Abstract
Background
To explore the correlation between effective dose to immune cells (EDIC) and vertebral bone marrow dose and hematologic toxicity (HT) for esophageal squamous cell carcinoma (ESCC) during neoadjuvant chemoradiotherapy (nCRT).
Methods
The study included 106 ESCC patients treated with nCRT. We collected dosimetric parameters, including vertebral body volumes receiving 10–40 Gy (V10, V20, V30, V40) and EDIC and complete blood counts. Associations of the cell nadir and dosimetric parameters were examined by linear and logistic regression analysis. The receiver operating characteristic (ROC) curves were used to determine the cutoff values for the dosimetric parameters.
Results
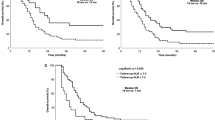
During nCRT, the incidence of grade 3–4 lymphopenia, leukopenia, and neutropenia was 76.4%, 37.3%, and 37.3%, respectively. Patients with EDIC ≤ 4.63 Gy plus V10 ≤ 140.3 ml were strongly associated with lower risk of grade 3–4 lymphopenia (OR, 0.050; P < 0.001), and patients with EDIC ≤ 4.53 Gy plus V10 ≤ 100.9 ml were strongly associated with lower risk of grade 3–4 leukopenia (OR, 0.177; P = 0.011), and patients with EDIC ≤ 5.79 Gy were strongly associated with lower risk of grade 3–4 neutropenia (OR, 0.401; P = 0.031). Kaplan-Meier analysis showed that there was a significant difference among all groups for grade 3–4 lymphopenia, leukopenia, and neutropenia (P < 0.05).
Conclusion
The dose of vertebral bone marrow irradiation and EDIC were significantly correlated with grade 3–4 leukopenia and lymphopenia, and EDIC was significantly correlated with grade 3–4 neutropenia. Reducing vertebral bone marrow irradiation and EDIC effectively reduce the incidence of HT.
Similar content being viewed by others
Introduction
Esophageal squamous cell carcinoma (ESCC) is a common digestive system malignancy worldwide. It is the seventh most common malignancy globally [1, 2]. At present, neoadjuvant chemoradiotherapy (nCRT) is the standard treatment for locally advanced resectable esophageal cancer. The evidence suggests that nCRT plus surgery improves overall survival compared with surgery alone among patients with locally advanced ESCC [3, 4]. However, severe acute hematological toxicity (HT) often occurs during nCRT and is associated with poor outcomes [5]. The presence of myelosuppression during treatment can also affect the progress of the treatment plan, leading to dose reductions and interruptions of radiotherapy [6]. Several studies have found that increased radiation doses in bone marrow during nCRT are associated with acute HT in a variety of cancer, including esophageal cancer [7,8,9,10]. In addition to the bone marrow, increased radiation doses to the heart, lung, and blood vessels, which were the organs with large blood supplies, may also produce a decrease in peripheral blood leukocytes leading to immunosuppression [11]. The innate and adaptive immune system plays a significant role in the progression of tumor and patient prognosis in cases of solid malignancies. Tumor-associated inflammation, mostly maintained by innate immune cells, promotes tumor growth in various contexts. Inflammatory, regenerative, and anti-inflammatory cytokines are released in response to initial innate activation, which in turn influences how the adaptive immune system reacts to the tumor [12]. Lymphocytes are a crucial part of cell-mediated immunity systems and are highly radiosensitive. They can be destroyed by radiotherapy even at very low radiation doses of < 1 Gy [13]. Jin and colleagues developed a model to estimate effective dose to immune cell (EDIC) to substitute the estimated dose of circulation immune pool, such as the heart, lung, blood vessels, and other organs [14]. Cai et al. found that higher EDIC was correlated with severe radiation induced lymphopenia and poorer clinical outcomes in patients with ESCC [15]. Tseng et al [16] found the lower radiation dose to the spleen and bone marrow plus the lower EDIC reduced the risk of grade 4 lymphopenia during definitive concurrent chemoradiotherapy in ESCC. Neutrophils could promote tumor angiogenesis, invasion, and metastasis to facilitate tumor progression primarily. Meanwhile, neutrophils can establish a bidirectional interaction with platelets, lymphocytes, and other components that can influence cancer outcomes [17, 18]. Accumulating evidence has found that high levels of neutrophils in blood and high neutrophil-to-lymphocyte ratios are associated with a poor prognosis in cancer [19].
