Abstract
Background
Diagnostic vitrectomy is an important method for evaluating uveitis, and its diagnostic utility is high regardless of whether the uveitis is infectious or non-infectious. The course of diagnostic vitreous surgery with 27-gauge pars plana vitrectomy and perioperative complications is reported.
Methods
An observational retrospective study of patients who underwent 27-gauge diagnostic vitrectomy due to atypical intraocular inflammation was conducted. The final diagnosis rate, complications due to surgery, preoperative visual acuity, and postoperative visual acuity (1 month and 6 months after surgery) were examined retrospectively.
Results
Diagnostic vitreous surgery was performed in 32 patients and 35 eyes (14 males and 18 females, age 14–85 years, median 67 years) during the study period. The average operation time was 52 min for 19 eyes with cataract surgery and 35 min for 16 eyes without cataract surgery. Preoperative log(minimum angle of resolution [MAR]) visual acuity was 0.84 ± 0.87, 1-month postoperative logMAR visual acuity was 0.41 ± 0.55 (p = 0.004, n = 28), and 6-month postoperative average logMAR visual acuity was 0.45 ± 0.73 (p = 0.012, n = 15). The diagnosis was made by diagnostic vitrectomy in 19 cases (54%). Postoperative complications were observed in 2 of 35 postoperative patients (5%); one involved increased intraocular pressure, and the other case involved vitreous hemorrhage of the eye, necessitating reoperation.
Conclusion
Diagnostic 27-gauge vitrectomy could be effective for evaluating intraocular inflammation.
Similar content being viewed by others
Introduction
Uveitis is divided into infectious and non-infectious, and there is a definition based on the site of occurrence [1,2,3,4,5]. Of them, posterior uveitis and pan uveitis, which cause significant problems in visual function, require accurate diagnosis [6,7,8,9]. In addition, even in the pathological condition that is being followed up as vitreous opacification in general medical care, very important diseases such as intraocular lymphoma may be hidden, and careful diagnosis is required [10,11,12].
Vitreous opacity is generally an age-associated change, but it can sometimes be caused by various illnesses affecting the whole body. For example, vitreous opacity can be associated with genetic predisposition, inflammatory infectious or non-infectious conditions, and degenerative, traumatic, or idiopathic causes [13].
We can determine the cause of vitreous opacity through ophthalmic examinations, medical examinations, laboratory tests, and image analysis, but because these approaches are limited, it may not be possible in some cases to identify the cause of the findings. One alternative for evaluating ophthalmic phenomena is diagnostic vitrectomy, which has been performed for a long time. In particular, the use of 25-gauge transconjunctival vitrectomy is increasing [14,15,16].
Several reports have described the safety and efficacy of 25-gauge transconjunctival vitrectomy. Mason et al. examined postoperative complications in 168 eyes of patients who had undergone sutureless 25-gauge vitrectomy for vitreous floaters. Cystoid macular edema and vitreous hemorrhage have been observed in some patients, but the rate of complications is low [17]. Yeh et al. assessed cases of 25-gauge transconjunctival sutureless vitrectomy for obtaining vitreous specimens in patients with intraocular lymphoma and reported the effectiveness of the technique for making a diagnosis, and they also reported a low rate of postoperative complications of 25-gauge transconjunctival sutureless vitrectomy for diagnosis and improvement in visual acuity compared to preoperative acuity [18].
In terms of the size of scars on the conjunctiva, 27-gauge vitrectomy has some advantages, since the sclerotomy is minimally invasive and less painful for patients [19]. However, there are fewer reports regarding the safety and efficacy of 27-gauge transconjunctival diagnostic vitrectomy. We therefore had a clinical interest in examining the benefits and complications associated with 27-gauge diagnostic vitrectomy, including that combined with cataract surgery. Therefore, the safety and effectiveness of 27-gauge diagnostic vitrectomy in a real-world setting at our hospital are reported.
