Abstract
Background
Retinitis Pigmentosa (RP) is a clinically and genetically progressive retinal dystrophy associated with severe visual impairments and sometimes blindness, the most common syndromic form of which is Usher syndrome (USH). This study aimed to further increase understanding of the spectrum of RP in the Khyber Pakhtunkhwa region of Pakistan.
Methodology
Four consanguineous families of Pashtun ethnic group were investigated which were referred by the local collaborating ophthalmologists. In total 42 individuals in four families were recruited and investigated using whole exome and dideoxy sequencing. Among them, 20 were affected individuals including 6 in both family 1 and 2, 5 in family 3 and 3 in family 4.
Result
Pathogenic gene variants were identified in all four families, including two in cone dystrophy and RP genes in the same family (PDE6C; c.480delG, p.Asn161ThrfsTer33 and TULP1; c.238 C > T, p.Gln80Ter) with double-homozygous individuals presenting with more severe disease. Other pathogenic variants were identified in MERTK (c.2194C > T, p.Arg732Ter), RHO (c.448G > A, p.Glu150Lys) associated with non-syndromic RP, and MYO7A (c.487G > A, p.Gly163Arg) associated with USH. In addition, the reported variants were of clinical significance as the PDE6C variant was detected novel, whereas TULP1, MERTK, and MYO7A variants were detected rare and first time found segregating with retinal dystrophies in Pakistani consanguineous families.
Conclusions
This study increases knowledge of the genetic basis of retinal dystrophies in families from Pakistan providing information important for genetic testing and diagnostic provision particularly from the Khyber Pakhtunkhwa region.
Similar content being viewed by others
Introduction
Retinitis pigmentosa (RP) is an inherited retinal dystrophy, affecting 1 in 4000 individuals [1]. RP is caused by the progressive degeneration of photoreceptors cells in the retina and characterized by absence or scarcity of retinal pigment deposits visible on fundus examination. Initially, degeneration of rod photoreceptors results in night blindness and then progressive loss of peripheral vision leads to tunnel vision. Disease progression results in decreased visual acuity due to cone photoreceptors degeneration that eventually leads to complete blindness [2]. It is generally considered that about 70-80% of all RP cases are non-syndromic, where eyes are exclusively affected [3]. However, the most common syndromic form of RP is Usher syndrome (USH), characterized by sensorineural hearing loss, RP, and, in some cases, vestibular dysfunction [4]. USH is the most frequent cause of deaf-blindness and affects more than 50% of both deaf and blind individuals in different populations [5]. Importantly, the age of onset, severity of symptoms and disease progression of both RP and USH may vary widely among patients, even within the same family [6,7,8,9].
RP manifests almost all patterns of inheritance, that is an autosomal dominant, autosomal recessive, X-linked, including rare non-Mendelian forms such as mitochondrial or digenic inheritance patterns [10, 11]. About 60% of RP cases are inherited in autosomal recessive manner [6]. In addition, the USH represents about 10–30% of all autosomal recessive RP (arRP) cases [5]. Although, RP shows no ethnic specificity, however, the autosomal recessive forms of RP have been more frequently reported in Chinese, Israeli, Saudi, Turkey, south Indian and Pakistani populations which are geographically isolated and display relatively high consanguinity rates [12,13,14,15,16]. Importantly, studying patients with phenotypes of recessively inherited diseases like RP and USH in geographically isolated and highly consanguineous populations may be useful to identify disease causal mutations [17].
RP has great phenotypic and genetic heterogeneity due to many associated genetic defects, each of which has numerous alleles and corresponds to a gene or locus-specific phenotype [16]. Over 130 genes have been found to be associated with RP (http://www.sph.uth.tmc.edu/RetNet), including approximately 90 genes for non-syndromic RP and about 40 genes for syndromic forms [18]. Genes commonly reported to cause RP include ABCA4 (MIM #601691), CRB1 (MIM #604210), CDHR1 (MIM #609502), PDE6A (MIM #180071), PDE6B (MIM #180072), RHO (MIM #180380), RP1 (MIM #603937), SPATA7 (MIM #609868), EYS (MIM #612424), RP1L1 (MIM #608581), TULP1 (MIM #602280), and USH2A (MIM #608400). Similarly, the commonly reported USH causative genes are MYO7A (MIM #276903), USH2A (MIM #608400), CDH23 (MIM #605516), CLRN1 (MIM #606397), PCDH15 (MIM #605514), USH1G (MIM #606943), and CIB2 (MIM #605564). In general, MYO7A is the most frequent cause of USH type1 accounting for approximately 50% of cases [19, 20]. Although, studies have reported variants in CRB1, PDE6A, PDE6B, RP1, TULP1, CLRN1, MERTK and CNGA1 causing non-syndromic RP and MYO7A, USH2A, CDH23, USH1H, PCDH15 genes are responsible for USH phenotypes in families of Pakistani origin [8, 21,22,23,24,25,26,27,28]. Among these genes, the most causative USH genes are MYO7A and CDH23 having relative abundance of 42.9% and 28.6% respectively [22]. There are many Pakistani families with non-syndromic RP and USH phenotypes, however, the underlying genetic cause remains undetermined.
