Abstract
Background
Vaginal CO2 laser therapy is a new treatment option for genitourinary syndrome of menopause. Its potential is particularly interesting in breast cancer survivors, where existing treatment options often are insufficient as hormonal treatment is problematic in these women. The objective of this study is to investigate the effectiveness of vaginal laser treatment for alleviation of genitourinary syndrome of menopause in breast cancer survivors treated with adjuvant endocrine therapy. The secondary objective is to explore the importance of repeated vaginal laser treatment and the long-term effects in this patient population.
Methods
VagLaser consist of three sub-studies; a dose response study, a randomized, participant blinded, placebo-controlled study and a follow-up study. All studies include breast cancer survivors in adjuvant endocrine therapy, and are conducted at the Department of Obstetrics and Gynecology, Randers Regional Hospital, Denmark. The first participant was recruited on 16th of February 2023. Primary outcome is vaginal dryness. Secondary subjective outcomes are vaginal pain, itching, soreness, urinary symptoms and sexual function. Secondary objective outcomes are change in vaginal histology (punch biopsy), change in vaginal and urine microbiota, and change in vaginal pH.
Discussion
More randomized controlled trials, with longer follow-up to explore the optimal treatment regimen and the number of repeat vaginal laser treatments for alleviation the symptoms of genitourinary syndrome of menopause in breast cancer survivors treated with endocrine adjuvant therapy, are needed. This study will be the first to investigate change in vaginal and urine microbiota during vaginal laser therapy in breast cancer survivors.
Trial registration
ClinicalTrials.gov: NCT06007027 (registered 22 August, 2023).
Protocol version: Version 1, Date 13.11.2023.
Similar content being viewed by others

Item from the World Health Organization trial registration data set
Data category | Information |
Primary registry and trial identifying number | ClinicalTrials.gov: NCT06007027 |
Date of registration in primary registry | 22 August, 2023 |
Primary sponsor | Pinar Bor |
Secondary sponsors | Marianne Glavind-Kristensen and Anders Bonde Jensen |
Contact for public queries | Sine Jacobsen, MD, Mobile + 4560244277, Email sinjac@rm.dk |
Contact for scientific queries | Sine Jacobsen, MD Department of Obstetrics and Gynaecology, Randers Regional Hospital, Denmark Department of Clinical Medicine, Aarhus University, Denmark |
Public title | Vaginal CO2 laser therapy for genitourinary syndrome in breast cancer survivors |
Scientific title | Vaginal CO2 laser therapy for genitourinary syndrome in breast cancer survivors—A randomized blinded, placebo-controlled trial |
Country of recruitment | Denmark |
Health condition(s) or problem(s) studied | Genitourinary syndrome of menopause |
Intervention(s) | Active comparator: SmartXIDE2V2LR, MonaLisa Touch, DEKA, Florence, Italy (Setting: dot power 30 W, dwell time 1000 μs, dot spacing 1000 μs and the smart stack parameter from 2–3) Placebo comparator: SmartXIDE2V2LR, MonaLisa Touch, DEKA, Florence, Italy (Setting: 0 W, dwell time 100 μs, dot spacing 2000 μs and the smart stack parameter from 1 to 1) |
Key inclusion and exclusion criteria | Key inclusion criteria: Breast cancer survivor in endocrine therapy, age > 18 years, symptomatic genitourinary syndrome of menopause with vaginal discomfort and/or dyspareunia Key exclusion criteria: Use of non-hormonal/hormonal vaginal therapies (1 and 12 months prior to the baseline visit, respectively), treatment with Chemotherapy (6 months prior to the baseline visit) |
Study type | Interventional Allocation: randomized Intervention model: parallel assignment Masking: blinded (participants) Primary purpose: reducing late effects of breast cancer treatment |
Date of first enrolment | February 2023 |
Target sample size | 90 participants |
Recruitment status | Recruiting |
Primary outcome | Vaginal dryness |
