Abstract
Background
A variety of solid tumours, including oral squamous cell carcinoma (OSCC), can cause coagulation abnormalities, and this phenomenon is known as tumour-associated hypercoagulation. We aimed to explore the preoperative thromboelastography (TEG) parameter profiles of OSCC patients, and to investigate their trends in relation to tumour stage progression, and to evaluate their value for predicting cervical lymph node metastasis.
Methods
Data on thromboelastographic parameters and conventional coagulation indices were retrospectively collected, and comparisons were performed among preoperative primary OSCC patients (n = 311), recurrent/metastatic OSCC patients (n = 44) and a control group (n = 71). Among primary OSCC patients, the correlation with tumour stage and the predictive role of cervical lymph node metastasis were analyzed.
Results
Hypercoagulability occurred in OSCC patients and tended to become more pronounced as the tumour progressed. The whole-time phase of coagulation increased with increasing T stage, while the early phase of coagulation increased with increasing N stage.
Conclusions
Preoperative TEG parameters are closely related to tumour stage and progression, suggesting that TEG can be used as an important indicator for predicting tumour stage and as a potential biomarker.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Oral cancer is one of the most common malignant tumours in the head and neck region, which accounts for approximately 3% of malignant tumour [1, 2]. More than 90% of oral cancers are oral squamous cell carcinoma (OSCC), which are prone to regional cervical lymph node metastasis [3, 4]. To date, the methods for the diagnosis and assessment of OSCC are still insufficient, so more in-depth exploration of biomarkers is needed.
The relationship between malignant tumours and coagulation was proposed as early as the 19th century by Trousseau [5], and has since been widely discussed. Lu et al. reported that pretreatment thrombocytosis is an independent predictor of poor prognosis in patients with OSCC and is closely associated with aggressive tumour growth, lymph node metastasis, and distant metastasis [6]. A previous study by our group revealed that an elevated preoperative D-dimer level was a poor prognostic factor for OSCC progression [7].
Thromboelastography (TEG) technology was invented by Hartert in 1948 [8]. This technology combines the physical properties of blood, such as viscoelasticity, by real-time detection of whole-blood samples and provides the dynamic changes in the whole coagulation-fibrinolysis process. Previous studies have shown significant correlations between TEG and conventional coagulation assays in the assessment of thrombotic and haemorrhagic risk in deep venous thrombosis (DVT) formation, chronic liver disease, fractures in elderly individuals, and postpartum haemorrhage [9,10,11]. However, analyses of TEG parameters among OSCC patients are lacking.
The aim of our study was to investigate the coagulation characteristics of OSCC patients, and their trends at various stages of tumour progression by analyzing the preoperative conventional coagulation indices and TEG parameters of OSCC patients.
Methods
Patient cohorts
We retrospectively collected data from OSCC patients and nonmalignant patients who visited the Department of Oral and Maxillofacial Surgery, Hospital of Stomatology, Sun Yat-sen University from January 2021 to July 2022. Informed consent was obtained. This study was approved by the Ethics Committee of Hospital of Stomatology, Sun Yat-sen University. All patients were aged between 20 and 80 year. All the OSCC patients were diagnosed by pathology. The control group included those who were hospitalized for other nonmalignant diseases. The exclusion criteria for patients were as follows: (1) history of coagulation system disorders or recent anticoagulant medication; (2) with other malignancies; (3) previous oncological treatment such as radiotherapy; or (4) menstruation, infection or inflammatory states, other severe haematologic diseases, or hepatic insufficiency.
Clinical data collection
Data on the demographic characteristics and clinical information of each patient were collected. Tumour TNM staging followed the 8th edition of the American Joint Committee on Cancer (AJCC)/International Union Against Cancer (UICC) Oral Cancer Staging Guidelines. Data on the preoperative coagulation indices of the above patients, including the platelet count (PLT), D-dimer level, activated partial thromboplastin time (APTT), prothrombin time (PT), thrombin time (TT), fibrinogen (FIB) and preoperative TEG parameters, were obtained. TEG data were detected and acquired via the TEG® 5000 Hemostasis Analyzer System (Haemonetics Corporation, USA). All the blood samples were performed by professional technicians from the department of clinical laboratory of the hospital according to standard operating procedures. The above coagulation test data were retrospectively collected from the medical records system. Thromboelastography is now widely used in clinical practice and, as a routine preoperative monitoring method in our hospital, it provides a more comprehensive assessment of the patient’s coagulation status, thereby reducing the risk of perioperative coagulation-related complications.
