Abstract
Background
To evaluate the ocular surface characteristics and the infestation of Demodex in Chinese paediatric and adult blepharokeratoconjunctivitis (BKC).
Methods
Fifty consecutive patients with BKC and 50 age- and sex-matched healthy subjects were enrolled. Lid margin characteristics and corneal disorders were evaluated under slit-lamp illumination. Four eyelashes were collected from each eye to examine Demodex infestation by light microscopy.
Results
Corneal neovascularization (P = 0.001) and scarring (P = 0.040) were significantly worse in children than in adults with BKC, whereas meibum quality was worse in adults (P = 0.008). Diagnosis delay was longer in children with BKC than in adults (2.2 vs 1.2 years, P = 0.022). Demodex infestation was more frequent in subjects with BKC than in healthy subjects (56% vs 26%, P = 0.002). The lid margin inflammation and meibomian gland dysfunction were worse in Demodex-positive subjects than in Demodex-negative subjects with BKC.
Conclusions
Children with BKC had severer corneal disorders compared with adult BKC patients, which may be caused by a long-delayed diagnosis. Ocular demodicosis was more common in subjects with BKC. Ocular Demodex infestation was associated with worse lid margin inflammation and meibomian gland dysfunction.
Similar content being viewed by others
Background
Blepharokeratoconjunctivitis (BKC) is a chronic and recurrent inflammatory disorder of the palpebral margin that is commonly associated with secondary conjunctival and corneal disorders [1, 2]. This disease is characterised by an inflamed lid margin (telangiectasia, thickening, and ulceration), meibomian gland dysfunction (MGD), and corneal disorders (punctate erosions, vascularisation, ulceration, and sometimes perforation) [3,4,5]. BKC affects the quality of life of patients, and due to the involvement of cornea, it may result in blindness [3, 5, 6]. However, BKC is often overlooked and misdiagnosed in the clinic [7, 8]. It was reported that BKC accounted for 12–25% of paediatric referrals for corneal diseases [9, 10]. But the delayed diagnosis is common, earlier studies showed the mean age at the onset of symptoms in children was 3.2–6.2 years and the mean age at diagnosis was 6.9–9.3 years [3, 5, 11]. So, the appropriate early diagnosis is very important in BKC. To understand the medical history and the ocular surface characteristics will be helpful for the early and correct diagnosis of BKC.
Demodex is a parasitic mite that lives in or near hair follicles and sebaceous glands. It was reported that Demodex was associated with chalazia, chronic blepharitis and MGD [12,13,14,15], as well as corneal manifestations such as corneal neovascularization, corneal infiltration, corneal opacity and scars, especially in patients with ocular rosacea [16]. However, there is scant research regarding its effect in BKC. Therefore, it will be valuable to examine the role of Demodex in the ocular surface changes of BKC.
In current study, we enrolled 50 consecutive BKC cases including children and adults to analyse the medical history and comprehensive ocular surface characteristics in BKC patients. We also compared the differences of clinical features between adult and pediatric BKC. Furthermore, we investigated the infestation of Demodex in BKC to evaluate the correlation between ocular Demodex and the ocular surface characteristics of patients with BKC.
Methods
Subjects
The study included 50 consecutive patients (50 eyes) who were first diagnosed with BKC at the Eye, Ear, Nose and Throat Hospital of Fudan University between April 2016 and March 2017. Patients were divided into two groups according to their age: patients aged ≤16 years were included in the paediatric group and patients aged > 16 years were included in the adult group. We also enrolled 50 age- and sex-matched healthy subjects (50 eyes) as a control group. All of the subjects were Chinese. The diagnostic criteria of BKC were as follows: (1) subjective symptoms, including tearing, photophobia, recurrent episodes of red eye, and (2) eyelid involvement, including anterior and/or posterior blepharitis (lid hyperemia, lid scaling or crusting, and lid margin hypertophy), chalazia and meibomitis; and (3) conjunctiva and cornea involvement, including conjunctivitis (conjunctival hyperemia, conjunctival chemosis, and conjunctival discharge), keratitis (superficial punctate keratopathy, corneal infiltration or ulceration), corneal vascularization, thinning, scarring or perforation. Subjects with other ocular surface diseases such as a history of atopy, vernal keratoconjunctivitis, or perennial allergic conjunctivitis, and a history of ocular surgery or systemic diseases that may affect ocular surface were excluded from the study. For the purpose of this study, we assessed the right eye or the affected eye in all subjects. Clinical data collection was approved by the Ethics Committee of Eye, Ear, Nose and Throat Hospital of Fudan University, in accordance with the Declaration of Helsinki.
