Abstract
Purpose
To compare the efficacy and safety of infliximab with that of adalimumab in the treatment of non-infectious uveitis (NIU).
Methods
We searched for relevant studies in the PubMed, Embase, ClinicalTrials.gov, Cochrane Library databases, Grey Matters, Grey Literature Report, OpenGrey, China National Knowledge Infrastructure (CNKI), and Wan Fang databases up to September 2022. The incidences of complete remission of inflammation, response to therapy, adverse events and corticosteroid-sparing effect were evaluated.
Results
Eleven clinical trials covering 1459 NIU patients were included. Complete remission of inflammation after therapy was achieved in 161 (37.5%) patients in the infliximab group and 151 (39.6%) patients in the adalimumab group. These two groups were not significantly different (P = 0.37). Four studies reported response to anti-TNF therapy involving 449 patients, of whom 241/272 (88.6%) treated with infliximab and 153/177 (86.4%) treated with adalimumab achieved partial or complete remission of inflammation. No significant difference was observed between the two cohorts in terms of response to therapy (P = 0.86). There was no significant difference between infliximab and adalimumab with regard to corticosteroid-sparing effect (P = 0.58). The pooled effect size (P = 0.001) showed a statistically significant difference, with the incidence of adverse events being 17.91% for infliximab and 12.12% for adalimumab.
Conclusion
Our systematic review and meta-analysis of 11 studies suggests that infliximab and adalimumab have similar therapeutic efficacy and corticosteroid-sparing effect in patients with NIU. However, adalimumab has a marginal advantage over infliximab in terms of adverse events. Large-scale RCTs with a longer follow-up are required to further evaluate these two anti-TNF-α agents in patients with NIU.
Similar content being viewed by others
Introduction
Uveitis is a heterogeneous collection of intraocular inflammatory diseases of the uveal tract [1]. The incidence is estimated to be 17–52/100,000 person-years [2], and 22% of patients with uveitis are at risk of going blind at the same time [3]. Non-infectious uveitis (NIU) is relatively more common than infectious uveitis in both adults [4] and children [5]. In a recently published article, NIU contributed to 65.7% of all 1199 patients with uveitis, and another national registry report [5] from Turkey demonstrated that 333 of 442 (75.3%) children with uveitis were NIU. The etiologies of NIU vary widely, such as Behçet’s syndrome, juvenile idiopathic arthritis (JIA), idiopathic uveitis, Vogt-Koyanagi-Harada (VKH) syndrome. In general, the NIU is considered to be a group of autoimmune-mediated disorders [6].
Corticosteroids, which remain the mainstay of current therapy for NIU, are effective in eliminating inflammation in partial NIU patients, but not so effective in patients with severe and refractory uveitis [7]. Even in patients under control with daily doses of corticosteroids, long-term side effects are a major concern. Therefore, corticosteroid-sparing agents are urgently required.
Anti-tumor necrosis factor-alpha (anti-TNF-α) as a potent, multifunctional, monoclonal antibody not only plays a crucial role in exerting the homeostatic functions of the immune system, but also has shown fairly excellent anti-inflammatory efficacy to manage refractory NIU [8]. What’s more, it has corticosteroid-sparing effect [9]. Infliximab (Remicade) and adalimumab (Humira) are two primary anti-TNF-α biologics, and both are full-length bivalent IgG monoclonal antibodies. What distinguishes infliximab from adalimumab is that infliximab is a chimeric protein of 75% human-derived and 25% mouse-derived amino acids whereas adalimumab is a fully human-derived monoclonal antibody agent [10]. Both two agents, clinically adopted as mediators of inflammation, has successfully mitigated NIU in selected patients, but Adalimumab is the only one that has completed phase III studies and has been approved for the treatment of NIU by several countries including China, the United States, Japan and European countries [11].
There is little large-scale randomized-control, double-blind trials or meta-analyses to compare Infliximab with Adalimumab for the efficacy and safety in NIU treatment, though a large number of literatures have been published in this aspect. Hence, we herein performed a systematic review and meta-analysis in order to get a higher-level evidence to evaluate the efficacy and safety of these two anti-TNF-α agents for the treatment of NIU.
Methods
This systematic review and meta-analysis was carried out in accordance with the preferred reporting items for systematic review and meta-analysis (PRISMA) statements and the protocol adhered to the PRISMA protocol guidelines.
