Abstract
Background
Conjunctival amyloidosis is a very rare condition, generally unilateral, and presents mostly as an isolated condition without systemic compromise. Our purpose is to present a new case of systemic amyloidosis with a bilateral conjunctival involvement.
Case Presentation
A 66-years-old caucasian female complaining of conjunctival hemorrhage and chemosis in both eyes for the last five years had been discontinuously treated with topical antibiotics and corticosteroids without any evident improvement. She presented with a pink-yellow infiltration in the inferior conjunctiva of both eyes. Conjunctival biopsy under optical microscopy revealed amyloid deposit, confirmed by Congo red staining. Mucosal biopsy from esophagus and rectus confirmed amyloidosis by Congo red stain. Immunohistochemistry of bone marrow biopsy showed an increased number of plasma cells and an over-expression of light chain kappa subunit. She was treated with corticosteroids and lubrication with an improvement of symptoms. Ocular lesions remained stable after a follow-up of 3 years.
Conclusions
Conjunctival amyloidosis is a rare entity that may be overlooked, and should be differentiated from chronic conjunctivitis and conjunctival malignancies. Although it presents most frequently as a local process, a systemic involvement should always be ruled out.
Similar content being viewed by others
Background
Amyloidosis is a rare group of disorders characterized by the deposition of insoluble fibrillar proteins in a β-pleated sheet configuration, known as amyloid, within the extracellular and perivascular space, as the consequence of a wrong folding process of normally soluble proteins, and may affect virtually any organ or tissue of the body [1–5].
Amyloidosis disorders are classified into three major forms: local, systemic, and hereditary systemic amyloidosis [2]. The acquired forms may be primary (immunologic) and secondary (reactive) [2]. In primary amyloidosis (AL) deposits contain immunoglobulin light chains, usually lambda and kappa monoclonal types, resulting from the abnormal production by plasmocytes in the bone marrow [2, 6]. Secondary amyloidosis (AA) is formed from serum protein A, an acute phase reactant protein that is synthesized in response to longstanding inflammation [7]. In hereditary amyloidosis protein deposits are constituted by a mutant form of the transport protein transthyretin [8].
Ocular amyloidosis occurs most frequently as the local deposition of amyloid in the same place where it originates or, rarely, may be part of a systemic disorder [3, 9]. Amyloid may accumulate in the eyelid, conjunctiva, cornea, vitreous, or anterior orbit [3, 10].
Conjunctival amyloidosis is one of the most common forms of ocular involvement, mostly occurring as a local deposition of amyloid and rarely in association with systemic involvement [3, 10–15]. Due to the rarity of conjunctival amyloidosis, its diagnosis can often be overlooked or confused with other conditions that may affect the conjunctiva. It is more commonly observed in middle-aged adult patients, presenting as an inflammatory or malignant conjunctival entity [3, 11]. Besides, conjunctival malignant lesions can lead to amyloidosis and they should be ruled out [3, 12].
The purpose of our study is to report a new case of systemic amyloidosis with bilateral conjunctival involvement.
Case presentation
A 66-year-old Caucasian woman complaining of conjunctival hemorrhage and chemosis in both eyes for the last five years had been discontinuously treated with topical antibiotics and corticosteroids without any evident improvement.
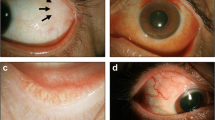
At the time of her referral, best-corrected visual acuity was 20/25 in both eyes. Biomicroscopy showed significant bilateral and rather symmetric edema of the inferior bulbar and lower fornix conjunctiva with areas of pink-yellow condensation and hemorrhages associated with follicular reaction (Fig. 1a). A conjunctival swap was obtained to rule out infection by common antibiotic resistant bacteria or Chlamydia spp. As direct fluorescent antibodies for Chlamydia spp were positive, she was put under treatment with oral doxycycline 200 mg/day and topical azithromycin 3 times/day for 20 days, without any improvement. Conjunctival biopsy was undertaken and optical microscopy revealed amorphous eosinophilic material positive for hematoxyline-eosin stain, with mild mono and polymorphonuclear inflammatory infiltrate and hemorrhagic suffusion (Fig. 1b and 1c). After Congo red staining, the samples showed a red-green birefringence and dichroism under polarized light microscopy consistent with amyloidosis (Fig. 1d). No evidence of malignancy was observed.
