Abstract
Background
This study aimed to compare the survival outcome and side effects in patients with primary high-grade glioma (HGG) who received carbon ion radiotherapy (CIRT) alone or as a boost strategy after photon radiation (photon + CIRTboost).
Patients and methods
Thirty-four (34) patients with histologically confirmed HGG and received CIRT alone or Photon + CIRTboost, with concurrent temozolomide between 2020.03–2023.08 in Wuwei Cancer Hospital & Institute, China were retrospectively reviewed. Overall survival (OS), progression-free survival (PFS), and acute and late toxicities were analyzed and compared.
Results
Eight WHO grade 3 and 26 grade 4 patients were included in the analysis. The median PFS in the CIRT alone and Photon + CIRTboost groups were 15 and 19 months respectively for all HGG cases, and 15 and 17.5 months respectively for grade 4 cases. The median OS in the CIRT alone and Photon + CIRTboost groups were 28 and 31 months respectively for all HGG cases, and 21 and 19 months respectively for grade 4 cases. No significant difference in these survival outcomes was observed between the CIRT alone and Photon + CIRTboost groups. Only grade 1 acute toxicities were observed in CIRT alone and Photon + CIRTboost groups. CIRT alone group had a significantly lower ratio of acute toxicities compared to Photon + CIRTboost (3/18 vs. 9/16, p = 0.03). No significant difference in late toxicities was observed.
Conclusion
Both CIRT alone and Photon + CIRTboost with concurrent temozolomide are safe, without significant differences in PFS and OS in HGG patients. It is meaningful to explore whether dose escalation of CIRTboost might improve survival outcomes of HGG patients in future randomized trials.
Similar content being viewed by others
Introduction
High-grade glioma (HGG) is the most commonly diagnosed and aggressive form of brain cancer in adults. The current NCCN guidelines recommend standard treatment of maximal safe resection for resectable lesions, followed by concurrent chemoradiotherapy with temozolomide and 6 cycles of adjuvant temozolomide chemotherapy [12]. For unresectable lesions, biopsy or subtotal resection is performed, followed by concurrent chemoradiotherapy and adjuvant chemotherapy [12]. Despite treatment, the median survival time for patients with glioblastoma, the most aggressive HGG, is around 15–18 months [7, 14, 15, 23].
Carbon ion radiotherapy (CIRT) is a type of heavy particle radiotherapy with distinct physical and biological properties compared to standard photon therapy. It has higher conformity and steeper dose gradients due to the Bragg peak [4]. CIRT also exerts significantly stronger biological effects than conventional X-rays and proton beams, primarily by inducing double-strand DNA breaks. The relative biological effectiveness (RBE) of carbon ions in treating glioblastoma ranges between 3 and 5 [28]. Due to these unique attributes, CIRT might be a promising treatment approach for radioresistant tumors in critical organs, such as gliomas in the brain [18]. CIRT can potentially provide clinical benefits for gliomas [28]. Clinical trials have explored the use of CIRT as an adjunctive boost to conventional photon radiotherapy postoperatively, in combination with concurrent chemotherapy [13, 19, 28], or alone for WHO grade 2 diffuse astrocytomas [11]. In a phase I/II clinical trial conducted in Japan, patients with glioma were treated with photon therapy and chemotherapy followed by CIRT. CIRT dose escalation from 16.8 GyE to 24.8 GyE resulted in a median overall survival (OS) of 35 months for anaplastic astrocytoma patients and 17 months for glioblastoma patients [19]. Another study in China involving 50 patients (34 with glioblastomas and 16 with anaplastic gliomas) treated with proton therapy or a proton plus carbon ion boost reported 12- and 18-month OS rates of 87.8% and 72.8%, respectively [13]. For CIRT alone in patients with WHO grade 2 diffuse astrocytomas, the median progression-free survival (PFS) was 18 months for the low-dose (46.2 GyE) group and 91 months for the high-dose group (55.2 GyE) [11].
According to data from a previous phase I/II trial, CIRT is generally safe for normal brain tissues, providing a foundation for treating gliomas with carbon ion beams [24]. However, Kong et al.’s reported 11 cases of grade I-II late side effects of radiation-induced brain necrosis after particle therapy [13]. Theoretically, carbon ions are high-linear energy transfer (LET) radiation with a high RBE value in the peak region. It causes significant tissue damage due to their high biological effectiveness. In the case of glioma target areas, an area up to 2 cm outside the GTV needs to be irradiated in the subclinical region. However, carbon ions to these regions may cause unpredictable radiation damage to normal brain tissue. Severe late toxicities (necrosis) in the normal brain after irradiation with CIRT alone was observed in one previous study [11]. Therefore, CIRT-induced brain injury cannot be ignored during therapy.