Search strategy
We conducted a systematic search in the PubMed, Embase, ClinicalTrials.gov, Cochrane Library databases, with language restricted to English, China National Knowledge Infrastructure (CNKI), and Wan Fang databases, with language restricted to Chinese, from database inception to September 15, 2022 to identify potential papers that compared infliximab with adalimumab treatment for NIU. To ensure inclusion of all potential studies, the grey literature was also searched in three databases including Grey Matters (https://www.cadth.ca/resources/finding-evidence/grey-matters), Grey Literature Report (http://www.greylit.org/home), and OpenGrey (http://www.opengrey.eu). Appropriate methods were used, which included the application of Medical Subject Headings (MeSH) and free words related to NIU, infliximab and adalimumab, including “non-infectious uveitis”, “NIU”, “Adalimumab”, “Humira”, “Infliximab”, “Remicade”, “anti-tumor necrosis factor-alpha”, “anti-TNF-α”. The search was limited to the title, abstract and keyword fields to filter out irrelevant studies.
Inclusion criteria and exclusion criteria
Inclusion criteria were as follows: (1) randomized controlled trials or retrospective studies comparing infliximab with adalimumab treatment in patients of any ethnicity, gender, or age with a diagnosis of NIU; (2) studies containing infliximab and adalimumab as the same cohort compared with other immunosuppressants, but the data of infliximab and adalimumab could be extracted separately; (3) studies that comprise one or more than one type of NIU, regardless of chronic, severe or refractory NIU; (4) the mean follow-up time was more than 6 months; 4) studies that have at least 10 patients with NIU in each group to avoid bias.
Exclusion criteria were defined as follows: (1) duplicate reports of the same study; (2) studies in which baseline information or outcomes were not clearly stated; (3) inability to extract the data from the paper; (4) reviews and meta-analyses.
Outcome measures
The outcome measures of efficacy included the proportion of NIU patients with remission of inflammation and assessment of corticosteroid-sparing effect. The outcome measure of safety was assessed by the incidence of adverse events. Adverse events included, but not limited to: (1) allergic reactions of injection site; (2) new-onset or reactivated infection; (3) gastrointestinal discomfort; (4) adverse event-related death.
Study selection and data extraction
Two reviewers (W.S.L. and D.B.) independently screened the titles and abstracts of all searched items and all potentially relevant articles with full text were retrieved for further assessment in accordance with the predetermined inclusion and exclusion criteria. Extraction table was used to collect extracted data from the included studies which were sorted by publication date. Disagreements between the two reviewers were resolved through discussion. If not, consensus was made through consultation with a third reviewer. The following data were extracted: (1) name of the first author; (2) date of publication; (3) design of study; (4) country of study; (5) sample size; (6) age of individuals; (7) length of follow-up; (8) type of anti-TNF-α agents; (9) type of NIU; (10) number of patients achieving complete remission of inflammation; 11) number of patients achieving corticosteroid reduction; 12) number of patients with adverse events.
Risk of bias and data analysis
The quality and risk of bias of each study were evaluated using the Methods Guide for Systematic Reviews of Medical Tests from the Agency for Healthcare Research and Quality (AHRQ) [12]. The total number of included patients who experienced the outcome was counted, and all dichotomous variables, reported as rates, including complete remission of inflammation and adverse events, were preferentially employed in this meta-analysis as odds ratio by Mantel-Haenszel with fixed-effects model along with 95% confidence intervals (95% CIs). For continuous variables including corticosteroid-sparing effect, we retrieved the mean and standard deviation (SD) of corticosteroid-sparing effect by formulae which uses the sample size, median, interquartile range [13]. The pooled mean and SD were estimated by heterogeneity, which determines a random-effects or a fixed-effects model to be adopted according to the results of I 2 test and chi-square-based Q test. When I 2 > 50% and P < 0.05, a random-effects model was used; otherwise, a fixed-effects model was adopted. Sensitivity analysis was conducted by omission of specific studies. All the statistical analyses were conducted with the aid of RevMan 5.4 software (Cochrane Library Software, Oxford, UK). Potential publication bias was assessed using funnel plots and the Egger’s test which was performed with the support of STATA 14.0 software (StataCorp, College Station, TX, USA).