In Pakistan, geographical constraints and marriage patterns within communities may give rise to genetic isolates in which an increased frequency of certain disease-associated founder variants may occur [29,30,31,32]. Knowledge of the specific spectrum and frequency of disease-associated gene variants within different regions is fundamental to the development of effective and more tailored diagnostic genetic testing strategies, targeting variants relevant to a particular population. As part of an ongoing international collaborations, we are conducting genomic studies to define the likely specific molecular cause of disease in a group of families from Pakistan with a preliminary clinical diagnosis of retinal dystrophies. In current study, four consanguineous Pakistani families were analyzed to elucidate the genetic basis of non-syndromic RP and USH.
Methodology
Subjects
The current study was approved by the Ethical Committee and Advanced Studies and Research Board (ASRB), KUST, Pakistan. Families with a preliminary clinical diagnosis of non-syndromic RP and USH were referred for the genetic analysis by the collaborating local ophthalmologists between September, 2021 and March, 2022 in Khyber Pakhtunkhwa region of Pakistan. Three families had non-syndromic RP and one family had USH phenotypes. The study was conducted in accordance with the Declaration of Helsinki, informed written consent was obtained from the participating members of the families and from the parents of minor children. Family histories and demographic characteristics of the investigated families were recorded, and pedigrees were drawn. All the families practice consanguineous marriages (Table 1). Disease associated features of probands and other affected individuals in families were documented. Blood samples were collected from affected and normal members of the families.
Genetic analysis
Genomic DNA was extracted from the blood samples via the ReliaPrep™ kit (Blood gDNA Miniprep System, Promega) and MagMAX DNA Multi-Sample Ultra 2.0 Kit using automated system KingFisher Apex (thermos scientific) and standard Phenol-Chloroform method. Whole exome sequencing (WES) was performed on the probands’ genomic DNA (III:1 in family-1, III:4 in family-2, III:1 in family-3 and II:6 in family-4) to find putative pathogenic variants. Coding regions were captured with HiSeq 4000 instrument (Illumina) with an average coverage of 100–120X at each nucleotide position and Twist human core exome kit (Twist Bioscience) through CeGat GmbH (Tübingen, Germany). Novoalign software (V3.08.00; Novocraft Technologies) was used to align the captured reads to reference human genome (build hg19). Picard version 2.140 SNAPSHOT used to remove duplicate reads. Genome analysis toolkit GATK (v3.8) was used for single base quality score and recalibration. Copy number variant (CNV) was detected with Exome Depth (v2.1). Happlotype Caller was used to generate Variant Call Format (VCF) file contain all genes variants [33]. AutoMap was used for homozygosity mapping [34]. Allele frequencies were detected using gnomAD database (https://gnomad.broadinstitute.org/), and conservation of variants was performed by using GERP [35]. Sanger sequencing was performed to likely pathogenic variant in all the recruited individuals. Single nucleotide polymorphisms (SNPs) were filtered-out, if present in the 1000 Genomes Project (www.1000genomes.org) or the Single Nucleotide Polymorphism Database (dbSNP; NCBI) to select the candidate genes. The variant-specific primers were designed using online available primer3 plus tool (https://www.primer3plus) to find the segregation of disease-causing variants in the family members. The DNA samples were amplified using standard PCR programing and protocols. The amplified products were sequenced by Source BioScience LifeSciences (https://www.sourcebioscience.com/) and Microsynth AG (https://www.microsynth.com). The segregating genetic variants were analyzed using SIFT (https://sift.edu.sg) and Mutation Taster (www.mutationtaster.org) to predict the impact of the sequence variations on encoded proteins’ function. The protein-protein interaction data was assembled from KEGG pathways (https://www.kegg/pathway) and String (https://string-db.org/) databases. In addition, the Varsome (https://varsome.com) online tool was used for variants classification according to the American College of Medical Genetics and Genomics (ACMG).
To compare and correlate the segregating genetic variants with phenotype, all reported variants were retrieved from HGMD (http://www.hgmd), OMIM (https://www.omim), PubMed (https://www.pubmed), ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/) databases.
Result
Families description
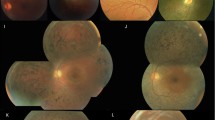
In the present study, 4 consanguineous families were analyzed from different regions of Khyber Pakhtunkhwa (Table 1). In total 42 individuals in four families were investigated, among them 20 were affected individuals including 6 in both family 1 and 2, 5 in family 3 and 3 in family 4. Three families (Family 2, 3 and 4) with non-syndromic RP had initial symptom of night blindness with variable age of onset whereas a family (Family 1) with USH phenotypes had profound congenital deafness, balance problems and age of onset of RP was in adolescence. Furthermore, maculopathy was observed in affected individuals of a family with RP (Family 2). In addition, nystagmus, cone dystrophy and complete blindness at the age of 20 year were observed in affected individuals of a family with RP (Family 3). In the same family, some affected members had mild symptoms of RP. The clinical signs observed on fundus of probands and affected individuals with retinal dystrophies are summarized in Table 1. Pedigrees analysis showed that all the recruited families had autosomal recessive pattern of disease inheritance due to consanguineous marriages.
Genetic findings
Likely causative genetic variants were identified in all the four families (Family-1, 2, 3 and 4) (Table 2).
A rare homozygous missense variant NM_000260.3:c.487G > A in exon 6 in the MYO7A gene was found segregating in family1 with USH phenotype. The MYO7A missense variant leads to the substitution of glycine with arginine at evolutionary conserved position at 163 (p.Gly163Arg) in protein. A rare homozygous missense variant NM_006343.3:c.2194 C > T in exon 17 in the MERTK gene was identified in family2 affected members who had both RP and maculopathy phenotypes. The MERTK variant is predicted to result in a premature stop codon (p.Arg732Ter) and expression of the aberrant transcript harboring truncating variant and its degradation by nonsense-mediated mRNA decay (NMD) has been predicted by in silico tools.