Exploring how to better utilize the physical and dosimetric advantages of carbon ions to improve tumor control, while reducing the incidence of high-dose radiation damage to surrounding brain tissues can provide new treatment recommendations for glioma radiotherapy. The current dose-adverse reaction relationship of carbon ions acting on brain tissue remains unclear. How carbon ions can be safely and rationally used for glioma treatment and the corresponding radiobiological effects of radiation brain injury need to be further studied. In this study, we retrospectively analyzed the survival outcome (OS and PFS) and side effects in patients with primary HGG and received CIRT alone or as a boost strategy after photon radiation in Wuwei Cancer Hospital & Institute, China from 2020.03–2023.02.
Materials and methods
Patients reviewed
This study was approved by the Ethical Committee of Wuwei Cancer Hospital & Institute, China (Approval no. 2022-ethicalcheck-16). Thirty-four (34) patients with histologically confirmed high-grade glioma and received CIRT alone or Photon + CIRTboost between 2020.03–2023.08 in Wuwei Cancer Hospital & Institute, China were retrospectively reviewed. Informed consent was obtained from all patients included. The following criteria were applied to select appropriate patients for this analysis:
-
1.
Age ≥ 14 and ≤ 80 years old;
-
2.
High-grade gliomas that can be diagnosed according to the 5th edition of the "WHO Classification of Central Nervous System Tumors" including grade 3 oligodendroglioma (1p/19 codeleted, IDH-mutant); grade 3 IDH-mutant astrocytoma; grade 4 IDH-mutant astrocytoma, grade 4 IDH wild-type glioblastoma and pediatric-type diffuse high-grade gliomas [21].
-
3.
Patients with these tumors, regardless of the completeness of the surgery (total resection, subtotal resection or partial resection after surgery, as well as after stereotactic or open biopsy.
-
4.
No history of other malignant tumors (except for cured skin cancer and stage 0 cervical cancer).
-
5.
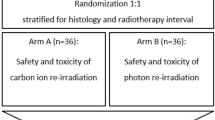
Patients received photon radiotherapy (Volumetric Modulated Arc Therapy, VMAT or Intensity-modulated radiation therapy, IMRT, 50 Gy/25F) plus CIRT boost (CIRTboost, 24.8 Gy (RBE)/8 Fx) (defined as Photon + CIRTboost) or CIRT alone (60.0 Gy (RBE)/16Fx). Concurrent and adjuvant TMZ was used for all patients (Concurrent TMZ 75 mg/m2, qd; adjuvant TMZ 150–200 mg/m2, D1-5/28 days).
Radiation strategy
The therapeutic decision of Photon + CIRTboost or CIRT alone was made by full consultation with the patients, with known pros and cons fully communicated. Patients included in this study received the standardized radiation strategy below:
Normal Tissue Dose Constraints: Photon radiotherapy dose constraints for first course: Visual pathway (evaluate optic chiasm and optic nerve separately) D1 < 54 Gy; brainstem D1 ≤ 54 Gy, V60 Gy < 1% PRV; temporal lobe V60 Gy ≤ 1%; spinal cord V50Gy < 1% PRV, Dmax < 45 Gy; eyeball Dmean < 35 Gy; lens Dmean < 6 Gy, D1 < 8 GyE; cochlea V55 Gy < 5%, Dmean < 36 Gy; hippocampus V40 < 5.0 Gy, Dmean < 7 Gy, Dmax < 10 Gy.
CIRT dose constraints for the second course: during the second-course planning and target delineation, distance from the normal organs at risk (OAR) such as visual pathway and brainstem were kept > 3 mm. SOBP region was conformed to GTV as much as possible. Thus normal tissue dose constraints are: Visual pathway (evaluate optic chiasm and optic nerve separately) D20 < 4 Gy (RBE); brainstem Dmax < 5 Gy (RBE), D1 ≤ 3 Gy (RBE); hippocampus V40 < 2.5 Gy (RBE), Dmean < 3 Gy (RBE), Dmax < 7 Gy (RBE).
Target delineation followed guidelines in Diagnosis and Treatment Guidelines for Glioma (2022 Edition) by National Health Commission of China. Target definition was performed according to the NCCN guidelines 2022. Gross tumor volume (GTV) is MRI T1 enhancement or T2-FLAIR abnormal signals and surgical cavity, excluding peritumoral edema. Clinical target volume (CTV)1 expands GTV by 2 cm, for bony structures, ventricles, falx cerebri, tentorium cerebelli, optic apparatus, brainstem etc., expand by 0–0.5 cm, edema is included in CTV1 of first course. CTV2 of second course only includes MRI T1 enhancement or T2-fluid attenuated inversion recovery (FLAIR) abnormal signals, residual/recurrent tumors and/or postoperative cavity with appropriate expansions. planning target volume (PTV) 1 and PTV2 expand CTV1 and CTV2 by 1–3 mm to account for setup errors plus particle range uncertainties.
