Abstract
Background
Myopia-related maculopathy is one of the leading causes of blindness in the world. The prevalence of myopia has been reported as high as 90 % in some Asian countries. Therefore, controlling myopia progression is an urgent public issue. The purpose of this study is to evaluate the effects of topical atropine with different concentrations on intraocular pressure measurements and myopia progression in school-aged children in Taiwan.
Methods
Fifty-six myopic children were divided into three groups: 32 children were treated with 0.125 % atropine eyedrop; 12 of them were treated with 0.25 % atropine eye drop and another 12 served as a control group. IOP, auto-refractor and manifest refraction were measured at baseline and every 3 months following treatment for one year.
Results
There were no significant differences for the mean age, gender and baseline IOPs among the three groups. During the follow up period, no significant IOP difference was found among three groups. The change between final and baseline mean IOPs also revealed no significant differences: 0.54 mmHg, −1.28 mmHg, −0.33 mmHg for the 0.125 % atropine, 0.25 % atropine and control groups. The baseline mean spherical equivalent similarly did not differ significantly among groups but the control group showed a significant myopic progression compared to the 0.125 % atropine group 6 months after treatment, and persisted for one year. The change between final and baseline mean spherical equivalents were −0.05 D, 0 D, −1.05 D for the 0.125 % atropine, 0.25 % atropine and control groups, with both atropine-treated groups showing significant myopic retardation compared to the control group.
Conclusions
Topical use of low concentration atropine for one year does not induce ocular hypertension and is effective for retarding myopic progression. However, further large scale studies with longer follow up period is necessary to validate the long term safety and efficacy.
Trial registration
ISRCTN33002849, 2016/01/19, retrospectively registered.
Similar content being viewed by others
Background
Myopia is a disease that was described two thousand years ago, and some physicians in Italy in the 16th century even started to use bifocal lenses as a tool to help people with myopia to see more clearly [1]. Currently, multiple interventions or management are designed to control the progression of myopia. Common effective methods for retarding myopic progression include spectacles (bifocals and multi-focal), ocular hypotensive medications, and contact lenses (including orthokeratology lenses) [1–3]. Atropine, a muscarinic receptor antagonist, has been successfully used to prevent progression of myopia in Taiwan since 1997 [4] and several clinical trials also demonstrated its effectiveness for reducing myopic progression compared with other medications and managements [1, 5–9]. In fact, topical atropine has become a mainstream of myopic treatment throughout eastern and south-eastern Asia [1, 5, 6, 8, 9].
However, some people suspect that the side effects caused by atropine will harm eyes. The side effects of topical atropine can be divided into two types: short-term and long-term effects. The short-term side effects include red eyes, photophobia, blurred vision, allergic dermatitis, risk of increase intraocular pressure (IOP) and angle closure glaucoma [1, 10–12]. The development of drug-induced acute angle closure glaucoma (AACG) by atropine was reported by Lachker et al. [10] but Greensteinet al. [13] pointed out that anti-muscarinic drugs such as atropine will not contribute to AACG unless there are predisposing factors such as a shallow anterior chamber and pupil-dilating medications. However, whether atropine leads to elevated intraocular pressure remains uncertain. The long-term side effects of atropine is also a mystery, though some proposed that prolonged ultraviolet light exposure due to the mydriatic effect of atropine could lead to several types of ocular damage, such as retinal vascular disease and cataract formation [14, 15]. In addition, previous reports also demonstrated that atropine may lead to drug-induced amnesia, impaired memory function, somnolence and seizure [16–18] so long-term administration should be cautious. Yet cataract or retinal diseases has not been proven in previous studies which continuously applied atropine with a follow up of 2 years [5, 12]. However, the safety profile of long-term atropine administration certainly deserves large scale and long term surveys.
Still, the relationship between the concentration of atropine and its effect on retarding myopia has not been elucidated. One study revealed that topical atropine with 1 % concentration is an effective method to prevent myopic progression; [6] however, other studies demonstrated that myopia could be successfully retarded with low concentration atropine eye drops, ranging from 0.01 % to 0.1 % [19, 20]. For these reasons, further evaluation of the effect of different concentrations of topical atropine on myopia progression is necessary.
Therefore, the aim of this study is to evaluate the effect of different concentrations of topical atropine on retarding the progression of low myopia and the measurements of intraocular pressures in school-aged children in Taiwan.