Meanings of TEG parameters
The parameters and clinical significance of TEG are summarized as follows: (1) R time (min) indicates the time from the start until the beginning of clot formation, representing the level and function of clotting factors; (2) K time (min) and Angle (°) respectively indicate the time (K) and speed (Angle) from the clot formation to when the clot reached an amplitude of 20 mm, representing the efficiency of the early stages of clot formation; (3) MA (mm) indicates the amplitude at the point of maximum clot strength, representing mainly the level and function of platelets; (4) LY30 (%) and EPL (%) indicate the rate (LY30) and the predicted rate (EPL) of clot dissolution after reaching the MA; (5) G (d/sc) indicates a clot strength score calculated on the basis of instrument-measured data; and (6) coagulation index (CI) indicates a comprehensive coagulation status.
Statistical analysis
With SPSS 25.0 software, each coagulation parameter of the primary OSCC group, recurrent/metastatic OSCC group, and control group was analyzed by means of the Kruskal-Wallis H test for comparisons among the three groups and by means of the Mann-Whitney U test for comparisons with the control group. The relationships between the preoperative coagulation parameters and the tumour stage of primary OSCC group was analyzed by means of the Mann-Whitney U test. The predictive value of coagulation indices for cervical lymph node metastasis was analyzed by means of the receiver operating characteristic (ROC) curve. P < 0.05 indicated statistical significance.
Results
OSCC patients presenting with preoperative hypercoagulability
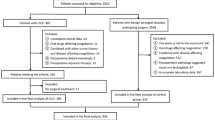
A total of 311 patients with primary OSCC, 44 patients with recurrent/metastatic OSCC and 71 patients in the control group were included in the study (Fig. 1). No distant metastasis was found in our cohort.
Among the 71 nonmalignant patients in the control group, 30 had benign jaw lesions, 9 had localized oral inflammation, 8 had benign salivary gland disease, 8 had oral leucoplakia (including mild–moderate dysplasia), 7 had benign oral tumours, 4 had dentofacial deformities, 2 had vascular malformations, 2 had impacted teeth, and 1 had dry eye syndrome.
As shown in Table 1, the baseline sex, age and body mass index (BMI) did not significantly differ between the OSCC patients and the control group. However, among OSCC patients, the proportions of patients with a history of tobacco or areca nut use were higher.
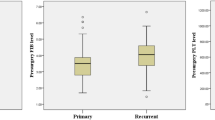
We compared the conventional coagulative indices and TEG parameters of the primary OSCC (primary group) and R/M OSCC (R/M group) to those of the control group (Table 2). The three-group comparison revealed significant differences in preoperative PLT, D-dimer and FIB values (P < 0.05). The TEG parameters, including K time, Angle, MA, G and CI, also differed among the groups (P < 0.05). Compared with that in the control group, the K time was lower, and the Angle was higher in the primary group. MA was increased in both the primary and R/M groups. The comprehensive coagulation scores, including G and CI scores, also increased. These findings indicate that patients with primary and R/M OSCC patients have a preoperative hypercoagulable state.
Coagulation-fibrinolytic characteristics are correlated with tumour stage
To further explore the relationship between coagulation-fibrinolytic status and tumour stage, we compared coagulation indices across different tumour stages in primary OSCC patients.
We found that with increasing pathological T stage (pT stage), the preoperative PLT, D-dimer, and FIB increased, and TT decreased. With respect to the TEG parameters, the R time and K time decreased, and the Angle, MA, G, and CI increased, indicating that hypercoagulability became more obvious with increasing pT stage (shown in Fig. 2).