Medical history
The main symptoms at the time of the examination, the age at onset, treatment history, and history of chalazion were recorded in all subjects with BKC.
Ocular examinations
All the subjects underwent slit-lamp examination, and ocular anterior segment photographs of the patients were taken. Ocular surface examinations included: (i) Tear breakup time (TBUT): The time before the first defect appeared on the stained tear film was recorded as the TBUT after the instillation of fluorescein. (ii) Schirmer’s I test (ST): Tear secretion test was measured by filter papers (Jingming New Technological Development Co. Ltd., Tianjin, China) placed in the lateral canthus for 5 min without topical anesthesia. (iii) Evaluation of corneal disorders: The corneal infiltration, ulceration, scarring and perforation was recorded. Corneal fluorescein staining of the upper, middle and lower parts of the cornea was assessed using a 4-point scale: no staining = 0; < 5 punctate stains = 1; 5 to < 10 punctate stains = 2; and 10 punctate stains or filamentous staining = 3. The total corneal staining score was determined as the summed score for all three parts, and ranged from 0 to 9 [17]. Corneal neovascularization was assessed on a range of 0–24 scale according to the number of quadrants affected, depth of involvement (superficial = anterior 1/3 of corneal thickness or deep = posterior 2/3) and location of vessels (peripheral = outer 1/3 of cornea, mid-peripheral = middle 1/3 and central = central 1/3). A score of 1 for each quadrant involved; a score of 1 was given for superficial vessels and 2 for deep vessels; and scores of 1, 2 and 3 for peripheral vessels, mid-peripheral vessels and central vessels respectively [18]. The lid margin was assessed to determine the presence of hyperaemia, telangiectasia and secretions (crusting and scaling on the eyelash). The meibomian gland was assessed in terms of meibum quality and meibum expressibility in accordance with the 2011 International Workshop on MGD [19]. Meibum quality was assessed in each of eight glands in the middle part of the lower eyelid, and scored on a 4-point scale: clear = 0; cloudy = 1; cloudy with particles = 2; and thickened, like toothpaste = 3. The scores for each eyelid were summed to generate a total score, which ranged from 0 to 24. Meibum expressibility was assessed in five glands in the middle parts of the lower eyelid with a 4-point scale according to the number of glands expressing meibum: all glands = 0; 3 or 4 glands = 1; 1 or 2 glands = 2; and no glands = 3. All examinations were completed by an experienced ophthalmologist at the same study site.
Assessment of Demodex infestation
Two eyelashes were removed from each eyelid on the points of trisection (four lashes from one eye) by forceps under a slit-lamp microscope. The lashes from each eyelid were placed separately on a glass slide and mounted with a coverslip. To improve the ability of detecting and counting mites, each slide was stained with fluorescein, by wetting a fluorescein strip (Jingming New Technological Development Co. Ltd., Tianjin, China) with a drop of 0.9% NaCl solution and applying the strip to the edge of the coverslip until the lash was immersed [20]. Demodex mites were counted under a light microscope at magnifications of 50× and 100×. Each slide was assessed within 1 h of sampling by another researcher who didn’t know the patient information.
Statistical analysis
All statistical analyses were performed using Stata 14.2 (StataCorp, College Station, TX, USA). Continuous variables are reported as the mean ± standard deviation. Categorical variables were recorded as the presence (yes) or absence (no), and reported as the number (percent) of subjects. Variables were compared between groups using Student’s t test, Wilcoxon’s rank-sum test, Pearson’s χ2 test, and Fisher’s exact test, as appropriate. In all analyses, P < 0.05 was considered statistically significant.