Prescription doses followed an early publication [19]. PTV1 receives photon radiotherapy first (starting within 30 days post-op), 50 Gy in 25 fractions. After photon RT, PTV2 receives carbon ion RT, 24.8 Gy (RBE) in 8 fractions; 3.1 Gy (RBE)/fx; 1fx/day, 5 days/week. A 95% prescription dose line should cover 95% of CTV or GTV while ensuring normal tissues are tolerable.
Eclipse 15.5 was used for photon planning. ci-Plan was used for passively scattered carbon ion planning. After carbon ion plan was approved, compensators were fabricated. Dose was verified before the plan was transferred to the ciTreat system for treatment.
TMZ administration
The stupp regimen was used for TMZ administration. Concurrent oral TMZ (75 mg/(m2·d)) was provided during radiotherapy for 42 days. 4 weeks after the completion of concurrent chemoradiotherapy, adjuvant chemotherapy stage was initiated. Oral TMZ (150–200 mg/(m2·d)) was provided for 5 days, repeated every 28 days, a total of 6 cycles.
Therapeutic responses and Toxicity assessment
Patients were followed and the therapeutic responses (Complete response (CR), partial response (PR), disease stability (SD), and disease progression (PD)) were assessed following The Response Evaluation Criteria in Solid Tumors (RECIST) [9].
Toxicities that occurred either during or within three months of starting CIRT were categorized as acute toxicities. On the other hand, toxicities that developed after three months from the initiation of CIRT or persisted for at least three months were classified as late toxicities. Both acute and late toxicities were assessed and scored according to the CTCAE, v4.03.
Statistical analysis
Progression-free survival (PFS) was defined as the time interval from the date of diagnosis to the date of disease progression or recurrence. Overall survival (OS) was defined as the time interval from the date of pathological diagnosis of high-grade glioma (HGG) to the date of death from any cause. Survival difference was assessed by generating Kaplan–Meier curves, with log-rank tests to compare the statistical difference. Characteristic and toxicity comparison between CIRT alone and Photon + CIRTboost was conducted by Fisher's exact or Chi-square test, except age comparison was performed using unpaired t-test. The Cox’s proportional hazards model [6] was applied for univariate analysis of therapeutic strategies (CIRT alone vs. Photon + CIRTboost) for PFS and OS. The assumption of proportional hazards was examined by the Schoenfeld residuals and log–log survival plots. p < 0.05 was considered statistical significance.
Results
Patient characteristics
Consecutive and non-selected 34 patients with histologically confirmed high-grade glioma meeting the inclusion criteria described above were retrospectively reviewed. Their clinical characteristics are summarized in Table 1. The 34 cases included 6 WHO grade 3 HGG and 28 WHO grade 4 HGG. Eighteen (18) cases received CIRT alone and 16 had Photon + CIRTboost therapy (Table 1). IDH1/2 gene mutation status was confirmed in 32 cases (Table 1). Then, we compared the clinical characteristics between CIRT alone and Photon + CIRTboost therapy groups. No significant differences were observed in gender, age, WHO grade, KPS scores, IDH1/2 gene mutations, or MGMT gene promoter methylation between the two groups (Table 2). The PFS and OS of all HGG and grade 4 cases are presented in Fig. 1. Median PFS was 15 months in both all HGG and grade 4 HGG (Fig. 1A). Median OS was 28 and 21 months in all HGG and grade 4 HGG (Fig. 1B).
PFS and OS comparison between CIRT alone and Photon + CIRTboost groups
The median follow-up for the CIRT alone and Photon + CIRTboost groups were 16.00 months (range, 3–38 months) and 13.00 months (range, 3–31 months). 13 patients had died at the time of this analysis (n = 9 in CIRT alone group and n = 4 in Photon + CIRTboost group).
For all HGG cases in CIRT alone group, the 12- and 18-month PFS rates were 64.7% (95%CI, 37.7%-82.3%) and 25.88% (95%CI, 8.1%-48.3%), respectively (Fig. 2A). In the Photon + CIRTboost group, the 12- and 18-month PFS rates were 72.92% (95%CI, 36.77%-90.5%) and 58.3% (95%CI, 21.2%-82.9%), respectively (Fig. 2A). The median PFS of the CIRT alone and Photon + CIRTboost group were 15 months and 19 months, respectively. Although the PFS seems longer in the Photon + CIRTboost group than in the CIRT alone group, no significant difference was observed (log-rank p = 0.32) (Fig. 2A). In the univariate Cox regression model, the risk of progression was similar between the two therapeutic strategies (CIRT alone vs. Photon + CIRTboost, HR: 1.678, 95%CI: 0.589–4.780, p = 0.332) (Supplementary Table 1).