A novel PDE6C frameshift deletion variant NM_006204.4:c.480delG in exon 1 and a rare TULP1 nonsense variant NM_003322.6:c.238 C > T in exon 4, were observed to segregate with progressive cone dystrophy and non-syndromic RP respectively in family 3. Notably, nystagmus and complete blindness at the age of 20 years were found additional features in an individual who was detected homozygous for both PDE6C and TULP1 mutant alleles. However, mild features of RP were observed in some individuals of the same family who were detected homozygous for only TULP1 variant alleles and cone dystrophy was observed in an individual who was carrying only PDE6C variant alleles in homozygous state (Table 1). The PDE6C deletion variant (c.480delG) result in a frameshift followed by a premature stop codon (p.Asn161ThrfsTer33) whereas TULP1 missense variant (c.238 C > T) also introduces a premature stop codon (p.Gln80Ter). The PDE6C variant c.480delG results in deletion of the last nucleotide in exon 1 therefore, some of the in-silico tools suggested that the variant (c.480delG) may result in broken wild type donor splice site (c.480 + 1delG) (Human Splicing Finder and Mutation Taster). However, a gain of splice donor site is also predicted by SpliceAI at 480 position suggesting normal splicing (Fig. 1c). In-silico analysis further revealed that the RNA transcripts with PDE6C and TULP1 truncating variants are degraded by NMD.
A homozygous missense variant NM_000539.3:c.448G > A in exon 2 in the RHO gene was found segregating with non-syndromic RP phenotype in family4. The missense RHO variant (c.448G > A) leads to the substitution of glutamic acid with lysine at evolutionary conserved position 150 (p.Glu150Lys) in protein. Importantly, the identified TULP1, MERTK and MYO7A variants were first time found segregating with non-syndromic RP and USH phenotypes in Pakistani families. Interestingly, the segregation data revealed that among the 22 participating clinically normal members in the investigated families in which genotype-phenotype correlations were established, 20 (90.90%) individuals were detected carriers for a single variant allele and about 7 (31.8%) members in family 3 were detected carriers for two variant alleles.
Overall, the variant alleles were detected inside the long homozygous contigs exceeding 11 Mb in size in probands of family1, 2 and 4 (Supplementary data Tables). The sizes of total homozygous contigs of the families having variant in MYO7A, MERTK and RHO were 243.38 Mb, 750.01 Mb and 244.18 Mb respectively (Fig. 1).
Families pedigrees and genetic findings: A. Pedigree of family 1 showing segregation of the identified variant in MYO7A gene, a. Homozygosity map of the proband (III:1), showing the runs of homozygosity as blue band. B. Pedigree of family 2 showing segregation of the identified variant in MERTK gene, b. Homozygosity map of the proband (III:4), showing the runs of homozygosity as blue band. C. Pedigree of family 3 showing segregation of the identified variants in TULP1 and PDE6C genes. c. Schematic representation of the pathogenic PDE6C mutation (c.480delG) on the protein sequence predicted by in-silico tools. D. Pedigree of family 4 showing segregation of the identified variant in RHO gene b. Homozygosity map of the proband (II:6), showing the runs of homozygosity as blue band
Discussion
Establishing molecular diagnosis in patients with RP is challenging in clinical practice due to the disease significant phenotypic and genetic heterogeneity [36]. Traditional approaches of individual gene screening are difficult, time consuming and don’t reveal the complete variant spectrum in RP patients. However, WES is currently the most efficient approach and widely used for identification of the molecular bases of heterogeneous genetic diseases [37]. In this study, causative variants in TULP1, PDE6C, RHO, MERTK and MYO7A genes were identified in all the 4 Pakistani families displayed either non-syndromic RP or USH phenotypes using WES approach. Studies have previously reported variants in CRB1, PDE6A, PDE6B, RP1, TULP1, CLRN1, MERTK and CNGA1 causing non-syndromic RP and variants in MYO7A, USH2A, CDH23, USH1H, PCDH15 genes causing USH in families of Pakistani origin [8, 21,22,23,24,25,26,27,28]. Importantly, delineating genetic basis of RP and USH in this study and in previous studies provides essential information for molecular diagnosis as well as for genetic counselling of extended families in order to reduce burden of these diseases in Pakistani population.
