Abstract
Background
To compare biometric parameters, especially lens parameters, in patients with high myopia and anisometropia.
Methods
Patients with spherical equivalent greater than -6D and at least one eye with an axial length greater than 26 mm and a difference in binocular axial length greater than 2 mm were included in this study. In each patient, the eye with a relatively shorter axial length was assigned to Group S, and the other eye was assigned to Group L. In patients whose binocular axial length difference was greater than 4 mm, the eye with the shorter axial length was assigned to Group S1 and the other eye was assigned to Group L1. In patients whose shorter eye axial was less than 26 mm, the eye with the shorter axial was assigned to Group S2 and the other eye was assigned to Group L2. Central corneal thickness, corneal curvature radius, axial length, anterior chamber depth, lens thickness, white-to-white corneal diameter and the radius of the anterior and posterior lens capsules were compared between Group S and Group L, Groups S1 and L1, and Groups S2 and L2.
Results
Sixty-four people were enrolled in the study. There were 26 people with an axial length difference more than 4 mm (Group S1 and Group L1) and 34 patients with an axial length less than 26 mm (Group S2 and Group L2). No significant differences were found in any parameters except axial length between Group S and Group L, Groups S1 and L1, or Groups S2 and L2 (p > 0.05).
Conclusions
The anterior parameters of patients with high myopia did not change with the axial length.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Myopia is one of the main causes of vision impairment and has become an important public health problem worldwide in recent years [1]. In 2010, uncorrected refractive error accounted for 53% of severe and moderate vision impairment, and the global economic burden related to myopia was estimated to be $244 billion in 2015 [2]. With the excessive use of digital products, the incidence of myopia has increased considerably each year. Myopia affects our work, study and daily life, especially for patients with high myopia, which will cause a variety of serious complications, such as cataract, lens dislocation, maculopathy, retinal detachment, and eventually leads to irreversible blindness [3,4,5]. Many scholars devote their work to the study of high myopia. These studies can not only help us understand the characteristics and pathogenesis of high myopia but can provide insights for doctors when performing operations on patients with high myopia [6,7,8]. High myopia usually occurs in both eyes and is symmetrical on both sides. However, there are a few patients whose axial lengths are significantly different; for some people, one eye is normal and the other eye has high myopia, or both eyes have high myopia and the condition is more serious in one eye. A comparative study of these patients can provide a better understanding of the biological characteristics and pathogenesis of high myopia and can avoid the influences of many factors, such as age, sex, environmental, individual and other factors. We have conducted an analysis of anterior segment characteristics in patients with high myopia and binocular axial lengths greater than 2 mm in our hospital since 2014. We aimed to further explore the pathogenesis of high myopia and the biological characteristics of the anterior segment and to provide insight into the clinical trials of secondary cataracts due to high myopia.
Methods
This study is a prospective study. It followed the tenets of the Declaration of Helsinki and was approved by the ethics committee of the Xiamen Eye Center. Written consent providing permission to use the patient’s data was obtained from the patients or their parents.
Patients with spherical equivalent (SE) greater than -6D and at least one eye with an axial length greater than 26 mm and a difference in binocular axial length greater than 2 mm were enrolled in the study from April 2014 to September 2019. Patients who had other ocular diseases, such as corneal diseases, retinal detachment, choroid exudation, congenital glaucoma, and abnormal lenses, such as dislocation or subluxation, were excluded.
Visual acuity, best corrected visual acuity, slit-lamp examination, fundus examination and medical optometry were performed for these patients. Intraocular pressure (IOP) was measured using the Goldman tonometer. Central corneal thickness (CCT), corneal curvature radius (CCR), axial length (AL), anterior chamber depth (from corneal rear surface to the front surface of the lens, ACD), lens thickness (LT) and white-to-white (WTW) corneal diameter were measured using a Lenstar 900 (HAAG-STREIT, USA). Ultrasound biomicroscopy (UBM) was performed to exclude lens abnormalities. Anterior optical coherence tomography (Tomey SS-1000 CASIA; Tomey, Nagoya, Japan) was used to measure the radius of the anterior and posterior curvature in the 4 mm central region of the crystal (radius of anterior capsule membrane, AR; radius of posterior capsule membrane, PR; Fig. 1). B scan, fundus photography, posterior OCT, and Opel examination were also performed to exclude other diseases.