Key secondary outcomes | Subjective outcomes are vaginal pain, itching, soreness, urinary symptoms and sexual function Objective outcomes are change in vaginal histology (punch biopsy), change in vaginal and urine microbiota and change in vaginal pH |
Background
Breast cancer (BC) is the most common type of cancer among women worldwide. Adjuvant endocrine therapy is offered to those 80% of the breast cancer patients with estrogen positive disease. Thus, pre- and peri-menopausal women are treated with tamoxifen, a selective estrogen receptor modulator (SERM) which will block the effect of estrogen, for 10 years if node positive and 5 years if node negative in the axilla. Post-menopausal women are treated with an aromatase inhibitor (AI) in five years, e.g., letrozole, which inhibits the production of estrogen. Notably, 50–75% of breast cancer survivors (BCS) experience one or more symptoms of genitourinary syndrome of menopause (GSM) [1], which is defined as a collection of signs and symptoms such as vaginal dryness, dyspareunia, irritation, urinary incontinence and urinary tract infections [2]. Vaginal treatment with estrogen can alleviates GSM symptoms but significant absorption through the vaginal epithelium has been reported [3]. This leads to concerns about the risk of cancer recurrence [4] and many BCS want to avoid estrogen-containing treatment. An effective, non-hormonal, and safe treatment of GSM in women diagnosed with BC is lacking today.
Fractional CO2 laser removes layers of skin tissue and causes regeneration of scar tissue. The treatment is given as arrays of small laser beams creating a matrix of microscopic epithelial and sub-epithelial thermal necrosis. This induces a wound-healing cascade with formation of elastin- and collagen fibers resulting in tissue remodeling [5, 6]. Furthermore, laser therapy may improve proliferation of vaginal epithelial cells and glycogen production, which is essential for the growth of vaginal lactobacilli. This results in increased lactobacillus flora and a lowering of vaginal pH needed to maintain vaginal health and avoid local inflammation [7]. The prevalence of lactobacilli has been reported to change from 30 to 79% in postmenopausal women after vaginal laser treatment [7]. Vagina and bladder share the same commensal bacteria. A high number of lactobacilli is also important in maintaining bladder health by lowering pH which inhibits growth of many uropathogens and prevents attachment of uropathogens to uroepithelial cells [8,9,10]. Overall, high occurrence of lactobacilli prevents infection. Vaginal laser therapy is a safe procedure, and no serious adverse events have been reported [11].
Previous studies showed improvements of GSM symptoms by vaginal laser treatment in women with spontaneous menopause and iatrogenic menopause [12,13,14,15]. However, iatrogenic menopause after breast cancer treatment with endocrine therapy represents a unique endocrine situation. Very limited studies have investigated the optimal treatment regime and the number of repeat laser treatments to obtain comparable effects of vaginal laser treatment on GSM in BSC. A recently published review by Mortensen et al. [11] concluded that larger long-term and high-quality RCTs are needed within this field before vaginal laser can be considered a routine treatment for GSM in BSC.
Objectives
The primary objective is to investigate the effectiveness of vaginal laser treatment for alleviation of vaginal dryness which is the cardinal symptom of GSM symptoms in BCS treated with endocrine adjuvant therapy in the placebo-controlled study. Vaginal pain, itching, soreness, urinary symptoms and sexual function will be accessed as secondary subjective outcomes and change in vaginal histology (punch biopsy), change in vaginal and urine microbiota and change in vaginal pH will be accessed as secondary objective outcomes. This project also evaluates the long-term effects, including provide information on the optimal number of repeat vaginal laser sessions and effectiveness of three versus four versus five vaginal laser treatment in this patient population.
Methods
The VagLaser trial is a single-center study containing three sub-studies:
-
I.