In family1 with USH phenotype, a rare homozygous missense variant (c.487G > A) in the MYO7A was found segregating with USH type 1 (USH1) phenotype, more specifically USH type IB (USH1B). This variant was first time reported by Sloan-Heggen et al. [38] in an affected individual with USH1 phenotype, later on this variant in compound heterozygous state was found to cause USH1 in an Algerian family [39], whereas, in homozygous state this variant caused non-syndromic hearing loss in a Turkish consanguineous family [40]. The findings of present and previous studies confirm that MYO7A is expressed in the retina and inner ear, thus variants in MYO7A are known to cause diseases affecting the retina and ear. MYO7A encodes myosin VIIA protein, a 2215 amino acids long protein in these organs where it acts on the transport processes through the cilia of the retinal photoreceptors or interacts with multiple proteins actin, harmonin, Sans, CDH23, and PCDH15 in stereocilia hair cells of the inner ear to form mechano-transduction complex, which is crucial for sound detection [41]. In the Human Gene Mutation Database (HGMD), more than 662 MYO7A variants have been listed till date that most commonly cause USH phenotypes. Among them, the variants such as p.Arg212Cys, p.Arg212His, p.Arg302His, p.Arg666Ter and p.Gln821Ter most frequently cause USH1 [42, 43]. In families of Pakistani origin, about 6.25% MYO7A variants have been reported to most likely cause congenital deafness and few variants cause USH1 [44]. The current study provides evidence of association of MYO7A variants with USH1. In addition, the reported high frequency of MYO7A variants causing congenital deafness in Pakistani population could be due to RP usual onset in adolescence and lack of clinical diagnostics facilities to make a diagnosis of RP in Pakistan.
In family2, a rarely reported nonsense MERTK variant c.2194 C > T caused non-syndromic RP and maculopathy. This variant was previously only reported by O’Sullivan et al. [45] in an RP patient from a British cohort. The MERTK gene encodes MER tyrosine kinase receptor that plays crucial role in phagocytosis of retinal pigment epithelium (RPE) [46]. This receptor exhibits four functional domains, such as immunoglobulin-like, fibronectin-like, transmembrane-like, and tyrosine kinase-like domains [47]. The MERTK receptor in retina is involved in the RPE phagocytosis in the inner segment to re-new the photoreceptor outer segments [48]. TULP1, Gas6 and protein S are the ligands that binds to MERTK receptor and activates the receptor upon phosphorylation of its kinase domain, that in turn activates the down-cascade for the phagocytosis. Previously reported MERTK variants (p.Ser627Ter, p.Arg651Ter, p.Asp487LeufsTer57, p.Trp131Ter, p.Ile103AsnfsTer4) were found to disturb phagocytosis pathway in the photoreceptor cells and consequently cause RP in consanguineous families [49,50,51]. However, MERTK variants in compound heterozygous state have been reported to cause arRP in multiple siblings of a non-consanguineous family as well [52]. The MERTK truncating variant p.Arg732Ter detected in current study is a loss of function variant due to the degradation of expressed aberrant transcript by NMD [53] that may lead to retinal dystrophies.
In family3, a novel frameshift deletion PDE6C variant (c.480delG, p.Asn161thrfs*33) and a rare nonsense TULP1 variant (c. 238 C > T, p.Gln80Ter) independent segregated with progressive cone dystrophy and non-syndromic RP respectively. Importantly, the genotype-phenotype correlations have been established for both types of retinal dystrophies in this family. Sequence variants in PDE6C have been reported previously to cause autosomal recessive cone dystrophy [54,55,56]. In cone dystrophy, cone cells in retina are affected causing decrease in visual acuity and increased sensitivity to light. PDE6C protein is expressed in cone photoreceptors and plays important role in the rapid decrease of intracellular cGMP levels in the outer segment. Normally, PDE6C protein is known to be directly involved in phototransduction pathway inside cone cells (UniProtKB-P51160). In current study, the identified frameshift deletion (p.Asn161ThrfsTer33) in the PDE6C has been predicted as a loss of function variant due to the degradation of expressed aberrant transcript by NMD [53] that can cause progressive cone dystrophy. In addition, at same position another pathogenic missense variant (c.480G > T, p.Lys160Asn) reported in the ClinVar database (ClinVar; VCV001213877.1) causes Achromatopsia, a type of stationary cone dystrophy usually appears in childhood. This can be explained by the fact that the PDE6C variants identified in previous and present studies resulted in a change at an evolutionarily conserved position that severely affected protein’s function and consequently caused cone degeneration, a common feature in both stationary and progressive cone dystrophy.
Although, cone dystrophy associated PDE6C variant independently segregated from RP associated TULP1 variant in family 3, however, nystagmus and complete blindness at the age of 20 years were observed in family members who carried both PDE6C and TULP1 variants. In addition, mild features of RP were observed in individuals who were carried only TULP1 variant. Previously, TULP1 variants have commonly been found associated with non-syndromic RP [57, 58]. As the Tub Like protein 1 is expressed from TULP1 gene in the rod and cone photoreceptor cells in retina and is involved in development of photoreceptor synapses as well as rhodopsin transportation from its site of synthesis in the inner segment of photoreceptor cells through the connecting cilium to the outer segment [59]. Therefore, most of the identified TULP1 variants have been described to affect normal functions of the TULP1 protein in retinal cells and consequently cause RP. Moreover, association of TULP1 variants with arRP has already been established [24, 57, 58, 60,61,62] and it was estimated that TULP1 variants account for 2% of arRP cases [63]. The identification of causal variants in a Pakistani consanguineous family in present study reaffirmed the role of TULP1 in the pathogenesis of arRP.