Therefore, we developed this study to explore the correlation between EDIC and vertebral marrow dose and HT, which could provide possibilities for optimizing a radiotherapy plan to reduce the incidence of HT.
Materials and methods
Patients and treatment
We identified 106 patients with clinical stage II-IVa ESCC (according to the eighth edition of the American Joint Committee on Cancer staging system) treated at Shandong Cancer Hospital with nCRT between May 2017 and May 2021. The institutional review board approved our study. We included patients if they were pathologically confirmed ESCC, completed nCRT followed by esophagectomy, had at least four available complete blood counts (CBC) records during nCRT weekly, and had available dosimetric parameters. Patients were excluded if they had distant metastatic disease, received a radiation dose less than 40 Gy or more than 50 Gy, had a history of radiotherapy, and had chronic inflammatory or autoimmune disease. Patients were treated with the intensity-modulated radiation therapy (IMRT) technique, most at a prescription dose of 41.4 Gy in 23 daily fractions, and a few at 40 Gy in 20 daily fractions or 45 Gy in 25 daily fractions, and concurrent or sequential cisplatin/taxane (TP) chemotherapy regimen (weekly paclitaxel 50 mg/m2 or docetaxel 30 mg/m2 and cisplatin 25 mg/m2 or triweekly paclitaxel 175mg/m2 or docetaxel 75 mg/m2 and cisplatin 75 mg/m2) or cisplatin/fluorouracil (PF) chemotherapy regimen (triweekly fluorouracil 1000mg/m2 and cisplatin 75 mg/m2). And patients who received induction chemotherapy did not have normal CBC at the start of nCRT and developed grade ≥ 2 HT according to the Common Terminology Criteria for Adverse Events (CTCAE) version 5.0 during the induction chemotherapy were excluded. Esophagectomy was performed within 4 to 8 weeks after the completion of nCRT.
Data collection
We retrospectively contoured the vertebral body bone marrow on radiation therapy (RT) planning CT scans, whose superior and inferior borders depend on the isodose line of PTV. The vertebral body volumes (ml) receiving 10–40 Gy (V10, V20, V30, V40) were recorded from the dose volume histogram (DVH) from Eclipse treatment planning systems. And the following parameters were also collected: RT technique, radiation dose, gross tumor volume (GTV), mean heart dose (MHD), mean lung dose (MLD), mean liver dose (MlD), mean body dose (MBD), and integral total dose volume (ITDV). In addition, some clinical factors were also collected, including age, gender, smoking history, alcohol history, tumor location, clinical stage, and CBC, including white blood cell count (WBC), neutrophil count (NEU), absolute lymphocyte count (ALC), platelet count (PLT), and hemoglobin (HGB) before and during (weekly) nCRT. The cell nadir was defined as the lowest cell count during nCRT. HT were graded according to the CTCAE version 5.0.