Correlations between preoperative coagulation parameters and the pT stage of primary OSCC patients. A-D, Conventional coagulation indexes. E-J, TEG parameters. T1 stage, n = 41. T2 stage, n = 117. T3 stage, n = 87. T4 stage, n = 66. All referring to pathological staging. The Kruskal-Wallis H test were used, P < 0.05*, P < 0.01**, P < 0.001***
With increasing pathological N stage, only preoperative D-dimer (P < 0.001) and FIB (P = 0.002) levels were elevated (Fig. 3-A, B). In terms of the TEG parameters, the K time (P = 0.019) decreased, and the Angle (P = 0.031) was increased (Fig. 3-C, D). There were no significant differences in the other TEG parameters (P > 0.05).
Correlations between preoperative coagulation parameters and the pN stage of primary OSCC. A-B, Conventional coagulation indexes. C-D, TEG parameters. N0 stage, n = 196. N1 stage, n = 40. N2 stage, n = 40. N3 stage, n = 35. All referring to pathological staging. The Kruskal-Wallis H test was used, P < 0.05*, P < 0.01**, P < 0.001***
Predictive role of coagulation indices in lymph node metastasis
We further evaluated whether coagulation parameters can predict cervical lymph node metastasis (pN stage). Among 311 patients with primary OSCC, 196 were pN0 stage and 115 were pN1-3 stage. The cut-off value of each variable was calculated with the Youden index (Supplementary Table 1). ROC curve analysis revealed that preoperative D-dimer (> 383ug/L), FIB (> 3.575 g/L), R time (< 5.95 min) and K time (< 1.75 min) were predictive of cervical lymph node metastasis, with the area under curve (AUC) of 0.660, 0.637, 0.569 and 0.571, respectively (Fig. 4).
ROC curves of preoperative coagulation parameters for the prediction of the pN stage of OSCC. A-B, Conventional coagulation indices. C-D, TEG parameters. Patients with primary OSCC (N = 311) were categorized as pN0 (n = 196) or pN1-3 (n = 115), and ROC curve analysis was used to predict lymph node metastases. AUC, area under curve. P < 0.05*, P < 0.01**, P < 0.001***
Among the 241 clinical N0 (cN0) patients, 66 patients (27.39%) presented with pathologically confirmed cervical lymph node metastases, which led us to consider whether coagulation indices are predictive of occult metastases. As shown in Fig. 5, among the cN0 patients, preoperative D-dimer (> 392.5ug/L) and FIB (> 3.575 g/L) were predictive of occult lymph node metastasis, with AUCs of 0.648 and 0.608, respectively. However, the TEG parameters were not predictive of occult metastases (P > 0.05).
ROC curves of preoperative coagulation parameters for the prediction of occult lymph node metastasis. A-B, Conventional coagulation indices. cN0 OSCC patients (N = 241) were included in ROC curve analysis, in which 66 patients were confirmed to have lymph node metastases. AUC, area under curve. P < 0.05*, P < 0.01**, P < 0.001***
Discussion
In this study, we innovatively elucidated the preoperative coagulation state in OSCC patients by combining TEG technology with conventional coagulation indices. We found that OSCC patients had an increased R time, K time, Angle and MA, indicating a whole-time-phase hypercoagulable state in the initial stage of coagulation, the early stage of blood clot formation, and the stage of coagulation cascade amplification. Though it is widely accepted for the use of TEG in numerous clinical scenarios such as surgery, trauma, and sepsis, its predictive value for disease progression in cancer patients has not been commonly recognized, with only studies involving relatively small case numbers reported. Zhou et al. revealed that preoperative TEG parameters such as K time, R time and MA can predict the clinical stage of lung cancer [12]. Another study revealed that Angle was closely related to postoperative local recurrence in pancreatic cancer patients, overall survival and disease-free survival [13]. Patients with papillary thyroid cancer had shorter R and K times, a higher Angle, and a higher CI than did the patients in the control group [14]. However, to our knowledge, in head and neck cancer, studies have been conducted only on the postoperative monitoring of microvascular anastomosis via TEG technology, but the oncological predictive value of TEG parameters has not been explored [15, 16]. Our study revealed for the first time that the predictive effect of TEG on OSCC tumour staging is good, further expanding its application value in the field of head and neck tumours. However, the potential impact of tobacco and areca nut use on coagulation function cannot be ruled out. Studies have confirmed that smoking may promote a hypercoagulable state [17, 18], while the effects of various components of areca nut on coagulation are still unclear [19, 20]. Further baseline matching with control groups is needed to support the hypercoagulable state in OSCC patients.