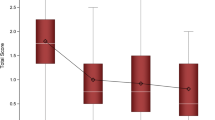
A dose–response study exploring the optimal number of laser treatments needed to achieve an effect on GSM symptoms in BCS. A total of 30 participants will be included for a maximum of five treatments of vaginal laser therapy at 4–6 weeks' intervals.
-
II.
A randomized, participant blinded, placebo-controlled study to compare vaginal laser therapy with sham laser therapy in 60 BCS, with a fixed number of treatments. The number of vaginal laser treatments depends on results obtained from study I.
-
III.
A one-year follow up study on participants from study II. The participants from the active laser group will be offered a single "booster" treatment.
Site
Department of Obstetrics and Gynecology, Randers Regional Hospital, Denmark.
Study period
The first participant was recruited the 16th of February 2023. The anticipated date of the last follow up is June 2025.
Approval of the study protocol
The study has been approved by the Danish Data Protection Agency (1–16-02–327-22) and by the Danish Ethical Committee (1–10-72–183-22).
Participants
The VagLaser trial includes breast cancer survivors in endocrine treatment (SERM or AI) with GSM symptoms. Inclusion and exclusion criteria for participation (Table 1) are verified before starting the first vaginal laser application.
Participants are recruited through Danish Breast Cancer Organization, Danish Organization for sequelae after cancer, social media (e.g., Facebook, Instagram), from Department of Obstetrics and Gynecology, Randers Regional Hospital, Department of Obstetrics and Gynecology, Aarhus University Hospital, Department of Oncology at Aarhus University Hospital, Department of Oncology at Aalborg University Hospital, Department of Oncology at Vejle Regional Hospital, Denmark.
Vaginal CO2 laser protocol
Active treatment
Included patients are treated intravaginally with the fractional microablative CO2 laser system (SmartXIDE2V2LR, MonaLisa Touch, DEKA, Florence, Italy), using the following settings: dot power 30 W, dwell time 1000 μs, dot spacing 1000 μs and the smart stack parameter from 2 to 3. At the level of the vaginal introitus, the dot power decreases to 20 Watt. The procedure is performed in the outpatient clinic and do not require any specific preparation (e.g. analgesia/anesthesia).
Sham procedure used in the randomized study
Included patients are treated intravaginally with the fractional microablative CO2 laser system (SmartXIDE2V2LR, Monalisa Touch, DEKA, Florence, Italy), using the following settings: dot power 0.5 W, dwell time 100 μs, dot spacing 2000 μs and the smart stack parameter from 1 to 1. This procedure is identical to the treatment procedure and even the noise involved with firing the laser is maintained allowing blinding of the participants.
Prohibited concomitant medications
The use of oral or vaginal hormonal therapies (e.g. Vagifem) is not permitted for the participants during the study period. If needed, participants may use a specific 92% rich fat cream ("Dr. Warming Critical Care") in the intimate area during the study period.
Outcome measures
Primary outcome
Vaginal dryness
Participant are asked to complete the 10-cm visual analog scale (VAS) ranging for 0 to 10, with higher score indicating worse vaginal dryness.
-
Study I: Primary outcome is difference of vaginal dryness between baseline visit, and after third, fourth and fifth laser treatment.
-
Study II: Primary outcome is difference in vaginal dryness four weeks after the last treatment between the laser group and the sham group.
-
Study III: Primary outcome is vaginal dryness one year after the last laser treatment. Secondary outcome is the effect of one booster treatment on vaginal dryness.
Subjective secondary outcomes
Vaginal pain, itching and soreness, evaluated with VAS for vaginal pain, itching, soreness.
Sexual function
Participant are asked to complete the questionnaire Female Sexual Function Index (FSFI) for sexual function parameters; desire, arousal, lubrication, orgasm, satisfaction and pain (range 2–36, the threshold of 26.55 indicates sexual dysfunction) [16] and Sexual complaint screener – women (SCS-W) questionnaire addressing all domains of sexual dysfunction (range 0–60, higher score indicate increased symptom severity [17].