Materials and methods
A total of 32 eyes of 29 patients who underwent 27-gauge diagnostic vitrectomy surgery at the Osaka City University Hospital from July 2018 to December 2020 were included in the study. Data for these patients were examined retrospectively. All procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the Institutional and/or National Research Committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Approval for this study was obtained prior to the start of the study from the Institutional Review Board at Osaka City University, Japan (IRB-4237). Written, informed consent for the storage of patient information in the hospital database and use in research was provided by all patients enrolled in the study.
The inclusion criteria for this study were as follows: (1) existence of inflammation or vitreous opacity; (2) no improvement of visual acuity, intraocular inflammation, or of the patient’s subjective symptoms with topical betamethasone and/or levofloxacin over 2 weeks; and (3) undergoing surgery with experienced vitrectomy surgeons (vitrectomy surgery > 2000 cases). The exclusion criterion was lack of written, informed consent.
The following data were collected: patient age and sex, best-corrected visual acuity (BCVA) preoperatively and 1 month and 6 months after surgery, duration of vitreous surgery, postoperative complications, and results of tests of vitreous specimens. All specimens underwent multiplex polymerase chain reaction (PCR) analysis for the presence of several different bacteria and viruses according to previously reported methods [9]. If patients were suspected of having intraocular lymphoma, concentrations of the cytokines interleukin IL-6 and IL-10 were determined, and gene arrangement studies (IgH arrangement) were conducted. An IL-10/IL-6 ratio > 1 strongly suggested a diagnosis of intraocular lymphoma [20].
Regarding visual acuity, the preoperative logarithm of the minimum angle of resolution (logMAR) visual acuity was compared with the 1-month, 3-month, and 6-month postoperative logMARs.
Surgical procedure
All surgeries were performed under sub-tenon anesthesia consisting of 2% lidocaine with epinephrine and 0.25% bupivacaine. The Constellation Vision system (Alcon Laboratories, Inc., Fort Worth, TX, USA) was used as a 27-gauge transconjunctival sutureless pars plana vitrectomy system with a wide-angle noncontact viewing system (Resight®; Carl Zeiss Meditec AG, Jena, Germany). Surgeries were performed by three vitreoretinal surgeons (M.T., M.Y., S.H.) who had performed more than 2000 cases of micro-incision vitrectomy surgery (MIVS). After surgeons positioned the three trocars on the conjunctiva, a vitreous sample of approximately 1–2 ml was collected while the infusion was not open. The surgical parameters were 20,000 cuts per minute (cpm) and a vacuum of 0–650 mmHg. During surgery, intraocular pressure (IOP) was controlled to 15–20 mmHg with an IOP control system. Inner limited membrane peeling was performed in 11 cases (6 cases with phacoemulsification and intraocular lens implantation (PEA + IOL), 5 cases without PEA + IOL) using Brilliant Blue-G, and air tamponade was performed in 4 cases (2 cases with PEA + IOL, others without PEA + IOL). No scleral port sites were found to be leaking at the end of the surgery, so that all cases were without scleral suture.
A total of 16 of 32 eyes had cataracts, and since this can be problematic for vitrectomy, these eyes were treated with PEA and IOL.
Statistical analyses
Collected data were entered into a Microsoft Excel spreadsheet (Microsoft, Redmond, WA) for further compilation and analysis. Statistical analyses were performed using Microsoft Excel, with a p-value < 0.05 considered significant. For the analyses, decimal visual acuity was converted to logMAR. When a patient’s decimal visual acuity was < 0.01, it was converted to logMAR according to the report of Johnson et al. [21].
Results
Preoperative characteristics
A total of 32 eyes of 29 patients underwent 3-port, 27-gauge pars plana diagnostic vitrectomy; there were 13 eyes of 12 male patients and 19 eyes of 17 female patients. The mean age of all 29 patients was 65.7 ± 14.9 (range 14–85) years, and the mean preoperative BVCA of all patients was 0.84 ± 0.87 logMAR. Of 16 of 32 eyes that underwent PEA + IOL, it was possible to follow 13 patients for 1 month, 11 patients for 3 months, and 8 patients for 6 months after the operation. Of 16 eyes without PEA + IOL, it was possible to follow 15 patients for 1 month, 9 patients for 3 months, and 7 patients for 6 months after the operation (Table 1).