Results
Study selection
A total of 704 references were retrieved from all of the aforementioned databases. After screening out 362 duplicate records, 342 items were left for further evaluation by browsing abstracts and titles. Subsequently, 48 potentially relevant articles were carefully reviewed by reading the full text, and 37 papers were scrapped for a variety of reasons, including absence of outcomes of interest, non-extractable results, sample size less than 10, and papers with the possibility of sharing the same cohort of already-included studies. Finally, 11 studies were selected for meta-analysis [14,15,16,17,18,19,20,21,22,23,24]. The flowchart of the selection process and the reasons for exclusion are demonstrated in Fig. 1.
Characteristics of included studies
The characteristics of the included studies are summarized in Table 1. Of the 11 studies published between 2011 and 2022, 9 were of retrospective design and the other 2 were prospective studies, involving 1459 patients (788 females (54%) and 671males (46%)). 777 NIU patients were treated with infliximab and 682 treated with adalimumab. All studies were conducted in European countries, except one in Turkey [22] and another one in Japan [21]. One study [21] did not disclose the mean follow-up time, the others ranged from 0.5 to 3 years. The mean age was reported by total population or by treatment type and ranged from 8.8 to 57.6 years. The top 2 causes of NIU are extracted and listed in the column of “Type of NIU”. Infliximab was administered intravenously with a loading dose of 3-5 mg/kg at 0, 2, 6 weeks, and continued every 4 to 8 weeks. Adalimumab was administered subcutaneously at a dose of 40 mg every 2 weeks with or without a loading dose of 80 mg.
Meta-analysis and small-study effects
Complete remission of inflammation
Complete remission of inflammation was defined as the absence of active uveitis (grade 0 for vitreous haze and anterior chamber cells) for more than 6 months. Complete remission of inflammation after infliximab therapy at 1 year or at the last evaluation was achieved in 161 (37.5%) patients from 5 studies with 429 patients, and 151 of 381 (39.6%) patients achieved complete remission of inflammation in the pooled cohort of adalimumab. As shown in Fig. 2, there was little heterogeneity (I 2 = 29%, P = 0.23). The pooled complete remission of inflammation between these two groups was not significantly different (P = 0.37).
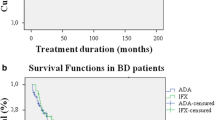
Response to therapy
The term “response to therapy” encompasses both complete and partial remission of inflammation in anti-TNF therapy. Two studies were excluded from the efficacy analysis of response to therapy, as Kunimi, et al. [21] assessed efficacy by mean change in visual acuity and Fabiani, et al. [19] assessed efficacy by mean change in best corrected visual acuity, rather than response rate. Additionally, Rio, et al.’ study [16] was dropped because they didn’t report the response to infliximab and adalimumab therapy separately. As a result, four studies reported response to anti-TNF therapy involving 449 patients, of whom 241/272 (88.6%) treated with infliximab and 153/177 (86.4%) treated with adalimumab achieved partial or complete remission of inflammation. No significant difference was observed between the two cohorts in terms of response to therapy (P = 0.86). Figure 3 illustrates that there was no significant heterogeneity (I2 = 31%, P = 0.23).
Corticosteroid-sparing effect
Corticosteroid-sparing effect was defined as a reduction in the daily corticosteroid dose required from the start of treatment with biological agents to the last assessment in the treatment of NIU. A total of 656 patients from 3 studies were adopted to compare infliximab with adalimumab in terms of corticosteroid- sparing effect. All the available data extracted from the original articles were converted and expressed as mean ± standard deviation (SD) using formulas [13, 25]. The mean daily corticosteroid dose at the end of the follow-up was pooled. (The studies by Leclercq, et al. and Maalouf, et al. were at six months; the study by Mateo, et al. was at one year.) There were no significant differences between infliximab and adalimumab as far as corticosteroid-sparing effect (P = 0.58) and heterogeneity (I 2 = 6%, P = 0.34) are concerned (Fig. 4).
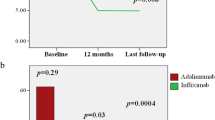
Adverse events
All 11 included studies consisting of 1459 patients were systematically reviewed for adverse events. Of these, 240 (16.45%) cases had adverse events that were adjudicated by the reviewers or the original authors. The meta-analysis data showed that there was a significant heterogeneity (I 2 = 61%, P = 0.005), so a random-effects model was chosen. There was no statistically significant difference in the incidence of adverse events between the two groups (OR = 1.35, 95% CI: 0.79 to 2.31, P = 0.27) (Fig. 5). We then performed a sensitivity analysis for adverse events. The heterogeneity (I 2 = 17%, P = 0.29) and pooled effect size (P = 0.001) showed statistically significant changes, with the incidence of adverse events being 17.91% for infliximab and 12.12% for adalimumab when we omitted the data from Kunimi, et al. [21] (Fig. 6), but not changing much when we omitted others.