EDIC calculation
The EDIC model which was constructed by Jin et al [14] was assumed that radiation dose was uniformly delivered to all cells for rapidly circulating ones, including the heart, lung, and blood vessels, and only to those in the irradiated volume for slowly circulating ones, like the lymphatic system and blood reservoirs (a portion of veins/capillaries). The equivalent uniform dose (EUD) to the total blood was calculated from the differential DVH that were computed using a similar model reported by Yovino S et al [20]. The EDIC was considered the sum of EUDs of organs that are irradiated in esophageal nCRT, mainly including lung, heart, liver, large vessels, and small vessels and capillaries in other organs. (estimated percentage of cardiac output: 12%, 8%, 15%, 45%, and 35%, respectively) [21]. The EUD of lung, heart, and large vessels was calculated as the percentage of cardiac output multiply mean organ dose (MOD). Integral total body dose can be used to replace the MOD for the large vessels and small vessels and capillaries in other organs, and 0.85 is a dose effectiveness factor for liver, small vessels, and capillaries. Therefore, the EDIC was calculated as follows [21]:
Since the percentage of large and small vessels were for the entire body, and CT images did not include the entire body. Therefore, we used the Vscan/61.8 × 103 factor to adjust the percentage of large and small vessels, which was achieved by assuming that each patient weighed 140 ponds, or 63 kg, or had a volume of 61.8 × 103 CC [21].
Statistical analysis
We used univariate linear regression analysis to examine the correlation between the dosimetry parameters along with clinicopathologic features and cell nadir. When multiple one marrow dosimetric parameters showed significance on univariate, we incorporated the variable with the lowest univariate p-value for multivariate analysis. We used Benjamini-Hochberg false discovery rate (FDR) correction for multiple hypothesis testing. Adjusted P values are denoted as Q values. To avoid multicollinearity, we used receiver operating characteristic curve (ROC) to transform the dosimetry parameters into binomial variables with the endpoint being the occurrence of grade 3 cell toxicity. Based on the cutoff values of the dosimetry parameters, patients were divided into subgroups, including the “all lower” group (patients who received EDIC and vertebral body volumes ≤ their corresponding best cutoffs), the “all higher” group (patients who received EDIC and vertebral body volumes > their corresponding best cutoffs), and the remaining patients were included in the “others” group. We used the Kaplan-Meier method to analyze the comparison of the cumulative incidence of cell toxicity between the dosimetry subgroups. All analyses were performed using SPSS (Version 26.0, IBM) and GraphPad Prism 8.0 software. Significance was defined as variables with a two-sided P value < 0.05.
Results
Patients characteristics
There were 106 patients incorporated in this study with a median age of 61 years (ranging from 48 to 73). Most patients were male (84.9%), with stage II-IVa disease (74.5%). There were 53 (50.0%) patients with tumors in the distal segment of the esophagus and others in the middle segment of the esophagus and above. Most patients received a radiation dose of 41.4 Gy (83.0%) and were treated with TP (89.0%) chemotherapy regimen. These results are summarized in Table 1.
CBC data
We acquired 106 patients’ CBC data, including WBC, NEU, ALC, HGB, and PLT from baseline until nCRT completion. The details of the CBC data are shown in Fig. 1. WBC, NEU, and ALC declined per week throughout nCRT with the rapid declines in the first two weeks, and generally reached nadir at week 3–4, and then recovered and continued to stabilize. HGB declined continuously from the beginning untill the end of nCRT. PLT steadily declined per week and reached nadir at week 3–4, and then quickly recovered.Meanwhile, the cell counts for week 1–5 during nCRT were as follows. For WBC, the median of baseline was 6.43 × 109/L, and it declined to 5.55, 4.10, 3.49, 3.59, and 3.54 × 109/L, respectively. For NEU, the median of baseline was 4.12 × 109/L, and it declined to 3.89, 2.94, 2.56, 2.54, and 2.58 × 109/L, respectively. For ALC, the median of baseline was 1.54 × 109/L, and it declined to 1.07, 0.70, 0.51, 0.42, and 0.46 × 109/L, respectively. For HGB, the median of baseline was 144 g/L, and it declined to 140, 137, 132, 129, and 127 g/L, respectively. For PLT, the median of baseline was 249.5 × 109/L, and it declined to 210, 178, 146, 143, and 168 × 109/L, respectively. During CRT, 81 (76.4%) developed at grade 3–4 lymphopenia, 40 patients (37.3%) developed grade 3–4 leukopenia, 40 patients (37.3%) developed grade 3–4 neutropenia, only 1 patients (0.94%) developed grade 3–4 anaemia, and no patients developed grade 3–4 thrombocytopenia.