There was a significant correlation between tumour T stage and various TEG parameters, which indicated that the primary lesion was the culprit of the cancer-associated hypercoagulable state, in which coagulation factors, platelets and fibrinogen all play important roles. On the one hand, tumour-derived inflammatory factors such as interleukin-6 (IL-6) can stimulate FIB production and platelet elevation [21]. Tumour cells can directly affect coagulation and fibrinolysis by secreting a variety of procoagulant substances, such as tissue factor (TF), prothrombin activator inhibitor-1 (PAI-1), adenosine diphosphate (ADP), and exosomes [22]. On the other hand, as the tumour grows larger, the hypoxic microenvironment, necrosis, and endothelial dysfunction within the tumour further promote local hypercoagulation [23,24,25].
Notably, decreased R and K times and increased Angle were closely associated with tumour N stage, suggesting that lymph node metastasis influences mainly the early stages of coagulation. It has been observed that the fibrinogen α chain can pass through the integrin-AKT pathway to promote lung cancer growth and metastasis [26]. Another promising finding was that fibrin and platelets can adhere to circulating tumour cells (CTCs) to form microthrombi, which can not only help CTCs escape immune surveillance and shear forces in the blood but also enable their spread to distant organs and formation of metastases [27]. Our previous study demonstrated that intratumoural platelet microthrombi are an independent risk factor for lymph node metastasis in OSCC patients [28], suggesting that platelets are also important members of the tumour microenvironment. Recent studies have also reported a reduction in tumour lung metastases in mouse models in which platelet activation is inhibited, suggesting that platelets may be involved in the occurrence of metastasis [29, 30]. In TEG parameters, the K time can to some extent reflect early platelet activation. The decreased K time in N + patients suggest that platelet early activation may be involved in metastasis. The MA value also reflects platelet function and quantity; however, we found that it is primarily associated with T stage and does not significantly predict lymph node metastasis.
However, it is difficult to comprehensively and accurately evaluate the functional status of coagulation members alone through TEG. Our study also found that D-dimer and FIB are more sensitive in predicting lymph node metastasis. It is still necessary to further clarify how coagulation members affect tumour progression through high-throughput screening methods [31].
Conclusions
Patients with OSCC are in a hypercoagulable state, which tends to become more pronounced as the tumour develops. Tumour T stage affects the whole-time phases of coagulation whereas tumour N stage affects coagulation only in the early stages of coagulation. Preoperative TEG parameters in OSCC patients may serve as potential biomarkers for tumour evaluation.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- ADP:
-
Adenosine diphosphate
- APTT:
-
Activated partial thromboplastin time
- AUC:
-
Area under curve
- BMI:
-
Body mass index
- CTCs:
-
Circulating tumour cells
- IL-6:
-
Interleukin-6
- FIB:
-
Fibrinogen
- OSCC:
-
Oral squamous cell carcinoma
- PAI-1:
-
Prothrombin activator inhibitor-1
- PLT:
-
Platelet count
- PT:
-
Prothrombin time
- ROC:
-
Receiver operating characteristic
- TEG:
-
Thromboelastography
- TT:
-
Thrombin time
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Zanoni DK, Montero PH, Migliacci JC, Shah JP, Wong RJ, Ganly I, Patel SG. Survival outcomes after treatment of cancer of the oral cavity (1985–2015). Oral Oncol. 2019;90:115–21.
Shah JP. Cervical lymph node metastases–diagnostic, therapeutic, and prognostic implications. Oncol (Williston Park). 1990;4(10):61–9. discussion 72, 76.
