Abstract
Background
Identifying lymph node metastasis areas during surgery for early invasive lung adenocarcinoma remains challenging. The aim of this study was to develop a nomogram mathematical model before the end of surgery for predicting lymph node metastasis in patients with early invasive lung adenocarcinoma.
Methods
In this study, we included patients with invasive lung adenocarcinoma measuring ≤ 2 cm who underwent pulmonary resection with definite pathology at Qilu Hospital of Shandong University from January 2020 to January 2022. Preoperative biomarker results, clinical features, and computed tomography characteristics were collected. The enrolled patients were randomized into a training cohort and a validation cohort in a 7:3 ratio. The training cohort was used to construct the predictive model, while the validation cohort was used to test the model independently. Univariate and multivariate logistic regression analyses were performed to identify independent risk factors. The prediction model and nomogram were established based on the independent risk factors. Recipient operating characteristic (ROC) curves were used to assess the discrimination ability of the model. Calibration capability was assessed using the Hosmer–Lemeshow test and calibration curves. The clinical utility of the nomogram was assessed using decision curve analysis (DCA).
Results
The overall incidence of lymph node metastasis was 13.23% (61/461). Six indicators were finally determined to be independently associated with lymph node metastasis. These six indicators were: age (P < 0.001), serum amyloid (SA) (P = 0.008); carcinoma antigen 125 (CA125) (P = 0. 042); mucus composition (P = 0.003); novel aspartic proteinase of the pepsin family A (Napsin A) (P = 0.007); and cytokeratin 5/6 (CK5/6) (P = 0.042). The area under the ROC curve (AUC) was 0.843 (95% CI: 0.779–0.908) in the training cohort and 0.838 (95% CI: 0.748–0.927) in the validation cohort. the P-value of the Hosmer–Lemeshow test was 0.0613 in the training cohort and 0.8628 in the validation cohort. the bias of the training cohort corrected C-index was 0.8444 and the bias-corrected C-index for the validation cohort was 0.8375. demonstrating that the prediction model has good discriminative power and good calibration.
Conclusions
The column line graphs created showed excellent discrimination and calibration to predict lymph node status in patients with ≤ 2 cm invasive lung adenocarcinoma. In addition, the predictive model has predictive potential before the end of surgery and can inform clinical decision making.
Similar content being viewed by others
Introduction
Lung cancer (LC) is the second most prevalent tumor and remains the leading cause of malignancy-related deaths worldwide by far [1]. LC is commonly classified into small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). Among them, adenocarcinoma is the most important subtype of NSCLC and the most common type of LC. With the increasing popularity of low-dose spiral computed tomography (CT) in health screening and disease diagnosis, the incidence of ≤ 2 cm lung cancer has been increasing [2]. For early-stage lung adenocarcinoma, more thoracic surgeons are accepting segmental or subsegmental resection and selective lymph node dissection as the optimal treatment modality [3, 4]. However, in some LC cases, lymph node metastasis (LNM) occurs in the early stages of the tumor. The incidence of LNM in LC cases with lesions ≤ 2 cm in diameter has been reported to be about 10% [5, 6]. Emerging evidence suggests that lymph node metastasis is a risk factor for poor prognosis in patients with early-stage lung adenocarcinoma [7]. Unfortunately, the accuracy of preoperative lymph node staging CT scans is only 45%-79% [8,9,10,11,12]. Preoperative mediastinoscopy and endobronchial ultrasound transbronchial needle aspiration are not routinely used in patients with clinical stage I disease, and these methods have produced a considerable number of false-negative results [13,14,15]. Complete clearance of metastatic lymph nodes during surgery plays a key role in improving the disease-free survival and overall survival of patients [16]. Therefore, it is necessary to accurately assess preoperative lymph nodes metastasis in NSCLC.
It has been shown that adenocarcinomas with micropapillary and solid growth patterns are more aggressive and have a poorer prognosis [17, 18]. In addition, blood inflammatory markers and tumor markers can be used to predict lymph node metastasis in lung cancer [19,20,21,22]. CT remains the most widely used tool to assess tumor and lymph node involvement in patients with early-stage non-small cell lung cancer [8,9,10,11]. Some researchers claim that frozen sections are a key indicator to guide the approach to resection [23] and that it is feasible to report histological subtypes and other pathological features during surgery [24, 25].
To date, many studies have explored independent predictors of lymph node metastasis [26,27,28,29,30,31,32]. These include carcinoembryonic antigen (CEA) [26], tumor size [26], standardized uptake value maximum (SUVmax) [27], female [28], never smoker[28], adenocarcinoma histology [28], positive N1 lymph nodes on positron emission tomography (PET) [29], blood inflammation biomarkers [30], neutrophil to lymphocyte ratio (NLR) [31] and consolidation-to-tumor ratio (CTR) [32], ect. However, only a few studies have developed comprehensive models to predict lymph node metastasis based on radiological features, patient clinical information, and hematological parameters.
In our study, we explored the risk factors for lymph node metastasis in a cohort of patients with early invasive lung cancer and developed a nomogram model for predicting the risk of lymph node metastasis based on patient clinical information, hematologic indicators, imaging features, and pathologic findings. The aim was to enable the nomogram to quickly and accurately predict the incidence of lymph node metastasis before or during surgery, which may provide a computational method for surgeons to make intraoperative decisions.
Materials and methods
Patients
This study was approved by the Ethics Committee of Qilu Hospital, Shandong University (registration number: KYLL-202008–023-1), and all patients signed an informed consent form for the use of their clinical information prior to the procedure.
Patients with invasive adenocarcinoma from January 2020 to December 2021 at Qilu Hospital of Shandong University were retrospectively evaluated.
The inclusion criteria were: (1) patients with a single intrapulmonary nodule suggested by chest CT within 1 month before surgery; (2) nodules with a maximum diameter ≤ 20 mm on CT; (3) undergoing pneumonectomy (lobectomy or subpneumonectomy) with systemic lymph node dissection; (4) complete pathological data and pathological type of Invasive lung adenocarcinoma; (5) not receiving neoadjuvant chemotherapy or radiotherapy before surgery; (6) no pulmonary atelectasis and active inflammatory images of the lungs. Exclusion criteria were (1) patients < 18 years of age, (2) open-heart surgery, (3) incomplete perioperative data, and (4) patients with a history of malignant disease within 5 years. (5) combination of acute infectious diseases that can cause changes in the levels of systemic inflammatory markers; (6) presence of distant metastases.