Methods
Patient group selection
This prospective, interventional, longitudinal and non-randomized study was conducted at Keelung Chang Gung Memorial Hospital, Taiwan. The study group consisted of 56 children in Northern Taiwan ranging in age from 6 to 12 years. The exclusion criteria included: [1] congenital eye disorder, [2] any disease influence the cornea, lens or retina, [3] best correct visual acuity < 20/25 using the Snellen chart, [4] primary intraocular pressure above 21 mmHg, [5] atropine application within 6 months before enrollment, and [6] patients who could understand the details of this study or could not adhere to the follow up schedule. Patients with a refractive error less than −3.0 diopters (D) were enrolled in this study and only the right eye of each subject was analyzed to prevent effect of atropine on the contra-lateral eye. For those participants who were willing to receive atropine treatment, we randomly assigned them to either 0.125 % atropine group or 0.25 % atropine group by drawing lots. Those who preferred spectacles for correcting myopia were enrolled in the control group without any eyedrop use during the study. After removing those participants that loss follow-up or being absent in at least 1 clinic visiting, we divided the participants into three groups. The first group, treated with 0.125 % atropine, consisted of 32 children (17 boys and 15 girls); the second group using 0.25 % atropine included 12 children (4 boys and 8 girls); and an additional 12 children (6 boys and 6 girls) in the control group. The intraocular pressures and spherical equivalent were measured every 3 months during the study period for one year.
Atropine administration
Two topical atropine sulphate eye drops were used in this study: 0.125 % and 0.25 % (both from Wu-Fu Laboratories Co, Ltd, Yilan, Taiwan). The concentration we used was the original concentration from the pharmacological corporation. No dilution or condensation happened during the whole study and no patient shared the same bottle of atropine. The research program was halted if severe allergic reaction happened to the patients, and the proper management was subsequently arranged by medical professionals. The control group did not receive any placebo eye drop in this study.
Ocular examination
All children were examined by the same technician (Y. F. Lin) for the measurement of intraocular pressure and the manifest refraction examinations during the study period. The slit-lamp biomicroscopy and fundoscopic examinations revealed normal status except for the refractive errors before the study. Because of rapid measurement and a good correlation with Goldmann applanation tonometer [21], we used a pneumatic tonometer (NT-530P, Nidek Co., Ltd, Gamagori, Japan) to measure the IOP in our patients. Each patient received 3 measurements and the average of those measurements was the final IOP. The spherical equivalent was measured and calculated by a Topcon auto-keratorefractometer (KR-3000, Topcon, Yamagata, Japan). All the refractions were performed under cycloplegic condition. If there was an elevation of IOP more than 5 mmHg compared to baseline, severe allergic reactions or other ocular side effects, we immediately halted the atropine application and withdrew the patient from this study. Our subject wore spectacle and no contact lens, progressive or photochromic lenses were applied during the whole follow up period.
Statistical analysis
All statistical analyses were conducted using SPSS software version 19 (SPSS Inc., Chicago, Illinois, USA). The gender and age among groups were evaluated by the Chi-square test and One-way ANOVA sequentially. For the comparisons of IOP and refractive errors within each group during different time periods, the pair-t test was applied. While comparing the IOP as well as refractive errors among the three groups, we analyzed the variance first. If the variances among the three groups were homogenous, we used One-way ANOVA for analysis and added Bonferroni test for post-hoc analysis. But if the variances among the three groups were heterogenous, we used Welch’s test for analysis and added Dunnett T3 test for post-hoc analysis. Confidence intervals of 95 % were regarded as a comparison for mean values and p < 0.05 was considered statistically significant in pair-t test, Chi-square, One-way ANOVA and Welch’s test but <0.025 in Bonferroni test and Dunnett T3 test since we need to reduce the family-wise error in post-hoc exam.