Small-study effects
We assessed the small-study effects using a funnel plot of adverse events. According to the basically symmetrical funnel plot, no significant small-study effects were found which was corroborated by the results of Egger’s test (P = 0.846) (Fig. 7).
Discussion
TNF-α is a pro-inflammatory cytokine produced by many cell types including almost all cells of the immune system and can bind to pigment epithelial cells of the retina, ciliary body and iris, leading to breakdown of the blood-ocular barrier. Under physiological conditions, serum levels of TNF-α are undetectable, but levels increase significantly in the aqueous humor and serum following an inflammatory stimulus such as NIU. The anti-TNF-α biologics infliximab and adalimumab can substantially neutralize TNF-α and markedly suppress ocular inflammation. To date, several meta-analyses have been published focusing mainly on the overall efficacy and safety of anti- TNF-α agents, but none of them compared the efficacy and safety between these agents. In the current meta-analysis, we collected all the available evidence on the use of infliximab and adalimumab in the same trial to evaluate their efficacy and safety in the treatment of NIU.
The pooled incidence rates of complete remission of inflammation in the infliximab and adalimumab groups were 37.5% and 39.6%, respectively, and of response to therapy (complete and partial remission of inflammation) were 88.6% and 86.4%, respectively. These data indicate that both infliximab and adalimumab can substantially suppress the inflammation but completely reduce inflammation only in partial patients (less than 50% of NIU patients). In addition, they were shown to have similar benefits for responders in terms of complete remission of inflammation (P = 0.37) and response to therapy (P = 0.86). The response to therapy appears to be higher than that in other meta-analyses where the proportions of inflammation remission were 68% with anti-TNF-α therapy in the review published by Hu, et al. [26] and 79% in another study [27] focusing on adalimumab. One possible reason is that we extracted the complete remission from response to therapy. If a study with only complete remission is pooled with other studies with response to therapy, there will be a relatively lower rate of inflammatory remission. Another reason may be that we included children with NIU in this study. Children with NIU have a lower prevalence of severe complications [28], and have a higher response rate which has been supported by two reviews [29, 30]. One study [29] summarized the literature spanned from Jan 2000 to Oct 2012 with the proportion of responding children being 87% for adalimumab and with no significant difference from infliximab (72%), while another [30] focusing on NIU children collected the literature spanned from Nov 2012 to Jan 2020 with the proportion of responders being 86% for adalimumab and with a significant difference from infliximab (68%). However, there was no such a significant difference between infliximab and adalimumab in the current study, which may be due to the inclusion of both adults and children with NIU.
We also evaluated the corticosteroid-sparing effect according to the currently available studies. Most studies reported the daily corticosteroid dosage with median and interquartile range, so we converted the data to mean ± SD according to the aforementioned literature [13, 25]. The mean dosages at the last follow-up were recorded and calculated. The pooled meta-analysis demonstrated that infliximab and adalimumab have similar corticosteroid-sparing effect (P = 0.58). Before drawing a firm conclusion from this result, one caveat must be noted. Although the formulas are scientific, the process of conversion inevitably introduces errors. We did not analyze the mean daily dose of corticosteroid reduction from the initial visit to the last follow-up. Because multiple conversions would amplify the errors and lead to no meaningful results. We also did not categorize the corticosteroid-sparing effect into corticosteroid-suspended and corticosteroid-tapered subtypes because of the limited number of studies reporting details.
The safety of anti-TNF-a is an aspect that cannot be neglected. We reviewed all the 11 included studies and analyzed the results for adverse events. The pooled results showed that 16.45% of the cases experienced at least one adverse event. A sensitivity analysis was performed because a significant heterogeneity (I 2 = 61%, P = 0.005) was identified during the process of analysis. Ultimately, we found that the study published by Kunimi, et al. [21] contributed to the heterogeneity. After careful examination of this study, the possible reason is that they included more infusion/injection reactions in the adverse events. 11 of 12 patients (91.7%) in the infliximab group and 22 of 26 patients (84.6%) in the adalimumab group had infusion/injection reactions. After exclusion of this study, adalimumab seems to be in advantage over infliximab in terms of adverse events (P = 0.001). The advantage appears to be marginal. Because there was no significant difference (P = 0.27) with all these studies using a random-effects model. The results should therefore be interpreted with caution.