A total of 2213 patients were included in this study, and after our exclusion according to the above-mentioned criteria, 522 patients with invasive lung adenocarcinoma with tumor size ≤ 2 cm were finally recruited in our study. Figure 1 shows the flow chart of included patients.
Clinical data of patients
Clinicopathological information was collected from the patient record management system as follows: age, gender, presence of preoperative comorbidities [hypertension, diabetes mellitus, and chronic obstructive pulmonary disease (COPD)], history of smoking, body mass index (BMI), predicted percent forceful expiratory volume in one second (FEV1% predicted), predicted percent maximum voluntary ventilation (MVV% predicted), and American Society of Anesthesiologists (ASA) score.
Hematological test
Record hematologic parameters within 2 weeks prior to surgery as follows. (1) Blood count: neutrophils, basophils, eosinophils, lymphocytes, monocytes, red blood cells, platelets, albumin, hemoglobin, blood glucose, blood type. (2) Serum enzyme count: serum 5'-nucleotidase (5'-NT), serum amylase (SA), lactate dehydrogenase (LDH). (3) Tumor markers: carcinoembryonic antigen 125 (CA125), neuron-specific enolase (NSE), carcinoembryonic antigen (CEA), gastrin-releasing peptide (pro-GRP), cytokeratin 19-fragment (cybra21-1), and squamous carcinoma antigen (SCC). (4) Inflammatory markers: serum complement C1q and derived neutrophil–lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR), monocyte-lymphocyte ratio (MLR), derived neutrophil–lymphocyte ratio (dNLR), neutrophil–lymphocyte and platelet ratio (NLPR), systemic inflammatory response syndrome (SIRS), total systemic inflammatory index (AISI) and systemic inflammatory index (SII). These derived inflammatory indicators were calculated as follows.
-
NLR = neutrophils/lymphocytes.
-
PLR = platelets/lymphocytes.
-
MLR = monocytes/lymphocytes.
-
dNLR = [neutrophils/ (leukocytes—neutrophils)].
-
NLPR = [Neutrophils/ (lymphocytes × platelets)].
-
SIRI = [(neutrophils × monocytes)/lymphocytes)].
-
AISI = [(neutrophils × monocytes × platelets)/lymphocytes].
-
SII = [(neutrophils x platelets)/lymphocytes)].
Imaging analysis
The morphological features of computed tomography include: location (central or peripheral), shape (regular or irregular), spiculation, calcification, cavity sign, bronchial sign, lobar sign, pleural adhesion sign, vascular penetration sign, pleural effusion sign, maximum tumor diameter, lymph node enlargement sign, and consolidation to tumor ratio (CTR). Two radiologists measured each imaging feature independently, and a third radiologist with more than 20 years of experience in chest radiology reassessed the discrepancies. Any disagreements were resolved by consensus.
Centrality was defined as nodules located in the bronchi, lobular bronchi, and segmental bronchi. Peripherality was defined as nodules located below the tertiary bronchi. Spiculation was defined as spread from the nodal margins to the lung parenchyma without contacting the pleural surface. Signs of calcification were defined as having one of these patterns on CT imaging: stratification, central nodule, diffusion, or popcorn pattern. Cavitation signs were defined as gas-filled spaces that are considered to be transparent or low-attenuation regions. The bronchial sign shows direct bronchial involvement of nodules on CT images. Lobulation was defined as the wavy or fan-shaped portion of the lesion surface and the strands extending from the nodal margins into the lung parenchyma. Signs of pleural adhesions were defined as linear attenuation or major or minor fissures toward the pleura. The vascular penetration sign was observed on the CT image with a pulmonary artery crossing the node. The pleural effusion sign was defined as a blunting of the rib-diaphragm angle visible on the CT image. The lymph node enlargement sign was the enlargement of mediastinal lymph nodes that can be observed on CT images.CTR was defined as the ratio of the diameter of the solid component of the lung nodule to the maximum diameter of the nodule.
Histological evaluation
All pathological specimens were fixed in formalin, stained with hematoxylin–eosin, and evaluated by two experienced lung pathologists. Histopathological evaluation was performed by examining hematoxylin–eosin-stained slides with a light microscope. All specimens were classified according to the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification of adenocarcinoma of the lung [33]. The pathological lymph node status of patients was confirmed according to the 8th edition of the TNM lung cancer classification.
The percentage of each histological component (mucinous, lepidic, acinar, papillary, micropapillary and solid pattern) was recorded in 5% increments and the tumors were classified according to the predominant pattern. The pattern was considered present if ≥ 5% of the histological pattern was present in the tumor.
DNA purification and quantification
Cutting all formalin-fixed paraffin-embedded (FFPE) specimens to 5–8 μm thickness. Thereafter, DNA and RNA extraction was performed using 5–30 tissue sections with at least 2% tumor cells using the FFPE DNA/RNA Nucleic Acid Extraction Kit (No. 8.0223601X036G, Xiamen Diagnostics, Xiamen, China). After isolation of DNA and RNA, the concentrations of DNA and RNA were determined using a microscopic spectrophotometer. the RNA concentrations ranged from 10 to 500 ng/μL and the DNA concentrations were > 2 ng/μL.
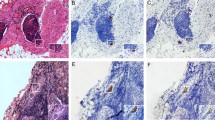
Immunohistochemistry Validation in Resected Patients
All IHC staining was performed in the clinical immunohistochemistry laboratory of our hospital pathology department. All IHC staining was performed in the clinical immunohistochemistry laboratory of our hospital pathology department. Briefly, specimens were sectioned at 5 μm, dewaxed and incubated with primary antibody. Staining characteristics as well as the intensity and distribution of staining patterns were reviewed and considered. If more than 5% of the tumor cells with the appropriate staining pattern were found, the case was considered positive; otherwise, the case was considered negative. Immunohistochemistry was verified for CK5/6, CK7, Napsin A, MUC-AC, P63, Ki-67% positive rate, CyclinD1, EMA, CD31, D2-40, etc.
special staining in resected patients
The Periodic Acid-Schiff (PAS) reaction, Periodic Acid-Schiff reaction with diastase (PAS-D) and elastic fibers are three special staining procedures that are commonly performed in a histology laboratory. The staining reaction was classified as positive or negative by three "blinded" observers.