Dosimetric parameters associated with HT
We performed univariate linear regression analysis to identify associations between clinicopathologic features of age, sex, smoking history, alcohol history, tumor location, GTV, clinical stage, chemotherapy regimen, and dosimetric parameters with cell count nadirs. These results are displayed in Table 2. For WBC, EDIC (P < 0.004), V10 (P < 0.008), V20 (P < 0.015), and age (P < 0.041) were associated with leukopenia. For NEU, EDIC (P < 0.022) and chemotherapy regimen (P = 0.040) were associated with neutropenia. For ALC, EDIC (P < 0.001), V10 (P < 0.001), V20 (P < 0.001), V30 (P < 0.001), V40 (P < 0.001), and tumor location (P = 0.037) were associated with lymphopenia. ROC curves were then made for the significient dosimetry parameters with the endpoint of grade 3 HT to obtain the cutoff values (Fig. 2). For ALC, EDIC < 4.63 Gy plus V10 < 140.3 ml went into “all lower” group, and EDIC ≥ 4.63 Gy plus V10 ≥ 140.3 ml went into “all higher” group, and remaining went into “others” group; for WBC, EDIC < 4.53 Gy plus V10 < 100.9 ml went into “all lower” group, and EDIC ≥ 4.53 Gy plus V10 ≥ 100.9 ml went into “all higher” group, and remaining went into “others” group; for NEU, EDIC < 5.79 Gy went into “lower” group, and EDIC ≥ 5.79 Gy went into “higher” group. Based on the multivariable analysis, “all lower” group in ALC (vs. “all higher” group; OR, 0.050; 95% CI, 0.010–0.251; P < 0.001), “all lower” group in WBC (vs. “all higher” group; OR, 0.177; 95% CI, 0.047–0.688; P = 0.011) and “lower” group in NEU (vs. “higher” group; OR, 0.401; 95% CI, 0.175–0.922; P = 0.031) were positively significant factors correlated with grade 3–4 cell toxicity during nCRT. And these associations were still significant after FDR adjustment. These results are shown in Table 3.
ROC curves for the dosimetry parameters with the endpoint of grade 3–4 cell toxicity. ROC curves for EDIC (a) and V10 (b) with the endpoint of grade 3–4 lymphopenia; ROC curves for EDIC (c) and V10 (d) with the endpoint of grade 3–4 leukopenia; ROC curves for EDIC (e) with the endpoint of grade 3–4 neutropenia. ROC receiver operating characteristic; EDIC effective dose to immune cells
Kaplan-Meier analysis for HT between dosimetry subgroups
The Kaplan-Meier analysis showed that there was a significant difference between the three groups for grade 3–4 lymphopenia, leukopenia, and neutropenia, and all the P-values were < 0.001. The results are showen in Fig. 3.
Discussion
In this study, we found that increasing vertebral body bone marrow radiation dose and EDIC were associated with the development of acute grade 3–4 HT in esophageal cancer patients treated with nCRT.