Results of diagnostic testing of vitrectomy specimens
The mean duration of all 3-port 27-gauge diagnosis vitrectomy operations was 40.1 ± 15.9 min. Based on whether PEA + IOL was conducted, the mean duration of vitrectomy with PEA + IOL was 46.4 ± 17.4 min, whereas the mean duration of vitrectomy without PEA + IOL was 34.8 ± 11.8 min (p = 0.04).
There were positive endogenous controls in all cases. All specimens were positive for the negative control in this test, so the validity of the test was confirmed. Nine patients had positive PCR results, as follows: Epstein-Barr virus (2 patients), Treponema pallidum (2 patients), bacterial 16-strip PCR (4 patients), human T-cell leukemia virus type-1 (1 patient), Varicella zoster virus (1 patient). Both T. pallidum and Epstein-Barr virus were found in the specimen of 1 patient.
In addition, 15 patients were tested for IL-6 and IL-10 levels to assess inflammatory status and diagnose lymphoma (Table 2).
Seven eyes of 5 patients were suspected of having intraocular lymphoma; the IL-10/IL-16 ratio was determined for 6 eyes of 5 patients, and 5 eyes of 4 patients were subjected to IgH arrangement analysis. In 4 eyes of 3 patients, the IL-6/IL-10 ratio was > 1; however, IgH arrangement was negative in 2 eyes, but the amount of the other specimens was too low for IgH arrangement analysis (these eyes were of the same patient). In patients in whom the IL-6/IL-10 ratio of the vitreous specimen was < 1, all IgH arrangement results were negative. In 1 patient, PCR testing of bacterial 16-strip was positive, and the IL-6/IL-10 ratio was also > 1 (IgH arrangement was negative). The diagnostic rate data are summarized in Table 3.
With regard to postoperative complications, 1 patient had increased (IOP after vitrectomy and was treated with dorzolamide and timolol maleate eye drops. There was also 1 patient with vitreous hemorrhage and decreased IOP; this patient underwent re-operation with 27-gauge vitrectomy, and the vitreous fluid was replaced with air.
Visual acuity
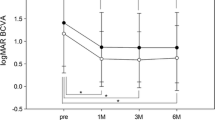
Postoperative mean BCVA improved to 0.42 ± 0.55 logMAR at 1 month (p = 0.004, n = 28), 0.47 ± 0.61 logMAR at 3 months (p = 0.003, n = 20), and 0.46 ± 0.73 logMAR at 6 months (p = 0.011, n = 15). In patients with PEA + IOL, mean BCVA improved to 0.37 ± 0.33 logMAR at 1 month (p = 0.03, n = 13), 0.39 ± 0.38 logMAR at 3 months (p = 0.02, n = 11), and 0.38 ± 0.31 logMAR at 6 months (p = 0.06, n = 8). Of the patients who underwent diagnostic vitrectomy without PEA + IOL, mean BCVA improved to 0.43 ± 0.69 logMAR at 1 month (p = 0.06, n = 15), 0.57 ± 0.80 logMAR at 3 months (p = 0.051, n = 9), and 0.45 ± 1.00 logMAR at 6 months (p = 0.09, n = 7). Comparing these two groups in terms of visual acuity, there was no significant difference at any point (p = 0.67 preoperatively, p = 0.79 at 1 month, p = 0.53 at 3 months, and p = 0.86 at 6 months after surgery), as summarized in Table 4.
