Abstract
Background
Despite recent advances in lung cancer therapeutics and improving overall survival, disparities persist among socially disadvantaged populations. This study aims to determine the effects of neighborhood deprivation indices (NDI) on lung cancer mortality. This is a multicenter retrospective cohort study assessing the relationship between NDI and overall survival adjusted for age, disease stage, and DNA methylation among biopsy-proven lung cancer patients. State-specific NDI for each year of sample collection were computed at the U.S. census tract level and dichotomized into low- and high-deprivation.
Results
A total of 173 non small lung cancer patients were included, with n = 85 (49%) and n = 88 (51%) in the low and high-deprivation groups, respectively. NDI was significantly higher among Black patients when compared with White patients (p = 0.003). There was a significant correlation between DNA methylation and stage for HOXA7, SOX17, ZFP42, HOXA9, CDO1 and TAC1. Only HOXA7 DNA methylation was positively correlated with NDI. The high-deprivation group had a statistically significant shorter survival than the low-deprivation group (p = 0.02). After adjusting for age, race, stage, and DNA methylation status, belonging to the high-deprivation group was associated with higher mortality with a hazard ratio of 1.81 (95%CI: 1.03–3.19).
Conclusions
Increased neighborhood-level deprivation may be associated with liquid biopsy DNA methylation, shorter survival, and increased mortality. Changes in health care policies that consider neighborhood-level indices of socioeconomic deprivation may enable a more equitable increase in lung cancer survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Lung cancer is the leading cause of cancer-related mortality, accounting for almost 25% of all cancer-related deaths [1, 2]. With the implementation of lung cancer screening, targeted therapies, and immunotherapy, lung cancer survival has improved dramatically over the past couple of decades [3]. However, disparities in survival continue to persist among socially deprived and disadvantaged populations and hinder the full potential of modern medical advances to benefit all in society. While individual-level risk factors, such as tobacco use, have long been hypothesized to underlie this phenomenon, the role of broader socioeconomic factors on health outcomes is gaining recognition [3]. Neighborhood-level deprivation often encompasses geospatially aggregated (e.g., within U.S. census tracts or block groups) indices of employment, occupation, education, housing conditions, income, and wealth, which cumulatively can have profound impacts on health (7). Indeed, neighborhood-level factors can have detrimental effects on health outcomes, including 30-day hospital readmission rates, cardiovascular disease, type II diabetes, asthma, and chronic obstructive pulmonary disease [4, 5]. This association has also been demonstrated in lung cancer incidence, with one study finding that the odds of developing lung cancer increased by 66% in neighborhoods with the greatest deprivation [6, 7]. While the relationship between neighborhood-level deprivation and lung cancer mortality has been explored [8,9,10], the specific biological mechanism by which neighborhood conditions promote lung cancer progression remains uncertain. Epigenetic modifications are heritable changes in gene expression that occur without changes in the DNA sequence and can be influenced by many environmental factors [11, 12]. Acquired epigenetic changes promote initiation and progression of cancer by modulating gene expression, which plays a significant role in the initiation and progression of several types of cancer, including lung cancer [13, 14]. One of the most influential epigenetic changes involves methylation of CpG islands within the promoters of genes. Promoter hypermethylation of tumor suppressor genes leads to transcriptional silencing, which drives carcinogenesis. The impact of neighborhood-level deprivation on epigenomic gene expression and lung cancer mortality has yet to be explored.
This study aimed to assess the association between neighborhood-level deprivation and lung cancer mortality within the context of the U.S. health care system, as well as investigate its effect on the methylation status of six lung cancer tumor suppressor genes obtained from liquid biopsies. We hypothesized that patients with lung cancer and greater levels of neighborhood deprivation have a decreased overall survival and higher levels of tumor suppressor gene methylation.
Methods
Study design
This is a multicenter retrospective cohort study assessing the relationship of NDI with survival adjusted for age, stage, and DNA methylation among biopsy-proven lung cancer from two tertiary academic medical centers between 2008 and 2020. The reporting of this study conforms to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [15].
Study population
Participants were referred for surgical resection based on a suspicious finding on chest CT. The inclusion criteria for this study comprised: (A) any adult age 30 or older with a diagnosis of non small cell lung cancer of any stage, either biopsy-proven or pathologically proven from a surgical specimen from surgery involving a lobectomy, pneumonectomy, or greater resection (stages were defined according to revised TNM guidelines classification criteria) [10]; (B) able to provide informed consent for this study. Exclusion criteria consisted of: (A) patients with other malignancies who preoperatively were incorrectly assumed to have primary lung cancer; (B) history of hereditary cancer; (C) radiotherapy or chemotherapy treatment had been given prior to surgical resection; (D) any patient < 30 years old; (E) pregnant patients. Clinical information collected included age at diagnosis, sex, race, tobacco use status (current vs. former vs. never), pack-year tobacco use history, tumor size, histology, stage at diagnosis, and residential address. This study was conducted in accordance with the Declaration of Helsinki. Institutional review board (IRB) approval was obtained prior to study initiation (IRB #2017–1286 and NA_00005998). Informed consent was obtained from all participants in the study.