The eye with a relatively shorter axial length of each patient was assigned to Group S, while the other eye with a longer axial length was assigned to Group L. CCT, CCR, AL, ACD, LT, WTW, AR and PR were compared between the two groups. Patients whose binocular axial length difference was greater than 4 mm were also analyzed. The eye with the lesser axial difference eye was assigned to Group S1, and the eye with the greater axial difference was assigned to Group L1. The above parameters were compared between both eyes. In addition, patients whose shorter eye axial was less than 26 mm were analyzed. The eye with the shorter axial was assigned to Group S2, and the eye with the longer axial was assigned to Group L2. The above parameters were also compared.
Statistical analysis was performed with SPSS software V.22 (SPSS, Inc., Chicago, IL). After identifying a normal distribution, a paired data t test was used for binocular comparison. P < 0.05 was considered statistically significant.
Results
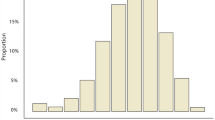
Sixty-four people (29 males, 35 females, aged 12 to 73 years) were enrolled in the study at Xiamen Eye Center. There were 26 people with an axial length greater than 4 mm (Groups S1 and L1) and 34 patients with a shorter axial length less than 26 mm (Groups S2 and L2). The AL in Group L is significantly larger than Group S (28.26 ± 2.04 mm VS 25.15 ± 2.08 mm), However, there were no significant differences in CCT, CCR, ACD, LT, WTW, AR and PR between the two groups (Table 1). When compared with Group L1 and Group S1, the difference of AL is greater than Group L and Group S, however, there is still no significant differences in CCT, CCR, ACD, LT, WTW, AR and PR (Table 2). The same results can be achieved when compared with Group L2 and Group S2 which has an AL shorter than 26 mm (Table 3).
Discussions
High myopia is increasingly becoming the leading eye disease that causes irreversible blindness in the world. Current research has mainly focused on the pathogenesis and changes in biological parameters, such as axial length, anterior chamber depth, corneal curvature, lens characteristics, and scleral, choroid and retinal changes. In our study, we aimed to determine the change in the anterior part of the eye through the comparison of parameters in patients with high myopia and anisometropia.
The anterior and posterior curvature radius of the lens is an important factor to describe crystal morphology. However, for the bulge of the iris in front of the lens, modern imaging equipment is unable to show the full picture and accurate biological parameters of the lens, lens thickness is the only parameter measured in clinical trials. The only published article about the curvature radius of the lens was conducted by Zheng in 2013, MRI was used to measure the change in curvature radius of the lens before and after adjustment in their article [9]. However, MRI examination cannot guarantee that the scanning plane is the central plane of the sagittal axis of the lens. In our study, anterior segment optical coherence tomography (AS-OCT) was used to accurately scan the lens image of the optic axis plane, and the anterior and posterior capsule images can be clearly viewed. The instrument's own software can measure the curvature radius of the anterior and posterior capsule of the lens in different diameter ranges semi-automatically and can also conduct 3D scanning imaging. In Zheng’s study, they found that the curvature radii of the anterior capsule and posterior capsule were 8.7 ± 0.8 mm and 6.2 ± 0.5 mm, respectively. As we all know, the radius of curvature of the cornea is generally 7–8 mm. The curvature radius of anterior capsule of the lens is slightly larger than that of the cornea in Zheng’s study and this is contrary to the fact that the anterior curvature of the lens is significantly larger than that of the front surface of the cornea from the OCT imagine. So, the results of Zheng’s study remain to be discussed.
The anterior chamber depth (ACD), central corneal thickness (CCT), corneal curvature and white-to-white distance were compared in patients with high myopia and anisometropia in our study. There were no significant differences between the two groups. This result is consistent with other studies [10,11,12,13,14,15]. However, contrary results in some parameters were found by other researchers [16,17,18]. The reason for the controversial conclusions of different scholars lies in the differences in research subjects, measuring instruments, and research designs.
In addition, we compared the biological parameters of patients with an axis length less than 26 mm and found that there were no significant differences in biological parameters other than axis length. Additionally, we drew the same conclusion when comparing patients with an axis length difference greater than 4 mm. So, we concluded that there is no change in anterior parameters, including the lens morphology, in patients with high myopia.
