Abstract
Background
Induction of posterior vitreous detachment (PVD) is a critical step during pars plana vitrectomy. Multiple techniques and utilities have been proposed for assistance with this step with no consensus on the safest and most effective means, especially in eyes with firmly adherent posterior hyaloid. Viscodissection or the utilization of perfluorocarbon liquid (PFCL) can be used to dissect the posterior hyaloid and widely adherent epiretinal membranes.
Methods
A technique of PFCL dissection of the posterior hyaloid in eyes with abnormal adhesion of the posterior hyaloid. After core vitrectomy, breaking into the posterior hyaloid face is made via active aspiration and cutting or a sharp dissection. This is followed by active and slow injection of PFCL into the potential space between the posterior cortical vitreous and the neurosensory retina. A wave of PFCL propagates anteriorly causing “vitreo-dissection” of the peripheral cortical vitreous.
Results
The technique was effective and safe in 8 successive cases, 4 cases with vitreoretinal traction syndrome and 4 with diabetic tractional membranes.
Conclusion
The technique can be considered in cases with abnormal firmly adherent posterior hyaloid when induction of PVD proves difficult.
Similar content being viewed by others
Background
Induction of posterior vitreous detachment (PVD) is one of the critical steps of pars plana vitrectomy (PPV) for the treatment of multiple retinal disorders [1]. Those include preretinal tractional membranes seen with proliferative diabetic retinopathy [2], and anomalous vitreomacular interface that causes traction (vitreomacular traction, VMT) [3]. The degree of preoperative PVD has been recently shown to correlate with visual outcomes and reoperation rate for tractional retinal detachment (TRD) in eyes with PDR that underwent PPV for non-clearing vitreous hemorrhage [4].
Classical teaching of how induction of PVD should be performed encompasses active aspiration of the cortical vitreous over the optic disc margin using the vitreous cutter. However, some cases may have a firmly adherent posterior hyaloid, and newer smaller-gauge probes have more distal openings on the probe’s shaft that reduces their grasping power, both factors could potentially lead to a more difficult PVD induction [5]. In such cases, forced induction of PVD may be associated with a higher incidence of iatrogenic breaks, which can lead to a poorer surgical outcome [6].
Multiple techniques and instruments have been proposed to induce a break in the posterior hyaloid and facilitate PVD. Those include using a diamond duster membrane scraper (DDMS) [7], a sharp instrument [5], or a membrane scraper made by polypropylene loop [8]. In 2019, Babu et al. [9] proposed the “mega Weiss-ring” for induction of PVD in eyes with retinal detachment. In this technique, Perfluorocarbon Liquid (PFCL) is injected after core vitrectomy, followed by gentle stroking of the posterior hyaloid using a DDMS to create a defect that is circumferentially enlarged to form a 4–5 disc diameter ring with rolled-out edges. Lifting the edges using an internal limiting membrane peeling forceps allows for the PFCL to fill the potential space between the posterior hyaloid and retina, and peripherally extends the PVD into completion.
Here, we provide a modification on the mega Weiss-ring technique to induce and propagate PVD assisted by PFCL in eyes with firmly adherent posterior hyaloid.
Methods
This technique was successfully used with both 23- and 25-guage PPV. After adequate core vitrectomy, staining of the posterior cortical vitreous is done by injection of 0.1 to 0.3 mL of triamcinolone acetate suspension. Multiple trials of PVD induction are initially made by active aspiration of the cortical vitreous over the optic disc (Fig. 1A). If this fails, a sharp instrument (28-gauge needle with bent tip) is used to penetrate the posterior hyaloid combined with active aspiration as described by Ellabban et al. [5].
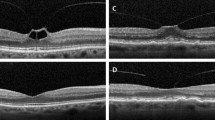
Vitreo-dissection technique using PFCL. Initial creation of a hole within the posterior hyaloid using active aspiration and cutting by the vitrectomy probe (A), followed by introduction of the PFCL cannula into the hole directed towards the potential space between the posterior cortical vitreous and the neurosensory retina (B), and injection of PFCL to form a bubble that propagates, elevating the posterior cortical vitreous away from the retina (C)
Injection of PFCL is then carried out through the hole in the posterior hyaloid, in the potential space between the posterior cortical vitreous and neurosensory retina in a manner that mimics the hydro-dissection or visco-dissection during cataract surgery in which the lenticular cortex is dissected from the inner capsular surface (Fig. 1B). However, controlled slow injection is crucial from a safety standpoint to avoid iatrogenic break formation; this can be carried out using an automated injection method via infusion attachment to the PFCL cannula and foot pedal control or manual injection, with the opening of the cannula aimed away from the fovea in both cases. A test outside the eye is important to ensure cannula patency and modify injection speed prior to injection inside the eye. A successful injection is heralded by a slow wave of PFCL propagating centrifugally, and separating the posterior hyaloid face from the inner paracentral then peripheral retinal surface (Fig. 1C). Continuation of the conventional steps of vitrectomy could then be carried out (supplemental digital content 1).
In our experience, this technique was most useful in cases with abnormal, firmly adherent posterior hyaloid. We utilized this technique with excellent results in eyes that underwent PPV for VMT or diabetic TRD. Possible complications are rare and included failure to propagate the PVD, the potential iatrogenic injury to the retina by the PFCL cannula which could lead to retinal break or bleeding, or the creation of iatrogenic breaks during dissection by the PFCL.
Results and discussion
We describe a simple and relatively safe technique for induction and propagation of PVD in eyes with abnormal adhesion of the posterior hyaloid. We have successfully performed this technique in 4 eyes with VMT and 4 eyes with diabetic TRD, with no detectable complications. The technique allows for quick propagation of a PFCL wave that separates the posterior cortical vitreous from the retinal surface; thus, avoiding the complications seen with sharp dissection [5].