Urinary symptoms
Evaluated by the questionnaire Urogenital Distress Inventory (UDI-6); irritative symptoms, obstructive/discomfort and stress symptoms (range 0–18, higher score indicate higher disability) [18] and International Consultation on Incontinence Questionnaire Female Urinary Tract Symptoms Sex (ICIQ-FLUTSsex) for evaluation of female sexual matters associated with their lower urinary tract symptoms (range 0–14, higher values indicating increased symptom severity) [19].
Vaginal health index (VHI)
A gynecologic examination is performed by an experienced gynecologist at the baseline visit and at each follow-up visits using the VHI. VHI includes subjective scoring of moisture, fluid volume, epithelial integrity and elasticity and objective scoring of pH (VHI ranges 5–25, higher VHI scores indicate better health).
Objective secondary outcomes
Change in vaginal pH
Vaginal pH is measured using pH-Indicator strips.
Change in vaginal histology
A punch biopsy of 4*4 mm is taken from the lateral left vaginal wall at the baseline visit and from the lateral right vaginal wall at the follow-up visit. The biopsy is immediately formalin fixated and then processed for light microscopy. Some sections are stained using haematoxylin and eosin (H&E), and others with Masson's trichrome stain and immunohistochemistry test. The biopsies are evaluated by a specialized gynecological pathologist at The Department of Pathology Randers Regional Hospital, reporting on the changes in the vaginal histology.
Change in vaginal and urine microbiota
One polyester swap (FLOQSwab) is used to sample mid-vagina for microbial analysis and immediately been placed at – 80 °C until further processing. Urine is collected in a 50 mL collection tube using the clean catch method for women. Prior to voiding, the urethral meatus/urinary opening is cleaned with sterile water. Afterwards aliquoted into 10 mL fractions and immediately been placed at – 80 °C until further processing.
DNA is isolated from samples using standard DNA isolation kits and microbiota composition determined using 16S rRNA gene sequencing, which are performed at Centre for Clinical Research, North Denmark Regional Hospital. Microbiota composition is compared between groups and over time based on alpha- and beta-diversity measures, as well as changes in relative abundances of individual bacteria.
Data collection
Data are collected electronically and stored in Research Electronic Data Capture (REDCap, Aarhus University), which is a secure online database. Demographic characteristics are collected from women included at baseline visit as follows: age, BMI, smoking, parities, age at menopause, years since breast cancer diagnosis, years since start at endocrine therapy, type of endocrine therapy.
-
Study I: Symptom data are collected at baseline, after each treatment visit and 6 months after the initial treatment. Vaginal biopsy is collected at baseline visit and 6 months after the initial treatment. Vaginal and urine microbiota are collected at baseline visit, at each treatment visit, and 6 months after initial treatment (Table 2).
-
Study II: Symptom data, vaginal biopsy, vaginal and urine microbiota are collected at baseline visit and one month after the last treatment (Table 3).
-
Study III: Symptom data, vaginal biopsy, vaginal and urine microbiota are collected at one year follow-up visit which is scheduled one year after the completion of the last treatment in the study II, and one month after the single "booster" treatment.
Randomization, blinding and informed consent
The women are e informed about the trial when they contact principal investigator. After signing of informed consent to participation, women are randomized in a 1:1 ratio to either laser group or sham group using an Internet-based randomization-program (REDCap, Aarhus University). Women are stratified by age, duration of prior endocrine treatment, and type of endocrine treatment. The participants in study II will be blinded to treatment allocation until the study has been completed.
Side effects and adverse event
Vaginal laser therapy is associated with a low risk of complications. Most patients (97%) experience almost no or only mild discomfort in relation to the treatment [20]. The mild immediate symptoms after vaginal laser therapy are seen within the first two days and include burning sensation, itching, bruising and swelling [21]. The investigator will report to the Danish research ethics committees all suspected unexpected serious adverse reactions/events as soon as possible.
