Abstract
Background
CCRT is presently the standard treatment for LA-NSCLC. RP is one of the main obstacles to the completion of thoracic radiation therapy, resulting in limited survival benefits in NSCLC patients. This research aims to explore the role of Endostar in the occurrence of grade≥2 RP and clinical curative effect in LA-NSCLC patients.
Methods
This study retrospectively analyzed 122 patients with stage III NSCLC who received CCRT from December 2008 to December 2017, or Endostar intravenous drip concurrently with chemoradiotherapy (Endostar + CCRT group). Standard toxicity of the pneumonitis endpoint was also collected by CTCAE V5.0. We further summarized other available studies on the role of Endostar in the prognosis of NSCLC patients and the incidence of RP.
Results
There were 76 cases in the CCRT group and 46 cases in the CCRT+ Endostar group. In the CCRT+ Endostar group, the occurrence of grade ≥2 RP in patients with V20Gy ≥25% was significantly higher than that in patients with V20Gy < 25% (p = 0.001). In the cohorts with V20Gy < 25%, 0 cases of 29 patients treated with Endostar developed grade ≥2 RP was lower than in the CCRT group (p = 0.026). The re-analysis of data from other available studies indicated that Endostar plus CCRT could be more efficient and safely in the occurrence of grade≥2 RP with LA-NSCLC.
Conclusions
When receiving CCRT for LA-NSCLC patients, simultaneous combination of Endostar is recommended to enhance clinical benefit and reduce pulmonary toxicity.
Similar content being viewed by others
Background
Lung cancer is the most common disease in terms of incidence and the leading cause of cancer death worldwide [1]. Over two-thirds of all cases of lung cancer are non-small cell lung cancer (NSCLC) [2], approximately one-third of which present locally advanced-stage disease at the time of initial diagnosis. Platinum-based chemotherapy plus concurrent radiotherapy is a standard treatment for patients with locally advanced non-small cell lung cancer (LA-NSCLC). A number of studies have shown that radiotherapy with vinorelbine combined with platinum has good efficacy. With these results, concurrent chemoradiotherapy with cisplatin and vinorelbine could be considered one of the new standard regimens for LA-NSCLC, although the employed vinorelbine doses in each phase II study were 12.5 mg/m2 and 15 mg/m2 [3,4,5]. Concurrent chemoradiotherapy (CCRT) followed by immunotherapy consolidation (CIT) can further improve the prognosis for LA-NSCLC patients [6]. However, radiotherapy-associated acute toxicities, especially radiation pneumonitis (RP), restrict the application of CIT after CCRT in patients with stage III unresectable NSCLC [7]. Endostatin is another broad-spectrum angiogenesis inhibitor widely used in antitumor treatment. A phase II trial HELPER study confirmed the synergistic interaction of Endostar and CCRT for patients with unresectable stage III NSCLC, and the incidences of grade 1, grade 2, and grade 3 RP were 10.4%, 7.5%, and 3.0%, respectively [8]. In addition, our previous study found that stage III lung squamous cell cancer (LSCC) patients with serum Lp (a) levels above 218 mg/L who received Endostar combined with concomitant chemoradiotherapy had longer progression-free survival (PFS) and overall survival (OS) [9]. A pooled analysis suggested that endostatin and CCRT combined to treat LA-NSCLC is effective and well-tolerated, and fewer toxicities including any grade and grade≥3 radiation pneumonitis occur [10]. Moreover, recombinant human endostatin (Rh-endostatin, or Endostar) was also identified to enhance radiosensitivity and reduce radiation-related pulmonary events in patients with advanced NSCLC [11]. Endostar was approved to apply in combination with CCRT to treat patients with unresectable stage III NSCLC in 2005 by the Chinese Food and Drug Administration.
The results from murine xenograft lung tumors showed that an anti-angiogenic drug axitinib in combination with radiotherapy could significantly decrease pneumonitis, vascular damage, and fibrosis in lung tissues [12]. Although Endostar in combination with CCRT is effective and well-tolerated, there is a lack of knowledge on whether Endostar can decrease the incidence of RP in patients more than CCRT patients treated without Endostar. Moreover, bilateral lungs receiving 20Gy(V20Gy) were an important dosimetric predictor of pneumonitis for LA-NSCLC patients treated with CCRT followed by CIT [13]. V20Gy in particular was the only factor associated with grade 2 or greater RP in lung cancer patients with NSCLC who were treated with CCRT [14]. Further, on the basis of a preliminary curative effect study [9], this study intended to explore the difference in the occurrence of grade ≥2 RP in LA-NSCLC patients treated with CCRT with or without Endostar, and the difference in LA-NSCLC patients with different V20Gy.