Neighborhood deprivation
Participants’ residential addresses at the sample collection were geocoded to U.S. census tracts using the U.S. Census Bureau geocoder and geographically linked to NDI values. State-specific (Illinois and Maryland tracts as the referent) NDI scores for each year between 2010 and 2020 were computed for U.S. census tracts using the “ndi” package in R [16, 17]. Messer et al. [18], previously defined and described the computation of NDI. Briefly, each census tract’s NDI value is its score from the first principal component of a Principal Component Analysis comprised of eight sociodemographic variables from the U.S. Census Bureau American Community Survey, including percent males in management, science, and arts occupation, percent of crowded housing, percent of households in poverty, percent of female-headed households with dependents, percent of households on public assistance, percent of households earning <$30,000 per year, percent earning less than a high school education, and percent unemployed [18]. Census tract-level NDI values were further categorized into quartiles, with the 4th quartile representing a census tract (i.e., neighborhood) with the highest deprivation and the 1st quartile representing a census tract (i.e., neighborhood) with the lowest deprivation (relative to all Illinois and Maryland census tracts). They were further dichotomized into a “low NDI” group defined as the 1st, 2nd, and 3rd quartiles and a “high NDI” group defined as the 4th quartile. The classification of high vs. low NDI was primarily based on maintaining a balanced sample size between groups to allow for robust statistical comparisons. We computed census tract-level NDI scores and quartiles per year (2010–2020) and geographically linked them to participant residential addresses for their year of collection. Participants collected in 2008 or 2009 were assigned 2010 census tract-level NDI scores and quartiles.
DNA methylation
DNA extraction and isolation from plasma-based liquid biopsy samples were performed following the same methodology as previously described [8, 9]. ß-Actin was used as a reference gene for normalization of methylation levels. Primers for CDO1, TAC1, HOXA7, HOXA9, SOX17, and ZFP42 were used. We have previously demonstrated that methylation of these six genes has a high sensitivity and specificity for non-small cell lung cancer (NSCLC) [8, 9].
Statistical analysis
Continuous variables were summarized using median (interquartile range, IQR) and categorical variables with frequency of events (%). Group comparisons were performed using non-paired wise Wilcoxon rank sum test for continuous variables and Fisher’s exact test for categorical variables. Spearman correlation analysis was used to assess the correlation between continuous variables. Two-sided statistical tests were used. Kaplan Meier curves with log-rank tests were used to compare overall survival between groups. Association with survival was quantified using hazard ratios (HRs) and 95% confidence intervals (CIs) assessed with univariate and multivariate Cox proportional hazard models. The nominal significance level was set at p = 0.05. Statistical analysis was performed using R statistical software, version 4.2.2 [16].
As a sensitivity analysis, we conducted univariate age-adjusted Cox proportional hazard models comparing choice of geographic reference (i.e., state-specific vs. U.S.-standardized NDI indices) or definition of NDI (i.e., Messer [18] vs. Powell-Wiley [19, 20] based on Roux and Mair [21]), and we did not observe major differences (Supplemental Table 1).
Results
Patient characteristics
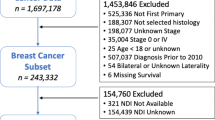
A total of 173 patients with non small cell lung cancer met inclusion/exclusion criteria. Across all participants, the median age was 64 years old, with 53% females, 45% White individuals, 43% Black individuals, with a median of 33 pack-year smoking history, 57% with a former smoking history, 24% current smoking individuals, 20% never smoking persons, median tumor size of 2.5 cm, 52% Stage I, 11% Stage II, 16% Stage III and 21% Stage IV (Table 1). Among Black participants, there were 22 (29%) current smokers, 47 (63%) former smokers, and 6 (8%) who had never smoked. In contrast, among White participants, there were 15 (19%) current smokers, 46 (59%) former smokers, and 17 (22%) who had never smoked (p = 0.04). The median pack-year smoked by Black participants was 40 (IQR 30–50), compared to 35 pack-years (IQR 12–48) among White participants (p = 0.04). A total of n = 85 (49%) and n = 88 (51%) participants were in the low-deprivation group and high-deprivation group, respectively. Baseline characteristics were similar among the two NDI groups, with no statistically significant differences.
