Abstract
Background
The combinations of PD-1 inhibitors with paclitaxel/cisplatinum (PD-1 + TP) and fluoropyrimidine/cisplatinum (PD-1 + FP) both have been shown to improve overall survival (OS) and progression-free survival (PFS) in patients with previously untreated, advanced esophageal squamous cell carcinoma (ESCC). However, there is no consensus on which chemotherapy regimen combined with PD-1 has better efficacy. To deal with this important issue in the first-line treatment of patients with ESCC, a network meta-analysis (NMA) was performed.
Methods
Data were collected from eligible studies searched in Medline, Web of Science, PubMed, the Cochrane Library and Embase. The pooled hazard ratio (HR) for the OS, and PFS, odds ratio (OR) for the objective response rate (ORR) and ≥ 3 grade treatment-related adverse events (≥ 3TRAEs) were estimated to evaluate the efficacy of PD-1 inhibitors combined with TP or FP.
Results
Five RCTs and one retrospective study involving 3685 patients and evaluating four treatments were included in this NMA. Compared to other treatments, PD-1 + TP was better. For the PFS, the HRs for PD-1 + TP compared to PD-1 + FP, TP and FP were 0.59 (0.44, 0.80), 0.56 (0.51, 0.61) and 0.45 (0.37, 0.56) respectively. For the OS, PD-1 + TP was also a better treatment compared to other treatments. The HRs were 0.74 (0.56, 0.96), 0.64 (0.57, 0.71), 0.53 (0.43, 0.67) respectively. For the ORR, there was no significant difference between PD-1 + TP and PD-1 + FP, and the ORs were 1.2 (0.69, 2.11). Compare with TP and FP, PD-1 + TP had an obvious advantage, ORs were 2.5 (2.04, 3.04) and 2.95 (1.91, 4.63). For ≥ 3TRAEs, PD-1 + TP compared to other treatments, ORs were 1.34 (0.74, 2.46) and 1.13 (0.92, 1.38) and 2.23 (1.35, 3.69).
Conclusion
PD-1 + TP significantly improved both PFS and OS compared to PD-1 + FP. Taking into account both efficacy and safety, PD-1 + TP may be a superior first-line treatment option for ESCC.
Similar content being viewed by others
Introduction
Esophageal cancer, with its high incidence and poor prognosis, is the seventh most common cancer and sixth leading cause of cancer death worldwide [1], with a 5-year survival rate of approximately 15%-20% [2]. Overall survival (OS) is less than one year if advanced esophageal cancer is detected [3, 4]. However, esophageal squamous cell carcinoma (ESCC) is not listed separately in major guidelines. Like adenocarcinoma, fluoropyrimidine and cisplatinum (FP) regimens are recommended as first-line treatment [5, 6]. In Asia, ESCC is a more common pathological type. Some studies have compared the efficacy of paclitaxel-based regimen and fluorouracil-based regimen in ESCC [7,8,9,10], but there is no consistent conclusion. In the era of immunotherapy, clinical studies have proved that chemotherapy combined with immune checkpoint inhibitors (PD-1 inhibitors) can confer greater benefit to patients with esophageal cancer than chemotherapy alone, especially in ESCC. For the first-line treatment of ESCC, FP or paclitaxel and cisplatin (TP) were selected as the chemotherapy regimen combined with PD1 inhibitors in different randomized controlled trials (RCTs) [4, 11,12,13,14]. However, for FP or TP, which regimen is more suitable for first-line treatment, and whether immunotherapy combined with different chemotherapy schemes has different efficacies, there is no direct comparative study. Thus, the value of pairwise meta-analysis is limited. Meta-analysis, which compares the advantages and disadvantages of multiple treatments simultaneously, is a better method of analysis [15]. Therefore, in the present study, NMA was performed to propose a better treatment plan in the first-line treatment of patients with ESCC.