Methods
Patients
Lung cancer patients who received CCRT in Taizhou Hospital between December 2008 and December 2017 were continuously enrolled according to the following criteria: a diagnosis of NSCLC established by histology; clinical stage III according to the 8th edition of the TNM staging classification used by the International Union Against Cancer; 0-1 on the Eastern Cooperative Oncology Group's Performance Score (ECOG PS). The exclusion criteria included patients without complete radiotherapy records; patients used other anti-angiogenic drugs or lost imaging materials. The need for written informed consent was waived by the Taizhou hospital of Zhejiang Province ethics committee due to the retrospective nature of the study.
Study design treatments and endpoints
The grouping scheme and comparative analysis were as follows.
Chemotherapy
Vinorelbine Tartrate (Jiangsu Hansoh Pharmaceutical Group Co., LTD., Trade name: Gaenuo, Sinopharm approved H19990278) injection 12.5mg/m2, intravenous infusion once weekly; Carboplatin (Qilu Pharmaceutical Co., LTD., Trade name: Bobei, Sinopharm approved 20020180) injection, the area under the curve (AUC) =2, intravenous infusion once weekly; for a total of 6 cycles.
Radiotherapy
Three-dimensional conformal radiation therapy (3D-CRT) with the radiotherapy prescription of 60 Gy/2.0 Gy/30 fractions to the planning target volume (PTV), once a day, 5 times a week.
Recombinant human endostatin (Endostar): In the CCRT + Endostar group, the administered dose of Endostar (Shandong Simcere-Medgenn Bio-pharmaceutical Co., LTD., trade name: Endostar, Sinopharm approved S20050088) was 7.5 mg/m2/day with 1–14 days of continuous administration. The cycle was repeated every other week for a total of 2 cycles.
Amifostine
Grade 2 or greater RP occurred more frequently after CCRT in NSCLC patients with V20Gy greater than or equal to 25% than in patients with V20Gy less than or equal to 25% [14, 15]. In this study, patients with V20Gy ≥25% were assigned to be treated with amifostine 400 mg hypodermic injection three times per week during CCRT, while patients with V20Gy<25% were treated without amifostine (Dalian Meiluo Pharmaceutical Factory Co., LTD., Trade name: Amifostine, Sinopharm approved H20010403) during CCRT.
The patients were reexamined once a week during chemoradiotherapy, 1 month after chemoradiotherapy, and once every 3 months thereafter. The reexamination included blood routine, blood biochemistry, chest CT, and physical examination. Chest CT was interpreted by a senior radiologist, and the imaging changes were mainly limited to spot shadows, pneumobronchial signs, line shadows, lung consolidation or cellular changes in the illuminated area, and a few patients also had imaging changes outside the radiation area. Eventually, RP was confirmed by 2 radiation oncologists unaware of the patient’s information according to the Common Terminology Criteria for Adverse Events version 5.0 (CTCAE V5.0) [16]. Evaluation of grade ≥2 RP was considered symptomatic RP, which requires medical intervention or limiting instrumental activities of daily living. The primary endpoint was set as the incidence of grade 2 or greater RP.
Statistical consideration
For description, categorical variables are reported as count and percentage. Continuous variables are reported as mean ± standard deviations. The chi-square test and Fisher’s exact test were used for categorical variables. The T test was used for continuous variables. All statistical procedures were performed with SPSS version 23.0 (SPSS Inc., Chicago, IL, USA). P < 0.05 was defined as a statistically significant difference (two-sided).
Results
Patients
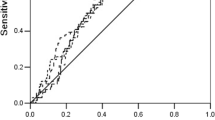
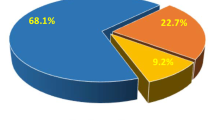
A total of 312 LA-NSCLC patients underwent CCRT from December 2008 to December 2017, of which 122 were enrolled according to the filter criteria (Fig. 1). A total of 46 patients received CCRT combined with Endostar (CCRT + Endostar group), while the others (N = 76) received CCRT alone (CCRT group). Of these, 25 patients (20.5%) developed grade ≥2 RP after treatment, 6 of which received Endostar (13.0%), and 19 of which received non-Endostar (25.0%). There was no significant difference in the patients grouped by baseline clinical factors including age, gender, smoking history, pathology, amifostine, total lung mean lung dose (MLD), clinical stage, or gross target volume (GTV) (Table 1).
Incidence of ≥ grade 2 RP
CCRT-cohorts were grouped by V20Gy≥25% to perform subgroup analysis (Table 2). Of the 19 patients with ≥grade 2 RP, there were 13 patients with V20Gy ≥25% and 6 patients with V20Gy <25%. The incidence of grade ≥2 RP in the patients with V20Gy ≥25% (30.2%) was greater than that in the patients with V20Gy <25% (18.2%), but without significant difference(P=0.229). In the CCRT + Endostar group, 6 (35.3%) of 17 patients with V20Gy ≥25% developed grade ≥2 RP, while 0 (0.0%) of 29 patients with V20Gy <25% developed grade ≥2 RP (P=0.001). Then, patients with V20Gy ≥25% were further grouped by treatment with or without amifostine There were 20 individuals treated without amifostine and 23 patients treated with amifostine in the CCRT group. Of 23 patients treated with amifostine, 3 (13.0%) developed grade ≥2 RP, while 10 (50.0%) of 20 patients treated without amifostine developed grade ≥2 RP (P=0.008). In the cohorts with V20Gy <25%, 6 (18.2%) of 33 patients treated without Endostar developed grade ≥2 RP, while 0 (0.0%) of 29 patients treated with Endostar developed grade ≥2 RP (P=0.026). In the cohorts with V20Gy ≥25%, 3 (13.0%) of 23 patients treated with amifostine alone developed grade ≥2 RP, while only 1 (10.0%) of 10 patients treated with amifostine plus Endostar developed grade ≥2 RP (P>0.05).