Discussion
Diagnostic vitrectomy is a very common and important clinical option for diagnosing uveitis, including primary intraocular lymphoma [18, 22, 23]. Some case reports have described the diagnostic rate of MIVS, including 27-gauge pars plana vitrectomy [24, 25]. As far as we know, this case series is the first report describing 27-gauge vitrectomy for the diagnosis of uveitis. Diagnostic and complication rates were acceptable even when compared with other gauges, including other MIVS in previous articles (Table 5).
In recent years, MIVS has shown remarkable progress, and the application of 27-gauge pars plana vitrectomy has become widespread, especially in Japan, with good clinical results to date [26, 27]. The present results indicate that diagnostic vitrectomy is very safe, and the frequency of complications is low, even in cases of uveitis. The low surgical complication rate of the 27-gauge system and its safety have already been reported in several studies [28,29,30]. In the present study, there were originally postoperative complications due to the activity of the uveitis, but there were no complications due to the surgical operation itself.
In addition, there was a possibility that the vitreous humor sample would be crushed when the MIVS became a small gauge, but it was possible to obtain a morphologically diagnosable sample by cytology in an HTLV-1 uveitis patient (Fig. 1). Table 5 summarizes previous reports describing 20-gauge and small-gauge techniques.
For uveitis of unknown cause, multiplex PCR is an established method for excluding an infectious origin. In particular, as reported by Sugita et al. and Nakano et al., the probability of diagnosis if infection is present is extremely high [7,8,9]. Not all of the present cases were strongly suspected of having an infectious etiology, but testing as an exclusionary diagnosis and positive endogenous control in all cases indicated that 27-gauge diagnostic vitrectomy is useful as a basic test.
In addition, the levels of IL-10 and IL-6 were investigated in cases suspected of having intraocular lymphoma. In addition, determining IL-6 levels in other cases of uveitis as well enables evaluation of the extent of intraocular inflammation and could thus prove beneficial in selecting treatment options such as tocilizumab [31, 32]. Furthermore, the improvement in visual acuity is only a secondary effect. This is because, in the combination cataract surgery cases, it could be caused by the improvement of the cataract, and it depends more on the pathological condition of uveitis itself than on the effect of vitrectomy in the first place, so that using visual acuity as a parameter may have been a confounding factor in this study.
In intraocular lymphoma cases, flow cytometry, cytokine evaluation, gene rearrangement studies, and cooperation with an ophthalmic pathologist are indispensable to reach an accurate diagnosis [11, 33,34,35,36]. Such patients are often diagnosed with uveitis of unknown cause and treated with long-term steroids; however, their symptoms worsen [37]. In terms of clinical diagnostic effectiveness, some studies have reported success with vitrectomy. Wittenberg et al., Davis et al., and Mrunthunjaya et al. reported diagnostic rates of 55.3%, 61.5%, and 38.8%, respectively, for 20-gauge diagnostic vitrectomy [14, 15, 22]. The present result was with a minimally invasive 27-gauge, with almost the same diagnostic accuracy as with 20-gauge, and there were not many complications (complication rate: 6.4% (2/31)).
The primary limitations of the present study include its small case series design (N = 31) and that it was a cohort study with no comparison group. In addition, the effect of improving visual acuity is more limited because it is related to the pathological condition of uveitis rather than the effect of vitrectomy. Another limitation of this study is the fact that all cases were not reviewed by an ocular pathologist. If they had been, the accuracy of diagnosis may have increased, and 27-gauge was not compared with the other MIVS systems in this case series.
In conclusion, the results of the present study are useful for diagnosing intraocular lymphoma and uveitis of unknown origin. Furthermore, the extent of inflammation can be estimated by measuring the levels of cytokines such as IL-6 using specimens obtained via minimally invasive 27-gauge vitrectomy. Notably, perioperative complications are the same as previously reported. Thus, 27-gauge diagnostic vitrectomy was helpful in the management of posterior uveitis or panuveitis of unknown origin.
Availability of data and materials
The data generated and/or analyzed for this study are available from the corresponding author upon request.