Statistical analysis
All statistical analyses were performed using SPSS 26.0 (SPSS Inc., Chicago, Illinois, USA) and R statistical software (Windows version 4.2.1, http: //www.r-project.org/). We used the “rms package” to plot the nomogram, “pROC” to plot the ROC curve, and “rmda” to plot the DCA curve. Categorical variables were compared using Pearson's Chi-square test or Fisher's exact test. Normally distributed continuous variables were expressed as mean ± standard deviation (SD) and compared using the Student's t-test. For non-normally distributed continuous variables, data were expressed as medians (interquartile range [IQR]) and compared between two groups using the Mann–Whitney U test. Statistical significance was described as a two-sided P value of less than 0.05.
We implement the random assignment of patients through the R. All enrolled patients were randomly assigned to the training and validation cohorts in a 7:3 ratio, using a randomly segmented sample. The training cohort was used to develop the prediction nomograms, while the validation cohort was used to verify the performance of the nomograms.
Predictive model development and validation
Construction of nomogram
The training cohort data were first analyzed by univariate logistic regression analysis to identify potential risk factors. Those factors with P-values less than 0.05 in univariate analysis were included in further multivariate logistic regression analyses. Finally, predictive models were developed using independent risk factors (P < 0.05 in multivariate logistic regression). A nomogram was created by using R statistical software (Windows version 4.2.1, http: //www.r-project.org/). Area under the curve (AUC) was determined, and receiver operating characteristic (ROC) curves were created. A regression model was used to calculate scores for each variable, and the predicted probability of risk of lymph node metastasis in small-sized non-small cell lung cancer could be derived by summing the scores for each variable.
Nomogram performance
An assessment of the performance of predictive nomograms is made by discriminative power, calibration and clinical utility. Discriminative power is the capability of a model to correctly differentiate between events and non-events.ROC curves are employed to assess the recognition efficiency of predictive nomograms [34]. A measurement of how well the predicted probability matches the actual result is called calibration. the Hosmer–Lemeshow test can be used to assess calibration ability, with a p-value greater than 0.05 indicating satisfactory calibration [35]. Subsequently a nomogram calibration plot is formed to further assess the calibration. This was verified internally by using a bootstrap method repeated 1000 times [36]. Predictive nomograms were evaluated for clinical effectiveness using decision curve analysis (DCA) based on the net benefit of different threshold probabilities [37]. The optimal cutoff value was determined when the Youden index (sensitivity + specificity-1) reached its maximum value based on ROC curve analysis of the training cohort.
Results
Patient characteristics
A total of 522 patients were enrolled in this study. The overall incidence of lymph node metastasis was 13.23% (61/461). Of all patients enrolled, 284 were women and 138 were men. The median age was 61 (range: 31–81) years. the median tumor size on CT was 1.2 (range: 0.3–2) cm. Demographic characteristics and variable data for both cohorts are shown in Table 1. The training cohort included 366 (70.1%) patients, whereas the validation cohort included 156 (29.9%) patients. The characteristics of the two cohorts were similar, with p-values > 0.05 except for MVV% predicted, and the differences in distribution were not statistically significant. Detailed information on the features of the two groups in the training and validation groups is shown in Table 2.
Identifying risk factors for lymph node metastasis
Univariate and then multivariate logistic regression analyses were performed in the training cohort to investigate independent risk factors for lymph node metastasis, and the results of the logistic regression analyses are shown in Table 3.
Univariate analysis showed that as many as 30 factors were potential risk factors for lymph node metastasis in early-stage small lung adenocarcinoma (P < 0.05). After further multivariate logistic regression analysis, six indicators were finally identified to be independently associated with lymph node metastasis. The six indicators were: age [odds ratio (OR) = 0.934; 95% confidence interval (CI): 0.871–0.996; P < 0.001]; SA (OR = 1.025; 95% CI: 0.937–1.109; P = 0.008); CA125 (OR = 1.103; 95% CI: 1.021–1.189; P = 0.042); Mucinous (no and yes; OR = 1.729; 95% CI: 0.371–7.519; P = 0.003); Napsin A (no and yes; OR = 2.704; 95% CI: 0.489–15.541; P = 0.007); and CK5/6 (no and yes; OR = 18.668; 95% CI: 2.938–154.991; P = 0.042). The results of the multifactorial logistic regression analysis of the 30 factors screened in this study are detailed in the forest plot (Fig. 2).
Multi-factor logistic regression analysis of forest plots. PNI, prognostic nutritional index; PLR, platelet-lymphocyte ratio; SA, serum amyloid; CA125, carcinoma antigen 125; BMI, body mass index; FEV1, forced expiratory volume in one second; TTF, thyroid transcription factor 1; PAS, Periodic Acid-Schiff reaction; PAS-D, Periodic Acid-Schiff reaction with diastase; CK 5/6, Cytokeratin 5/6; CK 7, Cytokeratin 7; MUC-AC, mucin-AC
Frequency of targeted gene alterations
Of the 522 patients, 46 underwent genetic alteration analysis using ARMS-PCR. Of these, 37 (80.4%) samples had gene mutations detected. The mutation frequencies of EGFR and KRAS genes were 71.7% (33/46) and 8.7% (4/46), respectively. EGFR mutations were the most common type of alteration, with 39.1% (18/46) of patients having mutations in Exon21, 26.1% (12/46) having mutations in Exon19, 2.2% (1/46) having mutations in Exon18, 2.2% (1/46) having mutations in Exon20, and 2.2% (1/46) having double mutations in Exon18 and Exon20. All of the KRAS mutations were mutations in Exon2, with a total of 4 cases or 8.7% (4/46). Of the 37 patients with genetic mutations, 4 had lymph node metastases and 33 did not. Considering the possibility of gene mutations in patients without genetic testing, this study will not include gene mutations in the univariate and multifactorial analyses, but will simply elaborate the findings.
