezing effect of the eyelids on the globe in near vision and then administered cycloplegic drops to eliminate their effect [46]. They observed that after treatment with the cycloplegic drug, neither spherical aberration nor spherical defocus increased with squeezing of the eyelids; however, vertical coma and astigmatism were still significantly induced. None of these changes were significant after correction. Accordingly, they concluded that vertical pressure from eyelids when a patient is squeezing them can result in LOA and HOA and cause reduced contrast sensitivity. They also reported that placing artificial eyelashes in front of a subject’s eye increased visual aberrations and reduced vision quality.
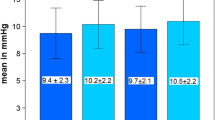
In 2015, Fowler et al. published a study assessing the contrast sensitivity of 78 eyes after functional blepharoplasty and ptosis surgery. They reported an 11% increase in contrast sensitivity [27]. Interestingly, this increase was reproducible with preoperative taping of the eyelids in the correct position; the level of contrast sensitivity in the preoperative taped and postoperative periods was not significantly different. In another study, Nalci et al. observed that three months after blepharoplasty for patients with dermatochalasis, contrast sensitivity significantly increased, and this increment was not related to improvement in eyelash ptosis [20]. They reported that this increase mainly occurred in the high spatial frequencies of the contrast sensitivity spectrum; given that this range may decrease with aging, they concluded that blepharoplasty for treatment of dermatochalasis can increase contrast sensitivity and thus improve vision quality in older patients. In their long-term prospective study, Bhattacharjee et al. followed 60 eyes that underwent upper blepharoplasty for a period of 12 months [21]. The authors demonstrated that the mean contrast sensitivity value, HOA, and cylindrical power remained stable and significantly improved. They concluded that older patients undergoing cataract surgery can gain additional visual benefits from upper blepharoplasty. Improvement in photopic and mesopic contrast sensitivity after treatment of dermatochalasis and lash ptosis has been reported in other studies as well [17].
Several reasons have been hypothesized for the increase in contrast sensitivity after blepharoplasty, including treatment of lash ptosis, corneal topographic changes, and reduction of HOA [42]. Redundant skin over the eyelids can reduce light entering the eye and exert a diffractive effect that reduces contrast sensitivity. If dermatochalasis involves the central region of the cornea it can decrease central vision; furthermore, lash ptosis can interfere with central vision [15]. A study conducted by Ekin and Ugurlu in 2019 indicated that contrast sensitivity and HOA significantly improved one month after blepharoplasty [22]. This improvement was more prominent in patients with preoperative MRD1—distance between the upper lid margin and corneal light reflex—lower than 2 mm. Kim et al. also demonstrated that after blepharoplasty, contrast sensitivity and functional vision improved due to reduction of HOA and correcting of eyelash position [2]. The authors reported a decrease in the 3rd and 4th order aberrations as well as coma and trefoil. Kumar et al. reported an increase in total root mean square (RMS) of HOA in the ptotic eyes compared to normal eyes [24]. They also noted significant differences in the mean of multiple Zernicke coefficients at 6 mm.
Briefly, contrast sensitivity significantly increases after blepharoplasty and ptosis correction surgeries (especially in higher spatial frequencies), potentially improving vision quality in patients with severe functional dermatochalasis. This increase in contrast sensitivity can be due to correction of eyelash ptosis and increased light entering the eye, as well as reduction of HOA. This improvement persists for at least three months after surgery; further studies are needed to examine changes beyond this time period [20, 27, 42,43,44,45,46].
Dry eye
Dry eye symptoms may be exacerbated following blepharoplasty due to several factors including chemosis, postoperative inflammation, lagophthalmos, excess orbicularis resection and/or denervation, eyelid retraction, and malfunction of the lacrimal pumping system [12, 15, 17, 21, 22, 24]. Note that aggressive blepharoplasty leading to lagophthalmos can exacerbate dry eye and lead to keratopathy and neurotrophic keratitis.
A study by Wee and Lee examining 51 eyes investigated the impact of Muller’s muscle-conjunctival resection surgery on dry eye [26]. Evaluation utilizing Schirmer’s test and tear break-up time (TBUT) test revealed that tear adequacy was significantly and transiently disrupted for 2 months following surgery but returned to preoperative levels thereafter. However, Kim et al. found no significant disruption in tear adequacy following either blepharoplasty or ptosis correction surgery [13]. Similarly, other studies did not report this disruption in tear adequacy during long-term follow-up [25, 47]. Interestingly, Rymer et al. demonstrated that dry eye symptoms improved significantly 3 months after blepharoplasty in conjunction with Muller’s muscle conjunctival resection but not in the blepharoplasty-only group [11]. Nevertheless, none of the objective tests such as Schirmer’s test, Rose Bengal staining test, fluorescein staining test or TBUT test showed significant differences between the two groups. The authors postulate that this discrepancy between subjective and objective evaluations may be attributed to an improvement in dermatochalasis and ptosis resulting in patient satisfaction and a reduction in dry eye complaints. Another potential explanation for this observation is that the correction of ptosis may lead to an improvement in blink eyelid excursion, resulting in enhanced distribution of the tear film.