Other studies about endostar
The available studies on the role of Endostar in the prognosis and RP incidence of NSCLC patients are summarized in Table 3. These studies contained complete information about follow-up data and radiation pneumonitis incidence [8, 11, 17,18,19,20]. The major objects were patients with unresectable LA-NSCLC. In these studies, a total of 234 evaluable patients received Endostar combined with CCRT and 168 evaluable patients received CCRT. Patients received a total dose of 60–66Gy in 30–33 fractions for 6–7 weeks. In this study, the incidence of grade ≥2 RP was 13% in the Endostar group and 25% in the CCRT group. Compared with other studies on Endostar, the incidence of grade ≥2 RP in this study was similar. The incidence of grade ≥2 RP was on the high side at 40% in the Zhu study, considering the small sample size and some stage IV patients. Endostar addition was confirmed to improve the survival outcomes in LA-NSCLC patients receiving CCRT while presenting a downward trend in the incidence of radiation-related pulmonary events (Fig 2). And previous studies analysis indicates that Endostar combined with CCRT presents a promising treatment modality in treatment of LA-NSCLC. Combination of Endostar and concurrent chemotherapy leads to better response rate, local control rate, and survival, demonstrating superior short- and long-term survival benefits.
Discussion
Radiation-induced lung injury (RILI) is one of the main obstacles to the completion of thoracic radiation therapy, resulting in limited survival benefits in NSCLC patients [21]. The acute injury stage (RP) and the chronic injury stage (radiation pulmonary fibrosis) are the major processes of RILI. Accumulated studies have identified various predictors of RP, such as smoking history, tumor location, age, and dosimetric variables of the lung (V20Gy and MLD) [22,23,24,25,26]. There was no significant difference in the patients grouped by baseline clinical factors including MLD. Because of V20Gy as an imbalanced risk factor and amifostine as the confounding factor in this study, stratified analysis was performed to determine the change in the incidence of grade ≥ 2 RP in different subgroups. Occurrence of grade ≥ 3 RP is the most common event to estimate radiation-induced intolerable toxicity affecting the prognosis of NSCLC patients [22, 23]. Nowadays, ICIs after CCRT are widely recommended for unresectable LA-NSCLC patients [6]. However, RP accounted for the majority of CCRT toxicities precluding the administration of ICIs and consisting mostly of grade 2 RP consisted [7, 27]. Therefore, the incidence of grade 2 or greater RP was set as the primary endpoint in this study. The dosimetric variable of the lung (V20Gy) was a significant risk factor in predicting the incidence of grade ≥ 2 RP [13, 27, 28]. Thus, we investigated the role of Endostar in LA-NSCLC patients grouped by V20Gy in this study. Our results showed that patients with V20Gy≥25% had a higher incidence of grade ≥ 2 RP.
Amifostine, a classical cytoprotective agent, significantly reduced the incidence of grade ≥2 RP in patients with V20Gy≥25%. Endostar not only reduced the incidence of grade ≥2 RP in patients with V20Gy<25% but also further enhanced amifostine-mediated reduction in the incidence of grade ≥2 RP in patients with V20Gy≥25%. Amifostine is used as a cytoprotective drug to protect normal tissue from radiation exposure, and it is preferentially accumulated in normal tissues through active transport [29]. Activated amifostine is quickly produced by vascular endothelial cell alkaline phosphatase in vivo, which converts inactive amifostine to the active free thiol and inorganic phosphate. Normal tissues preferentially take up the free thiol to eliminate irradiation-induced production of oxygen-free radicals, avoiding the damaging hydroperoxide radical-mediated DNA damage and promoting cell death [30]. Previous clinical investigations showed that amifostine may shield healthy tissues from the unexpected toxicity of radiation therapy and chemoradiotherapy without affecting anti-tumor effectiveness [31, 32]. Lung cancer patients treated with radiotherapy or chemoradiotherapy may benefit from amifostine. According to a meta-analysis [33], amifostine significantly decreased the occurrence of acute pulmonary toxicity by 44% compared to treatment without amifostine. The acute pulmonary toxicity caused by CCRT has been demonstrated to be mitigated by amifostine in many investigations [34,35,36]. There were similar results in the present study indicating that amifostine application significantly decreased the incidence of grade ≥2 RP across all subgroup analyses. The extra use of amifostine faces a challenge in economic costs and patient compliance. Amifostine also has side effects such as nausea, vomiting, and hypotension. It is necessary to explore the popular anti-tumor drugs that have an advantage in RP remission.