Nomogram construction
All six independent risk factors for lymph node metastasis in small invasive lung adenocarcinoma within 2 cm were included to create a logistic regression model. The probability of lymph node metastasis in small invasive lung adenocarcinoma could be calculated by the following formula: ln (p/1-p) = -0.068 × age + 0.025 × SA + 0.098 × CA125 + 0.547 × mucinous (no = 0; yes = 1) + 2.927 × CK5/6 (no = 0; yes = 1)—13.972. Based on the above equation, a nomogram of the predicted probability of lymph node metastasis in invasive lung adenocarcinoma within 2 cm was plotted using R statistical software (Fig. 3). As shown in this nomogram, there are 9 axes, and axes 2–7 represent the six variables in the prediction model. By drawing a line perpendicular to the highest point axis, the estimated score for each risk factor can be calculated and can be further summed to obtain a total score. The total score axis is then used to predict the probability of developing lymph node metastasis in invasive lung adenocarcinoma, which in turn can further guide the surgical approach.
Nomogram for predicting the probability of LNM in small invasive lung adenocarcinoma. SA, serum amyloid; CA125, carcinoma antigen 125; CK 5/6, Cytokeratin 5/6. As shown in this nomogram, there are 9 axes, and axes 2–7 represent the six variables in the prediction model. By drawing a line perpendicular to the highest point axis, the estimated score for each risk factor can be calculated and can be further summed to obtain a total score. The total score axis is then used to predict the probability of developing lymph node metastasis in invasive lung adenocarcinoma, which in turn can further guide the surgical approach
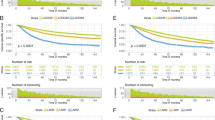
Predictive performance and validation of the nomogram
Discrimination ability of the prediction model and nomogram is assessed by the ROC curve (Fig. 4). ROC area under the curve (AUC) was 0.843 (95% CI: 0.779–0.908) for the training cohort and 0.838 (95% CI: 0.748–0.927) for the validation cohort, indicating that the nomogram has good predictive accuracy. The ROC curve for the training cohort had a threshold of 0.089 and sensitivities and specificities of 0.795 and 0.786, respectively (Table 4). Our Hosmer–Lemeshow test and calibration charts were used to assess calibration capability. Our p-value for the Hosmer–Lemeshow test was 0.0613 in the training cohort and 0.8628 in the validation cohort, indicating that the difference between the predicted and actual observed probabilities was negligible. A good calibration of the prediction nomogram is also demonstrated by the calibration plots of the training cohort (Fig. 5A) and the validation cohort (Fig. 5B). The bias-corrected C-index for the training cohort was 0.8444 and the bias-corrected C-index for the validation cohort was 0.8375, further demonstrating the goodness of the prediction model.
A, B Calibration curves of the prediction nomogram in the training cohort (A) and validation cohort (B). The X-axis represents the probability predicted by the nomogram and the Y-axis represents the actual probability of LNM in invasive lung adenocarcinoma within 2 cm. The black dashed line represents the ideal curve, the blue solid line represents the apparent curve (uncorrected), and the red solid line represents the deviation curve corrected by bootstrap method (B = 1000 times). LNM, lymph node metastasis
Clinical utility of the predictive nomogram
Just as shown in Fig. 6A and B, DCA was used to assess the clinical utility of the prediction nomogram. Findings show that the nomogram provided greater net benefit and broader threshold probabilities for predicting the risk of lymph node metastasis in invasive lung adenocarcinoma within 2 cm in both the training and validation cohorts, showing that the nomogram is clinically useful. Figure 7A and B show the clinical impact curves (CIC) for the validation cohort and the verification cohort, respectively. The curves show that a high benefit ratio is obtained within a probability threshold of 0.2–1.0. It suggests that the present model can indeed be used clinically to predict the probability of lymph node metastasis in small invasive lung adenocarcinoma.
A, B Decision curve analysis of predicted nomogram in the training cohort (A) and validation cohort (B). The y-axis measures the net benefit, the black line represents the hypothesis that no lymph node metastasis has occurred in invasive lung adenocarcinoma within 2 cm, and the gray line represents the hypothesis that lymph node metastasis has occurred in invasive lung adenocarcinoma measuring ≤ 2 cm. The blue line in Fig. 6A represents the training cohort, and the red line in Fig. 6B represents the validation cohort
A, B Clinical impact curves of predicted nomogram in the training cohort (A) and validation cohort (B). The horizontal coordinate is the probability threshold and the vertical coordinate is the number of people. The blue line indicates the number of people judged by the model to have lymph node metastasis at different probability thresholds; the red line indicates the number of people judged by the model to be at high risk and to have true lymph node metastasis at different probability thresholds. At the bottom, a cost: benefit ratio is also added, indicating the ratio of loss to benefit at different probability thresholds
Discussion
In this retrospective study, we developed a nomogram to predict the incidence of lymph node metastasis. In this study, age, SA, CA125, mucin composition, CK5/6, and napsin-A were found to be independent risk factors for lymph node metastasis. The results of genetic testing showed that EGFR was the most common alteration. A nomogram model was developed to assess the risk of lymph node metastasis, which showed consistent discriminatory performance and satisfactory calibration. In 2012, a related study by Terumoto Koike et al. identified the following four predictors of mediastinal lymph node metastasis: (age ≥ 67 years, CEA ≥ 3.5 ng/ml, tumor size ≥ 2.0 cm, and the CTR ≥ 89%) [26]. Advanced age was a common predictor in both our studies. As for hematologic components, our study showed SA and CA125 as predictors. CTR and tumor size were not shown to be associated with mediastinal lymph node metastasis in our study. The inclusion of immunologic components in the predictors is an innovative point of our study. These previously unpublished observations have potential implications for the therapeutic management of early-stage lung adenocarcinoma. This is because the nomogram may have the potential to predict lymph node status before the end of surgery and to guide surgeons in developing lymph node dissection strategies.
Many studies have been conducted on the effect of age on lymph node metastasis in non-small cell lung cancer [26, 38,39,40,41,42,43,44,45,46]. A part of the findings concluded that youth is an influential factor for lymph node metastasis in lung cancer, with a higher risk of lymph node metastasis in lung cancer patients at a younger age [26, 41,42,43]. Another part of the study showed that age had no significant effect on lymph node metastasis in lung cancer patients [44,45,46]. This discrepancy may be due to differences in the patients included in the study, sample size, and analysis methods. Therefore, the different conclusions reached in previous studies are explainable and acceptable. Based on our findings, we conclude that patients with young invasive lung adenocarcinoma are at greater risk for lymph node metastasis and require more thorough and meticulous lymph node dissection.