Results
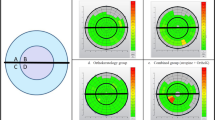
The mean age was 9.03, 8.16 and 8.33 years for the 0.125 % atropine, 0.25 % atropine and control groups, respectively. There was no statistical significance for both gender and age (p = 0.50 and 0.37, Chi-square test and One-way ANOVA sequentially) among the three groups. The baseline mean intraocular pressure initially was 13.90 ± 3.26 mmHg in the 0.125 % atropine group, 14.91 ± 3.09 mmHg in the 0.25 % atropine group and 14.50 ± 2.43 mmHg in the control group, respectively. The mean IOP measurements and the statistical analyses among the groups during the follow up period are shown in Table 1. All three groups demonstrated no significant difference between group comparisons at each time point during the study period (Table 1). In addition, with the exception of the 0.25 % atropine group which showed a significant difference (p = 0.03) at 3 months, all three groups during the follow up period demonstrated no statistically significant difference as compared to their baseline IOPs (Fig. 1). The data, demonstrated that a low concentration of atropine use for one year in school-aged children for myopia control did not induce IOP elevation.
The baseline mean spherical equivalent was −1.22 ± 0.55 D in the 0.125 % atropine group, −1.45 ± 0.69 D in the 0.25 % atropine group and −1.45 ± 1.00 D in the control group, which means none of the groups significantly differed from the others (p > 0.05). The mean spherical equivalents and the statistical analyses among the groups during the follow up period are presented in Table 2. The mean progression of myopia, i.e., the change of spherical equivalent, was −0.05 D in the 0.125 % atropine group, 0 D in the 0.25 % atropine group and 1.05 D in the control group. We found that the spherical equivalents in the atropine groups remained stable (no significant difference either between 0.125 % and 0.25 % atropine groups or compared to their baseline spherical equivalent at any time point). However, significant progression of myopia was noted in the control group compared to the 0.125 % atropine group (from 6-month after treatment till one year) and to the 0.25 % group (one year) (Fig. 2, p < 0.05). Moreover, a significant difference in spherical equivalent among three groups was also noted from 6 months to 12 months with the final refractive errors of −1.27 ± 0.85 D in the 0.125 % atropine group, −1.45 ± 1.00 D in the 0.25 % atropine group and −2.50 ± 1.31 D in the control group after treatment (Table 2, p = 0.03, <0.01 and <0.01, respectively, One-way ANOVA), indicating that atropine treatment effectively controlled myopia progression.
Discussion
Myopia is one of the most common causes of low vision in the world [22] and Chinese children and other Asian populations are more vulnerable to developing myopia, as compared to white populations, especially those who live in urban regions [22–24]. In Taiwan, the myopic group accounts for a large percentage of school-age children, similar to the Chinese population [22, 25]. The anti-accommodation property of atropine was believed to retard myopic progression [26], but it has recently been demonstrated that atropine retards myopia mainly via a non-accommodative mechanism by regulating the muscarinic receptor of the retina, choroid and sclera tissues [27–32]. Accumulating evidence has shown that topical atropine is effective in retarding myopic progression [1, 5, 8, 12, 33]. Kennedy et al. [34] revealed that mean myopic progression during atropine treatment was 0.05 D per year, whereas the control group had an annual progression of 0.36 D. Moreover, Chua et al. concluded that atropine not only retards the progression of myopia but also reduces the axial length elongation [5]. In our study, the mean progression of myopia evidenced no significant difference compared to the baseline in the 0.125 % and 0.25 % atropine groups, though the control group showed a significant progression (p < 0.01) during the follow up period. Our study is consistent with others, implying that atropine treatment may prevent myopia progression.
It was also demonstrated that a higher concentration of atropine use results in better myopia control [5, 6, 8, 35] Fan et al. used 1 % atropine and found that progression of myopia was +0.06 ± 0.79 D in the treatment group versus-1.19 ± 2.48 D in control group per year [6]. Chua et al. also reported a 0.92 D difference in myopic progression between the treatment group (1 % atropine) and control group [5]. In addition, Song et al. demonstrated that high concentrations (0.5 % and 1 %) were more effective to retard myopia progression than lower concentrations (0.05 %, 0.1 % and 0.25 %) [8]. A similar study by Shih et al. showed that 61 % of patient in the 0.5 % atropine group had no myopia progression, compared to 49 % in 0.25 % atropine group and 42 % in 0.1 % atropine group, thus indicating that higher concentrations are more effective [35]. However, side effects such as mydriasis, photophobia, blurred vision and allergic dermatitis by high concentration atropine have been reported [1, 7] which may limit the medication compliance [35] and impose psychological burdens on the parents. Cooper et al. demonstrated that 0.02 % atropine is the maximum dose that would not induce clinical symptoms [36], and for this reason, low atropine dose should probably be considered so as to limit adverse effects. In addition, lower concentrations of atropine may also effectively retard myopia progression even at a concentration of 0.01 % [20]. In our study, we found no significant difference between the 0.125 % atropine and 0.25 % atropine groups (p > 0.025) with a mean myopic progression of −0.05D in the 0.125 % atropine group and 0D in 0.25 % atropine group for the one year follow up period. Taken together, we recommend that a low concentration atropine should be considered first in terms of retarding myopia progression and avoiding intolerable side effects.