There are several predictive factors that can be used to determine which patients may be susceptible to dry eye symptoms following blepharoplasty surgery. Mohammed observed that a transient reduction in TBUT was seen only when the orbicularis muscle strip was removed during blepharoplasty [19]. Saadat and Dresner also suggested that blepharoplasty without orbicularis strip resection is safe for patients with dry eye disease [12]. Other risk factors for developing or aggravating dry eye after blepharoplasty include preoperative use of lubricating drugs, diabetes, hypothyroidism, a positive history of allergy, and a history of refractive surgery [10, 21]. Dry eye symptoms following blepharoplasty are typically transient and self-limited. McKinney and Byun do not recommend using tear production tests such as Schirmer’s test and TBUT for diagnosing dry eye after blepharoplasty because these tests measure reflex tear production rather than basal excretion [48]. Instead, they suggest that a patient's medical history and careful examination of eyelid anatomy are more accurate predictors of dry eye following eyelid surgery.
In brief, it is important to note that dry eye symptoms may be transiently aggravated during the first few weeks following blepharoplasty or ptosis correction surgery. Patients should be informed of this possibility prior to surgery. Typically, these symptoms will resolve within 2–3 months after eyelid surgery. The risk of induced dry eye can be minimized by performing minimal orbicularis muscle resection and denervation during surgery and by providing intensive treatment of dry eye and blepharitis prior to eyelid surgeries.
Similarities and differences between blepharoplasty and ptosis surgery
Both procedures can alter ocular properties and functions by modifying retinal lighting and ocular optics. Additionally, both surgeries can exacerbate dry eye symptoms and impact contrast sensitivity, which is a significant factor in visual quality.
However, ptosis correction surgery has a greater impact on corneal astigmatism than upper eyelid blepharoplasty. Fat removal during upper blepharoplasty has a greater effect on corneal astigmatism than skin removal alone. The severity of preoperative ptosis is also a predictor of postoperative corneal astigmatism alteration.
Conclusions
This review article highlights recent studies that have reported significant effects of upper eyelid surgery on refractive conditions, ocular aberrations, and visual quality. Contrast sensitivity, an important factor role in visual quality, is greatly affected by upper eyelid surgery. Additionally, eyelid surgery can exacerbate dry eye symptoms. However, ptosis correction surgery has been found to have a greater impact on corneal astigmatism than upper eyelid blepharoplasty. Therefore, it is important to consider these factors before undergoing surgery or when planning to have refractive or intraocular procedures after eyelid surgery.
Availability of data and materials
Not applicable.
Abbreviations
- IOP:
-
Intraocular pressure
- IOL:
-
Intraocular lens
- ATR:
-
Against-the-rule
- MRD1:
-
Margin reflex distance 1
- BCVA:
-
Best-corrected visual acuity
- WTR:
-
With-the-rule
- HOA:
-
Higher-order aberration
- LOA:
-
Low-order aberration
- RMS:
-
Root mean square
- TBUT:
-
Tear break-up time
References
Gadkaree SK, McCarty JC, Weitzman RE, Derakhshan A, et al. Associations between national financial trends and facial plastic surgery procedural volume. Laryngoscope. 2020;130:632–6.
Kim JW, Lee H, Chang M, Park M, Lee TS, Baek S. What causes increased contrast sensitivity and improved functional visual acuity after upper eyelid blepharoplasty? J Craniofac Surg. 2013;24:1582–5.
Kim Y, Lee J-H. Association of blepharoptosis with refractive error in the Korean general population. Eye. 2021;35:3141–6.
Sommer F, Untch E, Spoerl E, Herber R, Pillunat LE, Terai N. Effect of upper eyelid blepharoplasty on corneal biomechanical, topographic and tomographic parameters 4 weeks after surgery. Int Ophthalmol. 2022;42:113–21.
Aydemir E, Aydemir GA. Ptosis effects on intraocular lens power calculation. J Cataract Refract Surg. 2022:https://doi.org/10.1097/j.jcrs.0000000000001063.