Neighborhood deprivation, race, and lung cancer stage
There was a higher proportion of Black patients among 3rd and 4th quartile NDI census tracts and a greater proportion of White or other patients among 1st and 2nd quartile NDI census tracts (p = 0.003; Fig. 1A). Median NDI values were significantly higher among Black patients when compared with White patients (p = 0.001; Fig. 1B). The proportion of patients with stage I lung cancer was higher among patients living within 1st quartile NDI census tracts, and the proportion of patients with stage IV lung cancer was higher for those in 3rd and 4th quartile NDI census tracts (p = 0.001; Fig. 1C). Median NDI showed a trend towards significantly higher values for stage IV lung cancer patients when compared to stage I (p = 0.08; Fig. 1D). Higher NDI showed a trend towards significantly association with advanced lung cancer stage OR 1.15 (95%CI:0.99–1.34; p = 0.06).
Higher neighborhood deprivation index (NDI) values among Black patients and among patients with late lung cancer stages. (A) Proportion of patients by race/ethnicity among the different NDI quartiles. (B) Differences in NDI when comparing patients by race/ethnicity. (C) Proportion of stage at diagnosis among the different NDI quartiles. (D) Differences in NDI when comparing stage at diagnosis
DNA methylation & neighborhood deprivation
There was a significant positive correlation between DNA methylation obtained from liquid biopsies and stage for HOXA7, SOX17, ZFP42, HOXA9, CDO1 and TAC1 (Fig. 2A). Stage IV biopsies had significantly higher DNA methylation than stage I for HOXA7 (p = 0.0001), SOX17 (p = 0.0009) and ZFP42 (p = 0.0007) (Fig. 2B-D). HOXA9 had significantly lower DNA methylation with stage IV than stage I (p = 0.03) (Fig. 2E). When looking at the correlation between DNA methylation and NDI, only HOXA7 DNA methylation was positively correlated with NDI (p = 0.009; Fig. 2H). Patients in 4th quartile NDI census tracts had significantly higher HOXA7 DNA methylation when compared to the remaining NDI quartiles (p = 0.02; Fig. 2I).
Liquid biopsy epigenetic markers for lung cancer DNA methylation are associated with lung cancer stage and NDI. (A) Heatmap of Spearman’s rank correlation coefficient values between lung cancer stage and the DNA methylation for HOXA7, SOX17, ZFP42, HOXA9, CDO1 and TAC1. (B-G) Boxplots showing the differences in median DNA methylation ΔCt values for each of HOXA7, SOX17, ZFP42, HOXA9, CDO1 and TAC1genes when comparing stages, respectively. (H) Heatmap of Spearman’s rank correlation coefficient values between NDI and the DNA methylation for HOXA7, CDO1, TAC1, ZFP42, SOX17, and HOXA9. (I-N) Boxplots showing the differences in median DNA methylation ΔCt values for each HOXA7, CDO1, TAC1, ZFP42, SOX17, and HOXA9genes when comparing NDI quartiles, respectively. (Significance values: ****, P < 0.0001; ***, P < 0.001; **, P < 0.01; *, P < 0.05; ·, P < 0.1; ns, nonsignificant (P > 0.1))
Neighborhood deprivation & survival
Median overall survival was significantly shorter for the high-deprivation census tract (4th quartile NDI) with 75 months when compared to the low-deprivation census tract (1st, 2nd, and 3rd quartiles NDI) with 181 months (p = 0.02; Fig. 3). The 1-, 2- and 5-year survival rates for the high-deprivation census tract (4th quartile NDI) were 80, 70, and 50%, respectively, compared to 91, 84, and 73% in low-deprivation census tract (1st, 2nd, and 3rd quartiles NDI), respectively.
After adjusting for age, living in a 4th quartile NDI census tract was significantly associated with increased mortality with an HR of 2.86 (95%CI: 1.19–6.85; p = 0.02; Fig. 4A) compared to living in a 1st quartile NDI census tract. After adjusting for age, race, stage, and DNA methylation status, living in a high-deprivation census tract (4th quartile NDI) remained associated with a higher mortality with an HR of 1.81 (95%CI:1.03–3.19; p = 0.04; Fig. 4B) when compared to living in a low-deprivation census tract (1st, 2nd, and 3rd quartiles NDI).
Discussion
This study suggests that there may be an association between increasing neighborhood deprivation liquid biopsy DNA methylation, shorter survival, and increased mortality risk. Our epigenetic study is unique in that we quantified neighborhood deprivation defined by Messer et al. [18] a validated 8-factor-based index of socioeconomic disadvantage that combines income, educational level, employment status, and housing in a neighborhood (i.e., census tract), constructed from U.S census data, from two U.S metropolitan regions [19, 20]. Previous epigenetic investigations have observed increased DNA methylation [22] and epigenetic age acceleration [23] in those living in areas with higher deprivation defined by Kind et al. [24], and shorter telomere length was observed in participants of the 1999–2002 National Health and Nutrition Examination Surveys in neighborhoods of high deprivation defined by Roux & Mair [21, 25]. All three mentioned definitions of deprivation use information from surveys conducted by the U.S. Census Bureau and are likely correlated. Indeed, we did not observe large differences between neighborhood deprivation defined by Messer et al. [18] and Roux & Mair [21, 25] in a sensitivity analysis (Supplemental Table 1).