PFS and OS comparison between CIRT alone and Photon + CIRTboost groups. A-D Kaplan–Meier curves for PFS (A and C) and OS (B and D) were generated to compare the survival differences between CIRT alone and Photon + CIRTboost groups. Asymmetrical 95%CI was estimated (dot curves). Log-rank p values were calculated
For all HGG cases in CIRT alone group, the 12-, 18- and 24-month OS rates were 100%, 63.4% (95%CI, 35.8%-81.6%), and 50.7% (95%CI, 25.1%-71.6%) respectively (Fig. 2B). In Photon + CIRTboost group, the 12-,18- and 24-month OS rates were 90.0% (95%CI, 47.3%-98.5%), 57.9% (95%CI, 15.3%-85.2%) and 57.9% (95%CI, 15.3%-85.2%) respectively (Fig. 2B). The median OS of the CIRT alone and the Photon + CIRTboost group were 28 and 31 months, respectively. No significant difference was observed (log-rank p = 0.97) (Fig. 2B). In the univariate Cox regression model, the risk of death was similar between the two therapeutic strategies (CIRT alone vs. Photon + CIRTboost, HR: 0.926, 95%CI: 0.278–3.083, p = 0.900) (Supplementary Table 2).
For cases with grade 4 HGG in the CIRT alone group, the 12- and 18-month PFS rates were 53.9% (95%CI, 24.8%-76.0%) and 23.1% (95%CI, 5.6%-47.5%), respectively (Fig. 2C). In the Photon + CIRTboost group, the 12- and 18-month PFS rates were 66.7% (95%CI, 27.2%-88.1%) and 50.0% (95%CI, 13.4%-78.7%), respectively (Fig. 2C). The median PFS was 10 and 17.5 months, respectively. Although the PFS seems longer in the Photon + CIRTboost group than in the CIRT alone group, no significant difference was observed (log-rank p = 0.45) (Fig. 2C). In the univariate Cox regression model, the risk of progression was similar between the two therapeutic strategies (CIRT alone vs. Photon + CIRTboost, HR: 1.546, 95%CI: 0.527–4.535, p = 0.427) (Supplementary Table 3).
For cases with grade 4 HGG in the CIRT alone group, the 12-,18- and 24-month OS rates were 100%, 61.5% (95%CI, 30.8%-81.8%) and 38.5% (95%CI, 14.1%-62.8%), respectively (Fig. 2D). In the Photon + CIRTboost group, the 12-, 18- and 24-month OS rates were 87.5% (95%CI, 38.7%-98.1%), 72.9% (95%CI, 27.6%-92.5%) and 48.6% (95%CI, 7.7%-81.6%), respectively (Fig. 2D). The median OS of the CIRT alone and the Photon + CIRTboost group were 21 and 19 months, respectively. No significant difference was observed (log-rank p = 0.80) (Fig. 2D). In the univariate Cox regression model, the risk of death was similar between the two therapeutic strategies (CIRT alone vs. Photon + CIRTboost, HR: 1.152, 95%CI: 0.347–3.822, p = 0.818) (Supplementary Table 4).
Therapeutic responses
The therapeutic responses of the CIRT alone and the Photon + CIRTboost group were summarized in Table 3. Generally, no significant differences were observed in DCRs or ORRs between CIRT alone and Photon + CIRTboost groups, either in all HGG or WHO grade 4 only cases (Table 3).
At 12 months, the DCRs were 68.8% and 75.0% for all HGG cases in the CIRT alone and the Photon + CIRTboost group, respectively (Table 3). In WHO grade 4 cases, the DCRs were 58.3% and 70.0% respectively (Table 3). The ORRs were 43.8% and 66.7% in the CIRT alone and the Photon + CIRTboost group for all HGG cases, respectively (Table 3). In WHO grade 4 cases, the ORRs were 33.3% and 60.0%, respectively (Table 3).