One of the controversial side effects of atropine is its anti-cholinergic effect that leads to drug-induced acute angle closure glaucoma [10]. Although Herring et al. [37] found an IOP decrease in horse eyes after 1 % topical atropine use, Stadtbaumer [38] observed an IOP elevation in feline eyes from the same medication. The same inconsistency was also noted in human eyes. Harris et al. showed that atropine may lead to the elevations of IOP up to 23 % in proven open-angle glaucoma, but only 2 % in an apparently normal population [39]. Hadjikoutis et al. suggested careful use of atropine in neurological operation to prevent elevated IOP and angle closure glaucoma in susceptible patients [40]. However, the threshold concentration that may lead to such side effects was not disclosed in these studies. In a large scale study, Wu et al. [41] analyzed 621 myopic children with atropine dosages ranging from 0.1 % to 1 % and concluded that neither the duration of treatment nor cumulative dose of atropine would statistically elevate IOP. In our study, there was no IOP elevation in atropine treatment groups compared to either baseline measurements or to control group during the one year follow up. Though our results were consistent with those of Wu et al., our study was prospective-designed while their study was retrospective in nature. In addition, we used the average data of three measurements from every visit compared to only one digital reading by Wu et al., which may have increased their measurement errors. Therefore, these studies on school-aged children do not support the linkage between atropine use and the elevation of IOP in normal eyes.
It would be interesting to know if there is any relationship between intraocular pressure and myopia progression. Jensen et al. [42] concluded that IOP-lowering eye drops demonstrated no effectiveness on retarding myopic progression and indicated that IOP has no significant relation with myopia progression. However, a later study conducted by the same team revealed that if IOP was above 16 mmHg, a statistically significant difference of myopia progression would appear (1.32D in 2 years versus 0.86D in 2 years) [43]. The authors thus suggested using IOP measurements in studying myopia progression. A more recently study revealed that IOP would elevate after onset of myopia [44], though the relationship between IOP and refractive error remain unclear [45]. Our study did not evidence the relationship between IOP elevation and myopic progression in one year period, which probably because myopia progression was reduced in the 0.25 % and 0.125 % atropine groups. However, one should keep in mind that myopia may lead to IOP elevation and current study only showed that atropine didn’t contribute to IOP elevation. Therefore, further long-term study is mandatory to investigate the incidence and risk factors of myopic-induced glaucoma.
There are some limitations in our study. First, this study is not a double-blind randomized design. Second, the small sample size and relatively short follow up time are noted in our study. Long term side effects may be apparent in a long period of follow up.
Conclusions
In conclusion, when it comes to the elevation of intraocular pressure, there was no evidence that ocular hypertension would be increased by the application of atropine for one year in this study. Similar to other studies, topical atropine eye drop is effective in slowing the progression of low to moderate myopia even with a low concentration of 0.125 %. Therefore, low concentration atropine may be used in clinical practice to retard myopia. However, randomized controlled clinical trials with a large sample size and long follow up should be conducted in the future to validate our results.
Abbreviations
IOP, intraocular pressure; AACG, acute angle closure glaucoma; D, Diopter; SD, Standard deviation; GH, growth hormone
References
Saw SM, Gazzard G, Au Eong KG, Tan DT. Myopia: attempts to arrest progression. Br J Ophthalmol. 2002;86:1306–11.
Gwiazda J. Treatment options for myopia. Optom Vis Sci. 2009;86:624–8.
Cooper J, Schulman E, Jamal N. Current status on the development and treatment of myopia. Optometry. 2012;83:179–99.
Chou AC, Shih YF, Ho TC, Lin LL. The effectiveness of 0.5 % atropine in controlling high myopia in children. J Ocul Pharmacol Ther. 1997;13:61–7.
Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113:2285–91.