In contrast to many previous studies, ours was conducted in a country without a universal health care system, and we found a greater risk for lung cancer mortality in neighborhoods with greater socioeconomic deprivation relative to countries with access to universal healthcare [26, 27]. This suggests how access to care may shape outcomes within the U.S. employer-based health care system. One of the cities in which this study was conducted, Chicago, is known for having relatively high-income inequality (Gini index of 0.5335) and racial segregation [28]. Previous studies have reported that Black individuals have a higher mortality rate from lung cancer despite a lower amount of smoking, as only 8% of Black individuals who smoke cigarettes report heavy smoking (i.e., at least 25 cigarettes per day), as compared with 28% of White individuals [11, 12]. We found that lung cancer mortality was higher in Black individuals (Supplemental Fig. 1) and that neighborhood deprivation may play an integral role in this phenomenon as there was a greater proportion of Black patients in census tracts with the highest deprivation and a greater proportion of White patients in the census tracts with the least deprivation.
The precise mechanisms by which neighborhood deprivation promotes worse outcomes in lung cancer mortality are incompletely characterized; however, several possibilities exist. The Social Determinants Framework for Cancer Health Equity states that health-related disparities stem from social-structural factors [29]. Multi-level factors, including structural inequities, institutional environments, and living environments, are upstream conditions that create health inequities and consequent disparities in cancer. Neighborhood deprivation measures the economic, physical, social, and service environment that individuals live in, all of which impact healthcare access and outcomes. NDI, therefore, is a surrogate for access to care, which can serve as a significant barrier to receiving optimal care and encompasses health insurance, financial barriers, and physical barriers such as transportation. If a long distance is required to receive treatment and/or an individual does not have access to transportation, this can hinder preventative care, such as lung cancer screening, leading to cancer detection at a later stage. Additionally, the ability to regularly visit an infusion center for anti-cancer therapeutics or radiation therapy can lead to decreased efficacy and, hence, poorer outcomes. Discrimination and mistrust in the medical system amongst minority populations, such as Black individuals, may lead to delays in diagnosis and deter participation in clinical trials [13, 14]. Financial toxicity is a considerable barrier in oncologic care [30, 31]. Even if an individual has access to transportation, additional costs such as gas and parking can make cancer care financially infeasible. Only 54% of NCI-designated cancer centers have free parking available for chemotherapy appointments [32]. Furthermore, individuals from disadvantaged neighborhoods may rely more heavily on work income, leading to financial hardships if unable to work. Additionally, individuals may struggle to find necessary childcare to allow for optimal cancer care. Treatment cost itself represents a momentous financial hurdle. Recent studies estimated that the monthly out-of-pocket expenses for the general cancer population were between $316–741 [30, 31]. Additionally, at six months of follow-up, more than 25% of patients require using personal savings, borrowing from friends or family, changing housing, and selling personal assets, and 18% of patients could not afford basic needs [31]. New lung cancer treatments showed improved survival rates but come with a notable financial burden. Disparities persist, with younger, poorer, non-White patients with private insurance less likely to enroll [33]. Participation can lead to financial strain due to insurance issues, travel costs, lost wages, and lodging for follow-up visits.
The impact of deprivation on psychosocial distress within a neighborhood may also play a critical role in cancer mortality. Many neighborhoods with high deprivation have increased violent crime rates, which can, directly and indirectly, exacerbate psychosocial distress by increasing isolation, decreasing access to safe forms of exercise, and reducing access to healthy food [34]. Low-moderate intensity exercise has been shown to help with cancer-related fatigue, nausea, and pain experienced during active treatment [35]. Without safe access to exercise, individuals from disadvantaged neighborhoods will miss these benefits. Psychosocial stressors in cancer have been shown to promote inflammation and oxidative stress, decreased immune surveillance, and activation of the hypothalamic-pituitary-axis, [36] which may lead to increased cancer mortality. Increased prolonged dysregulation of the stress response, also known as allostatic load, is associated with worse survival in patients with cancer. [37] Furthermore, psychosocial distress may exacerbate tobacco smoking, alcoholism, and other substance use disorders, further augmenting adverse outcomes in lung cancer [38, 39].