In family4, a missense RHO variant (c.448G > A; p.Glu150Lys) was identified to cause non-syndromic RP phenotype. This variant has been previously reported in two unrelated consanguineous Pakistani families [64]. Identification of recurrent RHO variant (p.Glu150Lys) will aid in establishing its founder effect in population of Pakistan and should be suggestively screened in RP susceptible families for premarital counseling. Although, the RHO variants commonly cause adRP and rarely cause arRP [65,66,67,68], however, in both cases role of RHO is important for normal functions of rod cells in retina. RHO gene encodes rhodopsin, a light-detecting G-protein-coupled receptor that plays a vital role in phototransduction and rod photoreceptor cell health. Rhodopsin consists of four specialized domains: the cytoplasmic, intradiscal, ligand-binding, and transmembrane domains. Each domain assists in the maintenance of either the Rhodopsin proper structure and its trafficking through the cell or its vital role in the phototransduction. The cytoplasmic C-terminal domain of Rhodopsin is crucial in regulation of membrane trafficking and its interactions with other proteins in the phototransduction cascade [69, 70]. It has been elucidated that sequence variations in this domain lead to retinal degenerations such as adRP and arRP [71, 72]. The RHO variant (p.Glu150Lys) identified in current study lies in the cytoplasmic domain of Rhodopsin that affects its signaling activity as a G-protein-coupled receptor and consequential aberrant trafficking as well as initiation of retinal degeneration usually lead to RP.
The probands in investigated families were consanguineous offspring who have elevated levels of homozygosity. Autozygous stretches within their genome were detected which likely harbored loss of function variants and resulted in complete inactivation or dysfunction of genes. The identified MYO7A, MERTK and RHO variants in the current study lie within regions of homozygosity (41 Mb, 11 Mb and 62 Mb respectively). Therefore, in current study consanguinity and homozygosity were detected risk of arRP and USH in Pakistani families. In addition, majority (90.90%) of clinically normal members in the investigated families were detected carriers for a single variant allele and few individuals were detected carriers for two variant alleles in a family in which both PDE6C and TULP1 variants segregated independently. The high rate of carrier detection in investigated consanguineous families revealed that those individuals are at increased risk of transmitting the diseases to future generations.
Establishing the diagnosis for retinal dystrophies is quite challenging due to their high genetic heterogeneity and overlapping clinical presentations. These factors collectively make it extremely difficult to establish an accurate diagnosis based on clinical presentation alone in a country like Pakistan, where many families reside in highly remote rural regions and have limited access to primary healthcare as well as ophthalmic services. In addition, there is also limited availability of specific and expensive diagnostic investigations such as fundoscopy, electroretinography and optical coherence tomography that are required to assess ocular status in retinal dystrophies. It is worth mentioning here that application of modern genomic technologies enabled us to establish an accurate molecular diagnosis in investigated families with retinal dystrophies and has also facilitated informed genetic counselling.
In summary, the current study highlights the importance of next generation sequencing approach in finding the underlying genetic causes of RP and USH in Pakistani families. In addition, molecular genetic diagnosis was successfully established in all the four families. Unexpected genotype-phenotype correlations were identified in some families that confirmed association of RP with neurological and retinal defects. The current study provides substantial evidence that consanguinity and autozygosity increased risk for genetic diseases in our population. Furthermore, the carrier frequency for retinal dystrophies was found alarmingly high among phenotypically normal individuals in investigated Pakistani families.
Data Availability
The datasets generated and/or analyzed during the current study are available in the ClinVar repository, with the accession numbers i.e. SCV002599429, SCV002600101, SCV002600102, SCV002600103 and SCV002600104.
References
Verbakel SK, van Huet RA, Boon CJ, den Hollander AI, Collin RW, Klaver CC, et al. Non-syndromic retinitis pigmentosa. Progress in retinal and eye research. 2018;66:157–86.
Hamel C. Retinitis pigmentosa. Orphanet journal of rare diseases. 2006;1(1):1–12.
Ferrari S, Di Iorio E, Barbaro V, Ponzin D, S Sorrentino F, Parmeggiani F. Retinitis pigmentosa: genes and disease mechanisms. Current genomics. 2011;12(4):238–49.
Ahmed AN, Tahir R, Khan N, Ahmad M, Dawood M, Basit A, et al. USH2A gene variants cause Keratoconus and Usher syndrome phenotypes in pakistani families. BMC ophthalmology. 2021;21(1):191.
Millán JM, Aller E, Jaijo T, Blanco-Kelly F, Gimenez-Pardo A, Ayuso C. An update on the genetics of usher syndrome. Journal of ophthalmology. 2011;2011.
Hartong DT, Berson EL, Dryja TP. Retinitis pigmentosa. The Lancet. 2006;368(9549):1795–809.
Yan D, Liu XZ. Genetics and pathological mechanisms of Usher syndrome. Journal of human genetics. 2010;55(6):327–35.
Ahmed AN, Tahir R, Khan N, Ahmad M, Dawood M, Basit A, et al. USH2A gene variants cause Keratoconus and Usher syndrome phenotypes in pakistani families. BMC ophthalmology. 2021;21(1):1–8.
Bravo-Gil N, González-del Pozo M, Martín-Sánchez M, Méndez-Vidal C, Rodríguez-de La Rúa E, Borrego S, et al. Unravelling the genetic basis of simplex Retinitis Pigmentosa cases. Scientific reports. 2017;7(1):1–10.
Perea-Romero I, Gordo G, Iancu IF, Pozo-Valero D, Almoguera B, Blanco-Kelly F, et al. Genetic landscape of 6089 inherited retinal dystrophies affected cases in Spain and their therapeutic and extended epidemiological implications. Scientific reports. 2021;11(1):1–13.
Sharon D, Ben-Yosef T, Goldenberg‐Cohen N, Pras E, Gradstein L, Soudry S, et al. A nationwide genetic analysis of inherited retinal diseases in Israel as assessed by the israeli inherited retinal disease consortium (IIRDC). Human mutation. 2020;41(1):140–9.