Methods
Search strategy
We conducted a comprehensive search of Medline, Web of Science, Pubmed, the Cochrane Library and Embase databases up to April 2023. In addition, we systematically reviewed all abstracts from the American Society of Clinical Oncology (ASCO) and the European Society of Medical Oncology (ESMO) Congress between 2012 and 2023. Our search strategy was designed to identify published randomized controlled trials that evaluated first-line treatment options for patients with esophageal cancer.
Selection criteria
All RCTs assessing first-line treatments for esophageal cancer were included in this systematic review, without any restrictions on publication date, location or language. Eligible studies had to meet the following criteria: 1) prospective phase III randomized controlled trials; 2) included patients with metastatic, unresectable, or recurrent squamous of the esophagus; 3) first-line treatment setting; 4) compared at least two arms that consisted of the following agents: FP(5-fluorouracil, cisplatin), TP (paclitaxel, cisplatin), and PD-1 inhibitors.
Data extraction and quality assessment
Two authors (Zhao and Zhang) independently scrutinized the titles and abstracts of retrieved RCTs. They reviewed the full texts of selected RCTs to evaluate eligibility criteria for inclusion in NMA, extracted study characteristics and outcome data. Qu resolved any disagreements between the authors if necessary.
The Cochrane tools were utilized to evaluate the quality and risk of bias. HRs with their corresponding 95% CI for PFS and OS were extracted from various studies, while OR and its 95% CI were employed to indicate the frequencies of ORR. In cases where data on HR and its 95% CI could not be obtained, Kaplan–Meier curves were digitized using Engauge Digitizer (www.digitizer.sourceforge.net) followed by hazard ratio calculation in R.
Statistical analysis
Pairwise meta-analyses were conducted using the JAGS ‘Gemtc’ package in R software (version 4.0.3) [16, 17]. Heterogeneity among studies was evaluated by means of the Q test and I2 statistic [18]. The fixed-effect or random-effects model was selected based on the value of I2 (< 50% or > 50%, respectively). Results from pairwise meta-analysis were presented as HR with 95% CI for OS and PFS, and as OR with 95% CI for ORR and ≥ 3TRAEs. Network plots were generated using R (version 4.0.3) to compare different treatments and depict network geometry. Network meta-analysis (NMA) was performed under the Bayesian framework using JAGS and the "gemtc" package in R [17]. Both random effects and consistency models were utilized in NMA, with four independent Markov chains automatically generated for posterior distribution estimation through 5000 adaptation iterations and 20,000 inference iterations per chain.Run lengths were extended if the Brooks-Gelman-Rubin diagnostic or time series plots indicated that the Markov chains had not converged (Supplementary Fig. 2). The NMA results were presented as HRs with 95% credible intervals (CIs) for OS and DFS, and ORs with 95% CIs for ORR and ≥ 3TRAEs. The probability of each treatment regarding survival outcomes was ranked according to the HRs and the posterior probabilities. Two-sided p < 0·05 indicates statistical significance.
Consistency, global inconsistency assessment, and local inconsistency assessment were conducted to evaluate the study. The evaluation of global inconsistency was based on comparing the fit of consistency and inconsistency models using deviance information criterion (DIC). Similar DIC values among different models indicate good consistency [19, 20]. The local inconsistency was evaluated through comparing the direct and indirect evidence generated under the Bayesian framework using the node-splitting analysis, where p < 0·05 indicates significant inconsistency [21].