Results
Demographic characteristics and medical history
The paediatric BKC group included 18 patients (14 females and 4 males) with a mean age of 10.2 ± 3.8 years (range, 5–16 years). The adult BKC group included 32 patients (24 females and 8 males) with a mean age of 28.8 ± 7.1 years (range, 17–50 years). The paediatric control group included 17 children (12 females and 5 males) with a mean age of 9.3 ± 2.7 years (range, 6–16 years). The adult control group included 33 adults (22 females and 11 males) with a mean age of 32.2 ± 9.3 years (range, 17–52 years). The control and BKC groups were comparable in terms of the age and gender of subjects. Red eye was the main symptom in both groups, and was reported in 14/18 and 23/32 subjects, respectively. Recurrent chalazia affected 15/18 and 29/32 of subjects in the paediatric and adult BKC groups, respectively. The mean age of BKC related symptom onset was 7.9 ± 3.9 years in the paediatric group and 27.6 ± 7.5 years in the adult group; the mean diagnosis delay was 2.2 years and 1.2 years in the paediatric and adult BKC groups, respectively (P = 0.022). Before the diagnosis of BKC, many of the subjects had been diagnosed with viral keratitis or conjunctivitis; antiviral drugs had been prescribed to 29% of children and 28% of adults. The demographic characteristics and medical history of the paediatric and adult BKC groups are summarized in Table 1.
Clinical examination parameters
Adult BKC vs adult controls
TBUT was shorter in the adult BKC group than in the adult control group (P < 0.001), but the Schirmer I test was not significantly different among the two groups. The corneal staining score was significantly greater in adult BKC groups (P < 0.001). Regarding meibomian gland characteristics, the meibum quality and expressibility scores were significantly (both P < 0.001) worse in adult patients with BKC than in the respective control group.
Paediatric BKC vs paediatric controls
Comparison between children with BKC and those without found results similar to adult ones. Paediatric patients with BKC had a shorter TBUT and worse score of corneal staining, as well as poor meibum quality and meibum expressibility (all P < 0.001).
Paediatric BKC vs adult BKC
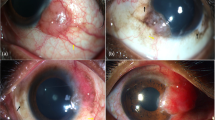
Paediatric patients with BKC had a longer Schirmer’s I test result than the adult BKC group, but similar result was also found in child and adult controls. Regarding corneal disorders, corneal neovascularization (P = 0.001) and scarring (P = 0.040) were significantly worse in the paediatric BKC group than in the adult BKC group. Lid margin characteristics were not significantly different between the paediatric and adult BKC groups, except for the meibum quality score, which was significantly worse in the adult BKC group than in the paediatric BKC group (P = 0.008). Comparison of ocular surface characteristics between pediatric and adult BKC is summarized in Table 2 and representative slit-lamp photographs are shown in Fig. 1.
Demodex infestation and the clinical characteristics of BKC
Demodex infestation was more frequent in subjects with BKC than in healthy subjects (56% vs 26%, P = 0.002). We divided the 50 BKC patients into Demodex-positive and Demodex-negative groups, and the characteristics of both groups are shown in Table 3. The Demodex-positive group (28 patients) comprised 24 females and 4 males, and the mean age was 23.8 ± 10.9 years (range, 6–50 years). The Demodex-negative group (22 patients) comprised 14 females and 8 males, and the mean age was 19.9 ± 10.7 years (range, 5–38 years). TBUT and the corneal neovascularization score were not significantly different between Demodex-positive and Demodex-negative groups. However, the corneal fluorescein staining score was significantly greater in the Demodex-positive group than in the Demodex-negative group (P = 0.0015). Lid margin secretion (P = 0.013) was more common in the Demodex-positive group than in the Demodex-negative group. There were also significant differences in lid margin hyperemia and telangiectasia (P = 0.033 and 0.016, respectively), as well as meibum quality and expression scores (P = 0.019 and 0.028, respectively) between the Demodex-positive and Demodex-negative groups. Recurrent chalazion was more prevalent in the Demodex-positive group, although the difference was not statistically significant.
Discussion
BKC is a chronic and recurrent inflammatory disease affecting the palpebral margin, and is accompanied with conjunctival and corneal lesions. BKC has a variety of manifestations, even neovascularization and scarring in severe cases, which may lead to impaired visual acuity. However, misdiagnosis or delayed diagnosis are common in BKC [3, 9]. In current study, we gave comprehensive examination on 50 consecutive patients with BKC to evaluate the characteristics of medical history and clinical symptoms. We also compared the difference of clinical parameters between adult and paediatric BKC patients. Furthermore, we investigated the potential role of ocular Demodex in this disease as well.