References
Rathinam S, Namperumalsamy P. Global variation and pattern changes in epidemiology of uveitis. Indian J Ophthalmol. 2007;55(3):173–83.
Tsirouki T, Dastiridou A, Symeonidis C, Tounakaki O, Brazitikou I, Kalogeropoulos C, et al. A focus on the epidemiology of uveitis. Ocul Immunol Inflamm. 2018;26(1):2–16.
Abaño JM, Galvante PR, Siopongco P, Dans K, Lopez J. Review of epidemiology of uveitis in Asia: pattern of uveitis in a tertiary hospital in the Philippines. Ocul Immunol Inflamm. 2017;25(sup1):S75–80.
London NJ, Rathinam SR, Cunningham ET. The epidemiology of uveitis in developing countries. Int Ophthalmol Clin. 2010;50(2):1–17.
Zhang Y, Amin S, Lung KI, Seabury S, Rao N, Toy BC. Incidence, prevalence, and risk factors of infectious uveitis and scleritis in the United States: a claims-based analysis. PLoS One. 2020;15(8):e0237995.
Group SoUNW. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509–16.
Sugita S, Shimizu N, Watanabe K, Mizukami M, Morio T, Sugamoto Y, et al. Use of multiplex PCR and real-time PCR to detect human herpes virus genome in ocular fluids of patients with uveitis. Br J Ophthalmol. 2008;92(7):928–32. https://doi.org/10.1136/bjo.2007.133967 Epub 2008/04/15. PubMed PMID: 18408082; PubMed Central PMCID: PMCPMC2564807.
Sugita S, Ogawa M, Shimizu N, Morio T, Ohguro N, Nakai K, et al. Use of a comprehensive polymerase chain reaction system for diagnosis of ocular infectious diseases. Ophthalmology. 2013;120(9):1761–8. https://doi.org/10.1016/j.ophtha.2013.02.020 Epub 2013/05/15. PubMed PMID: 23664179.
Nakano S, Tomaru Y, Kubota T, Takase H, Mochizuki M, Shimizu N, et al. Evaluation of a multiplex strip PCR test for infectious uveitis: a prospective multicenter study. Am J Ophthalmol. 2020;213:252–9. https://doi.org/10.1016/j.ajo.2019.10.031 Epub 2019/12/01. PubMed PMID: 31785234.
Whitcup SM, de Smet MD, Rubin BI, Palestine AG, Martin DF, Burnier M Jr, et al. Intraocular lymphoma: clinical and histopathologic diagnosis. Ophthalmology. 1993;100(9):1399–406.
Coupland SE, Heimann H, Bechrakis NE. Primary intraocular lymphoma: a review of the clinical, histopathological and molecular biological features. Graefes Arch Clin Exp Ophthalmol. 2004;242(11):901–13.
Mochizuki M, Singh AD. Epidemiology and clinical features of intraocular lymphoma. Ocul Immunol Inflamm. 2009;17(2):69–72.
Coupland SE. The pathologist’s perspective on vitreous opacities. Eye (Lond). 2008;22(10):1318–29. https://doi.org/10.1038/eye.2008.31 Epub 2008/03/18. PMID: 18344965.
Wittenberg LA, Maberley DA, Ma PE, Wade NK, Gill H, White VA. Contribution of vitreous cytology to final clinical diagnosis fifteen-year review of vitreous cytology specimens from one institution. Ophthalmology. 2008;115(11):1944–50. https://doi.org/10.1016/j.ophtha.2008.05.022 Epub 2008/08/02. PubMed PMID: 18672292.
Mruthyunjaya P, Jumper JM, McCallum R, Patel DJ, Cox TA, Jaffe GJ. Diagnostic yield of vitrectomy in eyes with suspected posterior segment infection or malignancy. Ophthalmology. 2002;109(6):1123–9. https://doi.org/10.1016/s0161-6420(02)01033-3 Epub 2002/06/05. PubMed PMID: 12045054.