Results
Description of selected trials
Eventually, after screening 1786 articles, only five RCTs met the eligibility criteria for this network meta-analysis (NMA) [4, 11,12,13,14] (Fig. 1). However, due to the inability to compare treatments simultaneously in a network among these RCTs, we identified a retrospective control study during our search that could link RCTs to a network and provide data on PFS, OS, ORR, and ≥ 3TRAEs [22]. Therefore, this study was included in our NMA. All clinical trials included in the present meta-analysis are listed in Table 1. A total of 3360 subjects were included, all of them received first-line treatment. Four treatment regimens (PD-1 + TP, PD-1 + FP, TP, FP) were included. KEYNOTE-590 and CheckMate-648 were compared with PD-1 + FP and FP. In KEYNOTE-590, the eligible patients had “unresectable or metastatic adenocarcinoma or squamous cell carcinoma of the esophagus or Siewert type 1 gastro-esophageal junction adenocarcinoma” [11]. In this NMA, only the squamous cell sub-group was included. CheckMate-648 included three arms, among which, the third arm (I + P) did not meet the standards, so was not included. The comparison between PD-1 + TP and TP was conducted via Escort1-st and JUPITER06 studies. In Orient-15, TP was administered as the base-line regimen to 94.5% of subjects. Therefore, the two arms of Orient-15 were considered PD-1 + TP and TP in this NMA. The hazard ratios (HRs) for the PFS and OS were not reported by Liu Y and Ren Z. The Kaplan–Meier curves were digitized using Engauge Digitizer (www.digitizer.sourceforge.net), and HRs were calculated in R. The OS and PFS were analyzed across all six trials, while only five trials were included for the ORR and ≥ 3TRAEs. Data on the ORR in the squamous subgroup were not provided in Keynote590.
Risk of bias and heterogeneity assessment
The primary outcome was the OS, while secondary endpoints included the PFS, ORR and ≥ 3TRAEs. Study quality was assessed using the Cochrane Risk of Bias tool, version 5.1.0, with items scored as low, high or unknown risk of bias. Based on I2 < 50%, there was no significant heterogeneity observed among the trials in the network.
Results of NMA and ranking of treatments
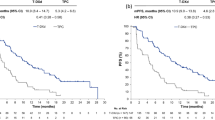
A network consisting of four treatments, namely PD-1 + TP, PD-1 + FP, TP, and FP (Fig. 2), was established. The results of the comparison among all treatments are summarized in Table 2. Given that there was no statistical heterogeneity in this network (I2 = 0%), a fixed effects model was adopted to report the findings. In terms of PFS, PD-1 + TP demonstrated superior efficacy compared with other treatments. The HRs for PD-1 + TP compared to PD-1 + FP, TP and FP were 0.59 (95% confidence interval [CI]: 0.44–0.80), 0.56 (95% CI: 0.51–0.61), and 0.45 (95% CI: 0.37–0.56), respectively (Table 2A). In terms of the OS, PD-1 + TP exhibited superior efficacy compared to other treatments. The HRs for PD-1 + TP compared to PD-1 + FP, TP and FP were 0.74 (95% CI: 0.56, 0.96), 0.64 (95% CI: 0.57, 0.71), 0.53 (95% CI: 0.43, 0.67) respectively (Table 2A). Due to the lack of data on the ORR in the squamous subgroup in Keynote590, only five trials were included for analysis of the ORR and ≥ 3TRAEs (Supplementary Fig. 1). No significant difference in the ORR was observed between PD-1 + TP and PD-1 + FP, as indicated by RRs of 1.2 (95% CI:0.69, 2.11). However, PD-1 + TP showed a significant advantage over TP and FP with ORs of 2.5 (95% CI: 2.04, 3.04) and 2.95 (95% CI: 1.91, 4.63), respectively (Table 2B). For security, PD-1 + TP had no significant difference with PD-1 + FP and TP, ORs of ≥ 3TRAEs were 0.75(95% CI:0.41,1.4) and 0.89(95% CI:0.73, 1.1). The results suggest that FP may have had superior security, with an OR of 2.23 (1.35, 3.69) (Table 2B). Forest plots were generated to visualize the network estimates (Fig. 3).