With regard to individuals, particular attention should be paid to elderly patients. As anti-TNF-α agents have the potential to increase the risk of serious infections such as bacteremia, pneumonia, tuberculosis [31,32,33]. The use of anti-TNF-α agents is not recommended by the New York Heart Association (NYHA) for patients with class III and IV heart failure [34]. In addition, an increased incidence of melanoma and lymphoma has been observed in patients taking anti-TNF-α agents [16, 17, 20, 24]. These rare but fatal adverse events call for vigilance during follow-up period. Regarding treatment costs, the annual cost of infliximab (15,799 Euro) is slightly higher than that of adalimumab (12,731 Euro) in the following strategy: Infliximab was administered intravenously with a loading dose of 5 mg/kg at 0, 2, 6 weeks, and continued every 8 weeks. Adalimumab was administered subcutaneously at a dose of 40 mg every 2 weeks [18].
Limitations
Most studies with 1 year of follow-up are not sufficient to comprehensively and precisely evaluate the efficacy and safety of infliximab and adalimumab. This is because infliximab has been observed to be effective in the short-term, and its efficacy seems to wane over time in children with NIU [35, 36]. As a consequence, higher doses of infliximab have been used to treat NIU in long-term follow-up [37, 38]. None of these included studies is a randomized controlled trial (RCT), which is another limitation of this meta-analysis. Hence, additional RCTs with a longer follow-up are warranted.
Conclusion
Our systematic review and meta-analysis of 11 studies suggests that infliximab and adalimumab have similar therapeutic efficacy and corticosteroid-sparing effect in patients with NIU. However, adalimumab has a marginal advantage over infliximab in terms of adverse events. Large-scale RCTs with a longer follow-up are required to further evaluate these two anti-TNF-α agents in patients with NIU.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Jaffe GJ, Dick AD, Brézin AP, Nguyen QD, Thorne JE, Kestelyn P, Barisani-Asenbauer T, Franco P, Heiligenhaus A, Scales D, et al. Adalimumab in patients with active noninfectious uveitis. N Engl J Med. 2016;375(10):932–43.
Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California epidemiology of Uveitis Study. Ophthalmology. 2004;111(3):491–500. discussion 500.
Durrani OM, Tehrani NN, Marr JE, Moradi P, Stavrou P, Murray PI. Degree, duration, and causes of visual loss in uveitis. Br J Ophthalmol. 2004;88(9):1159–62.
Rajan RS, Mohamed SO, Salowi MA. Demography and clinical pattern of newly diagnosed uveitis patients in Malaysia. J Ophthalmic Inflamm Infect. 2022;12(1):28.
Yalçındağ FN, Özdal P, Özyazgan Y, Batıoğlu F, Tugal-Tutkun I. Pediatric Uveitis in Turkey: the National Registry Report II. Ocul Immunol Inflamm 2022:1–7.
Cordero-Coma M, Sobrin L. Anti-tumor necrosis factor-α therapy in uveitis. Surv Ophthalmol. 2015;60(6):575–89.
Sen HN, Vitale S, Gangaputra SS, Nussenblatt RB, Liesegang TL, Levy-Clarke GA, Rosenbaum JT, Suhler EB, Thorne JE, Foster CS, et al. Periocular corticosteroid injections in uveitis: effects and complications. Ophthalmology. 2014;121(11):2275–86.
Khera TK, Dick AD, Nicholson LB. Mechanisms of TNFα regulation in uveitis: focus on RNA-binding proteins. Prog Retin Eye Res. 2010;29(6):610–21.
Suhler EB, Lowder CY, Goldstein DA, Giles T, Lauer AK, Kurz PA, Pasadhika S, Lee ST, de Saint Sardos A, Butler NJ, et al. Adalimumab therapy for refractory uveitis: results of a multicentre, open-label, prospective trial. Br J Ophthalmol. 2013;97(4):481–6.
Tracey D, Klareskog L, Sasso EH, Salfeld JG, Tak PP. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther. 2008;117(2):244–79.
Nguyen QD, Merrill PT, Jaffe GJ, Dick AD, Kurup SK, Sheppard J, Schlaen A, Pavesio C, Cimino L, Van Calster J, et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): a multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet. 2016;388(10050):1183–92.