Epigenetic modifications include promoter hypermethylation, chromatin remodeling, and microRNA expression and are known to drive biological aggressiveness in lung cancer. Social epigenomics is emerging as a biological mechanism by which socio-environmental factors influence health outcomes and disparities [28]. Epigenetic changes, such as promoter hypermethylation, can be influenced by diet, physical activity, psychosocial stress, and environmental exposures, which may be unique within particular neighborhoods. For instance, exposures to heavy metals such as cadmium and particulate matter in air pollution have been associated with epigenetic changes that promote tumorigenesis [40,41,42]. Several studies have found associations between socioeconomic status and epigenetic changes, including research on aging, depression, inflammation, atherosclerosis, and racial disparities [43,44,45,46,47,48,49,50]. In this current study, we found that HOXA7 DNA methylation was correlated with higher NDI, and methylation of HOXA7, SOX17, ZFP42, HOXA9, CDO1 and TAC1was associated with advanced stage disease in lung cancer.
There are a few limitations to our study. First, the inherent drawbacks associated with a retrospective study design and the scope of our study were limited by including patients only from two major U.S. cities alone. The sample size of our cohorts was another limitation that has potentially hindered the ability of some of our results to reach statistical significance. Furthermore, our study was limited to a specific set of genes associated with lung cancer. As a result, we were unable to investigate the effects of neighborhood deprivation on the entire epigenome scale. Additionally, since the DNA methylation of the six genes we studied is limited to the promoter gene region, we cannot assume that epigenetic changes occurring on different neighborhood deprivation levels are limited to the promoter gene regions. Our patient cohort was skewed towards earlier-stage disease compared to the incidence stage of lung cancer in the general population. A greater effect may be seen if more patients with metastatic disease were included, given the increased number of visits required relative to early-stage disease and disparities in clinical trial enrollment. According to the Cancer Statistics 2024 report from the American Cancer Society (ACS), [1] the proportion of lung cancer patients diagnosed at lower stages is indeed lower than what we observed in our cohort. In our study, patients were enrolled from two distinct institutions: Johns Hopkins School of Medicine and the University of Illinois Health at Chicago. Each of these institutions provided dedicated clinical coordinators who actively approached patients at oncology clinics at the time of diagnosis to facilitate their participation in our research study. We believe that this proactive approach made patients more receptive to their healthcare providers and navigators, leading to earlier detection of lung cancer within this population. This could explain the higher proportion of stage I diagnoses in our study compared to the ACS report. Lastly, further research is warranted to investigate the impact of neighborhood deprivation on epigenomic changes, with the ultimate goal of reducing disparities in lung cancer. While the exact mechanism remains unclear, it is plausible that the hypermethylation could be driven by the envioronmental effect on overexpression of DNA methyltransferases (DNMTs). This is supported by a growing body of evidence showing the impact of ecosystem, lifestyle, and social environment on DNA methylation [51,52,53,54]. Future studies are needed to better understand how disparities in neighborhood deprivation impact DNA methylation. Such research could inform strategies to reduce or prevent this effect.
The findings derived from this study could lead to establishing guidelines for the use of molecular markers in cancer detection, diagnosis, treatment, and monitoring. Biomarkers have the potential to prevent avoidable healthcare costs by providing consistent and accessible liquid-biopsy based screening practices across healthcare settings. Public health strategies can utilize molecular markers to enhance cancer prevention and early detection programs, effectively identifying high-risk individuals through accessible epigenetic testing and providing targeted interventions. Crucially, policy decisions on molecular testing and targeted therapies are essential for ensuring equitable access to underserved populations, thereby enhancing outcomes for these patients regardless of socioeconomic status or geographic location.
Conclusions
Increased neighborhood-level deprivation may be associated with liquid biopsy DNA methylation, shorter survival, and increased mortality. Changes in health care policy that account for community socioeconomic deprivation may enable more equitable improvement of overall lung cancer mortality.
Data availability
Data and materials availability statement: Data generated in this study are available upon request from the corresponding author. The code used to conduct this study analysis is publicly available at: https://github.com/idblr/geomethylation.
Abbreviations
- CDO1:
-
Cysteine dioxygenase type 1
- CI:
-
Confidence intervals
- CT:
-
Computed Tomography
- DNA:
-
Deoxyribonucleic acid
- HOXA7:
-
Homeobox protein Hox-A7
- HOXA9:
-
Homeobox protein Hox-A9
- HR:
-
Hazard ratios
- NCI:
-
National Cancer Institute
- NDI:
-
Neighborhood deprivation index
- NSCLC:
-
Non-small cell lung cancer
- SOX17:
-
SRY-box transcription factor 17
- STROBE:
-
Strengthening the reporting of observational studies in epidemiology
- TAC1:
-
Tachykinin precursor 1
- ZFP42:
-
Zinc finger protein 42
References
Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA: Cancer J Clin 2024.
SEER Cancer Statistics Review (CSR.) 1975–2018 [https://seer.cancer.gov/csr/1975_2018/]
Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–9.