Endostar, bevacizumab, and anlotinib are the most commonly used anti-angiogenic medications for the anti-tumor treatment of lung cancer patients. Only Endostar has been approved to be applied in combination with radiotherapy or CCRT for LA-NSCLC patients based on its superior safety profile and less harmful side effects. Endostar, a C-terminal fragment naturally derived from type XVIII collagen, performs better simulations of endogenous endostatin in tumor suppression in vivo with fewer side effects than other antiangiogenic drugs. Hypoxia increased macrophage infiltration, transforming growth factor beta (TGF-β) generation, and vascular endothelial growth factor (VEGF) upregulation to form radiation damage [37]. Tanabe et al [38] found that endostatin suppressed peritoneal fibrosis by significantly reducing vascular endothelial growth factor A (VEGF-A), alpha-smooth muscle actin (α-SMA), and the pro-fibrotic factor TGF-β1 in a mouse model. Another investigation revealed that Endostar alleviated radiation-induced pulmonary alveolitis, pulmonary edema, fibrosis, and TGF-β1 release in mice compared to radiation-exposed mice treated without Endostar, suggesting that Endostar can reduce radiation-induced pulmonary lesions [39]. Clinical data also showed that Endostar safely improved the effectiveness of chemoradiotherapy (CRT) in NSCLC [8, 11, 17], and, Endostar might lessen the frequency of acute RILI by suppressing the production of inflammatory markers associated with RILI [39]. In addition, anti-angiogenic medicines can promote the normalization of tumor blood vessels within a specific time window to remodel hypoxia and the immunosuppressive tumor microenvironment [40]. Endostar can regulate metabolism and hypoxia in the tumor microenvironment contributing to synergistically im-proving the anticancer effects of radiotherapy [41]. In this study, patients in the CCRT + Endostar group of the research received treatment every other week, utilizing the effect of antiangiogenic medicines on the "normalization" of tumor blood vessels during the window period of chemoradiotherapy. We found that Endostar effectively reduced the occurrence of grade ≥2 RP in LA-NSCLC patients, which suggested that Endostar may be an effective anti-tumor drug with an advantage in RP remission and can be safely utilized in combination with other anti-tumor treatments.
In addition, Endostar combined with immune checkpoint inhibitors (ICIs) in NSCLC has attracted a great deal of attention in ongoing clinical trials. The completed studies have presented favor results (Table 4) [42,43,44]. The research endpoint, including the objective response rate (ORR), disease control rate (DCR), duration of response (DOR), clinical benefit response rate (CBR), PFS, OS, and adverse events (AEs), saw positive results. Above all, Endostar plus CCRT or ICIs is an effective and safe therapeutic strategy for patients with advanced NSCLC.
Moreover, anti-angiogenesis therapy performed synergistic anti-tumor effects in combination with ICIs [45,46,47]. Numerous clinical trials have verified that patients with advanced NSCLC can benefit from combining ICIs and anti-angiogenic medicines with an acceptable safety profile [48,49,50,51]. Lv et.al [44] proposed that Endostar combined with nivolumab as a second-line or later treatment demonstrated encouraging effectiveness and good tolerability in patients with advanced NSCLC. However, the IMPOWER 150 study [52] found that patients treated with bevacizumab combined with ICIs suffered severe side effects. These findings suggested that Endostar may be a better option in the combination treatment with ICIs and anti-angiogenesis drugs. Similarly, when anti-angiogenic drugs are combined with ICI and thoracic radiotherapy, Endostar is the best choice because it can reduce the incidence of RP and improve the anticancer effects. These findings need further validation by more multi-center double-blind randomized controlled clinical studies.
This study has some shortcomings, as follows: to begin with, it was a retrospective study with an insufficient sample size, and radiotherapy was performed by 3D-CRT treatment, not intensity-modulated radiation therapy (IMRT). IMRT is a popular radiotherapy technology applied in the clinic to enhance accuracy and reduce toxicity. We have no idea whether the advantages of Endostar will be further developed in combination with IMRT. Moreover, Endostar combined with amifostine showed a further tendency of RP reduction in LA-NSCLC patients with V20Gy≥25%. This result needs prospective randomized clinical trials for confirmation. Addtional research is needed to validate the best dosing, frequency, and duration of Endostar in combination with CCRT for the treatment of inoperable LA-NSCLC.