Network of all treatment comparisons for the OS and PFS. The lines connect the regimens that were directly compared in clinical trails. The thickness of the lines corresponds to the number of RCTs. PD-1: Programmed death receptor 1 inhibitors; TP: Paclitaxel plus cis-platinum; FP: fluorouracil plus cis-platinum
Forest plots of all individual regimens compared with PD1 + TP. HRs and 95% credible intervals are given. A PFS of all individual regimens compared with PD1 + TP; B OSs of all individual regimens compared with PD1 + TP; C ORRs of all individual regimens compared with PD1 + TP; D ≥ 3TRAEs of all individual regimens compared with PD1 + TP
Discussion
Causes of distinct variations in the risk factors, incidence and distribution worldwide between both histological types of esophageal cancer are multifaceted [23]. Extensive clinical trials in western nations have primarily focused on patients with adenocarcinoma of the esophagus, and fluorouracil-based chemotherapy has been recommended for esophageal adenocarcinoma [24]. With the advancement of research of esophageal cancer, it has become evident that ESCC and adenocarcinoma are two distinct diseases. Currently, more clinical trials are focusing on ESCC, particularly in the “esophageal cancer belt”, which includes parts of northern Iran, southern Russia, central Asian countries, and northern China where squamous cell cancers account for up to 90% of all cases [25]. Paclitaxel combined with cisplatin is a widely used therapeutic regimen for ESCC in China. In a clinical investigation by Zhang L., the combination of paclitaxel and platinum showed improved survival rates during the postoperative adjuvant treatment of ESCC. Compared with the control group, the 3-year DFS rates were 56.3% v. 34.6% (P = 0.006). The 3-year OS rates were 55.0% v. 37.5% (P = 0.013) [26]. In a study by Kim J.Y., patients with advanced ESCC were treated with paclitaxel plus platinum. The median PFS was 5.0 months and median survival was 8.3 months, and the objective tumor response rate was 33.3%. TP is a standard chemotherapy regimen for first-line treatment of ESCC. In other types of squamous cell carcinomas, such as head and neck or lung cancer, anti-microtubule drugs are also recommended as a priority [27].
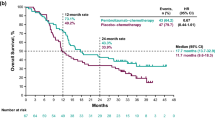
In the era of immunotherapy, PD-1 combined chemotherapy has demonstrated superior efficacy compared to traditional chemotherapy in various tumors, particularly non-small-cell lung cancer [28]. Recently, the use of immunotherapy in esophageal cancer has been increasingly promoted from second-line to first-line treatment. Significant benefits were observed with PD-1 + FP compared to FP in both KEYNOTE-590 and CheckMate-648 trials. In the KEYNOTE-590 trial, pembrolizumab plus chemotherapy exhibited a superior OS of 12.4 months compared to placebo-chemotherapy with an OS of 9.8 months (p < 0.0001) among all randomized patients; in the ESCC subgroup, the OS was also significantly improved at 12.6 months v. 9.8 months (p = 0.0006). Additionally, the PFS was prolonged from 5.8 months to 6.3 months (p = 0.0001).
In the CheckMate-648 study, the overall population demonstrated a significantly longer OS with nivolumab plus FP compared to FP alone (13.2 months v. 10.7 months; P = 0.002). Three additional RCTs, ESCORT1st, JUPITER06, and ORIENT05, initiated by Chinese scholars also confirmed that PD-1 combined with chemotherapy provided greater benefits than chemotherapy alone in first-line treatment of ESCC. The results of all three studies proved that the benefits of combining PD-1 with chemotherapy were significantly greater than those of chemotherapy alone, as evidenced by an OS rate of 15.3 months v. 12 months, 17 months v. 11 months, and 16.7 months v. 12.5 months respectively. Furthermore, the safety profile was comparable.
Immunotherapy combined with chemotherapy is recommended as first-line treatment of ESCC by the aforementioned RCTs. Notably, in studies comparing PD-1 + TP to TP (ESCORT1st, JUPITER06, ORIENT 05), the experimental groups demonstrated an OS of 15–17 months; however, in RCTs comparing PD-1 + FP to FP (KEYNOTE-590 and CheckMate-648), the experimental groups exhibited an OS ranging from 10–13 months. Could the differential effect be attributed to the combination of immunotherapy with different chemotherapy regimens? As there has been no head-to-head comparison between PD-1 + TP and PD-1 + FP, we designed a NMA to compare which chemotherapy combined with PD-1 is more beneficial in the first-line treatment of ESCC.