Subgroup analysis by gender, grade, IDH1/2 mutation status, and KPS scores
To explore the clinical characteristics that might influence survival in patients who received CIRT alone or Photon + CIRTboost, we performed subgroup PFS and OS analysis. For CIRT alone therapy, female patients and patients with IDH1/2 mutations had significantly better PFS (Fig. 3A and C) and OS (Fig. 4A and C) compared to their respective counterparts. No significant difference was observed by WHO tumor grade or KPS score separation (Figs. 3B and D and 4B and D). For Photon + CIRTboost therapy, no significant difference in PFS or OS was observed in all subgroup analyses (Figs. 3E-H and 4E-H). The typical dosimetry and MRI images of two representative CR cases in CIRT alone (Fig. 5A-B) and Photon + CIRTboost (Fig. 6A, B) were provided. For CIRT alone, three layered doses were designed, including GTV: 60.0 Gy (RBE)/20 Fx, V1: 30.0 Gy (RBE)/10 Fx, V2: 45.0 Gy (RBE)/15 Fx. Sequential boosting was performed using a three-course plan, gradually decreasing the target area (Fig. 5A).
Subgroup analysis of PFS in patients with different clinical characteristics. A-H In patients who received CIRT alone (A-D) or Photon + CIRTboost (E–H), Kaplan–Meier curves for PFS were generated to compare the survival differences between gender (A and E), WHO grade 3 and 4 (B and F), IDH1/2 wild-type (WT) and mutant (MT) (C and G) and KPS > 80 and ≤ 80 (D and H)
Subgroup analysis of OS in patients with different clinical characteristics. A-H In patients who received CIRT alone (A-D) or Photon + CIRTboost (E–H), Kaplan–Meier curves for OS were generated to compare the survival differences between gender (A and E), WHO grade 3 and 4 (B and F), IDH1/2 wild-type (WT) and mutant (MT) (C and G) and KPS > 80 and ≤ 80 (D and H)
Acute and late toxicities
Only grade 1 acute toxicities were observed in CIRT alone and Photon + CIRTboost groups (Table 4). CIRT alone group had a significantly lower ratio of acute toxicities compared to Photon + CIRTboost (3/18 vs. 9/16, p = 0.03) (Table 4). Similar rates of late toxicities were observed between the two groups (5/18 vs. 2/16, p = 0.40) (Table 4). However, all late toxicities of Photon + CIRTboost were grade 1. 4/5 were grade 2 in the CIRT alone group, including one case of cerebral necrosis (Table 4).
Discussion
Over the past 10 years, there has been general agreement about how to manage gliomas. For newly diagnosed HGGs, the standard treatment approach is maximally safe surgery, concurrent chemotherapy with temozolomide (75 mg/m2 daily for 42 days) plus radiotherapy, additional chemotherapy with temozolomide (150–200 mg/m2 for 5 days every 28 days) for 6–12 cycles, in combination with tumor treatment fields (TTF) in some countries [12, 15]. Patients enrolled in clinical trials testing new systemic therapies and those treated in regular clinical practice, typically receive 60 Gy of radiation delivered in 30 fractions [27]. This regimen has become the standard after multiple prior failed attempts at dose escalation, including hyperfractionation [2], stereotactic radiosurgery [22, 26], and brachytherapy boosts [16]. Despite promising results from phase I studies and modern dose escalation approaches [25], the NRG Oncology BN001 phase II study (NCT02179086) reconfirmed the lack of benefit from escalating the photon radiation dose to 75 Gy in 30 fractions, even with concurrent radiosensitizing chemotherapy [10]. Median OS was still 18.7 months, without significant improvement compared to standard-dose (60 Gy) [10].
In addition to clinical trials evaluating the dose and fractionation of photon radiation, recent research has also concentrated on the dosimetric and physical properties of particle therapies to improve tumor control. However, a randomized, prospective phase II trial found no difference in the onset of cognitive decline between proton therapy and modern photon techniques [5]. A secondary analysis also found no differences in PFS or response assessment (Al [1]). Carbon-ion beam-based strategies were also explored in clinical settings, either alone or as a boost after initial proton or photon therapy. A recent study reported the first use of particle therapy plus concurrent temozolomide to treat high-grade gliomas. They observed 18-month OS and PFS rates of 72.8% and 59.8%, respectively, with CIRTboost therapy and temozolomide [13]. In this study, we observed that in grade 4 HGG in received Photon + CIRTboost therapy, the 12- and 18-month PFS rates were 66.7% (95%CI, 27.2%-88.1%) and 50.0% (95%CI, 13.4%-78.7%), while the 12- and 18-month OS rates were 87.5% (95%CI, 38.7%-98.1%) and 72.9% (95%CI, 27.6%-92.5%). These findings are consistent with data from Kong et al.. The median OS was 19 months and the 24-month OS rate drastically dropped to 48.6% (95%CI, 7.7%-81.6%). CIRT alone had no statistically inferior effect in terms of PFS and OS compared to Photon + CIRTboost therapy.