The gender distribution of BKC is inconsistent in different studies. A study of predominantly Caucasian patients found no difference in the proportion of males and females with BKC [9]. Another study of Asian children with BKC reported that 80% of the patients were female [21]. In current study, females accounted for a greater proportion of the enrolled BKC cohort than males among both children and adults. Considering these findings, the difference in gender distribution of BKC may be related to race. BKC seems to be prone to attack female in Asian. When we considered the mean age of patients, we found the mean age of paediatric and adult BKC in current study was 10.2 ± 3.8 and 28.8 ± 7.1 years respectively, which indicated BKC is more common in young female in Asian.
Delayed diagnosis in paediatric BKC attracted much more attention. In prior studies of paediatric BKC, the authors reported a delay between the onset and the correct diagnosis and treatment ranging from 1.3 to 2.4 years [3, 4, 9, 22]. In current study, we had a similar founding. We found the mean delay of diagnosis of BKC in children was about 2.2 years. And, even in adult, there is still a delay with 1.2 years, which suggests that the diagnosis of BKC is easy to be delayed in both children and adults. When we looked further the medical history of our subjects, we found viral keratitis and conjunctivitis were two common primary diagnoses in our patients. It was believed that herpes simplex virus keratitis was the most frequent misdiagnosis in patients with BKC [11]. In our study, 29% of children and 28% of adults received an anti-virus treatment before the diagnosis of BKC, indicating a previous misdiagnosis of virus keratitis. Because the long term and frequent use of anti-virus eye drops could destroy the ocular surface, the anti-virus treatment might aggravate the ocular surface damage of BKC, which indicates the importance of early correct diagnosis of BKC. The ignorance on the examination of eyelid margin might be the most important reason for the delayed diagnosis of BKC. On the other hand, the high incidence of recurrent chalazia in both paediatric and adult BKC groups indicated the recurrent chalazia could be a helpful clue for considering the diagnosis of BKC.
In current study, we compared the difference of clinical parameters between paediatric and adult BKC. We found the paediatric group had a higher corneal neovascularization score and worse corneal scarring than the adults. The severer corneal disorder in children BKC may be associated with the longer diagnostic delay and inappropriate primary treatment. It also indicated the possibility of different physiopathology between paediatric and adult BKC patients. It was reported that the effect on vision in children with BKC was more marked than one would expect in adults [3]. The authors believed that children may be more susceptible to corneal disorders from the inflammatory and immune response to periocular bacteria. However, the potentially different susceptibility and mechanism between paediatric and adult patients with BKC still needs further study. In spite of the less cooperativity in examination, lid margin examination still must be done in paediatric patients who complained chronic red eye, and especially when the patients had a history of recurrent chalazia. Many studies have reported that paediatric and adult BKC patients had worse meibomian gland function than people without BKC [3, 6, 23, 24]. Consistent with these earlier findings, the scores of meibum quality and meibum expression were significantly worse in both paediatric and adult BKC groups than that in the control groups in current study. However, except worse meibum quality in the adult BKC group, there was no significant difference in other lid margin parameters between the paediatric and adult BKC. Considering the worse corneal neovascularization and scarring in the paediatric BKC group, we think that the severity of corneal involvement may not be associated with the grade of lid margin inflammation. The association between the lid margin disorder and the corneal disorders still need further study to explore the potential physiopathology and specific treatments in paediatric BKC.
Demodex commonly congregates in eyelash follicles, sebaceous glands, including meibomian glands. It has been reported that Demodex plays an important role in blepharitis and ocular surface irritation [25,26,27] . However, there are still some researchers reported that the rate and extent of Demodex infestation was not significantly different between healthy people and patients with blepharitis [28]. In present study, 56% of patients with BKC were Demodex positive, with a statistically significant difference compared to 26% of the control group. The Demodex-positive patients had severer lid margin hyperaemia, telangiectasia, and secretion, and had worse meibomian gland function, which indicated that Demodex may be associated with the severity of lid margin disorders in BKC. The lid margin inflammation may be fortified by Demodex as a vector for bacteria [29] and via delayed hypersensitivity reactions [30]. Kheirkhah et al. [16] reported that patients with Demodex blepharitis presented with corneal staining and neovascularization, both of which were significantly reduced after treating the lid with tea tree oil to kill ocular Demodex [31]. However, current study only showed worse corneal staining in the Demodex-positive patients with BKC, there was no obvious difference in other corneal disorder parameters between the Demodex-positive and Demodex-negative BKC patients. Based on the findings, we speculated that the increased infestation of Demodex in BKC might be secondary to the lid margin disorder and conversely it could aggravate the lid margin and corneal disorders. So, the infestation of Demodex should be considered when we diagnose and treat the BKC.