Kanavi MR, Soheilian M, Hosseini SB, Azari AA. 25-gauge transconjunctival diagnostic vitrectomy in suspected cases of intraocular lymphoma: a case series and review of the literature. Int J Ophthalmol. 2014;7(3):577–81. https://doi.org/10.3980/j.issn.2222-3959.2014.03.33 Epub 2014/06/27. PubMed PMID: 24967211; PubMed Central PMCID: PMCPMC4067679.
Mason JO, 3rd, Neimkin MG, Mason JOt, Friedman DA, Feist RM, Thomley ML, et al. Safety, efficacy, and quality of life following sutureless vitrectomy for symptomatic vitreous floaters. Retina. 2014;34(6):1055–61. Epub 2014/01/05. doi: https://doi.org/10.1097/iae.0000000000000063. PubMed PMID: 24384616.
Yeh S, Weichel ED, Faia LJ, Albini TA, Wroblewski KK, Stetler-Stevenson M, et al. 25-Gauge transconjunctival sutureless vitrectomy for the diagnosis of intraocular lymphoma. Br J Ophthalmol. 2010;94(5):633–8. https://doi.org/10.1136/bjo.2009.167940 Epub 2010/05/08. PubMed PMID: 20447965; PubMed Central PMCID: PMCPMC2928256.
Wu RH, Zhang R, Lin Z, Liang QH, Moonasar N. A comparison between topical and retrobulbar anesthesia in 27-gauge vitrectomy for vitreous floaters: a randomized controlled trial. BMC Ophthalmol. 2018;18(1):164. https://doi.org/10.1186/s12886-018-0838-7 Epub 2018/07/10. PubMed PMID: 29981573; PubMed Central PMCID: PMCPMC6035792.
Kimura K, Usui Y, Goto H. Clinical features and diagnostic significance of the intraocular fluid of 217 patients with intraocular lymphoma. Jpn J Ophthalmol. 2012;56(4):383–9. https://doi.org/10.1007/s10384-012-0150-7 Epub 2012/06/05. PubMed PMID: 22661396.
Johnson LN, Guy ME, Krohel GB, Madsen RW. Levodopa may improve vision loss in recent-onset, nonarteritic anterior ischemic optic neuropathy. Ophthalmology. 2000;107(3):521–6. https://doi.org/10.1016/s0161-6420(99)00133-5 Epub 2000/03/11. PubMed PMID: 10711891.
Davis JL, Miller DM, Ruiz P. Diagnostic testing of vitrectomy specimens. Am J Ophthalmol. 2005;140(5):822–9. https://doi.org/10.1016/j.ajo.2005.05.032 Epub 2005/11/29. PubMed PMID: 16310459.
Zhao XY, Xia S, Chen YX. Role of diagnostic pars plana vitrectomy in determining the etiology of uveitis initially unknown. Retina. 2020;40(2):359–69. https://doi.org/10.1097/iae.0000000000002372 Epub 2020/01/24. PubMed PMID: 31972807.
Kam AW, Galvin J, Cherepanoff S, Miller AA, Fung AT. Primary choroidal lymphoma diagnosed with 27-gauge pars plana vitrectomy choroidal biopsy. Case Rep Ophthalmol. 2019;10(2):213–20. https://doi.org/10.1159/000500238 Epub 2019/11/07. PubMed PMID: 31692619; PubMed Central PMCID: PMCPMC6760356.
Tang PH, Karkhur S, Nguyen QD. Obtaining undiluted vitreous sample using small gauge pars plana vitrectomy and air infusion. Am J Ophthalmol Case Rep. 2020;19:100768. https://doi.org/10.1016/j.ajoc.2020.100768 Epub 2020/07/09. PubMed PMID: 32637728; PubMed Central PMCID: PMCPMC7327279.