To date, there have been some case reports of elevated levels of SA being associated with lung cancer [47,48,49]. The predominance of salivary amylase was observed in these studies from the amylase isozyme pattern in serum and tumor tissues. Amylase levels were higher in tumor tissue than in normal lung tissue. Immunohistochemical studies revealed that amylase was located in tumor cells. Observation of ultrastructure revealed electron-dense particles in the cytoplasm of tumor cells. The findings suggest that in this case, amylase is produced by lung cancer. The possibility that serum amylase levels may be a highly sensitive marker for lung cancer was raised in these studies. Our findings found that lung adenocarcinoma patients with high levels of SA concentration in the blood had a higher risk of lymph node metastasis.
CA125 has long been recognized for its role as a classical tumor maker, not only as a predictor of lung cancer, but also as a direct correlate of tumor infiltration and metastasis. It has been confirmed that CA125 is associated with lymph node metastasis in lung cancer [50, 51]. CA125 provides important value in judging the extent of lung cancer metastasis and monitoring the progression of lung cancer disease. This study demonstrated the importance of CA125 in determining whether lymph node metastasis is present in lung cancer patients. Surgeons should be more cautious when performing lymph node dissection during lung cancer surgery when faced with patients with high serum CA125 levels.
Mucus is thought to play a key role in the development of cancer, as mucinous adenocarcinoma in many organs is associated with lymph node metastasis and poorer prognosis [52,53,54,55,56]. The mucinous glandular component of the tumor is histologically characterized by cupped and highly columnar epithelial cells and produces mucin, and the mucinous subtype is considered more malignant than other common subtypes of lung adenocarcinoma, such as squamous and alveolar subtypes [57,58,59]. Some reports with small sample sizes claim a low rate of lymph node metastasis in invasive mucinous adenocarcinoma [60,61,62,63]. The results of other studies hold the opposite opinion. The study by Zhu et al. claimed that the mucus subtype is a risk factor for distant metastasis of lung adenocarcinoma [64]. Our findings suggest that the mucus component is one of the risk factors for lymph node metastasis.
Napsin A is a human aspartate protease associated with pepsin, gastrin, renin, and histone protease [65]. IHC studies have demonstrated that Napsin A is expressed in normal human type II lung cells and alveolar macrophages [66]. Strong cytoplasmic staining for napsin A was observed in up to 87% of lung adenocarcinomas [67,68,69,70,71]. In contrast, CK5/6 is a sensitive and relatively specific marker of squamous differentiation [72,73,74]. The novelty of our study is that for the first time, lymph node metastasis was linked to these two immunohistochemical markers, demonstrating that CK5/6 and napsin A can be used to predict lymph node metastasis in invasive adenocarcinoma. However, the reasons behind why CK5/6 and napsin A can predict lymph node metastasis are still waiting to be explored and studied.
Our study has several advantages compared with other studies. First, for the first time, we included CK5/6, napsin A, and mucus components as influencing factors for lymph node metastasis in our prediction model. Second, the factors in our prediction model are common and easily available in clinical practice. Third, our prediction model has excellent discriminatory power, calibration, and clinical utility. The model is easy to use in clinical practice, and the associated nomogram guides surgeons to quickly select an optimized surgical approach.
Our study has several limitations. First, the analysis was based on retrospective data from a single institution, and the possibility of selection bias cannot be ruled out; results from other centers must be validated. Second, mutation testing was performed according to the patients' wishes. Thus, the sample size for testing their genomics is a subset of the entire cohort, which makes it challenging to include mutation information in a multiple regression analysis. Third, the limited number of cases may lead to potential bias, especially in histological subtype analysis.
Conclusion
In this study, a clinical prediction model for six risk factors was proposed. For invasive lung cancer, age, SA, CA125, mucin composition, CK5/6, and napsin-A are important risk factors associated with lymph node metastasis. Based on this line chart, surgeons may be able to predict lymph node status before the end of surgery.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author.
Abbreviations
- LNM( +):
-
Positive for lymph node metastasis
- LNM(-):
-
Negative for lymph node metastasis
- COPD:
-
Chronic obstructive pulmonary diseases
- ASA:
-
American Society of Anesthesiologists
- PNI:
-
Prognostic nutritional index
- NLR:
-
Neutrophil–lymphocyte ratio
- PLR:
-
Platelet-lymphocyte ratio
- MLR:
-
Monocyte-lymphocyte ratio
- dNLR:
-
Derived neutrophil-to-lymphocyte ratio
- NLPR:
-
Neutrophil to lymphocyte and platelet ratio
- SIRI:
-
Systemic inflammatory response syndrome
- AISI:
-
Aggregate index of systemic inflammation
- SII:
-
Systemic inflammation index
- LDH:
-
Lactate dehydrogenase
- SA:
-
Serum amyloid
- 5'-NT:
-
5'-Nucleotidase
- Pro-GRP:
-
Pro-gastrin-releasing peptide
- SCC:
-
Squamous cell carcinoma
- Cyfra21-1:
-
Cytokeratin 19-fragments
- CEA:
-
Carcinoembryonic antigen
- CA125:
-
Carcinoma antigen 125
- NSE:
-
Neuron-specific enolase
- BMI:
-
Body mass index
- FEV1:
-
Forced expiratory volume in one second
- MVV:
-
Maximal voluntary ventilation
- CTR:
-
Consolidation-to-tumor ratio
- TTF:
-
Thyroid transcription factor 1
- PAS:
-
Periodic Acid-Schiff reaction
- PAS-D:
-
Periodic Acid-Schiff reaction with diastase
- CK 5/6:
-
Cytokeratin 5/6
- CK 7:
-
Cytokeratin 7
- MUC-AC:
-
Mucin-AC
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33.
Walter JE, Heuvelmans MA, de Jong PA, Vliegenthart R, van Ooijen PMA, Peters RB, et al. Occurrence and lung cancer probability of new solid nodules at incidence screening with low-dose CT: analysis of data from the randomised, controlled NELSON trial. Lancet Oncol. 2016;17(7):907–16.
Kuroda H, Sakata S, Takahashi Y, Nakada T, Oya Y, Sugita Y, et al. Subsegmental resection preserves regional pulmonary function: a focus on thoracoscopy. Thorac Cancer. 2021;12(7):1033–40.