Smetana GW, Umscheid CA, Chang S, Matchar DB. Methods guide for authors of systematic reviews of medical tests: a collaboration between the Agency for Healthcare Research and Quality (AHRQ) and the Journal of General Internal Medicine. J Gen Intern Med. 2012;27(Suppl 1Suppl 1):1–3.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Simonini G, Taddio A, Cattalini M, Caputo R, De Libero C, Naviglio S, Bresci C, Lorusso M, Lepore L, Cimaz R. Prevention of flare recurrences in childhood-refractory chronic uveitis: an open-label comparative study of adalimumab versus infliximab. Arthritis Care Res (Hoboken). 2011;63(4):612–8.
Zannin ME, Birolo C, Gerloni VM, Miserocchi E, Pontikaki I, Paroli MP, Bracaglia C, Shardlow A, Parentin F, Cimaz R, et al. Safety and efficacy of infliximab and adalimumab for refractory uveitis in juvenile idiopathic arthritis: 1-year followup data from the Italian Registry. J Rheumatol. 2013;40(1):74–9.
Calvo-Río V, Blanco R, Beltrán E, Sánchez-Bursón J, Mesquida M, Adán A, Hernandez MV, Hernandez Garfella M, Valls Pascual E, Martínez-Costa L, et al. Anti-TNF-α therapy in patients with refractory uveitis due to Behçet's disease: a 1-year follow-up study of 124 patients. Rheumatol (Oxford). 2014;53(12):2223–31.
Vallet H, Riviere S, Sanna A, Deroux A, Moulis G, Addimanda O, Salvarani C, Lambert M, Bielefeld P, Seve P, et al. Efficacy of anti-TNF alpha in severe and/or refractory Behçet’s disease: Multicenter study of 124 patients. J Autoimmun. 2015;62:67–74.
Vallet H, Seve P, Biard L, Baptiste Fraison J, Bielefeld P, Perard L, Bienvenu B, Abad S, Rigolet A, Deroux A, et al. Infliximab Versus Adalimumab in the treatment of refractory inflammatory uveitis: a Multicenter Study from the french Uveitis Network. Arthritis Rheumatol. 2016;68(6):1522–30.
Fabiani C, Vitale A, Rigante D, Emmi G, Bitossi A, Lopalco G, Sota J, Guerriero S, Orlando I, Gentileschi S, et al. Comparative efficacy between adalimumab and infliximab in the treatment of non-infectious intermediate uveitis, posterior uveitis, and panuveitis: a retrospective observational study of 107 patients. Clin Rheumatol. 2019;38(2):407–15.
Atienza-Mateo B, Martín-Varillas JL, Calvo-Río V, Demetrio-Pablo R, Beltrán E, Sánchez-Bursón J, Mesquida M, Adan A, Hernández MV, Hernández-Garfella M, et al. Comparative study of Infliximab Versus Adalimumab in Refractory Uveitis due to Behçet’s Disease: National Multicenter Study of 177 cases. Arthritis Rheumatol. 2019;71(12):2081–9.
Kunimi K, Usui Y, Asakage M, Maehara C, Tsubota K, Mitsuhashi R, Umazume A, Kezuka T, Sakai JI, Goto H. Anti-TNF-α therapy for refractory Uveitis Associated with Behçet’s syndrome and sarcoidosis: a single Center Study of 131 patients. Ocul Immunol Inflamm. 2022;30(1):223–30.
Ucan Gunduz G, Yalcinbayir O, Cekic S, Yildiz M, Kilic SS. Anti-tumor necrosis factor treatment in the management of Pediatric Noninfectious Uveitis: Infliximab Versus Adalimumab. J Ocul Pharmacol Ther. 2021;37(4):236–40.
Leclercq M, Andrillon A, Maalouf G, Sève P, Bielefeld P, Gueudry J, Sené T, Moulinet T, Rouvière B, Sène D, et al. Anti-Tumor Necrosis Factor α versus Tocilizumab in the Treatment of Refractory Uveitic Macular Edema: A Multicenter Study from the French Uveitis Network. Ophthalmol. 2022;129(5):520–9.