Recently, a “mega Weiss-ring” technique was described by Babu et al. [9] for eyes with rhegmatogenous retinal detachment. In that technique, PFCL is injected prior to creation of a hole in the posterior hyaloid and then let to passively “slide” into the space between the cortical vitreous and retina by lifting the edges of the posterior hyaloid. In our technique, active rather than passive introduction of the PFCL allows for a more rapid dissection of the posterior vitreous face. The “mega Weiss-ring” technique also depends on the ability of PFCL to flatten the neurosensory retina against the retinal pigment epithelium, making it unsuitable for cases with advanced preretinal proliferation, traumatic and long-standing detachments. Our active “vitreo-dissection” obviates such contraindications.
Earlier on, Arevalo had described the “en bloc perfluorodissection” for TRD [10]. The technique also utilizes PFCL injection into a hole created in the mid-peripheral posterior hyaloid in eyes with advanced diabetic retinopathy and epimacular membranes. This allows for the complete separation of epiretinal tissue in an “en bloc” manner and was proven safe in the series of eyes operated on by the author.
Some limitations exist in our report, mainly the small sample size since we consider this a “proof-of-concept” study, and the grouping of different pathologies (PDR and VMT) together. An ongoing effort aims to assess outcomes of the technique in a larger cohort with specific pathologies. PFCL toxicity is another limitation that may hinder the use of our described technique, especially in cases where PFCL use had not been originally indicated for assisting the surgical repair. Short-term injection of PFCL in the vitreous cavity has been demonstrated to be well-tolerated in humans. Direct retinal toxicity is often related to subretinal retention of the liquid [11]. In the cases where we utilized the technique, no pre-existing breaks or macular holes were detectable preoperatively, potentially obviating the occurrence of such complication. The only possible route for PFCL to reach the subretinal space would be the creation of an iatrogenic break during the initial steps of PVD induction, which we did not observe in any of our cases. Nevertheless, such a scenario cannot be ruled out and should warrant caution during utilization of this technique.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- DDMS:
-
diamond duster membrane scraper
- PFCL:
-
perfluorocarbon liquid
- PPV:
-
pars plana vitrectomy
- PVD:
-
posterior vitreous detachment
- TRD:
-
tractional retinal detachment
- VMT:
-
vitreomacular traction
References
Dhoot AS, Popovic MM, Nichani PAH, Eshtiaghi A, Mihalache A, Sayal AP, et al. Pars Plana Vitrectomy versus scleral buckle: a comprehensive meta-analysis of 15,947 eyes. Surv Ophthalmol. 2022;67(4):932–49.
Berrocal MH, Acaba-Berrocal L. Early pars plana vitrectomy for proliferative diabetic retinopathy: update and review of current literature. Curr Opin Ophthalmol. 2021;32:203–8.
Santra M, Sharma M, Katoch D, Jain S, Saikia UN, Dogra MR, et al. Induction of posterior vitreous detachment (PVD) by non-enzymatic reagents targeting vitreous collagen liquefaction as well as vitreoretinal adhesion. Sci Rep. 2020;10:8250.
Tandias R, Lemire CA, Palvadi K, Arroyo JG. Posterior vitreous detachment status as a predictive factor for outcomes of vitrectomy for diabetic vitreous hemorrhage. Retina. 2022;42:1103–10.
Ellabban AA, Barry R, Sallam AAB. Surgical induction of posterior vitreous detachment using combined sharp dissection and active aspiration. Acta Ophthalmol. 2016;94:e524–5.
Chung SE, Kim K-H, Kang SW. Retinal breaks associated with the induction of posterior vitreous detachment. Am J Ophthalmol. 2009;147:1012–6.
Takeuchi M, Takayama K, Sato T, Ishikawa S, Fujii S, Sakurai Y. Non-aspiration technique to induce posterior vitreous detachment in minimum incision vitrectomy system. Br J Ophthalmol. 2012;96:1378–9.
Jiang F, Zhang W, Liu Y, Chen F, Xie Z. Membrane scraper made by polypropylene loop. Retina. 2021;41:2631–3.
Babu N, Kumar J, Kohli P, Ramasamy K. Perfluoro-n-octane-assisted mega Weiss-ring technique for posterior vitreous detachment induction in retinal detachment. Indian J Ophthalmol. 2019;67:1463.
Arevalo JF. En bloc perfluorodissection for tractional retinal detachment in proliferative diabetic retinopathy. Ophthalmology. 2008;115:e21–5.
Georgalas I, Ladas I, Tservakis I, Taliantzis S, Gotzaridis E, Papaconstantinou D, et al. Perfluorocarbon liquids in vitreoretinal surgery: a review of applications and toxicity. Cutan Ocul Toxicol. 2011;30:251–62.
Acknowledgements
None.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
IA devised the technique and performed the surgical procedures. MMH collected the data and prepared the media required for publication. YAF reviewed the literature and drafted the manuscript. All authors critically revised the manuscript and approved the final version for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics committee approval from Al Mashreq Eye Center Scientific Committee was obtained to conduct this study. Written informed consent was obtained from patients prior to the surgery. The study adhered to the tenets of the Declaration of Helsinki.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Digital Content 1.
Video demonstration of the “vitreo-dissection” technique. Gentle injection of PFCL into the potential space between the posterior cortical vitreous and the neurosensory retina.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Aziz, I.A., Hussein, M.M. & Fouad, Y.A. Perfluorocarbon liquid-assisted vitreo-dissection in eyes with firmly adherent posterior hyaloid. BMC Ophthalmol 22, 475 (2022). https://doi.org/10.1186/s12886-022-02715-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02715-1