Iwata H, Shirahashi K, Mizuno Y, Yamamoto H, Takemura H. Feasibility of segmental resection in non-small-cell lung cancer with ground-glass opacity. Eur J Cardiothorac Surg. 2014;46(3):375–9 (discussion 9).
Pani E, Kennedy G, Zheng X, Ukert B, Jarrar D, Gaughan C, et al. Factors associated with nodal metastasis in 2-centimeter or less non-small cell lung cancer. J Thorac Cardiovasc Surg. 2020;159(3):1088-96.e1.
Yu X, Li Y, Shi C, Han B. Risk factors of lymph node metastasis in patients with non-small cell lung cancer ≤ 2 cm in size: a monocentric population-based analysis. Thorac Cancer. 2018;9(1):3–9.
Higgins KA, Chino JP, Ready N, D’Amico TA, Berry MF, Sporn T, et al. Lymphovascular invasion in non-small-cell lung cancer: implications for staging and adjuvant therapy. J Thorac Oncol. 2012;7(7):1141–7.
Gdeedo A, Van Schil P, Corthouts B, Van Mieghem F, Van Meerbeeck J, Van Marck E. Prospective evaluation of computed tomography and mediastinoscopy in mediastinal lymph node staging. Eur Respir J. 1997;10(7):1547–51.
Gupta NC, Graeber GM, Bishop HA. Comparative efficacy of positron emission tomography with fluorodeoxyglucose in evaluation of small (<1 cm), intermediate (1 to 3 cm), and large (>3 cm) lymph node lesions. Chest. 2000;117(3):773–8.
Prenzel KL, Mönig SP, Sinning JM, Baldus SE, Brochhagen HG, Schneider PM, et al. Lymph node size and metastatic infiltration in non-small cell lung cancer. Chest. 2003;123(2):463–7.
Sioris T, Järvenpää R, Kuukasjärvi P, Helin H, Saarelainen S, Tarkka M. Comparison of computed tomography and systematic lymph node dissection in determining TNM and stage in non-small cell lung cancer. Eur J Cardiothorac Surg. 2003;23(3):403–8.
Steinert HC, Hauser M, Allemann F, Engel H, Berthold T, von Schulthess GK, et al. Non-small cell lung cancer: nodal staging with FDG PET versus CT with correlative lymph node mapping and sampling. Radiology. 1997;202(2):441–6.
Hermens FH, Van Engelenburg TC, Visser FJ, Thunnissen FB, Termeer R, Janssen JP. Diagnostic yield of transbronchial histology needle aspiration in patients with mediastinal lymph node enlargement. Respiration. 2003;70(6):631–5.
Annema JT, Veseliç M, Versteegh MI, Willems LN, Rabe KF. Mediastinal restaging: EUS-FNA offers a new perspective. Lung Cancer. 2003;42(3):311–8.
FreixinetGilart J, García PG, de Castro FR, Suárez PR, Rodríguez NS, de Ugarte AV. Extended cervical mediastinoscopy in the staging of bronchogenic carcinoma. Ann Thorac Surg. 2000;70(5):1641–3.
Boffa DJ, Kosinski AS, Paul S, Mitchell JD, Onaitis M. Lymph node evaluation by open or video-assisted approaches in 11,500 anatomic lung cancer resections. Ann Thorac Surg. 2012;94(2):347–53 (discussion 53).
Ohtaki Y, Yoshida J, Ishii G, Aokage K, Hishida T, Nishimura M, et al. Prognostic significance of a solid component in pulmonary adenocarcinoma. Ann Thorac Surg. 2011;91(4):1051–7.
Nitadori J, Bograd AJ, Kadota K, Sima CS, Rizk NP, Morales EA, et al. Impact of micropapillary histologic subtype in selecting limited resection vs lobectomy for lung adenocarcinoma of 2cm or smaller. J Natl Cancer Inst. 2013;105(16):1212–20.
Wu J, Chen J, Lv X, Yang Q, Yao S, Zhang D, et al. Clinical value of serum and exhaled breath condensate inflammatory factor IL-11 levels in non-small cell lung cancer: Clinical value of IL-11 in non-small cell lung cancer. Int J Biol Markers. 2021;36(2):64–76.
Chen JL, Wu JN, Lv XD, Yang QC, Chen JR, Zhang DM. The value of red blood cell distribution width, neutrophil-to-lymphocyte ratio, and hemoglobin-to-red blood cell distribution width ratio in the progression of non-small cell lung cancer. PLoS ONE. 2020;15(8):e0237947.
Jiang C, Zhao M, Hou S, Hu X, Huang J, Wang H, et al. The indicative value of serum tumor markers for metastasis and stage of non-small cell lung cancer. Cancers (Basel). 2022;14(20):5064.
Moon Y, Choi SY, Park JK, Lee KY. Risk factors for occult lymph node metastasis in peripheral non-small cell lung cancer with invasive component size 3 cm or less. World J Surg. 2020;44(5):1658–65.
Liu S, Wang R, Zhang Y, Li Y, Cheng C, Pan Y, et al. Precise diagnosis of intraoperative frozen section is an effective method to guide resection strategy for peripheral small-sized lung adenocarcinoma. J Clin Oncol. 2016;34(4):307–13.
Su H, Xie H, Dai C, Zhao S, Xie D, She Y, et al. Procedure-specific prognostic impact of micropapillary subtype may guide resection strategy in small-sized lung adenocarcinomas: a multicenter study. Ther Adv Med Oncol. 2020;12:1758835920937893.
Yeh YC, Nitadori J, Kadota K, Yoshizawa A, Rekhtman N, Moreira AL, et al. Using frozen section to identify histological patterns in stage I lung adenocarcinoma of ≤ 3 cm: accuracy and interobserver agreement. Histopathology. 2015;66(7):922–38.
Koike T, Koike T, Yamato Y, Yoshiya K, Toyabe S. Predictive risk factors for mediastinal lymph node metastasis in clinical stage IA non-small-cell lung cancer patients. J Thorac Oncol. 2012;7(8):1246–51.
Ye B, Cheng M, Li W, Ge XX, Geng JF, Feng J, et al. Predictive factors for lymph node metastasis in clinical stage IA lung adenocarcinoma. Ann Thorac Surg. 2014;98(1):217–23.