The relationships between vertebral body bone marrow radiation dosimetric parameters and HT in patients with ESCC during CRT has received increasing attention in recent years. Fabian [7] found in a study of patients with ESCC receiving CRT that increasing thoracic marrow radiation dose was associated with grade ≥ 3 HT. Liu et al [22] found in a study of 99 patients of thoracic oesophageal cancer treated with radical radiotherapy that the mean dose of the thoracic vertebrae and thoracic vertebrae V20 were associated with lymphocytopenia. Lee [23] analyzed 41 patients with esophageal cancer treated with nCRT and found that greater thoracic vertebrae dose such as thoracic vertebrae V10 and V20, were associated with increased grade ≥ 3 leukopenia risk. In addition to the effects of bone marrow irradiation dose, attention has been focused on the relationship between irradiation of the large number of vascular structures and blood pool in the thoracic cavity and hematological toxicity in recent years. Anderson [24] collected 46 patients with ESCC undergoing CRT and conducted multiple logistic regression analysis on the potential predictors of HT, finding that mean cardiopulmonary dose was associated with lower WBC and NEU nadirs (p < 0.05) and grade 4 lymphopenia was significantly associated with thoracic vertebral V10 and V20 (all p < 0.05). However, there may be some limitations to their use of the mean cardiopulmonary dose substitute for the peripheral hematological peripheral hematological dose, such as not taking into account the dose delivery and cardiovascular dynamics. Jin et al [14] further developed a model to estimate the EDIC, which is a surrogate for the estimated dose to the circulation immune pool, and discovered that greater EDIC was associated with a worse prognosis for patients with lung cancer in the Radiation Therapy Oncology Group (RTOG) 0617 trial. Higher EDIC (> 4.0 Gy) was also found to be strongly associated with severe lymphopenia in esophageal cancer patients treated with neoadjuvant or definitive concurrent chemoradiotherapy [15]. Tseng [16] analyzed the grade 4 lymphopenia in patients in the ESO-Shanghai 1 and ESO-Shanghai 2 trials and found that in ESCC patients who received definitive concurrent chemoradiotherapy, when the EDIC ≤ 8.3 Gy plus spleen V0.5 ≤ 11.1% and bone marrow V10 ≤ 33.2%, the incidence of grade 4 lymphopenia decreased. In our study, we reached some similar and some dissimilar conclusions as well.
In our study, we found that WBC, NEU, ALC, and PLT nadirs occurred at the 3–4 week of nCRT and then recovered, while HGB demonstrated a continuous decline throughout and ALC declined rapidly during nCRT, which is a reflection of cell‘s variation in intrinsic radiosensitivity and lymphocyte’s high radiosensitivity. And these results were simillar with a previous report by Anderson [24] et al. In analyzing the relationship between dosimetric parameters and HT, we combined EDIC and bone marrow dosimetric parameters into a single variable to eliminate the influence of possible multicollinearity between dosimetric parameters. This was supported by Tseng et al [16], where the authors demonstrated that smaller irradiations of the spleen and bone marrow and smaller EDIC reduced the risk of grade 4 lymphopenia, which echoes our finding. We found that increasing irradiation doses to thoracic bone marrow plus higher EDIC was associated with a risk of grade 3–4 lymphopenia and leukopenia, and higher EDIC was associated with a risk of grade 3–4 neutropenia, but not anaemia or thrombocytopenia. We found that increasing the irradiation dose to the bone marrow of the vertebral body was not associated with neutropenia, which may be due to the different radiosensitivity of neutrophils in the peripheral circulation and bone marrow. Berkow et al [25] found that morphologically mature neutrophils in the bone marrow exhibited reduced phagocytosis, slow stimulated superoxide anion production, reduced NADPH oxidase activity, and reduced AP activity compared to peripheral circulating neutrophils, which remained functionally immature. Kaplan-Meier analysis showed that the “all lower” group, which both had lower bone marrow irradiation dose and lower EDIC, had a lower incidence of grade 3–4 lymphopenia and leukopenia compared to the other two groups, and “lower group”, which had lower EDIC, had a lower incidence of grade 3–4 lymphopenia and neutropenia compared to the “higher” group. The results of the study suggest that adjusting the radiotherapy plans to reduce the irradiation of organs such as the vertebral bone marrow and the heart, lungs, and large blood vessels could reduce the risk of hematological toxicity, which may benefit the treatment of the tumor.
There are several limitations in our study. Our study is subject to a retrospective nature and may not be able to consider all potential factors, requiring further validation with prospective data. And we did not include the spleen in the analysis because the patients in our study all received very small incidental spleen irradiation or even none. It was found that even when patients with distal esophageal cancer received radiotherapy, not all patients received significant incidental radiation doses [26]. Further efforts should be made to improve it by taking these other organs into account in future studies.