High myopia is a most common risk factor for advanced intracapsular IOL dislocation, with reported incidence ranging from 19.7 to 40% [19, 20]. Most researchers consider the suspensory ligament of patients with high myopia to be fragile and loose [19, 21, 22]. Hao Zhou discovered that the suspensory ligament is sparse and even reduced significantly in number in a guinea pig model of high myopia [23]. Na Liao found that the suspensory ligament length of patients with high myopia was significantly longer than that of patients with normal myopia (SD < -6.0 D) [24]. Other researchers consider that the lens capsule of patients with high myopia is larger and cause the excessive elongation of the zonular fibers for it has to support greater stress than in normal axial length eyes [19, 22]. The fragile and sparse zonular fibers causes the downward shift of IOL after cataract surgery [21]. Our research found that the lens thickness and curvature of the anterior and posterior capsules did not change as the axis of the eyeball lengthened. Therefore, we conclude that there is no change in lens morphology in patients with high myopia. The reason of the fragile and hyperextended suspensory ligament still needs more research.
Conclusion
Our research compared the biometric parameters in patients with high myopia and anisometropia and concluded that there were no significant differences in ACD, CCT, corneal curvature, LT, anterior or posterior capsule curvature other than the axis length. This result is consistent with the theory that the pathogenesis of high myopia lies in the posterior part of the eye [25]. In addition, abnormalities in the suspensory ligament and vitreous cause lens instability in patients with high myopia, which leads to complications during and after cataract surgery. Although we compared the biometric parameters of patients with an axis length less than 26 mm and patients with a binocular axis difference greater than 4 mm, more detailed observation about the suspensory ligament is required in future research.
Availability of data and materials
The data analyzed during the current study are not publicly available due to the use of internal and confidential patient medical record data stored on internal, confidential and protected hard drives, but de-identified and redacted data are available from the corresponding author on reasonable request.
References
Bourne RR, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, Jonas JB, Keeffe J, Leasher J, Naidoo K, et al. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health. 2013;1(6):e339–49.
Naidoo KS, Fricke TR, Frick KD, Jong M, Naduvilath TJ, Resnikoff S, Sankaridurg P. Potential lost productivity resulting from the global burden of myopia: systematic review, meta-analysis, and modeling. Ophthalmology. 2019;126(3):338–46.
Ikuno Y. Overview of the complications of high myopia. Retina. 2017;37(12):2347–51.
Liu X, Wan X. The progress of studies on intraocular lens implantation in cataract with high myopia. Zhonghua Yan Ke Za Zhi. 2015;51(7):548–51.
Wu L, Sun X, Zhou X, Weng C. Causes and 3-year-incidence of blindness in Jing-An District, Shanghai, China 2001–2009. BMC Ophthalmol. 2011;11:10.
Zhou XT, Qu J. Selection of animal model in myopia research. Zhonghua Yan Ke Za Zhi. 2005;41(6):486–7.
Deng J, Jin J, Lv M, Jiang W, Sun S, Yao C, Zhu J, Zou H, Wang L, He X, et al. Distribution of scleral thickness and associated factors in 810 Chinese children and adolescents: a swept-source optical coherence tomography study. Acta Ophthalmol. 2019;97(3):e410–8.
Wu H, Chen W, Zhao F, Zhou Q, Reinach PS, Deng L, Ma L, Luo S, Srinivasalu N, Pan M, et al. Scleral hypoxia is a target for myopia control. Proc Natl Acad Sci U S A. 2018;115(30):E7091–100.
Zheng SL, Zhang A, Shi JJ, Zhou YX. Magnetic resonance imaging study of effects of accommodation on human lens morphological characters. Zhonghua Yi Xue Za Zhi. 2013;93(41):3280–3.
Zhao HL, Wang RQ, Wu MQ, Jiang J. Dynamic changes of ocular biometric parameters: a modified form-deprivation myopia model of young guinea pigs. Int J Ophthalmol. 2011;4(5):484–8.
Franco AM, Lopes YC, Souza PH, Allemann N. Biometry in the growth of the high myopic eye in childhood. Arq Bras Oftalmol. 2013;76(5):265–9.