In this NMA, PD-1 + TP exhibited improved survival compared to PD-1 + FP. Previous studies have suggested a stronger synergistic effect between paclitaxel and immunotherapy. The mechanism can be explained by the fact that paclitaxel exhibits a stronger ability to enhance immunogenicity of cell death, thereby shaping a more favorable inflammatory immune microenvironment and promoting activation of immune cells through release of various proinflammatory cytokines by tumor cells; when combined with PD-1, it may achieve better synergistic effects [29,30,31,32].
The primary indications of esophageal cancer patients are progressive dysphagia and retrosternal pain, with malnutrition frequently resulting from the former and negatively impacting prognosis [33]. Achieving superior disease control rates is particularly crucial in treating this condition. In ESCORT-1st, the ORR for PD-1 + TP was 72.1%, while CheckMate-648 saw an ORR of 47% for PD-1 + FP. In terms of numerical values, there was a significant gap between the two regimens; however, this NMA found no statistical difference in ORRs between PD-1 + TP and PD-1 + FP, which may be attributed to the limited number of studies included in the analysis of ORR. As a potentially superior alternative, PD-1 + TP has been extensively investigated in neoadjuvant treatments for ESCC, including KEYSTONE-001 [34] (MPR 72.4%) and ESPRIT (ORR 66.67%) [35]. These studies have demonstrated high response rates with the use of PD-1 + TP. However, further RCTs are necessary to provide more compelling evidence.
Limitations: some limitations of this NMA should be acknowledged. In the five RCTs involved in this NMA, the group of ESCC with highly expressed PD-L1 had a more benefit from PD-1 plus chemotherapy, but subgroups defined were different. Some limitations of this NMA must be acknowledged: although the group with high PD-L1 expression in ESCC benefited more from PD-1 plus chemotherapy in the five RCTs included, but in this NMA, we found that there were differences in subgroup definitions. CheckMate-648 defined subgroups according to the tumor cell PD-L1 expression of 1% or greater, but KEYNOTE-590 and ORIENT-15 subgroups were defined by CPS ≥ 10. In ESCORT-1st analysis the three different selected PD-L1 expressions were classified into subgroups (TPS ≥ 10, TPS ≥ 1, TPS < 1): regardless of the PD-L1 expression level, patients can benefit from combination immunotherapy. JUPITER 06 did not set subgroups for different PD-L1 expressions, but the analysis incorporated all randomized patients in toto. Therefore, this MNA could not perform subgroup analysis based on the level of expression of PD-L1.
Conclusion
Based on the findings of this NMA, it appears that the combination therapy of TP and PD-1 inhibitors is a superior first-line treatment option for ESCC. Further RCTs are warranted to optimize first-line treatment strategies and generate evidence-based medicine.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- NMA:
-
Network Meta-analysis
- ESCC:
-
Esophageal Squamous Cell Carcinoma
- RCTs:
-
Randomized Controlled Trials
- TRAEs:
-
Treatment-related Adverse Events
- OS:
-
Overall Survival
- PFS:
-
Progression-free Survival
- HR:
-
Hazard Ratio
- ORR:
-
Objective Response Rate
- DIC:
-
Deviance Information Criterion
- PD-1 + TP:
-
PD-1 Inhibitors with Paclitaxel/Cisplatinum
- PD-1 + FP:
-
PD-1 Inhibitors with Fluoropyrimidine/Cisplatinum
- FP:
-
Fluoropyrimidine and Cisplatinum
- TP:
-
Paclitaxel and Cisplatinum
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660. Epub 2021 Feb 4 PMID: 33538338.
Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381(9864):400–12. https://doi.org/10.1016/S0140-6736(12)60643-6. PMID: 23374478.
Moehler M, Maderer A, Thuss-Patience PC, Brenner B, Meiler J, Ettrich TJ, et al. Cisplatin and 5-fluorouracil with or without epidermal growth factor receptor inhibition panitumumab for patients with non-resectable, advanced or metastatic oesophageal squamous cell cancer: a prospective, open-label, randomised phase III AIO/EORTC trial (POWER). Ann Oncol. 2020;31(2):228–35. https://doi.org/10.1016/j.annonc.2019.10.018. Epub 2019 Dec 16. PMID: 31959339.