Our study had several limitations. Although the lash sampling and microscopic examination was commonly used to identify the mites in the lashes, especially easy performed on children, it may miss the Demodex accumulated in the follicles of eyelashes. In vivo confocal microscopy (IVCM) may provide a more complete examination of the follicles [32]. Another consideration is that the reliability of meibomian glands examinations in paediatric patients which should be interpreted with caution. Moreover, although the simple slit-lamp analysis could partially elucidate the lid margin and corneal physiopathology of BKC, for further understanding the physiopathology mechanism of BKC, the analysis of tear of impression cytology will be necessary in the future study.
Conclusions
In conclusion, we gave a comprehensive examination on the medical history and clinical parameters of 50 consecutive paediatric and adult BKC patients. We found that children with BKC had severer corneal disorders and longer delayed diagnosis compared with adult BKC patients. Ocular demodicosis was more common in subjects with BKC. Ocular Demodex infestation was associated with worse lid margin inflammation and meibomian gland dysfunction in BKC patients. Based on these findings, we thought a future study with a larger number of patients will be necessary to reveal the association between the lid margin disorders and the corneal disorders, and to identify the specific role of Demodex on the clinical parameters in BKC. Further study with the support of impression cytology and IVCM is also necessary to investigate the possibly different physiopathology mechanism between paediatric and adult BKC.
Abbreviations
- BKC:
-
Blepharokeratoconjunctivitis
- IVCM:
-
In vivo confocal microscopy
- MGD:
-
Meibomian gland dysfunction
- ST:
-
Schirmer’s I test
- TBUT:
-
Tear breakup time
References
McCulley JP, Dougherty JM, Deneau DG. Classification of chronic blepharitis. Ophthalmology. 1982;89(10):1173–80.
O'Gallagher M, Bunce C, Hingorani M, et al. Topical treatments for blepharokeratoconjunctivitis in children. Cochrane Database Syst Rev. 2017;2:CD011965.
Jones SM, Weinstein JM, Cumberland P, et al. Visual outcome and corneal changes in children with chronic blepharokeratoconjunctivitis. Ophthalmology. 2007;114(12):2271–80.
Viswalingam M, Rauz S, Morlet N, et al. Blepharokeratoconjunctivitis in children: diagnosis and treatment. Br J Ophthalmol. 2005;89(4):400–3.
Rodriguez-Garcia A, Gonzalez-Godinez S, Lopez-Rubio S. Blepharokeratoconjunctivitis in childhood: corneal involvement and visual outcome. Eye (Lond). 2016;30(3):438–46.
Hamada S, Khan I, Denniston AK, et al. Childhood blepharokeratoconjunctivitis: characterising a severe phenotype in white adolescents. Br J Ophthalmol. 2012;96(7):949–55.
Mehta JS, Sagoo MS, Tuft SJ. Subconjunctival crystals in paediatric blepharokeratoconjunctivitis. Acta Ophthalmol Scand. 2006;84(4):557–8.
Suzuki T, Kinoshita S. Meibomitis-related keratoconjunctivitis in childhood and adolescence. Am J Ophthalmol. 2007;144(1):160–1 author reply 1.
Hammersmith KM, Cohen EJ, Blake TD, et al. Blepharokeratoconjunctivitis in children. Arch Ophthalmol. 2005;123(12):1667–70.
Gupta N, Dhawan A, Beri S, et al. Clinical spectrum of pediatric blepharokeratoconjunctivitis. Journal of AAPOS. 2010;14(6):527–9.
Hammersmith KM. Blepharokeratoconjunctivitis in children. Curr Opin Ophthalmol. 2015;26(4):301–5.
Liang L, Ding X, Tseng SCG. High prevalence of demodex brevis infestation in chalazia. Am J Ophthalmol. 2014;157(2):342–8 e1.