Cockerham WC, Hamby BW, Oates GR. The Social determinants of Chronic Disease. Am J Prev Med. 2017;52(1S1):S5–12.
Galiatsatos P, Woo H, Paulin LM, Kind A, Putcha N, Gassett AJ, Cooper CB, Dransfield MT, Parekh TM, Oates GR, et al. The Association between Neighborhood Socioeconomic Disadvantage and Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2020;15:981–93.
Singh GK, Jemal A. Socioeconomic and Racial/Ethnic disparities in Cancer Mortality, incidence, and Survival in the United States, 1950–2014: over six decades of changing patterns and widening inequalities. J Environ Public Health 2017, 2017:2819372.
Adie Y, Kats DJ, Tlimat A, Perzynski A, Dalton J, Gunzler D, Tarabichi Y. Neighborhood Disadvantage and Lung Cancer incidence in ever-smokers at a Safety Net Health-Care System: a retrospective study. Chest. 2020;157(4):1021–9.
Hulbert A, Jusue-Torres I, Stark A, Chen C, Rodgers K, Lee B, Griffin C, Yang A, Huang P, Wrangle J, et al. Early detection of Lung Cancer using DNA promoter hypermethylation in plasma and Sputum. Clin Cancer Res. 2017;23(8):1998–2005.
Liu B, Ricarte Filho J, Mallisetty A, Villani C, Kottorou A, Rodgers K, Chen C, Ito T, Holmes K, Gastala N, et al. Detection of promoter DNA methylation in urine and plasma aids the detection of Non-small Cell Lung Cancer. Clin Cancer Res. 2020;26(16):4339–48.
Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, Bruno DS, Chang JY, Chirieac LR, DeCamp M, et al. NCCN Guidelines(R) Insights: Non-small Cell Lung Cancer, Version 2.2023. J Natl Compr Canc Netw. 2023;21(4):340–50.
Haiman CA, Stram DO, Wilkens LR, Pike MC, Kolonel LN, Henderson BE, Le Marchand L. Ethnic and racial differences in the smoking-related risk of lung cancer. N Engl J Med. 2006;354(4):333–42.
DeSantis CE, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Cancer statistics for African americans, 2019. CA Cancer J Clin. 2019;69(3):211–33.
Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97(7):1283–9.
Mullins MA, Peres LC, Alberg AJ, Bandera EV, Barnholtz-Sloan JS, Bondy ML, Funkhouser E, Moorman PG, Peters ES, Terry PD, et al. Perceived discrimination, trust in physicians, and prolonged symptom duration before ovarian cancer diagnosis in the African American Cancer Epidemiology Study. Cancer. 2019;125(24):4442–51.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
R Core Team. In: Vienna, editor. R: a Language and Environment for Statistical Computing. Austria: R Foundation for Statistical Computing; 2022.
Budler ID. Ndi: Neighborhood Deprivation Indices. The Comprehensive R Archive Network 2022, v0.1.2.
Messer LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, Elo I, Burke JG, O’Campo P. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041–62.
Andrews MR, Tamura K, Claudel SE, Xu S, Ceasar JN, Collins BS, Langerman S, Mitchell VM, Baumer Y, Powell-Wiley TM. Geospatial analysis of Neighborhood Deprivation Index (NDI) for the United States by County. J Maps. 2020;16(1):101–12.
Slotman BA, Stinchcomb DG, Powell-Wiley TM, Ostendorf DM, Saelens BE, Gorin AA, Zenk SN, Berrigan D. Environmental data and methods from the Accumulating Data to optimally predict obesity treatment (ADOPT) core measures environmental working group. Data Brief. 2022;41:108002.
Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–45.
Shen J, Fuemmeler BF, Sheppard VB, Bear HD, Song R, Chow WH, Zhao H. Neighborhood disadvantage and biological aging biomarkers among breast cancer patients. Sci Rep. 2022;12(1):11006.
Lawrence KG, Kresovich JK, O’Brien KM, Hoang TT, Xu Z, Taylor JA, Sandler DP. Association of Neighborhood Deprivation with Epigenetic Aging using 4 Clock Metrics. JAMA Netw Open. 2020;3(11):e2024329.
Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible - The Neighborhood Atlas. N Engl J Med. 2018;378(26):2456–8.
Diez Roux AV, Borrell LN, Haan M, Jackson SA, Schultz R. Neighbourhood environments and mortality in an elderly cohort: results from the cardiovascular health study. J Epidemiol Community Health. 2004;58(11):917–23.
Panczak R, Galobardes B, Voorpostel M, Spoerri A, Zwahlen M, Egger M, Swiss National C. Swiss Household P: a Swiss neighbourhood index of socioeconomic position: development and association with mortality. J Epidemiol Community Health. 2012;66(12):1129–36.