Our subgroup analysis found that when CIRT was provided alone, the PFS and OS differences in patients stratified by gender and IDH1/2 mutation status were statistically significant. Thu, these characteristics should be carefully considered if CIRT was provided alone. However, these subgroup data should be carefully interpreted since the sample size in each subgroup is relatively small. In addition, for the difference in grade separation, only 2 or 3 grade 3 patients were included in one group. We could not make reliable conclusions based on such a small sample size. In patients with Photon + CIRTboost therapy, these characteristics might not affect survival outcomes.
In terms of acute and late toxicity, only grade 1 toxicities were observed in Photon + CIRTboost, although it had a significantly higher ratio of acute toxicities than CIRT alone. Grade 3 toxicities were not observed in both therapeutic strategies.
This study also has several limitations. Firstly, the relatively small number of patients reviewed might hamper the statistical power. Secondly, this study is a retrospective analysis. Potential selection bias was inevitable. Thirdly, over 50% of patients in this study had no MGMT promoter methylation status information, making subgroup analysis impossible. However, the insights gained from this study lay the groundwork for subsequent prospective randomized trials. By highlighting the safety profile and potential efficacy of CIRT, either alone or as a Photon + CIRTboost, our research identifies key questions and considerations for future investigations. Thirdly, the recent surge in the popularity of such non-linear models highlights their potential advantages over traditional Cox proportional hazards regression in oncology research. For example, ensemble learning methods might capture complex interactions and nonlinear relationships in the data, potentially leading to improved predictive performance compared to standard parametric or semiparametric survival models [20]. Bayesian additive regression trees (BART) and soft BART have demonstrated promising results in various survival analysis settings, including clustered and interval-censored data [3, 17]. Additionally, the incorporation of grouping information, as described in the work by Du and Linero [8], can be particularly relevant for our study, where we stratified the analysis by patient characteristics like gender and IDH mutation status. Such group-based ensemble approaches may provide additional insights into the heterogeneous treatment effects observed in our cohort in the future.
Conclusion
CIRT alone and Photon + CIRTboost with concurrent temozolomide are safe, without significant differences in PFS and OS in HGG patients. In grade 4 HGG received Photon + CIRTboost, the 12- and 18-month PFS rates were 66.7% (95%CI, 27.2%-88.1%) and 50.0% (95%CI, 13.4%-78.7%), while the 12- and 18-month OS rates were 87.5% (95%CI, 38.7%-98.1%) and 72.9% (95%CI, 27.6%-92.5%), which is comparable to the dose-intensification group in the NRG Oncology BN001 phase II study. It is meaningful to explore whether dose escalation of CIRTboost might improve survival outcomes of HGG patients in future randomized trials.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Al Feghali KA, Randall JW, Liu DD, Wefel JS, Brown PD, Grosshans DR, McAvoy SA, Farhat MA, Li J, McGovern SL, McAleer MF, Ghia AJ, Paulino AC, Sulman EP, Penas-Prado M, Wang J, De Groot J, Heimberger AB, Armstrong TS, Gilbert MR, Mahajan A, Guha-Thakurta N, Chung C. Phase II trial of proton therapy versus photon IMRT for GBM: secondary analysis comparison of progression-free survival between RANO versus clinical assessment. Neurooncol Adv. 2021;3:vdab073.
Ali AN, Zhang P, Yung WKA, Chen Y, Movsas B, Urtasun RC, Jones CU, Choi KN, Michalski JM, Fischbach AJ, Markoe AM, Schultz CJ, Penas-Prado M, Garg MK, Hartford AC, Kim HE, Won M, Curran WJ, JR. NRG oncology RTOG 9006: a phase III randomized trial of hyperfractionated radiotherapy (RT) and BCNU versus standard RT and BCNU for malignant glioma patients. J Neurooncol. 2018;137:39–47.
Basak P, Linero A, Sinha D, Lipsitz S. Semiparametric analysis of clustered interval-censored survival data using soft Bayesian additive regression trees (SBART). Biometrics. 2022;78:880–93.
Brown A, Suit H. The centenary of the discovery of the Bragg peak. Radiother Oncol. 2004;73:265–8.
Brown PD, Chung C, Liu DD, Mcavoy S, Grosshans D, Al Feghali K, Mahajan A, Li J, Mcgovern SL, Mcaleer MF, Ghia AJ, Sulman EP, Penas-Prado M, De Groot JF, Heimberger AB, Wang J, Armstrong TS, Gilbert MR, Guha-Thakurta N, Wefel JS. A prospective phase II randomized trial of proton radiotherapy vs intensity-modulated radiotherapy for patients with newly diagnosed glioblastoma. Neuro Oncol. 2021;23:1337–47.