Ergun MA, Citirik M, Bilgili G, Ergun SG, Polat G. A novel RP1 mutation demonstrated in a turkish family with autosomal recessive retinitis pigmentosa. Gene Reports. 2018;11:1–5.
Aldahmesh MA, Safieh LA, Alkuraya H, Al-Rajhi A, Shamseldin H, Hashem M, et al. Molecular characterization of retinitis pigmentosa in Saudi Arabia. Molecular vision. 2009;15:2464.
Sharon D, Banin E. Nonsyndromic retinitis pigmentosa is highly prevalent in the Jerusalem region with a high frequency of founder mutations. Molecular vision. 2015;21:783.
Zafar S, Ahmed K, Ali A, Baig R. Retinitis pigmentosa genes implicated in south asian populations: a systematic review. Journal of the Pakistan Medical Association. 2017;67(11):1734.
Gao F-J, Li J-K, Chen H, Hu F-Y, Zhang S-H, Qi Y-H, et al. Genetic and clinical findings in a large cohort of chinese patients with suspected retinitis pigmentosa. Ophthalmology. 2019;126(11):1549–56.
Erzurumluoglu AM, Shihab HA, Rodriguez S, Gaunt TR, Day IN. Importance of genetic studies in consanguineous populations for the characterization of novel human gene functions. Annals of human genetics. 2016;80(3):187–96.
Karali M, Testa F, Brunetti-Pierri R, Di Iorio V, Pizzo M, Melillo P, et al. Clinical and genetic analysis of a european cohort with pericentral retinitis pigmentosa. International journal of molecular sciences. 2019;21(1):86.
Toms M, Pagarkar W, Moosajee M. Usher syndrome: clinical features, molecular genetics and advancing therapeutics. Therapeutic advances in ophthalmology. 2020;12:2515841420952194.
Jaijo T, Aller E, Beneyto M, Najera C, Graziano C, Turchetti D, et al. MYO7A mutation screening in Usher syndrome type I patients from diverse origins. Journal of medical genetics. 2007;44(3):e71-e.
Ahmed ZM, Riazuddin S, Bernstein SL, Ahmed Z, Khan S, Griffith AJ, et al. Mutations of the protocadherin gene PCDH15 cause Usher syndrome type 1F. The American Journal of Human Genetics. 2001;69(1):25–34.
Ahmed Z, Riazuddin S, Riazuddin S, Wilcox E. The molecular genetics of Usher syndrome. Clinical genetics. 2003;63(6):431–44.
Khan MI, Kersten FF, Azam M, Collin RW, Hussain A, Shah ST-A, et al. CLRN1 mutations cause nonsyndromic retinitis pigmentosa. Ophthalmology. 2011;118(7):1444–8.
Ajmal M, Khan MI, Micheal S, Ahmed W, Shah A, Venselaar H, et al. Identification of recurrent and novel mutations in TULP1 in pakistani families with early-onset retinitis pigmentosa. Molecular vision. 2012;18:1226.
Zhang Q, Zulfiqar F, Riazuddin SA, Xiao X, Ahmad Z, Riazuddin S, et al. Autosomal recessive retinitis pigmentosa in a pakistani family mapped to CNGA1 with identification of a novel mutation. Mol Vis. 2004;10(884):9.
Shahzadi A, Riazuddin SA, Ali S, Li D, Khan SN, Husnain T, et al. Nonsense mutation in MERTK causes autosomal recessive retinitis pigmentosa in a consanguineous pakistani family. British journal of ophthalmology. 2010;94(8):1094–9.
Khaliq S, Abid A, Ismail M, Hameed A, Mohyuddin A, Lall P, et al. Novel association of RP1 gene mutations with autosomal recessive retinitis pigmentosa. Journal of medical genetics. 2005;42(5):436–8.
Ullah I, Kabir F, Gottsch CBS, Naeem MA, Guru AA, Ayyagari R, et al. Mutations in phosphodiesterase 6 identified in familial cases of retinitis pigmentosa. Human genome variation. 2016;3(1):1–4.
Khan MI, Azam M, Ajmal M, Collin RW, den Hollander AI, Cremers FP, et al. The molecular basis of retinal dystrophies in pakistan. Genes (Basel). 2014;5(1):176–95.
Maranhao B, Biswas P, Gottsch AD, Navani M, Naeem MA, Suk J, et al. Investigating the molecular basis of Retinal Degeneration in a familial cohort of pakistani decent by Exome sequencing. PLoS One. 2015;10(9):e0136561.
Li L, Chen Y, Jiao X, Jin C, Jiang D, Tanwar M, et al. Homozygosity mapping and genetic analysis of autosomal recessive Retinal Dystrophies in 144 consanguineous pakistani families. Invest Ophthalmol Vis Sci. 2017;58(4):2218–38.
Hussain R, Bittles AH. The prevalence and demographic characteristics of consanguineous marriages in Pakistan. J Biosoc Sci. 1998;30(2):261–75.
DePristo MA, Banks E, Poplin R, Garimella KV, Maguire JR, Hartl C, et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nature genetics. 2011;43(5):491–8.
Quinodoz M, Peter VG, Bedoni N, Royer Bertrand B, Cisarova K, Salmaninejad A, et al. AutoMap is a high performance homozygosity mapping tool using next-generation sequencing data. Nature communications. 2021;12(1):1–7.