Conclusions
Endostar and amifostine were shown to decrease the incidence of grade ≥ 2 RP in LA-NSCLC patients treated with CCRT. Endostar can improve the clinical benefits of CCRT while it may reduce the incidence of grade ≥2 RP. When receiving CCRT for LA-NSCLC patients, simultaneous combination of Endostar is recommended to enhance clinical benefit and reduce pulmonary toxicity.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CCRT:
-
concurrent chemoradiotherapy
- LA-NSCLC:
-
locally advanced non-small cell lung cancer
- RP:
-
radiation pneumonitis
- NSCLC:
-
non-small cell lung cancer
- CTCAE V5.0:
-
Common Terminology Criteria for Adverse Events version 5.0
- CIT:
-
immunotherapy consolidation
- LSCC:
-
lung squamous cell cancer
- PFS:
-
progression-free survival
- OS:
-
overall survival
- ECOG PS:
-
Eastern Cooperative Oncology Group's Performance Score
- AUC:
-
area under the curve
- 3D-CRT:
-
three-dimensional conformal radiation therapy
- PTV:
-
planning target volume
- MLD:
-
mean lung dose
- GTV:
-
gross target volume
- ICIs:
-
immune checkpoint inhibitors
- ORR:
-
objective response rate
- DCR:
-
disease control rate
- DOR:
-
duration of response
- CBR:
-
clinical benefit response rate
- AEs:
-
Adverse Events
- RILI:
-
radiation-induced lung injury
- TGF-β:
-
transforming growth factor beta
- VEGF:
-
vascular endothelial growth factor
- VEGF-A:
-
vascular endothelial growth factor-A
- α-SMA:
-
alpha-smooth muscle actin
- CRT:
-
chemoradiotherapy
- IMRT:
-
intensity modulated radiation therapy
- RT:
-
radiation therapy
- PCTV:
-
planning clinical target volume
- PGTV:
-
planning gross target volume
- HR:
-
hazard ratio
- 95%CI:
-
95% confidence interval
- NR:
-
not reference
- EGFR:
-
epidermal growth factor receptor
- ALK:
-
anaplastic lymphoma kinase
- mPFS:
-
median progression-free survival
- mOS:
-
median overall survival
- TRAEs:
-
treatment-related adverse events
- RCCEP:
-
reactive cutaneous capillary endothelial proliferation
Reference
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Janssen-Heijnen MLG, van Erning FN, De Ruysscher DK, Coebergh JWW. Groen HJM: Variation in causes of death in patients with non-small cell lung cancer according to stage and time since diagnosis. Ann Oncol. 2015;26(5):902–7.
Semrau S, Klautke G, Virchow JC, Kundt G, Fietkau R. Impact of comorbidity and age on the outcome of patients with inoperable NSCLC treated with concurrent chemoradiotherapy. Respir Med. 2008;102(2):210–8.
Zatloukal P, Petruzelka L, Zemanova M, Havel L, Janku F, Judas L, Kubik A, Krepela E, Fiala P, Pecen L. Concurrent versus sequential chemoradiotherapy with cisplatin and vinorelbine in locally advanced non-small cell lung cancer: a randomized study. Lung Cancer. 2004;46(1):87–98.
Patel AB, Edelman MJ, Kwok Y, Krasna MJ, Suntharalingam M. Predictors of acute esophagitis in patients with non-small-cell lung carcinoma treated with concurrent chemotherapy and hyperfractionated radiotherapy followed by surgery. Int J Radiat Oncol Biol Phys. 2004;60(4):1106–12.
Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, Kurata T, Chiappori A, Lee KH, de Wit M, et al. Overall Survival with Durvalumab after Chemoradiotherapy in Stage III NSCLC. N Engl J Med. 2018;379(24):2342–50.
Shaverdian N, Offin MD, Rimner A, Shepherd AF, Wu AJ, Rudin CM, Hellmann MD, Chaft JE, Gomez DR. Utilization and factors precluding the initiation of consolidative durvalumab in unresectable stage III non-small cell lung cancer. Radiother Oncol. 2020;144:101–4.
Zhai Y, Ma H, Hui Z, Zhao L, Li D, Liang J, Wang X, Xu L, Chen B, Tang Y, et al. HELPER study: A phase II trial of continuous infusion of endostar combined with concurrent etoposide plus cisplatin and radiotherapy for treatment of unresectable stage III non-small-cell lung cancer. Radiother Oncol. 2019;131:27–34.
Xu H, Lv D, Meng Y, Wang M, Wang W, Zhou C, Zhou S, Chen X, Yang H. Endostar improved efficacy of concurrent chemoradiotherapy with vinorelbine plus carboplatin in locally advanced lung squamous cell carcinoma patients with high serum Lp(a) concentration. Ann Palliat Med. 2020;9(2):298–307.
Zhang SL, Han CB, Sun L, Huang LT, Ma JT. Efficacy and safety of recombinant human endostatin combined with radiotherapy or chemoradiotherapy in patients with locally advanced non-small cell lung cancer: a pooled analysis. Radiat Oncol. 2020;15(1):205.