(a)Photograph of the patient showing in both eyes diffuse, yellow-pink diffuse mass extending from the inferior bulbar conjunctiva to the lower fornix with areas of waxy-yellow condensations, prominent intrinsic vessels and subconjunctival hemorrhage. b Optical microscopy of conjunctival biopsy shows an amorphous eosinophilic material with mild mono and polymorphonuclear inflammatory infiltrate and hemorrhagic suffusion; (H&E; original magnification x100). c A higher magnification shows the amorphous material replacing the normal stroma of the conjunctiva; (H&E; original magnification x400). d Polarization microscopy of conjunctival specimen stained with Congo red shows a characteristic red-green birefringence and dichroism of amyloid
A complete systemic evaluation was carried out. Liver and heart function evaluation was normal. Immunofixation of blood samples revealed polyclonal hypergammaglobulinemy, and no monoclonal bands were observed by immunofixation of urine sample. Mucosal biopsy from esophagus, and rectus confirmed amyloidosis by the Congo red staining (not shown). In order to rule out multiple myeloma or plasma cells dyscrasia, a bone marrow biopsy was obtained showing a positive expression of CD 138+ (Fig. 2a), a well known marker for identification and quantification of plasma cells in bone marrow and other tissues, as well as an increased population of plasma cells with over-expression of the light chain kappa subunit (Fig. 2b).
The patient was treated with topical lubrication and the ocular lesions of both eyes remained stable after a follow-up of 3 years. She continues with periodical clinical controls to assess the eventual manifestation and progression of the systemic disease.
Discussion
Conjunctival amyloidosis, predominantly affecting middle-aged adults, usually begins at the fornices, spreading to the bulbar and palpebral conjunctiva [3]. This progression appears to affect more deeply the palpebral than the bulbar conjunctiva [3, 16]. In our patient, a bilateral diffuse pink-yellow infiltration with hemorrhagic areas was found throughout the lower bulbar conjunctiva without affecting the palpebral function and position, in contrast with the findings of Demirci et al [4] that observed a unilateral involvement in all of their six cases.
Associated spontaneous conjunctival hemorrhages, as observed in our patient, are a common finding that may be explained by the fact that amyloid infiltration of vessel walls induces rigidity and disruption of conjunctival vessels [3]. A complete systemic evaluation to discard a primary systemic form of the disease is recommended [10] as conjunctival amyloidosis might be an early manifestation of systemic amyloidosis [3]. In our case, the initial presentation of conjuctival amyloidosis led to the systemic findings that were asymptomatic. Only five cases have been reported as systemic amyloidosis with conjunctival involvement [3, 12–15].
Even though the condition may be clinically suspected, a tissue biopsy of the involved organ should be taken to confirm the diagnosis. In systemic disease the sampling can be performed directly in the organ or tissue affected, or in a clinically uninvolved site such as subcutaneous fat, minor salivary glands or rectal mucosa [1, 3]. Furthermore, testing for monoclonal protein population should be determined by serum and urine protein electrophoresis and immunofixation [1]. In our patient, immunofixation of blood samples only revealed polyclonal hypergammaglobulinemy, and rectal and esophageal mucosal biopsies confirmed the diagnosis of systemic amyloidosis. In addition, immunohistochemical studies of bone marrow biopsies showed an increased population of plasma cells with the amyloidogenic overexpression of the subunit kappa.
There is still no consensus on the management of conjunctival amyloidosis and none of the available treatments are radical. Some authors recommend conservative treatment using lubricants and topical anti-inflammatories [3]. Others believe that a more aggressive treatment should be done in order to prevent progression or recurrence [17]. Cryotherapy, [18] radiotherapy, [19] surgical debulking, [20] and mucous membrane graft implantation, [21] are among the techniques that could be used. A conservative topical treatment was offered to our patient, as lesions remained stable over time and the patient referred no major ocular complaints.
Conclusions
Conjunctival amyloidosis is a rare entity that may be overlooked and should be differentiated from chronic conjunctivitis and conjunctival malignancies. Although commonly a local process, a systemic involvement should always be ruled out.
Consent
Written informed consent was obtained from the patient for publication of this Case report and any of the accompanying images. A copy of the written consent is available for review by the Editors of BMC Ophthalmology.
References
Goveric PD. An overview of amiloidosis. UpToDate® Wolters Kluwer Health. 2013; http://www.uptodate.com/contents/an-overview-of-amyloidosis
Westermark P, Benson MD, Buxbaum JN, Cohen AS, Frangione B, Ikeda S, et al. Amyloid: Toward terminology clarification. Report from the Nomenclature Committee of the International Society of Amyloidosis. Amyloid. 2005;12:1–4.
Leibovitch I, Selva D, Goldberg RA, Sullivan TJ, Saeed P, Davis G, et al. Periocular and orbital amyloidosis: clinical characteristics, management, and outcome. Ophthalmology. 2006;113:1657–64.
Demirci H, Shields CL, Eagle Jr RC, Shields JA. Conjuctival amyloidosis: report of six cases and review of the literature. Surv Ophthalmol. 2006;51:419–33.
Westermark GT, Fändrich M, Westermark P. AA amyloidosis: pathogenesis and targeted therapy. Annu Rev Pathol. 2015;10:321–44.
Glenner GG, Terry W, Harada M, Isersky C, Page D. Amyloid fibril proteins: proof of homology with immunoglobulin light chains by sequence analyses. Science. 1971;172:1150–1.