Saw SM, Chua WH, Gazzard G, Koh D, Tan DT, Stone RA. Eye growth changes in myopic children in Singapore. Br J Ophthalmol. 2005;89(11):1489–94.
Kim SY, Cho SY, Yang JW, Kim CS, Lee YC. The correlation of differences in the ocular component values with the degree of myopic anisometropia. Korean J Ophthalmol. 2013;27(1):44–7.
Xie R, Zhou XT, Lu F, Chen M, Xue A, Chen S, Qu J. Correlation between myopia and major biometric parameters of the eye: a retrospective clinical study. Optom Vis Sci. 2009;86(5):E503–8.
Wang DJ, Sheng Y, Huang YF. Measurement of ocular anterior segment in myopic patients with pentacam scheimplug system. J Chinese PLA Postgrad Med Sch. 2010;31(03):230–4.
Hayes BP, Fitzke FW, Hodos W, Holden AL. A morphological analysis of experimental myopia in young chickens. Invest Ophthalmol Vis Sci. 1986;27(6):981–91.
Sun CW, Wang QM, Xue AQ, Wang SL, Zhu SQ. The correlation among axial length, diopter, anterior chamber depth and keratorefractive power of high myopia. Zhejiang Med. 2007;05:414–6.
Xing YQ, Zhang DD, Li T. Effect of long axial-length on anterior segment morphology. J Clin Ophthalmol. 2016;24(01):9–11.
Fernandez-BuenagaAlioPerez-ArdoyLarrosa-QuesadaPinilla-CortesBarraquerAlioMunoz-Negrete RJLALALRJLFJ 2nd. Late in-the-bag intraocular lens dislocation requiring explantation: risk factors and outcomes. Eye. 2013;27(7):795–801 (Quiz 2).
Rey A, Jurgens I, Dyrda A, Maseras X, Morilla A. Surgical outcome of late in-the-bag intraocular lens dislocation treated with pars plana vitrectomy. Retina. 2016;36(3):576–81.
Wang D, Yu X, Li Z, Ding X, Lian H, Mao J, Zhao Y, Zhao YE. The effect of anterior capsule polishing on capsular contraction and lens stability in cataract patients with high myopia. J Ophthalmol. 2018;2018:8676451.
Cheng HM, Singh OS, Kwong KK, Xiong J, Woods BT, Brady TJ. Shape of the myopic eye as seen with high-resolution magnetic resonance imaging. Optom Vis Sci. 1992;69(9):698–701.
Zhou H, Chu RY, Zhou XT, Dai JH, Chen HD. Ultrastruct ure changes of lens zonule in experimental myopia induced by eye lid suture. Acad J Sec mil med Univ. 2003;12:1347–8.
Liao N, Tang XL, Huang YZ, Li NL, Fang W. Study on preoperative observation of cataract patients’zanules by ultrasound biomicroscopy. West China Med J. 2016;31(12):1995–9.
Ohno-Matsui K, Lai TY, Lai CC, Cheung CM. Updates of pathologic myopia. Prog Retin Eye Res. 2016;52:156–87.
Acknowledgements
The authors thank Dr.Zhiming Zhao, Jianhua Zhang and Yuedi Lu for the research support.
Disclosure
None of the authors has a financial or proprietary interest in any material or method mentioned.
Funding
Supported by Key laboratory of myopia, National Health Commission/Chinese Academy of Medical Sciences (Fudan University).
Author information
Authors and Affiliations
Contributions
Yuhong Wang and Jinkun Liu contributed equally to this work. Data curation: Fei Wang, Yingying Xue, Mengnan Wu, Fei Yu, Ruxin Gao. Methodology: Weiyi Huang, Yazhang Xu, Resources: Weiyi Huang, Yazhang Xu, Supervision: Yuhong Wang. Writing original draft: Yuhong Wang, Jinkun Liu. Writing – review & editing: Jinkun Liu. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the ethics committee of the Xiamen Eye Center. Written informed consent from the patients or their parents that their data can be used was acquired.
Consent for publication
Not applicable.
Competing interests
The author declares that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, J., Wang, Y., Huang, W. et al. Comparison of the biometric parameters in patients with high myopia and anisometropia. BMC Ophthalmol 22, 229 (2022). https://doi.org/10.1186/s12886-022-02450-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02450-7