Jianbo Zhu, Guangpeng Chen, Kai Niu, Yongdong Feng, Lijiao Xie, Si Qin, Zhongyu Wang, Jixi Li, Song Lang. Zhuo Wenlei et al Efficacy and safety of recombinant human endostatin during peri-radiotherapy period in advanced non-small-cell lung cancer. Future Oncology. 2022;18(9):1077–87.
Hillman GG, Lonardo F, Hoogstra DJ, Rakowski J, Yunker CK, Joiner MC, Dyson G, Gadgeel S, Singh-Gupta V. Axitinib Improves Radiotherapy in Murine Xenograft Lung Tumors. Transl Oncol. 2014;7(3):400–9.
Gao RW, Day CN, Yu NY, Bush A, Amundson AC, Prodduturvar P, Majeed U, Butts E, Oliver T, Schwecke AJ, et al. Dosimetric predictors of pneumonitis in locally advanced non-small cell lung cancer patients treated with chemoradiation followed by durvalumab. Lung Cancer. 2022;170:58–64.
Tsujino K, Hirota S. Masahiro Endo, Kayoko Obayashi, Kotani Y, Miyako Satouchi, Kado T, Takada Y: Predictive value of dose-volume histogram parameters for predicting radiation pneumonitis after concurrent chemoradiation for lung cancer. J Radiat Oncol Biol Phys. 2003;55(1):110–5.
Palma DA, Senan S, Tsujino K, Barriger RB, Rengan R, Moreno M, Bradley JD, Kim TH, Ramella S, Marks LB, et al. Predicting radiation pneumonitis after chemoradiation therapy for lung cancer: an international individual patient data meta-analysis. Int J Radiat Oncol Biol Phys. 2013;85(2):444–50.
Institute. NC: Common Terminology Criteria for Adverse Events v5.0. (CTCAE) Publish date November 27, 2017. (https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50. ). Accessed April 11, 2022.
Ma H, Peng F, Xu Y, Bao Y, Hu X, Wang J, Fang M, Kong Y, Dong B, Chen M. Five-year survival rate analysis: the combination of fortnightly-administration of endostar and concurrent chemoradiotherapy versus concurrent chemoradiotherapy in the treatment of inoperable locally advanced non-small cell lung cancer. Ann Palliat Med. 2021;10(7):7560–70.
Sun XJ, Deng QH, Yu XM, Ji YL, Zheng YD, Jiang H, Xu YP, Ma SL. A phase II study of Endostatin in combination with paclitaxel, carboplatin, and radiotherapy in patients with unresectable locally advanced non-small cell lung cancer. BMC cancer. 2016;16:266.
Bao Y, Peng F, Zhou QC, Yu ZH, Li JC, Cheng ZB, Chen L, Hu X, Chen YY, Wang J, et al. Phase II trial of recombinant human endostatin in combination with concurrent chemoradiotherapy in patients with stage III non-small-cell lung cancer. Radiother Oncol. 2015;114(2):161–6.
Honglian M, Zhouguang H, Fang P, Lujun Z, Dongming L, Yujin X, Yong B, Liming X, Yirui Z, Xiao H, et al. Different administration routes of recombinant human endostatin combined with concurrent chemoradiotherapy might lead to different efficacy and safety profile in unresectable stage III non-small cell lung cancer: Updated follow-up results from two phase II trials. Thorac Cancer. 2020;11(4):898–906.
Bernchou U, Christiansen RL, Asmussen JT, Schytte T, Hansen O, Brink C. Extent and computed tomography appearance of early radiation induced lung injury for non-small cell lung cancer. Radiother Oncol. 2017;123(1):93–8.
Bradley JD, Paulus R, Komaki R, Masters G, Blumenschein G, Schild S, Bogart J, Hu C, Forster K, Magliocco A, et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study. Lancet Oncol. 2015;16(2):187–99.
Tsujino Kayoko, Hashimoto Tomohisa, Shimada Temiko, Yoden Eisaku, Fujii Osamu, Ota Yosuke, Satouchi Miyako, Negoro Shunichi, Adachi Shuji. Soejima T: Combined analysis of V20, VS5, pulmonary fibrosis score on baseline computed tomography, and patient age improves prediction of severe radiation pneumonitis after concurrent chemoradiotherapy for locally advanced non-small-cell lung cancer. J Thorac Oncol. 2014;9(7):983–90.
Wu K, Xu X, Li X, Wang J, Zhu L, Chen X, Wang B, Zhang M, Xia B, Ma S. Radiation pneumonitis in lung cancer treated with volumetric modulated arc therapy. J Thorac Dis. 2018;10(12):6531–9.
Jun D, Guang L, Lianghua M, Rao D, Shuang Z, Chong H, Shuo Z, Lei Y. Predictors of grade ≥ 2 and grade ≥ 3 radiation pneumonitis in patients with locally advanced non-small cell lung cancer treated with three-dimensional conformal radiotherapy. Acta Oncol. 2012;52(6):1175–80.