Conclusion
During neoadjuvant radiotherapy for ESCC, the dose of vertebral bone marrow irradiation and EDIC were significantly correlated with G3-4 leukopenia and lymphopenia, and EDIC was again significantly correlated with G3-4 neutropenia. The reduction of vertebral bone marrow irradiation and EDIC was effective in reducing the incidence of hematological toxicity.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALC:
-
Absolute lymphocyte count
- CBC:
-
Complete blood counts
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- DVH:
-
Dose volume histogram
- EDIC:
-
Effective dose to immune cells
- ESCC:
-
Esophageal squamous cell carcinoma
- EUD:
-
Equivalent uniform dose
- GTV:
-
Gross tumor volume
- HGB:
-
Hemoglobin
- HT:
-
Hematologic toxicity
- IMRT:
-
Intensity-modulated radiation therapy
- ITD:
-
Integral total dose
- MBD:
-
Mean body dose
- MHD:
-
Mean heart dose
- MlD:
-
Mean liver dose
- MLD:
-
Mean lung dose
- MOD:
-
Multiply mean organ dose
- nCRT:
-
Neoadjuvant chemoradiotherapy
- NEU:
-
Neutrophil count
- PF:
-
Cisplatin/fluorouracil
- PLT:
-
Platelet count
- ROC:
-
Receiver operating characteristic
- RT:
-
Radiation therapy
- TP:
-
Cisplatin/taxane
- WBC:
-
White blood cell count
References
Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33.
Sung H, Ferlay J, Siegel RL, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 Countries[J]. CA Cancer J Clin. 2021;71(3):209–49.
Shapiro J, Van Lanschot JJB, Hulshof M, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial[J]. Lancet Oncol. 2015;16(9):1090–8.
Yang H, Liu H, Chen Y, AME Thoracic Surgery Collaborative Group, et al. Neoadjuvant Chemoradiotherapy followed by surgery versus surgery alone for locally advanced squamous cell carcinoma of the Esophagus (NEOCRTEC5010): a phase III Multicenter, Randomized, open-label clinical trial. J Clin Oncol. 2018;36(27):2796–803.
Damen PJJ, Kroese TE, van Hillegersberg R, et al. The influence of severe Radiation-Induced Lymphopenia on overall survival in solid tumors: a systematic review and Meta-analysis. Int J Radiat Oncol Biol Phys. 2021;111(4):936–48.
Ai D, Ye J, Wei S, et al. Comparison of 3 paclitaxel-based chemoradiotherapy regimens for patients with locally advanced esophageal squamous cell Cancer: a Randomized Clinical Trial. JAMA Netw Open. 2022;5(2):e220120.
Fabian D, Ayan A, DiCostanzo D, et al. Increasing Radiation Dose to the thoracic marrow is Associated with Acute Hematologic toxicities in patients receiving chemoradiation for Esophageal Cancer. Front Oncol. 2019;9:147.
Barney CL, Scoville N, Allan E, et al. Radiation Dose to the thoracic vertebral bodies is Associated with Acute Hematologic toxicities in patients receiving concurrent chemoradiation for Lung Cancer: results of a single-Center Retrospective Analysis. Int J Radiat Oncol Biol Phys. 2018;100(3):748–55.
Lee AY, Golden DW, Bazan JG, et al. Hematologic nadirs during Chemoradiation for Anal Cancer: temporal characterization and dosimetric predictors. Int J Radiat Oncol Biol Phys. 2017;97(2):306–12.
Zhou P, Zhang Y, Luo S, et al. Pelvic bone marrow sparing radiotherapy for cervical cancer: a systematic review and meta-analysis. Radiother Oncol. 2021;165:103–18.
Thor M, Montovano M, Hotca A. Are unsatisfactory outcomes after concurrent chemoradiotherapy for locally advanced non-small cell lung cancer due to treatment-related immunosuppression? Radiother Oncol. 2020;143:51–7.