Davydov EV, Goode DL, Sirota M, Cooper GM, Sidow A, Batzoglou S. Identifying a high fraction of the human genome to be under selective constraint using GERP++. PLoS computational biology. 2010;6(12):e1001025.
Sorrentino F, Gallenga C, Bonifazzi C, Perri P. A challenge to the striking genotypic heterogeneity of retinitis pigmentosa: a better understanding of the pathophysiology using the newest genetic strategies. Eye. 2016;30(12):1542–8.
Neveling K, Feenstra I, Gilissen C, Hoefsloot LH, Kamsteeg EJ, Mensenkamp AR, et al. A post-hoc comparison of the utility of S anger sequencing and exome sequencing for the diagnosis of heterogeneous Diseases. Human mutation. 2013;34(12):1721–6.
Sloan-Heggen CM, Bierer AO, Shearer AE, Kolbe DL, Nishimura CJ, Frees KL, et al. Comprehensive genetic testing in the clinical evaluation of 1119 patients with hearing loss. Human genetics. 2016;135(4):441–50.
Abdi S, Bahloul A, Behlouli A, Hardelin J-P, Makrelouf M, Boudjelida K, et al. Diversity of the genes implicated in algerian patients affected by Usher syndrome. PLoS One. 2016;11(9):e0161893.
Atik T, Onay H, Aykut A, Bademci G, Kirazli T, Tekin M, et al. Comprehensive analysis of deafness genes in families with autosomal recessive nonsyndromic hearing loss. PloS one. 2015;10(11):e0142154.
Zong L, Chen K, Wu X, Liu M, Jiang H. Compound heterozygous MYO7A mutations segregating Usher syndrome type 2 in a Han family. International Journal of Pediatric Otorhinolaryngology. 2016;90:150–5.
Ouyang XM, Yan D, Du LL, Hejtmancik JF, Jacobson SG, Nance WE, et al. Characterization of Usher syndrome type I gene mutations in an Usher syndrome patient population. Human genetics. 2005;116(4):292–9.
Nájera C, Beneyto M, Blanca J, Aller E, Fontcuberta A, Millán JM, et al. Mutations in myosin VIIA (MYO7A) and usherin (USH2A) in spanish patients with Usher syndrome types I and II, respectively. Human Mutation. 2002;20(1):76–7.
Shahzad M, Sivakumaran TA, Qaiser TA, Schultz JM, Hussain Z, Flanagan M, et al. Genetic analysis through OtoSeq of pakistani families segregating prelingual hearing loss. Otolaryngology–Head and Neck Surgery. 2013;149(3):478–87.
O’Sullivan J, Mullaney BG, Bhaskar SS, Dickerson JE, Hall G, O’Grady A, et al. A paradigm shift in the delivery of services for diagnosis of inherited retinal disease. Journal of medical genetics. 2012;49(5):322–6.
Ksantini M, Lafont E, Bocquet B, Meunier I, Hamel CP. Homozygous mutation in MERTK causes severe autosomal recessive retinitis pigmentosa. European journal of ophthalmology. 2012;22(4):647–53.
Tada A, Wada Y, Sato H, Itabashi T, Kawamura M, Tamai M, et al. Screening of the MERTK gene for mutations in japanese patients with autosomal recessive retinitis pigmentosa. Mol Vis. 2006;12:441–4.
Al-Khersan H, Shah KP, Jung SC, Rodriguez A, Madduri RK, Grassi MA. A novel MERTK mutation causing retinitis pigmentosa. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2017;255(8):1613–9.
Yang M, Li S, Liu W, Yang Y, Zhang L, Zhang S, et al. Targeted next-generation sequencing reveals a novel Frameshift mutation in the MERTK gene in a chinese family with retinitis pigmentosa. Genetic Testing and Molecular Biomarkers. 2018;22(3):165–9.
Liu S, Bi JG, Hu Y, Tang D, Li B, Zhu P, et al. Targeted next generation sequencing identified novel loss-of‐function mutations in MERTK gene in chinese patients with retinitis pigmentosa. Molecular Genetics & Genomic Medicine. 2019;7(4):e00577.
Gal A, Li Y, Thompson DA, Weir J, Orth U, Jacobson SG, et al. Mutations in MERTK, the human orthologue of the RCS rat retinal dystrophy gene, cause retinitis pigmentosa. Nature genetics. 2000;26(3):270–1.
Jonsson F, Burstedt M, Kellgren TG, Golovleva I. Non-homologous recombination between Alu and LINE-1 repeats results in a 91 kb deletion in MERTK causing severe retinitis pigmentosa. Molecular Vision. 2018;24:667.
Hillman RT, Green RE, Brenner SE. An unappreciated role for RNA surveillance. Genome biology. 2004;5(2):1–16.
Nasiri S, Talebi F, Asl JM, Mardasi FG. Identification of a Novel Non-Stop Mutation in PDE6C gene in an iranian family with con-rod dystrophy. Acta Medica Iranica. 2020:297–300.
Boulanger-Scemama E, El Shamieh S, Démontant V, Condroyer C, Antonio A, Michiels C, et al. Next-generation sequencing applied to a large french cone and cone-rod dystrophy cohort: mutation spectrum and new genotype-phenotype correlation. Orphanet journal of rare diseases. 2015;10:85.