Lachmann HJ, Goodman HJ, Gilbertson JA, Gallimore JR, Sabin CA, Gillmore JD, et al. Natural history and outcome in systemic AA amyloidosis. N Engl J Med. 2007;356:2361–71.
Rowczenio DM, Noor I, Gillmore JD, Lachmann HJ, Whelan C, Hawkins PN, et al. Online registry for mutations in hereditary amyloidosis including nomenclature recommendations. Hum Mutat. 2014;35:E2403–12.
Al-Nuaimi D, Bhatt PR, Steeples L, Irion L, Bonshek R, Leatherbarrow B. Amyloidosis of the orbit and adnexae. Orbit. 2012;31:287–98.
Aryasit O, Preechawai P, Kayasut K. Clinical presentation, treatment, and prognosis of periocular and orbital amyloidosis in a university-based referral center. Clin Ophthalmol. 2013;7:801–5.
Ray M, Tan AW, Thamboo TP. Atypical presentation of primary conjuctival amiloidosis. Can J Ophthalmol. 2012;47:e2–4.
Abdallah AO, Westfall C, Brown H, Muzaffar J, Atrash S, Nair B. Unilateral conjunctival AL kappa amyloidosis with trace evidence of systemic amyloidosis. Am J Case Rep. 2012;13:102–5.
Purcell Jr JJ, Birkenkamp R, Tsai CC, Riner RN. Conjunctival involvement in primary systemic nonfamilial amyloidosis. Am J Ophthalmol. 1983;95:845–7.
Iijima S. Primary systemic amyloidosis: a unique case complaining of diffuse eyelid swelling and conjunctival involvement. J Dermatol. 1992;19:113–8.
Shields JA, Eagle RC, Shields CL, Green M, Singh AD. Systemic amyloidosis presenting as a mass of the conjunctival semilunar fold. Am J Ophthalmol. 2000;130:523–5.
Rodrigues G, Sanghvi V, Lala M. A rare cause of unilateral upper and lower eyelid swelling: isolated conjuctival amyloidosis. Korean J Ophthalmol. 2001;15:38–40.
Patrinely JR, Koch DD. Surgical management of advanced ocular adnexal amyloidosis. Arch Ophthalmol. 1992;110:882–5.
Fraunfelder FW. Liquid nitrogen cryotherapy for conjunctival amyloidosis. Arch Ophthalmol. 2009;127:645–8.
Khaira M, Mutamba A, Meligonis G, Rose GE, Plowman PN, O´Donnell H. The use of radiotherapy for the treatment of localized orbital amyloidosis. Orbit. 2008;27:432–7.
Murdoch IE, Sullivan TJ, Moseley I, Hawkins PN, Pepys MB, Tan SY, et al. Primary localized amyloidosis of the orbit. Br J Ophthalmol. 1996;80:1083–6.
Seider N, Beiran I, Kaltreider SA. Advanced localized primary conjunctival amyloidosis: surgical rehabilitation using mucous membrane graft implantation. Isr Med Assoc J. 2006;8:439–40.
Acknowledgements
The authors are grateful to Dr. Ana V. Sanchez and Dr. Ana B. de Diller from the Department of Pathology, Hospital Privado Centro Medico de Cordoba, Argentina, for their invaluable assistance concerning bone marrow biopsy analysis and imaging.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LJC participated in the conception and design of the work, drafted the manuscript, participated in the follow-up of patient acquisition, performed in the analysis and interpretation of data, participated in figures selection and edition; manuscript revision and text editing; final manuscript critical revision and correction. JPM performed clinical diagnosis, treatment and follow-up of patient, participated in the conception and design of the work, carried out the analysis and interpretation of data, participated in the final manuscript critical revision, and provided the clinical picture. EE participated in the follow-up of patient, acquisition, analysis and interpretation of data, in writing of the manuscript and text editing, and in the final manuscript critical revision and correction. RM participated in the follow-up of patient, acquisition, analysis and interpretation of data, and in the final manuscript critical revision and correction. MEG-C participated in the follow-up of patient, in the acquisition, analysis and interpretation of data, and in the manuscript revision and correction. MP performed hystopathologic studies, carried out the analysis and interpretation of data and selection of hystopathologic images, and participated in manuscript revision. HMS participated in the writing of the manuscript and text editing, and in the final manuscript critical revision and correction. JAU-Z participated in the conception and design of the work; carried out the analysis and interpretation of data; participated in the writing of the manuscript and text editing, and in the final manuscript critical revision and correction. All authors read and approved the final manuscript, and are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Correa, L.J., Maccio, J.P., Esposito, E. et al. Systemic amyloidosis with bilateral conjunctival involvement: a case report. BMC Ophthalmol 15, 77 (2015). https://doi.org/10.1186/s12886-015-0075-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-015-0075-2