Luo H, Lu J, Bai Y, Mao T, Wang J, Fan Q, et al. ESCORT-1st investigators. Effect of Camrelizumab vs Placebo added to Chemotherapy on Survival and Progression-Free Survival in patients with Advanced or metastatic esophageal squamous cell carcinoma: the ESCORT-1st Randomized Clinical Trial. JAMA. 2021;326(10):916–25. https://doi.org/10.1001/jama.2021.12836. PMID: 34519801; PMCID: PMC8441593.
Waddell T, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D. Gastric cancer: ESMO-ESSO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Eur J Surg Oncol. 2014;40(5):584–91. https://doi.org/10.1016/j.ejso.2013.09.020. PMID: 24685156.
Ajani JA, Bentrem DJ, Besh S, D’Amico TA, Das P, Denlinger C, et al. National Comprehensive Cancer Network. Gastric cancer, version 2.2013: featured updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2013;11(5):531–46. https://doi.org/10.6004/jnccn.2013.0070. PMID: 23667204.
Dröge LH, Karras PJ, Guhlich M, Schirmer MA, Ghadimi M, Rieken S, Conradi LC, Leu M. Preoperative radiochemotherapy in esophageal squamous cell Cancer with 5-Fluorouracil/Cisplatin or Carboplatin/Paclitaxel: treatment practice over a 20-Year period and implications for the Individual Treatment Modalities. Cancers (Basel). 2021;13(8):1834. https://doi.org/10.3390/cancers13081834. PMID: 33921384; PMCID: PMC8068912.
Su PH, Hsueh SW, Tseng CK, Ho MM, Su PJ, Hung CY, Yeh KY, Chang PH, Hung YS, Ho YW, Lin YC, Chou WC. Paclitaxel and Carboplatin Versus Cisplatin and 5-Fluorouracil in concurrent chemoradiotherapy in patients with Esophageal Cancer. In Vivo. 2021;35(6):3391–9. https://doi.org/10.21873/invivo.12638. PMID: 34697174; PMCID: PMC8627782.
Hu G, Wang Z, Wang Y, Zhang Q, Tang N, Guo J, Liu L, Han X. Comparison of cisplatinum/paclitaxel with cisplatinum/5-fluorouracil as first-line therapy for nonsurgical locally advanced esophageal squamous cell carcinoma patients. Drug Des Devel Ther. 2016;10:2129–36. https://doi.org/10.2147/DDDT.S105441. PMID: 27445460; PMCID: PMC4936807.
Xu L, Chen X, Wang L, Han J, Wang Q, Liu S, Zhang X, Han C. Paclitaxel combined with platinum (PTX) versus fluorouracil combined with cisplatin (PF) in the treatment of unresectable Esophageal cancer: a systematic review and meta-analysis of the efficacy and toxicity of two different regimens. J Gastrointest Oncol. 2023;14(2):1037–51. https://doi.org/10.21037/jgo-23-33. Epub 2023 Apr 12. PMID: 37201087; PMCID: PMC10186517.
Sun JM, Shen L, Shah MA, Enzinger P, Adenis A, Doi T, et al. KEYNOTE-590 Investigators. Pembrolizumab plus chemotherapy versus chemotherapy alone for first-line treatment of advanced oesophageal cancer (KEYNOTE-590): a randomised, placebo-controlled, phase 3 study. Lancet. 2021;398(10302):759–71. https://doi.org/10.1016/S0140-6736(21)01234-4. Erratum. In: Lancet. 2021;398(10314):1874 PMID: 34454674.
Doki Y, Ajani JA, Kato K, Xu J, Wyrwicz L, Motoyama S, et al. CheckMate 648 Trial Investigators. Nivolumab Combination Therapy in Advanced Esophageal Squamous-Cell Carcinoma. N Engl J Med. 2022;386(5):449–62. https://doi.org/10.1056/NEJMoa2111380. PMID: 35108470.