Oshima Y, Wakabayashi T, Sato T, Ohji M, Tano Y. A 27–Gauge instrument system for transconjunctival sutureless microincision vitrectomy surgery. Ophthalmology. 2010;117(1):93-102.e2. https://doi.org/10.1016/j.ophtha.2009.06.043.
Khan MA, Shahlaee A, Toussaint B, Hsu J, Sivalingam A, Dugel PU, et al. Outcomes of 27 gauge microincision vitrectomy surgery for posterior segment disease. Am J Ophthalmol. 2016;161:36-43.e2. https://doi.org/10.1016/j.ajo.2015.09.024.
Mitsui K, Kogo J, Takeda H, Shiono A, Sasaki H, Munemasa Y, et al. Comparative study of 27-gauge vs 25-gauge vitrectomy for epiretinal membrane. Eye. 2016;30(4):538–44.
Naruse S, Shimada H, Mori R. 27-gauge and 25-gauge vitrectomy day surgery for idiopathic epiretinal membrane. BMC Ophthalmol. 2017;17(1):1–7.
Otsuka K, Imai H, Fujii A, Miki A, Tagami M, Azumi A, et al. Comparison of 25-and 27-gauge pars plana vitrectomy in repairing primary rhegmatogenous retinal detachment. J Ophthalmol. 2018;2018:7643174.
Cunningham ET, Adán A, Nguyen QD, Zierhut M. Tocilizumab for the treatment of ocular inflammatory disease. Ocul Immunol Inflamm. 2021;29(1):2–5. https://doi.org/10.1080/09273948.2020.1859257 Epub 2021/01/13. PubMed PMID: 33434090.
Silpa-Archa S, Oray M, Preble JM, Foster CS. Outcome of tocilizumab treatment in refractory ocular inflammatory diseases. Acta Ophthalmol. 2016;94(6):e400-6. https://doi.org/10.1111/aos.13015 Epub 2016/03/25. PubMed PMID: 27010181.
Ahn JK, Yu HG, Chung H, Park YG. Intraocular cytokine environment in active Behçet uveitis. Am J Ophthalmol. 2006;142(3):429-34. e1.
Fisson S, Ouakrim H, Touitou V, Baudet S, Ben Abdelwahed R, Donnou S, et al. Cytokine profile in human eyes: contribution of a new cytokine combination for differential diagnosis between intraocular lymphoma or uveitis. PLoS One. 2013;8(2):e52385.
Vos AD, Hoekzema R, Kijlstra A. Cytokines and uveitis, a review. Curr Eye Res. 1992;11(6):581–97.
Chan C-C, Buggage RR, Nussenblatt RB. Intraocular lymphoma. Curr Opin Ophthalmol. 2002;13(6):411–8.
Ohta A, Ebihara N, Hiratsuka Y, Yokoyama T, Murakami A, Oshimi K. A clinical study of intraocular malignant lymphoma. Nippon Ganka Gakkai Zasshi. 2006;110(8):588–93 Epub 2006/09/16 PubMed PMID: 16972650.
Acknowledgement
Not applicable.
Funding
None of the authors has any proprietary or financial interests to declare.
Author information
Authors and Affiliations
Contributions
AS and MT wrote the main text of the manuscript and prepared the figures. Datasets were prepared by AS, MT, NM, MY, and SH. TK and SH reviewed the manuscript and verified the statistical analyses. All authors have read and approved the manuscript in its final form. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the Institutional and/or National Research Committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Approval for this study was obtained prior to the start of the study from the institutional review board at Osaka City University, Japan (IRB-4239). Written, informed consent for the storage of patient information in the hospital database and use in the research was provided by all patients enrolled in the study. Written, informed consent was obtained from a parent or guardian for participants under 16 years old.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sakai, A., Tagami, M., Misawa, N. et al. Safety and efficacy of 27-gauge transconjunctival vitrectomy for the diagnosis of posterior uveitis or pan uveitis of unknown origin. BMC Ophthalmol 22, 178 (2022). https://doi.org/10.1186/s12886-022-02405-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02405-y