Fan DS, Lam DS, Chan CK, Fan AH, Cheung EY, Rao SK. Topical atropine in retarding myopic progression and axial length growth in children with moderate to severe myopia: a pilot study. Jpn J Ophthalmol. 2007;51:27–33.
Leo SW, Young TL. An evidence-based update on myopia and interventions to retard its progression. J AAPOS. 2011;15:181–9.
Song YY, Wang H, Wang BS, Qi H, Rong ZX, Chen HZ. Atropine in ameliorating the progression of myopia in children with mild to moderate myopia: a meta-analysis of controlled clinical trials. J Ocul Pharmacol Ther. 2011;27:361–8.
Fang YT, Chou YJ, Pu C, Lin PJ, Liu TL, Huang N. Prescription of atropine eyedrops among children diagnosed with myopia in Taiwan from 2000 to 2007: a nationwide study. Eye (Lond). 2013;27:418–24.
Lachkar Y, Bouassida W. Drug-induced acute angle closure glaucoma. Curr Opin Ophthalmol. 2007;18:129–33.
Ganesan P, Wildsoet CF. Pharmaceutical intervention for myopia control. Expert Rev Ophthalmol. 2010;5:759–87.
Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5 %, 0.1 %, and 0.01 % doses (Atropine for the Treatment of Myopia 2). Ophthamology. 2012;119:347–54.
Greenstein SH, Abramson DH, Pitts 3rd WR. Systemic atropine and glaucoma. Bull N Y Acad Med. 1984;60:961–8.
Kao SC, Lu HY, Liu JH. Atropine effect on school myopia. A preliminary report. Acta Ophthalmol Suppl. 1988;185:132–3.
Walsh JE, Bergmanson JP. Does the eye benefit from wearing ultraviolet-blocking contact lenses? Eye Contact Lens. 2011;37:267–72.
Balakrishnan S, Pearce RA. Midazolam and atropine alter theta oscillations in the hippocampal CA1 region by modulating both the somatic and distal dendritic dipoles. Hippocampus. 2014;24:1212–31.
Wilson ME, Lee GK, Chandra A, Kane GC. Central anticholinergic syndrome following dobutamine-atropine stress echocardiography. Echocardiography. 2011;28:E205–6.
Wygnanski-Jaffe T, Nucci P, Goldchmit M, Mezer E. Epileptic seizures induced by cycloplegic eye drops. Cutan Ocul Toxicol. 2014;33:103–8.
Wu PC, Yang YH, Fang PC. The long-term results of using low-concentration atropine eye drops for controlling myopia progression in schoolchildren. J Ocul Pharmacol Ther. 2011;27:461–6.
Chia A, Lu QS, Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01 % eyedrops. Ophthalmology. 2016;123:391–9.
Tsukahara S, Sasaki T. Postural change of IOP in normal persons and in patients with primary wide open-angle glaucoma and low-tension glaucoma. Br J Ophthalmol. 1984;68:389–92.
Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012;32:3–16.
Wen G, Tarczy-Hornoch K, McKean-Cowdin R, Cotter SA, Borchert M, Lin J, et al. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthamology. 2013;120:2109–16.
Li SM, Wu SS, Kang MT, Liu Y, Jia SM, Li SY, et al. Atropine slows myopia progression more in Asian than white children by meta-analysis. Optom Vis Sci. 2014;91:342–50.
Guo YH, Lin HY, Lin LL, Cheng CY. Self-reported myopia in Taiwan: 2005 Taiwan National Health Interview Survey. Eye (Lond). 2012;26:684–9.
Wallman J. Nature and nurture of myopia. Nature. 1994;371:201–2.
Glasser A, Howland HC. A history of studies of visual accommodation in birds. Q Rev Biol. 1996;71:475–509.
Stone RA, Pardue MT, Iuvone PM, Khurana TS. Pharmacology of myopia and potential role for intrinsic retinal circadian rhythms. Exp Eye Res. 2013;114:35–47.
McBrien NA, Jobling AI, Truong HT, Cottriall CL, Gentle A. Expression of muscarinic receptor subtypes in tree shrew ocular tissues and their regulation during the development of myopia. Mol Vis. 2009;15:464–75.
Zou L, Liu R, Zhang X, Chu R, Dai J, Zhou H, et al. Upregulation of regulator of G-protein signaling 2 in the sclera of a form deprivation myopic animal model. Mol Vis. 2014;20:977–87.