Wang ZX, Cui C, Yao J, Zhang Y, Li M, Feng J, et al. Toripalimab plus chemotherapy in treatment-naïve, advanced esophageal squamous cell carcinoma (JUPITER-06): A multi-center phase 3 trial. Cancer Cell. 2022;40(3):277-288.e3. https://doi.org/10.1016/j.ccell.2022.02.007. Epub 2022 Mar 3 PMID: 35245446.
Lu Z, Wang J, Shu Y, Liu L, Kong L, Yang L, ORIENT-15 study group, et al. Sintilimab versus placebo in combination with chemotherapy as first line treatment for locally advanced or metastatic oesophageal squamous cell carcinoma (ORIENT-15): multicentre, randomised, double blind, phase 3 trial. BMJ. 2022;377:e068714. https://doi.org/10.1136/bmj-2021-068714. PMID: 35440464; PMCID: PMC9016493.
Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;331(7521):897–900. https://doi.org/10.1136/bmj.331.7521.897. PMID: 16223826; PMCID: PMC1255806.
Dias S, Sutton AJ, Ades AE, et al. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network metaanalysis of randomized controlled trials. Med Decis Making. 2013;33(5):607–17.
van Valkenhoef G, Lu G, de Brock B, et al. Automating network meta-analysis. Res Synth Methods. 2012;3(4):285–99.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557. PMID: 12958120; PMCID: PMC192859.
Lu G, Ades AE. Assessing evidence inconsistency in mixed treatment comparisons. J Am Stat Assoc. 2006;101:447–59. https://doi.org/10.1198/016214505000001302.
Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. National Institute for Health and Care Excellence (NICE); London: 2014. NICE DSU technical support document 4: inconsistency in networks of evidence based on randomised controlled trials.
van Valkenhoef G, Dias S, Ades AE, Welton NJ. Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res Synth Methods. 2016;7(1):80–93. https://doi.org/10.1002/jrsm.1167. Epub 2015 Oct 13. PMID: 26461181; PMCID: PMC5057346.
Liu Y, Ren Z, Yuan L, Xu S, Yao Z, Qiao L, Li K. Paclitaxel plus Cisplatin vs. 5-fluorouracil plus cisplatin as first-line treatment for patients with advanced squamous cell Esophageal cancer. Am J Cancer Res. 2016;6(10):2345–50 PMID: 27822423; PMCID: PMC5088297.
Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of Esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13(6):1010–21. https://doi.org/10.1007/s12328-020-01237-x. Epub 2020 Sep 23. PMID: 32965635.
Ajani JA, D’Amico TA, Bentrem DJ, Chao J, Corvera C, Das P, et al. Esophageal and Esophagogastric Junction Cancers, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2019;17(7):855–83. https://doi.org/10.6004/jnccn.2019.0033. PMID: 31319389.
Alsop BR, Sharma P. Esophageal Cancer. Gastroenterol Clin North Am. 2016;45(3):399–412. https://doi.org/10.1016/j.gtc.2016.04.001. PMID: 27546839.
Li H, Fang Y, Gu D, Du M, Zhang Z, Sun L, et al. Paclitaxel and cisplatin combined with concurrent involved-field irradiation in definitive chemoradiotherapy for locally advanced esophageal squamous cell carcinoma: a phase II clinical trial. Radiat Oncol. 2022;17(1):105. https://doi.org/10.1186/s13014-022-02078-3. PMID: 35681233; PMCID: PMC9185874.
Zhu L, Chen L. Progress in research on paclitaxel and Tumor immunotherapy. Cell Mol Biol Lett. 2019;24:40. https://doi.org/10.1186/s11658-019-0164-y. PMID: 31223315; PMCID: PMC6567594.
Rodríguez-Abreu D, Powell SF, Hochmair MJ, Gadgeel S, Esteban E, Felip E, et al. Pemetrexed plus platinum with or without pembrolizumab in patients with previously untreated metastatic nonsquamous NSCLC: protocol-specified final analysis from KEYNOTE-189. Ann Oncol. 2021;32(7):881–95. https://doi.org/10.1016/j.annonc.2021.04.008. Epub 2021 Apr 22. PMID: 33894335.