Pentenero M, Gandolfo S, Carrozzo M. Importance of tumor thickness and depth of invasion in nodal involvement and prognosis of oral squamous cell carcinoma: a review of the literature. Head Neck. 2005;27(12):1080–91.
Trousseau A. Clinique médicale de l’Hôtel-Dieu de Paris. Volume 1. J.-B. Baillière et fils; 1861.
Lu CC, Chang KW, Chou FC, Cheng CY, Liu CJ. Association of pretreatment thrombocytosis with disease progression and survival in oral squamous cell carcinoma. Oral Oncol. 2007;43(3):283–8.
Liang YJ, Mei XY, Zeng B, Zhang SE, Yang L, Lao XM, Liao GQ. Prognostic role of preoperative D-dimer, fibrinogen and platelet levels in patients with oral squamous cell carcinoma. BMC Cancer. 2021;21(1):122.
Hartert H. Blutgerinnungsstudien Mit Der Thrombelastographie, Einem Neuen Untersuchungsverfahren. Klinische Wochenschrift. 1948;26(37):577–83.
Lloyd-Donald P, Vasudevan A, Angus P, Gow P, Mårtensson J, Glassford N, Eastwood GM, Hart GK, Jones D, Weinberg L, et al. Comparison of Thromboelastography and Conventional Coagulation tests in patients with severe liver disease. Clin Appl Thromb Hemost. 2020;26:1076029620925915.
Liu C, Guan Z, Xu Q, Zhao L, Song Y, Wang H. Relation of thromboelastography parameters to conventional coagulation tests used to evaluate the hypercoagulable state of aged fracture patients. Med (Baltim). 2016;95(24):e3934.
Mao C, Xiong Y, Fan C. Comparison between thromboelastography and conventional coagulation assays in patients with deep vein thrombosis. Clin Chim Acta. 2021;520:208–13.
Zhou Y, Guo Y, Cui Q, Dong Y, Cai X, Zhang Z, Wu X, Yi K, Zhang M. Application of Thromboelastography to Predict Lung Cancer Stage. Technol Cancer Res Treat. 2020;19:1533033820952351.
Schulick AC, Moore HB, Schulick RD, Del Chiaro M. Thrombelastography as a Prognostic Tool in Adenocarcinoma of the pancreas. Ann Surg. 2020;272(6):e288–9.
Lu S, Kang R, Wang Y, Zhu M, Zhao L, Xu Q, Song Y, Liu C. Altered TEG parameters identify Hypercoagulablilty and are of diagnosis value for papillary thyroid carcinoma patients. Exp Clin Endocrinol Diabetes. 2020;128(5):297–302.
Di ZS-m, Saimaiti ADILIJIANG, Kadi ZULIHUMA, Yashengjiang MUHESEN, Nuermuhanmode NIJIATI, Tuerdi MAIMAITITUXUN. Perioperative thromboelastography evaluation in70free flap transplantations for oral, maxillofacial reconstruction. China J Oral Maxillofacial Surg. 2022;20(3):244–50.
Spielbauer KK, Sunde J, Buchakjian M, Casper KA, Malloy KM, Stucken CL, Prince ME, Rosko AJ, Schechtman S, Chinn SB. Use of rotational thromboelastometry (ROTEM®) to predict thrombotic complications of microvascular head and neck reconstruction. Oral Oncol. 2022;124:105515.
Blann AD, Steele C, McCollum CN. The influence of smoking and of oral and transdermal nicotine on blood pressure, and haematology and coagulation indices. Thromb Haemost. 1997;78(09):1093–6.
Sandhya M, Satyanarayana U, Mohanty S, Basalingappa D. Impact of chronic cigarette smoking on platelet aggregation and coagulation profile in apparently healthy male smokers. Int J Clin Experimental Physiol. 2015;2(2):128–128.
SAEED SA, FARNAZ S, SIMJEE RU. MALIK A: Triterpenes and B-sitosterol from piper betle: isolation, antiplatelet and anti-inflammatory effects. In.: Portland Press Ltd.; 1993.