Dang J, Li G, Zang S, Zhang S, Yao L. Comparison of risk and predictors for early radiation pneumonitis in patients with locally advanced non-small cell lung cancer treated with radiotherapy with or without surgery. Lung Cancer. 2014;86(3):329–33.
Jang JY, Kim SS, Song SY, Kim YJ, Kim SW, Choi EK. Radiation pneumonitis in patients with non-small-cell lung cancer receiving chemoradiotherapy and an immune checkpoint inhibitor: a retrospective study. Radiat Oncol. 2021;16(1):231.
Meng Y, Luo W, Wang W, Zhou C, Zhou S, Tang X, Hou L, Kong FS, Yang H. Intermediate Dose-Volume Parameters, Not Low-Dose Bath, Is Superior to Predict Radiation Pneumonitis for Lung Cancer Treated With Intensity-Modulated Radiotherapy. Front Oncol. 2020;10:584756.
Tannehill SP, Mehta MP, Larson M, Storer B, Pellet J, Kinsella TJ, Schiller JH. Effect of amifostine on toxicities associated with sequential chemotherapy and radiation therapy for unresectable non-small-cell lung cancer: results of a phase II trial. J Clin Oncol. 1997;15(8):2850–7.
Calabro-Jones P, Fahey R, Smoluk G, Ward J. Alkaline phosphatase promotes radioprotection and accumulation of WR-1065 in V79–171 cells incubated in medium containing WR-2721. Int J Radiat Biol Relat Stud Phys Chem Med. 1985;47(1):23–7.
Antonadou, Coliarakis N, Synodinou M, Athanassiou H, Kouveli CV, Georgakopoulos G, Panoussaki K, Karageorgis P, Throuvalas N. Group CROH Randomized phase III trial of radiation treatment amifostine in patients with advanced-stage lung cancer. Int J Radiat Oncol Biol Phys. 2001;51(4):915–22.
Bourhis J, Blanchard P, Maillard E, Brizel DM, Movsas B, Buentzel J, Langendijk JA, Komaki R, Swan Leong S, Levendag P, et al. Effect of amifostine on survival among patients treated with radiotherapy: a meta-analysis of individual patient data. J Clin Oncol. 2011;29(18):2590–7.
Devine A, Marignol L. Potential of Amifostine for Chemoradiotherapy and Radiotherapy-associated Toxicity Reduction in Advanced NSCLC: A Meta-Analysis. Anticancer Res. 2016;36(1):5–12.
Komaki R, Lee JS, Milas L, Lee HK, Fossella FV, Herbst RS, Allen PK, Liao Z, Stevens CW, Lu C, et al. Effects of amifostine on acute toxicity from concurrent chemotherapy and radiotherapy for inoperable non-small-cell lung cancer: report of a randomized comparative trial. Int J Radiat Oncol Biol Phys. 2004;58(5):1369–77.
Komaki R, Lee JS, Kaplan B, Allen P, Kelly JF, Liao Z, Stevens CW, Fossella FV, Zinner R, Papadimitrakopoulou V, et al. Randomized phase III study of chemoradiation with or without amifostine for patients with favorable performance status inoperable stage II-III non-small cell lung cancer: preliminary results. Semin Radiat Oncol. 2002;12(1 Suppl 1):46–9.
Antonadou D, Throuvalas N, Petridis A, Bolanos N, Sagriotis A, Synodinou M. Effect of amifostine on toxicities associated with radiochemotherapy in patients with locally advanced non–small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2003;57(2):402–8.
Jackson IL, Chen L, Batinic-Haberle I, Vujaskovic Z. Superoxide dismutase mimetic reduces hypoxia-induced O2*-, TGF-beta, and VEGF production by macrophages. Free Radic Res. 2007;41(1):8–14.
Tanabe K, Maeshima Y, Ichinose K, Kitayama H, Takazawa Y, Hirokoshi K, Kinomura M, Sugiyama H, Makino H. Endostatin peptide, an inhibitor of angiogenesis, prevents the progression of peritoneal sclerosis in a mouse experimental model. Kidney Int. 2007;71(3):227–38.
Zhang K, Yang S, Zhu Y, Mo A, Zhang D, Liu L. Protection against acute radiation-induced lung injury: a novel role for the anti-angiogenic agent Endostar. Mol Med Rep. 2012;6(2):309–15.
Huang Y, Yuan J, Righi E, Kamoun WS, Ancukiewicz M, Nezivar J, Santosuosso M, Martin JD, Martin MR, Vianello F, et al. Vascular normalizing doses of antiangiogenic treatment reprogram the immunosuppressive tumor microenvironment and enhance immunotherapy. Proc Natl Acad Sci U S A. 2012;109(43):17561–6.