Shalapour S, Karin M. Pas de deux: control of anti-tumor immunity by Cancer-Associated inflammation. Immunity. 2019;51(1):15–26.
Sellins KS, Cohen JJ. Gene induction by Gamma-Irradiation leads to DNA fragmentation in lymphocytes. J Immunol. 1987;139(10):3199–206.
Jin JY, Hu C, Xiao Y, et al. Higher radiation dose to immune system is correlated with poorer survival in patients with stage III nonesmall cell lung cancer: a secondary study of a phase 3 cooperative group trial (NRG oncology RTOG 0617). Int J Radiat Oncol Biol Phys. 2017;99:S151–152.
Xu C, Jin JY, Zhang M, et al. The impact of the effective dose to immune cells on lymphopenia and survival of esophageal cancer after chemoradiotherapy. Radiother Oncol. 2020;146:180–6.
Tseng I, Li F, Ai D, et al. Less irradiation to lymphocyte-related organs reduced the risk of G4 Lymphopenia in Esophageal Cancer: re-analysis of prospective trials. Oncologist. 2023;28(8):e645–52.
Segal BH, Giridharan T, Suzuki S, et al. Neutrophil interactions with T cells, platelets, endothelial cells, and of course tumor cells. Immunol Rev. 2023;314(1):13–35.
Scapini P, Cassatella MA. Social networking of human neutrophils within the immune system. Blood. 2014;124(5):710–9.
Maiorino L, Daßler-Plenker J, Sun L, et al. Innate immunity and Cancer pathophysiology. Annu Rev Pathol. 2022;17:425–57.
Yovino S, Kleinberg L, Grossman SA, et al. The etiology of treatment-related lymphopenia in patients with malignant gliomas: modeling radiation dose to circulating lymphocytes explains clinical observations and suggests methods of modifying the impact of radiation on immune cells. Cancer Invest. 2013;31:140–4.
Jin JY, Hu C, Xiao Y, et al. Higher Radiation dose to the Immune cells correlates with Worse Tumor Control and Overall Survival in patients with stage III NSCLC: a secondary analysis of RTOG0617. Cancers (Basel). 2021;13(24):6193.
Liu M, Li X, Cheng H, et al. The impact of Lymphopenia and Dosimetric parameters on overall survival of Esophageal Cancer patients treated with definitive Radiotherapy. Cancer Manag Res. 2021;13:2917–24.
Lee J, Lin JB, Sun FJ, et al. Dosimetric predictors of acute haematological toxicity in oesophageal cancer patients treated with neoadjuvant chemoradiotherapy. Br J Radiol. 2016;89(1066):20160350.
Anderson JL, Newman NB, Anderson C, et al. Mean cardiopulmonary dose and vertebral marrow dose differentially predict lineage-specific leukopenia kinetics during radiotherapy for esophageal cancer. Radiother Oncol. 2020;152:169–76.
Berkow RL, Dodson RW. Purification and functional evaluation of mature neutrophils from human bone marrow. Blood. 1986;68(4):853–60.
Ellis R, Cole AJ, O’Hare J, Whitten G, Crowther K, Harrison C. Coincidental splenic irradiation and risk of functional hyposplenism in oesophageal cancer treatment. J Med Imaging Radiat Oncol. 2021;65(7):925–30.
Acknowledgements
None.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 82102173, 82072094, 12275162).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Meng Zhang, and Zhenjiang Li. The first draft of the manuscript was written by Meng Zhang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved was granted by the Institutional Review Board of the Shandong Cancer Hospital and written informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, M., Li, Z. & Yin, Y. Association of effective dose to immune cells and vertebral marrow dose with hematologic toxicity during neoadjuvant chemoradiotherapy in esophageal squamous cell carcinoma. BMC Cancer 24, 779 (2024). https://doi.org/10.1186/s12885-024-12531-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12531-z