Dogan AS, Acar M, Kosker M, Arslan N, Gurdal C. Alterations in corneal epithelial thickness in patients with congenital myogenic eyelid ptosis. Int Ophthalmol. 2018;38:53–7.
Li X, Liu C, Mao Z, Liang X, et al. Effect of congenital blepharoptosis on corneal biomechanical properties and changes after ptosis surgery. Eye. 2020;34:1055–62.
Uğurbaş SH, Zilelioğlu G. Corneal topography in patients with congenital ptosis. Eye. 1999;13:550–4.
Simsek IB, Yilmaz B, Yildiz S, Artunay O. Effect of upper eyelid blepharoplasty on vision and corneal tomographic changes measured by pentacam. Orbit. 2015;34:263–7.
Fagien S. Reducing the incidence of dry eye symptoms after blepharoplasty. Aesthet Surg J. 2004;24:464–8.
Rymer BL, Marinho DR, Cagliari C, Marafon SB, Procianoy F. Effects of Muller’s muscle-conjunctival resection for ptosis on ocular surface scores and dry eye symptoms. Orbit. 2017;36:1–5.
Saadat D, Dresner SC. Safety of blepharoplasty in patients with preoperative dry eyes. Arch Facial Plast Surg. 2004; 6:101
Kim HH, De Paiva CS, Yen MT. Effects of upper eyelid blepharoplasty on ocular surface sensation and tear production. Can J Ophthalmol. 2007;42:739–42.
Zinkernagel MS, Ebneter A, Ammann-Rauch D. Effect of upper eyelid surgery on corneal topography. Arch Ophthalmol. 2007;125:1610–2.
Rogers SA, Khan-Lim D, Manners RM. Does upper lid blepharoplasty improve contrast sensitivity? Ophthal Plast Reconstr Surg. 2012;28:163–5.
Dogan E, Akbas Kocaoglu F, Yalniz-Akkaya Z, Elbeyli A, Burcu A, Ornek F. Scheimpflug imaging in dermatochalasis patients before and after upper eyelid blepharoplasty. Semin Ophthalmol; 2015; 30:193–196.
An SH, Jin SW, Kwon YH, Ryu WY, Jeong WJ, Ahn HB. Effects of upper lid blepharoplasty on visual quality in patients with lash ptosis and dermatochalasis. Int J Ophthalmol. 2016;9:1320.
Kim YK, In JH, Jang SY. Changes in corneal curvature after upper eyelid surgery measured by corneal topography. J Craniofac Surg. 2016;27:e235–8.
F Mohammed M. Impact of orbicularis oculi muscle strip excision during upper lid blepharoplasty on tear film break up time and postoperative dry eye symptoms. Al-Azhar Med J. 2018;47:539–550.
Nalci H, Hosal MB, Gunduz OU. Effects of upper eyelid blepharoplasty on contrast sensitivity in dermatochalasis patients. Turk J Ophthalmol. 2020;50:151–6.
Bhattacharjee K, Misra D, Singh M, Deori N. Long-term changes in contrast-sensitivity, corneal topography and higher-order aberrations after upper eyelid blepharoplasty: A prospective interventional study. Indian J Ophthalmol. 2020;68:2906.
Altin Ekin M, Karadeniz US. Prospective analysis of visual function changes in patients with dermatochalasis after upper eyelid blepharoplasty. Eur J Ophthalmol. 2020;30:978–84.
Brown MS, Siegel IM, Lisman RD. Prospective analysis of changes in corneal topography after upper eyelid surgery. Ophthal Plast Reconstr Surg. 1999;15:378–83.
Kumar DA, Agarwal A, Prakash G, Boptm NV, Packiyalakshmi S, Agarwal A. Effect of unilateral congenital ptosis on ocular higher order aberrations in children. Med Hypothesis Discov Innov Ophthalmol. 2013;2:86.
Uğurbaş SH, Alpay A, Bahadır B, Uğurbaş SC. Tear function and ocular surface after muller muscle-conjunctival resection. Indian J Ophthalmol. 2014;62:654.
Wee SW, Lee JK. Clinical outcomes of Conjunctiva-Müller muscle resection: association with phenylephrine test-negative blepharoptosis and dry eye syndrome. J Craniofac Surg. 2014;25:898–901.
Fowler BT, Pegram TA, Cutler-Peck C, Kosko M, et al. Contrast sensitivity testing in functional ptosis and dermatochalasis surgery. Ophthal Plast Reconstr Surg. 2015;31:272–4.