Jeng J-H, Chen S-Y, Liao C-H, Tung Y-Y, Lin B-R, Hahn L-J, Chang M-C. Modulation of platelet aggregation by areca nut and betel leaf ingredients: roles of reactive oxygen species and cyclooxygenase. Free Radic Biol Med. 2002;32(9):860–71.
Hufnagel DH, Cozzi GD, Crispens MA, Beeghly-Fadiel A. Platelets, thrombocytosis, and ovarian cancer prognosis: surveying the landscape of the literature. Int J Mol Sci. 2020;21(21):8169.
Abdol Razak NB, Jones G, Bhandari M, Berndt MC, Metharom P. Cancer-Associated thrombosis: an overview of mechanisms, risk factors, and treatment. Cancers (Basel) 2018, 10(10).
Jain RK. Molecular regulation of vessel maturation. Nat Med. 2003;9(6):685–93.
Xu Y, Ouyang X, Yan L, Zhang M, Hu Z, Gu J, Fan X, Zhang L, Zhang J, Xue S, et al. Sin1 (stress-Activated protein kinase-interacting protein) regulates Ischemia-Induced Microthrombosis through Integrin αIIbβ3-Mediated Outside-In signaling and hypoxia responses in platelets. Arterioscler Thromb Vasc Biol. 2018;38(12):2793–805.
Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324(5930):1029–33.
Wang M, Zhang G, Zhang Y, Cui X, Wang S, Gao S, Wang Y, Liu Y, Bae JH, Yang WH, et al. Fibrinogen alpha chain knockout promotes Tumor Growth and Metastasis through Integrin-AKT signaling pathway in Lung Cancer. Mol Cancer Res. 2020;18(7):943–54.
Feinauer MJ, Schneider SW, Berghoff AS, Robador JR, Tehranian C, Karreman MA, Venkataramani V, Solecki G, Grosch JK, Gunkel K, et al. Local blood coagulation drives cancer cell arrest and brain metastasis in a mouse model. Blood. 2021;137(9):1219–32.
Duan W, Wu Z, Mei X, Li J, Lu H, Liang Y, Lao X, Liao G. Intratumoral platelet microthrombi in oral squamous cell carcinoma: a marker of lymph node metastasis. Oral Dis 2023.
Ren J, He J, Zhang H, Xia Y, Hu Z, Loughran P, Billiar T, Huang H, Tsung A. Platelet TLR4-ERK5 Axis facilitates NET-Mediated capturing of circulating Tumor cells and distant metastasis after Surgical stress. Cancer Res. 2021;81(9):2373–85.
Shirai T, Revenko AS, Tibbitts J, Ngo ATP, Mitrugno A, Healy LD, Johnson J, Tucker EI, Hinds MT, Coussens LM, et al. Hepatic thrombopoietin gene silencing reduces platelet count and breast cancer progression in transgenic MMTV-PyMT mice. Blood Adv. 2019;3(20):3080–91.
‘t Veld S, Arkani M, Post E, Antunes-Ferreira M, D’Ambrosi S, Vessies DCL, Vermunt L, Vancura A, Muller M, Niemeijer AN, et al. editors. Detection and localization of early- and late-stage cancers using platelet RNA. Cancer Cell 2022, 40(9):999–1009.e1006.
Acknowledgements
Not applicable.
Funding
The study was funded by National Natural Science Foundation of China (Grant No.82103550).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Wan Duan analyzed the data and wrote the manuscript. Zhangxia Wu and Hong Jiang collected the clinical data of the patients. Guiqing Liao analyzed and interpreted the patient data. Yujie Liang commented on previous versions of the manuscript. Xiaomei Lao provided the funding support and revised the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. All patient clinical information was collected with the approval of the Ethics Committee of Hospital of Stomatology, Sun Yat-sen University (Approval Number: KQEC-2021-55-01) with informed consent of the patients.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Duan, W., Wu, Z., Jiang, H. et al. Preoperative thromboelastography parameters in predicting the tumour stage of oral squamous cell carcinoma. BMC Cancer 24, 1136 (2024). https://doi.org/10.1186/s12885-024-12868-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12868-5