Patel N, Aldahmesh MA, Alkuraya H, Anazi S, Alsharif H, Khan AO, et al. Expanding the clinical, allelic, and locus heterogeneity of retinal dystrophies. Genetics in Medicine. 2016;18(6):554–62.
Ge Z, Bowles K, Goetz K, Scholl HP, Wang F, Wang X, et al. NGS-based molecular diagnosis of 105 eyeGENE® probands with Retinitis Pigmentosa. Scientific reports. 2015;5(1):1–9.
Singh HP, Jalali S, Narayanan R, Kannabiran C. Genetic analysis of indian families with autosomal recessive retinitis pigmentosa by homozygosity screening. Investigative ophthalmology & visual science. 2009;50(9):4065–71.
Grossman GH, Watson RF, Pauer GJ, Bollinger K, Hagstrom SA. Immunocytochemical evidence of Tulp1-dependent outer segment protein transport pathways in photoreceptor cells. Experimental eye research. 2011;93(5):658–68.
Al-Hindi H, Chauhan M, Sanders R, Samarah H, DeBenedictis M, Traboulsi E, et al. TULP1 related retinal dystrophy: report of rare and novel variants with a previously undescribed phenotype in two cases. Ophthalmic Genetics. 2022;43(2):277–81.
Woodard DR, Xing C, Ganne P, Liang H, Mahindrakar A, Sankurathri C, et al. A novel homozygous missense mutation p. P388S in TULP1 causes protein instability and retinitis pigmentosa. Molecular Vision. 2021;27:179.
Xu W, Xu M, Yin Q, Liu C, Deng Y, Liu S, et al. A novel homozygous Tub mutation associated with autosomal recessive retinitis pigmentosa in a consanguineous chinese family. 2022.
Paloma E, Hjelmqvist L, Bayés M, García–Sandoval B, Ayuso C, Balcells S, et al. Novel mutations in the TULP1 gene causing autosomal recessive retinitis pigmentosa. Investigative ophthalmology & visual science. 2000;41(3):656–9.
Azam M, Khan MI, Gal A, Hussain A, Shah STA, Khan MS, et al. A homozygous p. Glu150Lys mutation in the opsin gene of two pakistani families with autosomal recessive retinitis pigmentosa. Molecular vision. 2009;15:2526.
Chen H, Chen Y, Horn R, Yang Z, Wang C, Turner MJ, et al. Clinical features of autosomal dominant retinitis pigmentosa associated with a rhodopsin mutation. ANNALS-ACADEMY OF MEDICINE SINGAPORE. 2006;35(6):411.
Zhang XL, Liu M, Meng XH, Fu WL, Yin ZQ, Huang JF, et al. Mutational analysis of the rhodopsin gene in chinese ADRP families by conformation sensitive gel electrophoresis. Life sciences. 2006;78(13):1494–8.
Dryja TP, Hahn LB, Cowley GS, McGee TL, Berson EL. Mutation spectrum of the rhodopsin gene among patients with autosomal dominant retinitis pigmentosa. Proceedings of the National Academy of Sciences. 1991;88(20):9370-4.
Inglehearn CF, Keen TJ, Bashir R, Jay M, Fitzke F, C. Bird A, et al. A completed screen for mutations of the rhodopsin gene in a panel of patients with autosomal dominant retinitis piamentosa. Human molecular genetics. 1992;1(1):41–5.
Deretic D. Post-golgi trafficking of rhodopsin in retinal photoreceptors. Eye. 1998;12(3):526–30.
Palczewski K. G protein–coupled receptor rhodopsin. Annu Rev Biochem. 2006;75:743–67.
Rafiee Komachali S, Siahpoosh Z, Salehi M. Retinitis pigmentosa: a Case Report with Thr17Arg as a Novel Mutation in RHO Gene. Journal of Epigenetics. 2022;3(1):1–6.
Kartasasmita A, Fujiki K, Iskandar E, Sovani I, Fujimaki T, Murakami A. A novel nonsense mutation in rhodopsin gene in two indonesian families with autosomal recessive retinitis pigmentosa. Ophthalmic genetics. 2011;32(1):57–63.
Acknowledgements
The authors would like to thank the patients and their family members for participation in the study. We are also thankful to Professor Carlo Rivolta and Dr. Mathieu Quinodoz for helping in Whole Exome Sequencing.
Funding
This study was supported by the Kohat University of Science and Technology, Kohat, Pakistan as well as two different institutions RILD Wellcome Wolfson Centre (Level 4), Royal Devon and Exeter NHS Foundation Trust, UK.
Author information
Authors and Affiliations
Contributions
Clinical data collection, collation, and analysis: IUS, LER, ELB and SS; Genetic testing and data analysis: MM, MD, MTH, MK, MU, LER, ELB, AHC and SS; Manuscript writing: MM, MD, NK and SS; Manuscript revision;MU, ELB and AHC; Study supervision and coordination: AHC and SS. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethical Committee of Kohat University of Science and Technology. The study was conducted in accordance with Declaration of Helsinki. Informed written consent was obtained from the participating members of the families and the parents of the minor children.
Consent for publication
Not applicable.
Competing interests
The author(s) declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Marwan, M., Dawood, M., Ullah, M. et al. Unravelling the genetic basis of retinal dystrophies in Pakistani consanguineous families. BMC Ophthalmol 23, 205 (2023). https://doi.org/10.1186/s12886-023-02948-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-02948-8