Li X, Sundquist J, Zoller B, Sundquist K. Neighborhood deprivation and lung cancer incidence and mortality: a multilevel analysis from Sweden. J Thorac Oncol. 2015;10(2):256–63.
Mancilla VJ, Peeri NC, Silzer T, Basha R, Felini M, Jones HP, Phillips N, Tao MH, Thyagarajan S, Vishwanatha JK. Understanding the Interplay between Health Disparities and Epigenomics. Front Genet. 2020;11:903.
Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC. Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J Clin. 2020;70(1):31–46.
Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR. Financial hardships experienced by Cancer survivors: a systematic review. J Natl Cancer Inst 2017, 109(2).
Friedes C, Hazell SZ, Fu W, Hu C, Voong RK, Lee B, Feliciano JL, Nicholas LH, McNutt TR, Han P, et al. Longitudinal trends of Financial toxicity in patients with Lung Cancer: a prospective cohort study. JCO Oncol Pract. 2021;17(8):e1094–109.
Lee A, Shah K, Chino F. Assessment of parking fees at National Cancer Institute-Designated Cancer Treatment Centers. JAMA Oncol. 2020;6(8):1295–7.
Chino F, Zafar SY. Financial Toxicity and Equitable Access to clinical trials. Am Soc Clin Oncol Educ Book. 2019;39:11–8.
Richardson AS, Troxel WM, Ghosh-Dastidar M, Hunter GP, Beckman R, Colabianchi N, Collins RL, Dubowitz T. Pathways through which higher neighborhood crime is longitudinally associated with greater body mass index. Int J Behav Nutr Phys Act. 2017;14(1):155.
van Waart H, Stuiver MM, van Harten WH, Geleijn E, Kieffer JM, Buffart LM, de Maaker-Berkhof M, Boven E, Schrama J, Geenen MM, et al. Effect of low-intensity physical activity and moderate- to High-Intensity Physical Exercise during Adjuvant Chemotherapy on physical fitness, fatigue, and Chemotherapy Completion Rates: results of the PACES Randomized Clinical Trial. J Clin Oncol. 2015;33(17):1918–27.
Bortolato B, Hyphantis TN, Valpione S, Perini G, Maes M, Morris G, Kubera M, Kohler CA, Fernandes BS, Stubbs B, et al. Depression in cancer: the many biobehavioral pathways driving tumor progression. Cancer Treat Rev. 2017;52:58–70.
Obeng-Gyasi S, Graham N, Kumar S, Lee JW, Jacobus S, Weiss M, Cella D, Zhao F, Ip EH, O’Connell N, et al. Examining allostatic load, neighborhood socioeconomic status, symptom burden and mortality in multiple myeloma patients. Blood Cancer J. 2022;12(4):53.
Rojewski AM, Tanner NT, Dai L, Ravenel JG, Gebregziabher M, Silvestri GA, Toll BA. Tobacco Dependence predicts higher Lung Cancer and Mortality Rates and Lower Rates of Smoking Cessation in the National Lung Screening Trial. Chest. 2018;154(1):110–8.
Edwards CV, Sheikh AR, Dennis MJ, Hunter A, Mackay ZP, Catudal EC, Elias R, Cabral HJ, Sarosiek SR, Tapan U. The impact of substance use on health care utilization, treatment, and outcomes in patients with non-small cell lung cancer. J Thorac Dis. 2022;14(10):3865–75.
Nawrot TS, Martens DS, Hara A, Plusquin M, Vangronsveld J, Roels HA, Staessen JA. Association of total cancer and lung cancer with environmental exposure to cadmium: the meta-analytical evidence. Cancer Causes Control. 2015;26(9):1281–8.
Li J, Li WX, Bai C, Song Y. Particulate matter-induced epigenetic changes and lung cancer. Clin Respir J. 2017;11(5):539–46.
Hill W, Lim EL, Weeden CE, Lee C, Augustine M, Chen K, Kuan FC, Marongiu F, Evans EJ Jr., Moore DA, et al. Lung adenocarcinoma promotion by air pollutants. Nature. 2023;616(7955):159–67.
Lam LL, Emberly E, Fraser HB, Neumann SM, Chen E, Miller GE, Kobor MS. Factors underlying variable DNA methylation in a human community cohort. Proc Natl Acad Sci U S A. 2012;109(Suppl 2):17253–60.
Tehranifar P, Wu HC, Fan X, Flom JD, Ferris JS, Cho YH, Gonzalez K, Santella RM, Terry MB. Early life socioeconomic factors and genomic DNA methylation in mid-life. Epigenetics. 2013;8(1):23–7.
Needham BL, Smith JA, Zhao W, Wang X, Mukherjee B, Kardia SL, Shively CA, Seeman TE, Liu Y, Diez Roux AV. Life course socioeconomic status and DNA methylation in genes related to stress reactivity and inflammation: the multi-ethnic study of atherosclerosis. Epigenetics. 2015;10(10):958–69.