Dr COX. Regression Models and Life-Tables. J Royal Stat Soc Series B (Methodological). 1972;34:187–202.
Dong X, Noorbakhsh A, Hirshman BR, Zhou T, Tang JA, Chang DC, Carter BS, Chen CC. Survival trends of grade I, II, and III astrocytoma patients and associated clinical practice patterns between 1999 and 2010: A SEER-based analysis. Neurooncol Pract. 2016;3:29–38.
Du J, Linero A. Incorporating Grouping Information into Bayesian Decision Tree Ensembles. In: Kamalika C, Ruslan S, editors. Proceedings of the 36th International Conference on Machine Learning. Alexandria: Proceedings of Machine Learning Research: PMLR; 2019.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Gondi V, Pugh S, Tsien C, Chenevert T, Gilbert M, Omuro A, McDonough J, Aldape K, Srinivasan A, Rogers CL, Shi W, Suh JH, Algan O, Nedzi LA, Chan MD, Bahary JP, Mehta MP. Radiotherapy (RT) Dose-intensification (DI) Using Intensity-modulated RT (IMRT) versus Standard-dose (SD) RT with Temozolomide (TMZ) in Newly Diagnosed Glioblastoma (GBM): Preliminary Results of NRG Oncology BN001. Int J Radiat Oncol Biol Phys. 2020;108:S22–3.
Hasegawa A, Mizoe JE, Tsujii H, Kamada T, Jingu K, Iwadate Y, Nakazato Y, Matsutani M, Takakura K, Organizing committee of the central nervous system tumor working G. Experience with carbon ion radiotherapy for WHO Grade 2 diffuse astrocytomas. Int J Radiat Oncol Biol Phys. 2012;83:100–6.
Horbinski C, Nabors LB, Portnow J, Baehring J, Bhatia A, Bloch O, Brem S, Butowski N, Cannon DM, Chao S, Chheda MG, Fabiano AJ, Forsyth P, Gigilio P, Hattangadi-Gluth J, Holdhoff M, Junck L, Kaley T, Merrell R, Mrugala MM, Nagpal S, Nedzi LA, Nevel K, Nghiemphu PL, Parney I, Patel TR, Peters K, Puduvalli VK, Rockhill J, Rusthoven C, Shonka N, Swinnen LJ, Weiss S, Wen PY, Willmarth NE, Bergman MA, Darlow S. NCCN Guidelines(R) Insights: Central Nervous System Cancers, Version 2.2022. J Natl Compr Canc Netw. 2023;21:12–20.
Kong L, Wu J, Gao J, Qiu X, Yang J, Hu J, Hu W, Mao Y, Lu JJ. Particle radiation therapy in the management of malignant glioma: Early experience at the Shanghai Proton and Heavy Ion Center. Cancer. 2020;126:2802–10.
Koshy M, Villano JL, Dolecek TA, Howard A, Mahmood U, Chmura SJ, Weichselbaum RR, McCarthy BJ. Improved survival time trends for glioblastoma using the SEER 17 population-based registries. J Neurooncol. 2012;107:207–12.
Kotecha R, Odia Y, Khosla AA, Ahluwalia MS. Key clinical principles in the management of glioblastoma. JCO Oncol Pract. 2023;19:180–9.
Laperriere NJ, Leung PM, McKenzie S, Milosevic M, Wong S, Glen J, Pintilie M, Bernstein M. Randomized study of brachytherapy in the initial management of patients with malignant astrocytoma. Int J Radiat Oncol Biol Phys. 1998;41:1005–11.
Linero AR, Basak P, Li Y, Sinha D. Bayesian Survival Tree Ensembles with Submodel Shrinkage. Bayesian Anal. 2022;17(997–1020):24.
Malouff TD, Peterson JL, Mahajan A, Trifiletti DM. Carbon ion radiotherapy in the treatment of gliomas: a review. J Neurooncol. 2019;145:191–9.
Mizoe JE, Tsujii H, Hasegawa A, Yanagi T, Takagi R, Kamada T, Tsuji H, Takakura K, Organizing committee of the central nervous system tumor working G. Phase I/II clinical trial of carbon ion radiotherapy for malignant gliomas: combined X-ray radiotherapy, chemotherapy, and carbon ion radiotherapy. Int J Radiat Oncol Biol Phys. 2007;69:390–6.
Safiyari A & Javidan R. Predicting lung cancer survivability using ensemble learning methods. 2017 Intelligent Systems Conference (IntelliSys); 2017. pp 684-688
Segura PP, Quintela NV, Garcia MM, Del Barco Berron S, Sarrio RG, Gomez JG, Castano AG, Martin LMN, Rubio OG, Losada EP. SEOM-GEINO clinical guidelines for high-grade gliomas of adulthood (2022). Clin Transl Oncol. 2023;25:2634–46.