Mohammed AE-G, Amin Anwar El-Masry M, El-Shiekh AE-S. Corneal topographic changes after eyelid ptosis surgeries measured by corneal topography. Al-Azhar Med J. 2021;50:1119–1126.
Karabulut GO, Fazil K. Corneal topographical changes after Müller’s muscle-conjunctival resection surgery. Ophthal Plast Reconstr Surg. 2019;35:177–81.
Youssef AY, Abo-eleinin MA-e, Salama OH. Corneal topographic changes after eyelid ptosis surgery. Al-Azhar Int Med J. 2020;1:236–241.
Gandhi A, Mehta A, Naik M. Does frontalis sling surgery for congenital ptosis change the corneal topography and refractive characteristics postoperatively? Clinical Ophthalmology (Auckland, NZ). 2020;14:3667.
Numata A, Yunoki T, Otsuka M, Hayashi A. Corneal topographic changes after blepharoptosis surgery in patients with deepening of the upper eyelid sulcus. Jpn J Ophthalmol. 2021;65:282–7.
Assadi FA, Narayana S, Yadalla D, Rajagopalan J, Joy A. Effect of congenital ptosis correction on corneal topography-A prospective study. Indian J Ophthalmol. 2021;69:1527.
Mongkolareepong N, Mekhasingharak N, Pimpha O. Factors associated with corneal astigmatism change after ptosis surgery. Int J Ophthalmol. 2022;15:576.
ABDEL RAHMAN IH, ISMAIL ZF, ELREDY AS, SHAAT AA. Corneal topographic changes after correction of ptosis by Levator muscle resection measured by Scheimpflug Imaging. Med J Cairo Univ. 2022;90:747–753.
Ceylan NA, Yeniad B. Effects of Upper Eyelid Surgery on the Ocular Surface and Corneal Topography. Turk J Ophthalmol. 2022;52:50.
Helmholtz HL. Helmholtz's treatise on physiological optics. Dover; 1962.
Holck D, Dutton JJ, Wehrly SR. Changes in astigmatism after ptosis surgery measured by corneal topography. Ophthal Plast Reconstr Surg. 1998;14:151–8.
Parbhu KC, Hawthorne KM, McGwin G Jr, Vicinanzo MG, Long JA. Patient experience with blepharoplasty. Ophthal Plast Reconstr Surg. 2011;27:152–4.
Agrawal G, Ravani S. Astigmatic changes following ptosis correction surgery in 30 consecutive children seen in a regional institute of ophthalmology. Int J Curr Res. 2016;8:1.
Sussenbach EC, Thomas DA, Patterson EG, Bogorad DD. Keratoconus unmasked by unilateral ptosis repair. Ophthal Plast Reconstr Surg. 2012;28:e32–3.
Hollander MH, Contini M, Pott JW, Vissink A, Schepers RH, Jansma J. Functional outcomes of upper eyelid blepharoplasty: a systematic review. J Plast Reconstr Aesthet Surg. 2019;72:294–309.
Gingold MP, Ehlers WH, Rodgers IR, Hornblass A. Changes in refraction and keratometry after surgery for acquired ptosis. Ophthal Plast Reconstr Surg. 1994;10:241–6.
Rosa N, Lanza M, De Bernardo M, Signoriello G, Chiodini P. Relationship between corneal hysteresis and corneal resistance factor with other ocular parameters. Semin Opthalmol. 2015; 30:335–339.
Packer M, Fine IH, Hoffman RS. Functional vision, contrast sensitivity, and optical aberrations. Int Ophthalmol Clin. 2003;43:1–3.
Han W, Kwan W, Wang J, Yip SP, Yap M. Influence of eyelid position on wavefront aberrations. Ophthalmic Physiol Opt. 2007;27:66–75.
Dailey RA, Saulny SM, Sullivan SA. Müller muscle–conjunctival resection: effect on tear production. Ophthal Plast Reconstr Surg. 2002;18:421–5.
McKinney P, Byun M. The value of tear film breakup and Schirmer's tests in preoperative blepharoplasty evaluation. Plast Reconstr Surg. 1999;104:566–569; discussion 570.
Acknowledgements
Not applicable.
Funding
No financial support.
Author information
Authors and Affiliations
Contributions
SMR and MTR conceived and designed the research. MH and AAH did the literature review and wrote the paper. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study follows the tenets of the Declaration of Helsinki. Ethical approval was waived because it is a review.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Heidari, M., Haydar, A.A., Rajabi, M.T. et al. Corneal biophysical changes after upper eyelid blepharoplasty and ptosis surgery: a review. BMC Ophthalmol 23, 253 (2023). https://doi.org/10.1186/s12886-023-03010-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-03010-3