Kanzaki R, Higashiyama M, Fujiwara A, Tokunaga T, Maeda J, Okami J, et al. Occult mediastinal lymph node metastasis in NSCLC patients diagnosed as clinical N0–1 by preoperative integrated FDG-PET/CT and CT: Risk factors, pattern, and histopathological study. Lung Cancer. 2011;71(3):333–7.
Farjah F, Lou F, Sima C, Rusch VW, Rizk NP. A prediction model for pathologic N2 disease in lung cancer patients with a negative mediastinum by positron emission tomography. J Thorac Oncol. 2013;8(9):1170–80.
Goksel S, Ozcelik N, Telatar G, Ardic C. The role of hematological inflammatory biomarkers in the diagnosis of lung cancer and in predicting TNM stage. Cancer Invest. 2021;39(6–7):514–20.
Xu F, Xu P, Cui W, Gong W, Wei Y, Liu B, et al. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios may aid in identifying patients with non-small cell lung cancer and predicting Tumor-Node-Metastasis stages. Oncol Lett. 2018;16(1):483–90.
Yip R, Li K, Liu L, Xu D, Tam K, Yankelevitz DF, et al. Controversies on lung cancers manifesting as part-solid nodules. Eur Radiol. 2018;28(2):747–59.
Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger K, Yatabe Y, et al. International association for the study of lung cancer/American Thoracic Society/European Respiratory Society: international multidisciplinary classification of lung adenocarcinoma: executive summary. Proc Am Thorac Soc. 2011;8(5):381–5.
Obuchowski NA, Bullen JA. Receiver operating characteristic (ROC) curves: review of methods with applications in diagnostic medicine. Phys Med Biol. 2018;63(7):07tr1.
Nattino G, Pennell ML, Lemeshow S. Assessing the goodness of fit of logistic regression models in large samples: a modification of the Hosmer-Lemeshow test. Biometrics. 2020;76(2):549–60.
Rosenfeld JP, Donchin E. Resampling (bootstrapping) the mean: a definite do. Psychophysiology. 2015;52(7):969–72.
Vickers AJ, Holland F. Decision curve analysis to evaluate the clinical benefit of prediction models. Spine J. 2021;21(10):1643–8.
Huang L, Li W, Zhao L, Li B, Chai Y. Risk factors of lymph node metastasis in lung squamous cell carcinoma of 3 cm or less in diameter. Medicine (Baltimore). 2017;96(29):e7563.
Haruki T, Wakahara M, Matsuoka Y, Miwa K, Araki K, Taniguchi Y, et al. Clinicopathological characteristics of lung adenocarcinoma with unexpected lymph node metastasis. Ann Thorac Cardiovasc Surg. 2017;23(4):181–7.
Xia W, Wang A, Jin M, Mao Q, Xia W, Dong G, et al. Young age increases risk for lymph node positivity but decreases risk for non-small cell lung cancer death. Cancer Manag Res. 2018;10:41–8.
Chen B, Wang X, Yu X, Xia WJ, Zhao H, Li XF, et al. Lymph node metastasis in Chinese patients with clinical T1 non-small cell lung cancer: A multicenter real-world observational study. Thorac Cancer. 2019;10(3):533–42.
Shafazand S, Gould MK. A clinical prediction rule to estimate the probability of mediastinal metastasis in patients with non-small cell lung cancer. J Thorac Oncol. 2006;1(9):953–9.
Zhang Y, Sun Y, Xiang J, Zhang Y, Hu H, Chen H. A prediction model for N2 disease in T1 non-small cell lung cancer. J Thorac Cardiovasc Surg. 2012;144(6):1360–4.
Zhang Y, Sun Y, Shen L, Li Y, Xiang J, Zhang Y, et al. Predictive factors of lymph node status in small peripheral non-small cell lung cancers: tumor histology is more reliable. Ann Surg Oncol. 2013;20(6):1949–54.
Li X, Zhang H, Xing L, Xu X, Xie P, Ma H, et al. Predictive value of primary fluorine-18 fluorodeoxyglucose standard uptake value for a better choice of systematic nodal dissection or sampling in clinical stage ia non–small-cell lung cancer. Clin Lung Cancer. 2013;14(5):568–73.
Sakao Y, Nakazono T, Sakuragi T, Natsuaki M, Itoh T. Predictive factors for survival in surgically resected clinical IA peripheral adenocarcinoma of the lung. Ann Thorac Surg. 2004;77(4):1157–61 (discussion 61-2).
Yanagitani N, Kaira K, Sunaga N, Naito Y, Koike Y, Ishihara S, et al. Serum amylase is a sensitive tumor marker for amylase-producing small cell lung cancer? Int J Clin Oncol. 2007;12(3):231–3.
Minami S, Komuta K, Asai M. A case of amylase-producing lung cancer. Nihon Kokyuki Gakkai Zasshi. 2003;41(10):717–21.
Tsukawaki M, Izawa M, Yoshida M, Araki N, Hashiba Y, Nakagawa H, et al. A case of amylase-producing lung cancer. Intern Med. 1992;31(1):60–3.
Zhu J, Xu WG, Xiao H, Zhou Y. Application of a radiomics model for preding lymph node metastasis in non-small cell lung cancer. Sichuan Da Xue Xue Bao Yi Xue Ban. 2019;50(3):373–8.
Liang Z, Wang HF, Wu AZ, Cai JH. Clinical value of multi-tumor markers protein biochip in the diagnosis of pulmonary carcinoma. Nan Fang Yi Ke Da Xue Xue Bao. 2010;30(11):2516–8.
Consorti F, Lorenzotti A, Midiri G, Di Paola M. Prognostic significance of mucinous carcinoma of colon and rectum: a prospective case-control study. J Surg Oncol. 2000;73(2):70–4.
Enciu M, Aşchie M, Deacu M, Poinăreanu I. Morphological characteristics of a mucinous adenocarcinoma of the prostate: differential diagnosis considerations. Rom J Morphol Embryol. 2013;54(1):191–4.
Kunisaki C, Akiyama H, Nomura M, Matsuda G, Otsuka Y, Ono HA, et al. Clinicopathologic characteristics and surgical outcomes of mucinous gastric carcinoma. Ann Surg Oncol. 2006;13(6):836–42.