Maalouf G, Andrillon A, Leclercq M, Sève P, Bielefeld P, Gueudry J, Sené T, Titah C, Moulinet T, Rouvière B, et al. Lower Relapses Rate with Infliximab Versus Adalimumab in Sight-Threatening Uveitis: a Multicenter Study of 330 patients. Am J Ophthalmol. 2022;238:173–80.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27(6):1785–805.
Hu Y, Huang Z, Yang S, Chen X, Su W, Liang D. Effectiveness and safety of Anti-Tumor Necrosis factor-alpha Agents Treatment in Behcets’ Disease-Associated Uveitis: a systematic review and Meta-analysis. Front Pharmacol. 2020;11:941.
Ming S, Xie K, He H, Li Y, Lei B. Efficacy and safety of adalimumab in the treatment of non-infectious uveitis: a meta-analysis and systematic review. Drug Des Devel Ther. 2018;12:2005–16.
Treudler R, Orfanos CE, Zouboulis CC. Twenty-eight cases of juvenile-onset Adamantiades-Behçet disease in Germany. Dermatology. 1999;199(1):15–9.
Simonini G, Druce K, Cimaz R, Macfarlane GJ, Jones GT. Current evidence of anti-tumor necrosis factor α treatment efficacy in childhood chronic uveitis: a systematic review and meta-analysis approach of individual drugs. Arthritis Care Res (Hoboken). 2014;66(7):1073–84.
Maccora I, Fusco E, Marrani E, Ramanan AV, Simonini G. Changing evidence over time: updated meta-analysis regarding anti-TNF efficacy in childhood chronic uveitis. Rheumatology (Oxford). 2021;60(2):568–87.
Askling J, Fored CM, Brandt L, Baecklund E, Bertilsson L, Feltelius N, Cöster L, Geborek P, Jacobsson LT, Lindblad S, et al. Time-dependent increase in risk of hospitalisation with infection among swedish RA patients treated with TNF antagonists. Ann Rheum Dis. 2007;66(10):1339–44.
Bongartz T, Sutton AJ, Sweeting MJ, Buchan I, Matteson EL, Montori V. Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA. 2006;295(19):2275–85.
Wood KL, Hage CA, Knox KS, Kleiman MB, Sannuti A, Day RB, Wheat LJ, Twigg HL. 3rd: histoplasmosis after treatment with anti-tumor necrosis factor-alpha therapy. Am J Respir Crit Care Med. 2003;167(9):1279–82.
Danila MI, Patkar NM, Curtis JR, Saag KG, Teng GG. Biologics and heart failure in rheumatoid arthritis: are we any wiser? Curr Opin Rheumatol. 2008;20(3):327–33.
Simonini G, Zannin ME, Caputo R, Falcini F, de Martino M, Zulian F, Cimaz R. Loss of efficacy during long-term infliximab therapy for sight-threatening childhood uveitis. Rheumatology (Oxford). 2008;47(10):1510–4.
Tugal-Tutkun I, Ayranci O, Kasapcopur O, Kir N. Retrospective analysis of children with uveitis treated with infliximab. J aapos. 2008;12(6):611–3.
Rajaraman RT, Kimura Y, Li S, Haines K, Chu DS. Retrospective case review of pediatric patients with uveitis treated with infliximab. Ophthalmology. 2006;113(2):308–14.
Ardoin SP, Kredich D, Rabinovich E, Schanberg LE, Jaffe GJ. Infliximab to treat chronic noninfectious uveitis in children: retrospective case series with long-term follow-up. Am J Ophthalmol. 2007;144(6):844–9.
Acknowledgements
The authors would like to thank the Shaanxi Administration of Traditional Chinese Medicine.
Funding
This work was supported by the Shaanxi Administration of Traditional Chinese Medicine [Grant Numbers 2021-03-ZZ-006].
Author information
Authors and Affiliations
Contributions
Conceptualization: Lieling Kou.Data curation: Dan Bai, Weishai Liu.Formal analysis: Weishai Liu.Software: Weishai Liu.Supervision: Lieling Kou.Validation: Lieling Kou.Writing – original draft: Weishai Liu, Dan BaiWriting – review & editing: Weishai Liu, Lieling KouWeishai Liu and Dan Bai contributed equally to this paper. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors certify that they have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, W., Bai, D. & Kou, L. Comparison of infliximab with adalimumab for the treatment of non-infectious uveitis: a systematic review and meta-analysis. BMC Ophthalmol 23, 240 (2023). https://doi.org/10.1186/s12886-023-02987-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-02987-1