Swartz JR, Hariri AR, Williamson DE. An epigenetic mechanism links socioeconomic status to changes in depression-related brain function in high-risk adolescents. Mol Psychiatry. 2017;22(2):209–14.
McDade TW, Ryan C, Jones MJ, MacIsaac JL, Morin AM, Meyer JM, Borja JB, Miller GE, Kobor MS, Kuzawa CW. Social and physical environments early in development predict DNA methylation of inflammatory genes in young adulthood. Proc Natl Acad Sci U S A. 2017;114(29):7611–6.
Santos HP Jr., Bhattacharya A, Martin EM, Addo K, Psioda M, Smeester L, Joseph RM, Hooper SR, Frazier JA, Kuban KC, et al. Epigenome-wide DNA methylation in placentas from preterm infants: association with maternal socioeconomic status. Epigenetics. 2019;14(8):751–65.
Laubach ZM, Perng W, Cardenas A, Rifas-Shiman SL, Oken E, DeMeo D, Litonjua AA, Duca RC, Godderis L, Baccarelli A, et al. Socioeconomic status and DNA methylation from birth through mid-childhood: a prospective study in Project viva. Epigenomics. 2019;11(12):1413–27.
Yannatos I, Stites S, Brown RT, McMillan CT. Contributions of neighborhood social environment and air pollution exposure to Black-White disparities in epigenetic aging. PLoS ONE. 2023;18(7):e0287112.
Baccarelli A, Tarantini L, Wright RO, Bollati V, Litonjua AA, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J. Repetitive element DNA methylation and circulating endothelial and inflammation markers in the VA normative aging study. Epigenetics. 2010;5(3):222–8.
Nwanaji-Enwerem JC, Colicino E, Trevisi L, Kloog I, Just AC, Shen J, Brennan K, Dereix A, Hou L, Vokonas P et al. Long-term ambient particle exposures and blood DNA methylation age: findings from the VA normative aging study. Environ Epigenet 2016, 2(2).
Huang SK, Tripathi P, Koneva LA, Cavalcante RG, Craig N, Scruggs AM, Sartor MA, Deng F, Chen Y. Effect of concentration and duration of particulate matter exposure on the transcriptome and DNA methylome of bronchial epithelial cells. Environ Epigenetics. 2021;7(1):dvaa022.
Wu H, Eckhardt CM, Baccarelli AA. Molecular mechanisms of environmental exposures and human disease. Nat Rev Genet. 2023;24(5):332–44.
Acknowledgements
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Departments of Veterans Affairs and Health and Human Services or the United States government.
Funding
A.H: University of Illinois at Chicago Department of Surgery. A.H: Jesse Brown VA Medical Center LPOP (Lung Precision Oncology Program).
Author information
Authors and Affiliations
Contributions
KK: Conceptualization, Methodology, Investigation, Data Curation, Writing - Original Draft, Writing - Review & Editing. IJ: Conceptualization, Methodology, Software, Validation, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Visualization. IB: Conceptualization, Methodology, Software, Validation, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Visualization. ER: Methodology, Validation, Writing - Original Draft, Writing - Review & Editing, Supervision. AM: Methodology, Investigation, Resources, Data Curation, Writing - Original Draft, Writing - Review & Editing. KR: Writing - Original Draft, Writing - Review & Editing. BL: Methodology, Validation, Writing - Original Draft, Writing - Review & Editing, Supervision. MM: Writing - Original Draft, Writing - Review & Editing. MP: Writing - Original Draft, Writing - Review & Editing. RN: Writing - Original Draft, Writing - Review & Editing. FW: Writing - Original Draft, Writing - Review & Editing. IR: Writing - Original Draft, Writing - Review & Editing. JH: Writing - Original Draft, Writing - Review & Editing, Supervision. MB: Writing - Original Draft, Writing - Review & Editing, Supervision. LF: Writing - Original Draft, Writing - Review & Editing, Funding acquisition. MA: Methodology, Validation, Writing - Original Draft, Writing - Review & Editing, Supervision. AH: Conceptualization, Methodology, Software, Validation, Investigation, Resources, Data Curation, Writing - Original Draft, Writing - Review & Editing, Supervision, Project administration, Funding acquisition.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study conforms with The Code of Ethics of the World Medical Association (Declaration of Helsinki). Institutional Review Board approval was obtained prior to study initiation (IRB #2017–1286 for University of Illinois at Chicago and NA_00005998 for Johns Hopkins University School of Medicine, respectively), and all patients signed informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kennedy, K., Jusue-Torres, I., Buller, I.D. et al. Neighborhood-level deprivation and survival in lung cancer. BMC Cancer 24, 959 (2024). https://doi.org/10.1186/s12885-024-12720-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12720-w