Kawamura H, Kondo Y, Osawa S, Nisida Y, Okada K, Isizu H, et al. A clinicopathologic study of mucinous adenocarcinoma of the stomach. Gastric Cancer. 2001;4(2):83–6.
Beatty PL, Narayanan S, Gariépy J, Ranganathan S, Finn OJ. Vaccine against MUC1 antigen expressed in inflammatory bowel disease and cancer lessens colonic inflammation and prevents progression to colitis-associated colon cancer. Cancer Prev Res (Phila). 2010;3(4):438–46.
Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6(2):244–85.
Travis WD, Brambilla E, Riely GJ. New pathologic classification of lung cancer: relevance for clinical practice and clinical trials. J Clin Oncol. 2013;31(8):992–1001.
Cadranel J, Quoix E, Baudrin L, Mourlanette P, Moro-Sibilot D, Morere JF, et al. IFCT-0401 Trial: a phase II study of gefitinib administered as first-line treatment in advanced adenocarcinoma with bronchioloalveolar carcinoma subtype. J Thorac Oncol. 2009;4(9):1126–35.
Russell PA, Wainer Z, Wright GM, Daniels M, Conron M, Williams RA. Does lung adenocarcinoma subtype predict patient survival?: a clinicopathologic study based on the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary lung adenocarcinoma classification. J Thorac Oncol. 2011;6(9):1496–504.
Lee HY, Cha MJ, Lee KS, Lee HY, Kwon OJ, Choi JY, et al. Prognosis in resected invasive mucinous adenocarcinomas of the lung: related factors and comparison with resected nonmucinous adenocarcinomas. J Thorac Oncol. 2016;11(7):1064–73.
Kadota K, Yeh YC, D’Angelo SP, Moreira AL, Kuk D, Sima CS, et al. Associations between mutations and histologic patterns of mucin in lung adenocarcinoma: invasive mucinous pattern and extracellular mucin are associated with KRAS mutation. Am J Surg Pathol. 2014;38(8):1118–27.
Kakegawa S, Shimizu K, Sugano M, Miyamae Y, Kaira K, Araki T, et al. Clinicopathological features of lung adenocarcinoma with KRAS mutations. Cancer. 2011;117(18):4257–66.
Pang Z, Liu H, Chen Z, Zhu L. Establishment and validation of a novel nomogram for predicting distant metastasis in patients with invasive lung adenocarcinoma. J Coll Physicians Surg Pak. 2022;32(12):1563–9.
Tatnell PJ, Powell DJ, Hill J, Smith TS, Tew DG, Kay J. Napsins: new human aspartic proteinases. Distinction between two closely related genes. FEBS Lett. 1998;441(1):43–8.
Mori K, Kon Y, Konno A, Iwanaga T. Cellular distribution of napsin (kidney-derived aspartic protease-like protein, KAP) mRNA in the kidney, lung and lymphatic organs of adult and developing mice. Arch Histol Cytol. 2001;64(3):319–27.
Bishop JA, Sharma R, Illei PB. Napsin A and thyroid transcription factor-1 expression in carcinomas of the lung, breast, pancreas, colon, kidney, thyroid, and malignant mesothelioma. Hum Pathol. 2010;41(1):20–5.
Ueno T, Linder S, Elmberger G. Aspartic proteinase napsin is a useful marker for diagnosis of primary lung adenocarcinoma. Br J Cancer. 2003;88(8):1229–33.
Stoll LM, Johnson MW, Gabrielson E, Askin F, Clark DP, Li QK. The utility of napsin-A in the identification of primary and metastatic lung adenocarcinoma among cytologically poorly differentiated carcinomas. Cancer Cytopathol. 2010;118(6):441–9.
Turner BM, Cagle PT, Sainz IM, Fukuoka J, Shen SS, Jagirdar J. Napsin A, a new marker for lung adenocarcinoma, is complementary and more sensitive and specific than thyroid transcription factor 1 in the differential diagnosis of primary pulmonary carcinoma: evaluation of 1674 cases by tissue microarray. Arch Pathol Lab Med. 2012;136(2):163–71.
Agackiran Y, Ozcan A, Akyurek N, Memis L, Findik G, Kaya S. Desmoglein-3 and Napsin A double stain, a useful immunohistochemical marker for differentiation of lung squamous cell carcinoma and adenocarcinoma from other subtypes. Appl Immunohistochem Mol Morphol. 2012;20(4):350–5.
Camilo R, Capelozzi VL, Siqueira SA, Del Carlo BF. Expression of p63, keratin 5/6, keratin 7, and surfactant-A in non-small cell lung carcinomas. Hum Pathol. 2006;37(5):542–6.
Downey P, Cummins R, Moran M, Gulmann C. If it’s not CK5/6 positive, TTF-1 negative it’s not a squamous cell carcinoma of lung. APMIS. 2008;116(6):526–9.
Loo PS, Thomas SC, Nicolson MC, Fyfe MN, Kerr KM. Subtyping of undifferentiated non-small cell carcinomas in bronchial biopsy specimens. J Thorac Oncol. 2010;5(4):442–7.
Acknowledgements
Not applicable.
Funding
This work was funded by National Key Research and Development Program (2021YFC2500904, and 2021YFC2500905) and Natural Science Foundation of Shandong Province (ZR2021LSW006).
Author information
Authors and Affiliations
Contributions
Conceptualization, HT and MX. Methodology, MX. Software, MX. Validation, ML. and MX. Formal analysis, MX. Investigation, ZL and JL. Resources, ZL and JL. Data curation, WL and HZ. Writing—original draft preparation, MX. Writing—review and editing, MX and ML. Visualization, MX and HT. Supervision, HT. Project administration, HT. All authors contributed to the article and approved the submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Qilu Hospital, Shandong University (registration number: KYLL-202008–023-1), and all patients signed an informed consent form for the use of their clinical information prior to the procedure. All methods were performed in accordance with the Declaration of Helsinki.
Consent for publication
NA.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xue, M., Liu, J., Li, Z. et al. The role of adenocarcinoma subtypes and immunohistochemistry in predicting lymph node metastasis in early invasive lung adenocarcinoma. BMC Cancer 24, 139 (2024). https://doi.org/10.1186/s12885-024-11843-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-11843-4