Souhami L, Seiferheld W, Brachman D, Podgorsak EB, Werner-Wasik M, Lustig R, Schultz CJ, Sause W, Okunieff P, Buckner J, Zamorano L, Mehta MP, Curran WJJR. Randomized comparison of stereotactic radiosurgery followed by conventional radiotherapy with carmustine to conventional radiotherapy with carmustine for patients with glioblastoma multiforme: report of Radiation Therapy Oncology Group 93–05 protocol. Int J Radiat Oncol Biol Phys. 2004;60:853–60.
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B, Belanger K, Hau P, Brandes AA, Gijtenbeek J, Marosi C, Vecht CJ, Mokhtari K, Wesseling P, Villa S, Eisenhauer E, Gorlia T, Weller M, Lacombe D, Cairncross JG, Mirimanoff RO, European organisation for R, Treatment of cancer brain T, Radiation oncology G & National cancer institute of canada clinical trials G. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10:459–66.
Tabrizi S, Yeap BY, Sherman JC, Nachtigall LB, Colvin MK, Dworkin M, Fullerton BC, Daartz J, Royce TJ, Oh KS, Batchelor TT, Curry WT, Loeffler JS, Shih HA. Long-term outcomes and late adverse effects of a prospective study on proton radiotherapy for patients with low-grade glioma. Radiother Oncol. 2019;137:95–101.
Tsien CI, Brown D, Normolle D, Schipper M, Piert M, Junck L, Heth J, Gomez-Hassan D, ten Haken RK, Chenevert T, Cao Y, Lawrence T. Concurrent temozolomide and dose-escalated intensity-modulated radiation therapy in newly diagnosed glioblastoma. Clin Cancer Res. 2012;18:273–9.
Vordermark D, Kolbl O. Lack of survival benefit after stereotactic radiosurgery boost for glioblastoma multiforme: randomized comparison of stereotactic radiosurgery followed by conventional radiotherapy with carmustine to conventional radiotherapy with carmustine for patients with glioblastoma multiforme: report of radiation therapy oncology group 93-05 protocol: in regard to Souhami et al. (Int J Radiat Oncol Biol Phys 2004;60:853-860). Int J Radiat Oncol Biol Phys. 2005;62:296–7.
Walker MD, Strike TA, Sheline GE. An analysis of dose-effect relationship in the radiotherapy of malignant gliomas. Int J Radiat Oncol Biol Phys. 1979;5:1725–31.
Wang Y, Liu R, Zhang Q, Dong M, Wang D, Chen J, Ou Y, Luo H, Yang K, Wang X. Charged particle therapy for high-grade gliomas in adults: a systematic review. Radiat Oncol. 2023;18:29.
Acknowledgements
Not applicable.
Funding
This study was supported by The Longyuan Young Talents Project in Gansu Province, China, and National Clinical Key Specialty Construction Project of Tumor Radiotherapy Department, Wuwei Cancer Hospital, Gansu Province, China. The funding organization(s) plays no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the report for publication.
Author information
Authors and Affiliations
Contributions
XiaoJun Li, YanShan Zhang, and YanCheng Ye conceptualized and designed the study. XiaoJun Li and YanShan Zhang were involved in data collection and performed the data analysis. YanShan Zhang also contributed to the interpretation of data. YanCheng Ye provided overall leadership and was responsible for the project administration and securing the funding. Suqing Tian contributed to the methodology and validated the analytical methods. TingChao Hu, HongYu Chai and Faxin Wen assisted in data collection and were involved in the initial drafting of the manuscript. TianE Zhang provided critical revisions that were important for the intellectual content of the manuscript. All authors contributed to the manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of Wuwei Cancer Hospital&Institute, China (Approval no. 2022-ethicalcheck-16). Informed consent was obtained from all patients included.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12885_2024_12606_MOESM1_ESM.docx
Additional file 1: Supplementary Table 1. Univariate analysis for PFS in all HGG cases. Supplementary Table 2. Univariate analysis for OS in all HGG cases. Supplementary Table 3. Univariate analysis for PFS in grade 4 HGG cases. Supplementary Table 4. Univariate analysis for OS in grade 4 HGG cases.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, X., Zhang, Y., Ye, Y. et al. Carbon-ion radiotherapy alone vs. standard dose photon radiation with carbon-ion radiotherapy boost for high-grade gliomas: a retrospective study. BMC Cancer 24, 837 (2024). https://doi.org/10.1186/s12885-024-12606-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12606-x