Fong A, Durkin A, Lee H. The potential of combining tubulin-targeting Anticancer therapeutics and Immune Therapy. Int J Mol Sci. 2019;20(3) PMID: 30704031; PMCID: PMC6387102.
Galluzzi L, Humeau J, Buqué A, et al. Immunostimulation with chemotherapy in the era of immune checkpoint inhibitors[J]. Nat Rev Clin Oncol. 2020;17(12):725–41.
GARNETT C T, SCHLOM J, HODGE JW. Combination of docetaxel and recombinant vaccine enhances T-cell responses and antitumor activity: effects of docetaxel on immune enhancement. Clin Cancer Res. 2008;14(11):3536–44.
Pfannenstiel LW, Lam SS, Emens LA, et al. Paclitaxel enhances early dendritic cell maturation and function through TLR4 signaling in mice[J]. Cell Immunol. 2010;263(1):79–87.
Okada G, Matsumoto Y, Habu D, Matsuda Y, Lee S, Osugi H. Relationship between GLIM criteria and disease-specific symptoms and its impact on 5-year survival of Esophageal cancer patients. Clinical Nutrition. 2021;40(9):5072–8. https://doi.org/10.1016/j.clnu.2021.08.008.
Shang X, Zhao G, Liang F, Zhang C, Zhang W, Liu L, et al. Safety and effectiveness of pembrolizumab combined with paclitaxel and cisplatin as neoadjuvant therapy followed by Surgery for locally advanced resectable (stage III) esophageal squamous cell carcinoma: a study protocol for a prospective, single-arm, single-center, open-label, phase-II trial (Keystone-001). Ann Transl Med. 2022;10(4):229. https://doi.org/10.21037/atm-22-513. PMID: 35280363; PMCID: PMC8908169.
Retrieved, May. 17, 2022. from https://www.prnasia.com/story/361640-1.shtml.
Acknowledgements
The authors would like to acknowledge the Key Laboratory of Precision Diagnosis and Treatment of Gastrointestinal Tumors, Ministry of Education (China Medical University, Shenyang, China) for providing the space and equipment for conducting the experiments.
Funding
This work was supported by Scientist partner between China Medical University and Shenyang Branch of Chinese Academy of Sciences project (ZHB2022002, HZHB2022014), Science and Technology Plan Project of Liaoning Province (2021-BS-102).
Author information
Authors and Affiliations
Contributions
JZ and SMZ independently scrutinized the titles and abstracts of retrieved RCTs. They reviewed the full texts of selected RCTs to evaluate eligibility criteria for inclusion in NMA, extracted study characteristics and outcome data. XJQ resolved any disagreements between the authors if necessary. XYG, BWY, SW and CL wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consent participate
The RCTs involved in the article had approvaled by Ethics, Law and Policy Group.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Data 1. Literature search strategies on PubMed. Supplementary Table 1. Checklist of the PRISMA extension for network meta-analysis. Supplementary Figure 1. Network of alltreatment comparisons for ORR and ≥3TRAEs. The lines connect the regimens that were directly compared in clinical trails. The thickness of the lines corresponds to the number of RCTs. PD1:Programmed death receptor 1 inhibitors; TP: Paclitaxelpluscis-platinum; FP:fluorouracilpluscis-platinum. Supplementary Figure 2. Convergence of the four chains established by inspection of the Brooks-Gelman-Rubin diagnostic and the density trace plot. (A) PFS; (B) OS; (C) ORR; (D) ≥3TRAEs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, J., Zhang, S., Guo, X. et al. PD-1 inhibitors combined with paclitaxel and cisplatin in first-line treatment of esophageal squamous cell carcinoma (ESCC): a network meta-analysis. BMC Cancer 23, 1221 (2023). https://doi.org/10.1186/s12885-023-11715-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11715-3