Angelini C, Costa M, Morescalchi F, Cimoli G, Coniglio L, Falugi C, et al. Muscarinic drugs affect cholinesterase activity and development of eye structures during early chick development. Eur J Histochem. 1998;42:309–20.
Duncan G, Collison DJ. Role of the non-neuronal cholinergic system in the eye: a review. Life Sci. 2003;72:2013–9.
Bedrossian RH. The effect of atropine on myopia. Ophthalmology. 1979;86:713–7.
Kennedy RH, Dyer JA, Kennedy MA, Parulkar S, Kurland LT, Herman DC, et al. Reducing the progression of myopia with atropine: a long term cohort study of Olmsted County students. Binocul Vis Strabismus Q. 2000;15:281–304.
Shih YF, Chen CH, Chou AC, Ho TC, Lin LL, Hung PT. Effects of different concentrations of atropine on controlling myopia in myopic children. J Ocul Pharmacol Ther. 1999;15:85–90.
Cooper J, Eisenberg N, Schulman E, Wang FM. Maximum atropine dose without clinical signs or symptoms. Optom Vis Sci. 2013;90:1467–72.
Herring IP, Pickett JP, Champagne ES, Troy GC, Marini M. Effect of topical 1 % atropine sulfate on intraocular pressure in normal horses. Vet Ophthalmol. 2000;3:139–43.
Stadtbäumer K, Frommlet F, Nell B. Effects of mydriatics on intraocular pressure and pupil size in the normal feline eye. Vet Ophthalmol. 2006;9:233–7.
Harris LS. Cycloplegic-induced intraocular pressure elevations a study of normal and open-angle glaucomatous eyes. Arch Ophthalmol. 1968;79:242–6.
Hadjikoutis S, Morgan JE, Wild JM, Smith PE. Ocular complications of neurological therapy. Eur J Neurol. 2005;12:499–507.
Wu TE, Yang CC, Chen HS. Does atropine use increase intraocular pressure in myopic children? Optom Vis Sci. 2012;89:161–7.
Jensen H. Timolol maleate in the control of myopia. A preliminary report. Acta Ophthalmol Suppl. 1988;185:128–9.
Jensen H. Myopia progression in young school children and intraocular pressure. Doc Ophthalmol. 1992;82:249–55.
Edwards MH, Brown B. IOP in myopic children: the relationship between increases in IOP and the development of myopia. Ophthalmic Physiol Opt. 1996;16:243–6.
Lee AJ, Saw SM, Gazzard G, Cheng A, Tan DT. Intraocular pressure associations with refractive error and axial length in children. Br J Ophthalmol. 2004;88:5–7.
Acknowledgments
Not applicable.
Funding
CMRPG260391 from the Chang Gung Medical Research Foundation.
Availability of data and materials
We apologize for not sharing our data to the public at present because the cohort in this study will be included as the patient group in our ongoing study.
Authors’ contributions
YFL participated in the collection of the data. CYL participated in drafting the initial manuscript, analysis and interpretation of the data and revision of the manuscript. CCS and KKL participated in the conception and design of the work, follow-up of the patients, collection of the data, analysis and interpretation of the data, and drafting and revision of the manuscript. All authors read and approved the final manuscript, and are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Authors’ information
CYL: Department of Medicine, Chang Gung University, physician in Keelung Chang Gung Memorial Hospital.
CCS: Attending physician of Ophthalmology department in Keelung Chang Gung Memorial Hospital, and Associate Professor of Chang Gung University.
YFL: Stuff of Ophthalmology department in Keelung Chang Gung Memorial Hospital.
KKL: Attending physician of Ophthalmology department in Linkou Chang Gung Memorial Hospital.
Competing interests
The authors have no proprietary or commercial interest in any materials discussed in this article.
Consent for publication
Not applicable.
Ethics approval and consent to participate
We certify that this study adhered to the tenets of the Declaration of Helsinki and informed consents were obtained from the parents or guardians of our subjects. Moreover, the study protocol was approved by the institutional review board at Chang Gung Memorial Hospital (97-1988A3).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lee, CY., Sun, CC., Lin, YF. et al. Effects of topical atropine on intraocular pressure and myopia progression: a prospective comparative study. BMC Ophthalmol 16, 114 (2016). https://doi.org/10.1186/s12886-016-0297-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-016-0297-y