Zheng YF, Ge W, Xu HL, Cao DD, Liu L, Ming PP, Li CH, Xu XM, Tao WP, Tao ZZ. Endostar enhances the antitumor effects of radiation by affecting energy metabolism and alleviating the tumor microenvironment in a Lewis lung carcinoma mouse model. Oncol Lett. 2015;10(5):3067–72.
Wu L, Pu X, Chen B, Wang Q, Liu L, Li K, Kong Y, Xu F, Li J, Xu L, et al. P40.14 Efficacy and Safety of Endostar Combined With Camrelizumab and Chemotherapy in Treatment of Advanced NSCLC A Multi-Center Retrospective Study. J Thorac Oncol. 2021;16(10):S1075–6.
Wu L, Pu XX, Chen LB, Wang ZQ, Liu YL, Li K, et al. EP08.01-095 efficacy and safety of combining Endostar with Camrelizumab plus chemotherapy in advanced NSCLC patients: a multi-center retrospective study. J Thorac Oncol. 2022;17(9):S388.
Lv W, Pei X, Zhao W, Cong Y, Wei Y, Li T, Zhang H, Lin Z, Saito Y, Kim JJ, et al. Safety and efficacy of nivolumab plus recombinant human endostatin in previously treated advanced non-small-cell lung cancer. Translational Lung Cancer Research. 2022;11(2):201–12.
Yang Y, Li L, Jiang Z, Wang B, Pan Z. Anlotinib optimizes anti-tumor innate immunity to potentiate the therapeutic effect of PD-1 blockade in lung cancer. Cancer Immunol Immunother. 2020;69(12):2523–32.
Wu J, Zhao X, Sun Q, Jiang Y, Zhang W, Luo J, Li Y. Synergic effect of PD-1 blockade and endostar on the PI3K/AKT/mTOR-mediated autophagy and angiogenesis in Lewis lung carcinoma mouse model. Biomed Pharmacother. 2020;125:109746.
Zhao S, Ren S, Jiang T, Zhu B, Li X, Zhao C, Jia Y, Shi J, Zhang L, Liu X, et al. Low-Dose Apatinib Optimizes Tumor Microenvironment and Potentiates Antitumor Effect of PD-1/PD-L1 Blockade in Lung Cancer. Cancer Immunol Res. 2019;7(4):630–43.
Chu T, Zhong R, Zhong H, Zhang B, Zhang W, Shi C, Qian J, Zhang Y, Chang Q, Zhang X, et al. Phase 1b Study of Sintilimab Plus Anlotinib as First-line Therapy in Patients With Advanced NSCLC. J Thorac Oncol. 2021;16(4):643–52.
Zhou C, Wang Y, Zhao J, Chen G, Liu Z, Gu K, Huang M, He J, Chen J, Ma Z, et al. Efficacy and Biomarker Analysis of Camrelizumab in Combination with Apatinib in Patients with Advanced Nonsquamous NSCLC Previously Treated with Chemotherapy. Clin Cancer Res. 2021;27(5):1296–304.
Taylor MH, Lee CH, Makker V, Rasco D, Dutcus CE, Wu J, Stepan DE, Shumaker RC, Motzer RJ. Phase IB/II Trial of Lenvatinib Plus Pembrolizumab in Patients With Advanced Renal Cell Carcinoma, Endometrial Cancer, and Other Selected Advanced Solid Tumors. J Clin Oncol. 2020;38(11):1154–63.
Herbst RS, Arkenau H-T, Santana-Davila R, Calvo E, Paz-Ares L, Cassier PA, Bendell J, Penel N, Krebs MG, Martin-Liberal J, et al. Ramucirumab plus pembrolizumab in patients with previously treated advanced non-small-cell lung cancer, gastro-oesophageal cancer, or urothelial carcinomas (JVDF): a multicohort, non-randomised, open-label, phase 1a/b trial. Lancet Oncol. 2019;20(8):1109–23.
Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, Rodriguez-Abreu D, Moro-Sibilot D, Thomas CA, Barlesi F, et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288–301.
Acknowledgments
We would like to thank all authors for their efforts on this article.
Funding
This study was funded by the Chinese National Science Foundation Projects (NSFC81874221), the Basic Public Welfare Research Project of Zhejiang Province (LGF21H160027), and the Open project of Zhejiang Key Laboratory of Radiation Oncology(2022ZJCCRAD03).
Author information
Authors and Affiliations
Contributions
HH Y conceived and conceptualized the study,provided funding. SN Z performed data review and analyses, reviewed and edited the manuscript. KF C managed project execution, performed experimental design & data review and analyses, drafted the manuscript. SL L, M C, ZC J and XF S performed experimental design and execution. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The need for written informed consent was waived by the Taizhou hospital of Zhejiang Province ethics committee due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, K., Li, S., Chen, M. et al. Endostar acts as a pneumonitis protectant in patients with locally advanced non-small cell lung cancer receiving concurrent chemoradiotherapy. BMC Cancer 24, 257 (2024). https://doi.org/10.1186/s12885-024-12001-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12001-6