Yam JCS, Tang BSF, Chan T-M, et al. Ocular demodicidosis as a risk factor of adult recurrent chalazion. Eur J Ophthalmol. 2014;24(2):159–63.
Coston TO. Demodex folliculorum blepharitis. Trans Am Ophthalmol Soc. 1967;65:361–92.
English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981;91(3):362–72.
Kheirkhah A, Casas V, Li W, et al. Corneal manifestations of ocular demodex infestation. Am J Ophthalmol. 2007;143(5):743–9.
Toda I, Tsubota K. Practical double vital staining for ocular surface evaluation. Cornea. 1993;12(4):366–7.
Faraj LA, Said DG, Al-Aqaba M, et al. Clinical evaluation and characterisation of corneal vascularisation. Br J Ophthalmol. 2016;100(3):315–22.
Tomlinson A, Bron AJ, Korb DR, et al. The international workshop on meibomian gland dysfunction: report of the diagnosis subcommittee. Invest Ophthalmol Vis Sci. 2011;52(4):2006–49.
Kheirkhah A, Blanco G, Casas V, et al. Fluorescein dye improves microscopic evaluation and counting of demodex in blepharitis with cylindrical dandruff. Cornea. 2007;26(6):697–700.
Teo L, Mehta JS, Htoon HM, et al. Severity of pediatric blepharokeratoconjunctivitis in Asian eyes. Am J Ophthalmol. 2012;153(3):564–70.
Doan S, Gabison EE, Nghiem-Buffet S, et al. Long-term visual outcome of childhood blepharokeratoconjunctivitis. Am J Ophthalmol. 2007;143(3):528–9.
Suzuki T, Teramukai S, Kinoshita S. Meibomian glands and ocular surface inflammation. The ocular surface. 2015;13(2):133–49.
Yin Y, Gong L. The evaluation of meibomian gland function, morphology and related medical history in Asian adult blepharokeratoconjunctivitis patients. Acta Ophthalmol. 2017;95(6):634–8.
Kabatas N, Dogan AS, Kabatas EU, et al. The effect of Demodex infestation on blepharitis and the ocular symptoms. Eye Contact Lens. 2017;43(1):64–7.
Nicholls SG, Oakley CL, Tan A, et al. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol. 2017;37(1):303–12.
Liang L, Safran S, Gao Y, et al. Ocular demodicosis as a potential cause of pediatric blepharoconjunctivitis. Cornea. 2010;29(12):1386–91.
Kemal M, Sumer Z, Toker MI, et al. The prevalence of Demodex folliculorum in blepharitis patients and the normal population. Ophthalmic Epidemiol. 2005;12(4):287–90.
English FP, Iwamoto T, Darrell RW, et al. The vector potential of Demodex folliculorum. Arch Ophthalmol. 1970;84(1):83–5.
Liu J, Sheha H, Tseng SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505–10.
Gao Y-Y, Di Pascuale MA, Li W, et al. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br J Ophthalmol. 2005;89(11):1468–73.
Randon M, Liang H, El Hamdaoui M, et al. In vivo confocal microscopy as a novel and reliable tool for the diagnosis of Demodex eyelid infestation. Br J Ophthalmol. 2015;99(3):336–41.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural Science Foundation for Young Scientists of China (No. 81100636). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The dataset supporting the conclusions of this study is available in the Additional file 1.
Author information
Authors and Affiliations
Contributions
Design of the study (MW, YW); data collection (YW, JH); statistical analysis (MW, XW); preparation of the manuscript (MW, XW, YW); critical revision (TS, YW). All authors read and approved the manuscript to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This cross-sectional study was approved by the ethics committee of Eye, Ear, Nose and Throat Hospital of Fudan University (No.2015010), and written informed consent was obtained from all patients or their parent if they were under the age of sixteen.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Raw data for BKC study. Clinical data of ocular surface characteristics in controls and BKC patients. (XLSX 17 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wu, M., Wang, X., Han, J. et al. Evaluation of the ocular surface characteristics and Demodex infestation in paediatric and adult blepharokeratoconjunctivitis. BMC Ophthalmol 19, 67 (2019). https://doi.org/10.1186/s12886-019-1074-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-019-1074-5