Power calculation and statistical analysis
Considering the VAS score ranging for 0 to 10 for vaginal dryness as the primary outcome. In study one the sample size was calculated based on an expected mean 30% improvement on the VAS score for vaginal dryness from the third treatment compared to the fifth treatment. Aiming for a power of 90% and an alpha of 0.05 and a standard deviation of 2.9 was adopted [22], a sample size of 23 women were required. With an estimate loss of 20% participants during the five laser treatments, a total of 30 women will be included in study I. In study two the sample size was calculated based on an expected 30% improvement on the VAS score for vaginal dryness in the active laser group compared to the sham laser group. To achieve a power of 90% and an alpha of 0.05 with a standard deviation of 2.9 [22] it was determined that [22], a sample size of 21 women in each group was required. With an estimate loss of 20% participants during the second study, a total of 52 women will be included in study II, 26 in each group.
Statistical analyses will be performed using STATA. If the data followed a Gaussian distribution, the Student’s t-test will be used to test for differences between variable means. Otherwise, Mann Whitney's test will be used. For ordinal data from the questionnaires, Pearson’s χ2 and linear-by-linear tests will be performed. Paired test with one-way ANOVA will be used to evaluate change over time. Groups variables will be tested for change over time with two-way ANOVA (repeated measurements). A 2-sided P-value < 0.05 will be chosen as the level of statistically significance. Data are given as mean ± SD if they followed a Gaussian distribution; otherwise, median (range) are indicated.
Discussion
One of the main problems among BCS in endocrine therapy are symptoms of GSM, and the fact that untreated GSM worsens over time exacerbate the problems further [23]. Local estrogen treatment seems to be safe in most BCS, but a large number of BCS are concerned about risk of cancer relapse and want to avoid any kind of estrogen-containing treatment. Thus, an alternative non-hormonal treatment for GSM in BCS is much needed. A recent published study by Mension et al. [24] found an overall improvement after vaginal laser therapy in BCS, but no statistically significant differences were observed in the active vaginal laser therapy group compared to the sham laser therapy group. In conclusion more RCTs with longer follow-up to explore the optimal treatment regime and the number of repeat vaginal laser treatments for alleviation of GSM symptoms in BCS treated with endocrine adjuvant therapy, are needed. Furthermore, this study will be the first to investigate change in vaginal and urine microbiota during vaginal laser therapy in BCS.
Ancillary and Post-Trial Care
Participants that are enrolled into the study are covered by the Danish public patient compensation scheme, if unforeseen late effects of the treatment are seen.
Availability of data and materials
The trial is ongoing. When the primary data from the trial are published the data will become publicly available.
Abbreviations
- AI:
-
Aromatase inhibitor
- BCS:
-
Breast cancer survivors
- GSM:
-
Genitourinary syndrome of menopause
- SERM:
-
Selective estrogen receptor modulator
References
Sousa MS, Peate M, Jarvis S, Hickey M, Friedlander M. A clinical guide to the management of genitourinary symptoms in breast cancer survivors on endocrine therapy. Ther Adv Med Oncol. 2017;9(4):269–85.
Arunkalaivanan A, Kaur H, Onuma O. Laser therapy as a treatment modality for genitourinary syndrome of menopause: a critical appraisal of evidence. Int Urogynecol J. 2017;28(5):681–5.
Labrie F, Cusan L, Gomez JL, Côté I, Bérubé R, Bélanger P, et al. Effect of one-week treatment with vaginal estrogen preparations on serum estrogen levels in postmenopausal women. Menopause. 2009;16(1):30–6.
Biglia N, Bounous VE, D’Alonzo M, Ottino L, Tuninetti V, Robba E, et al. Vaginal atrophy in breast cancer survivors: attitude and approaches among oncologists. Clin Breast Cancer. 2017;17(8):611–7.
Salvatore S, Leone Roberti Maggiore U, Athanasiou S, Origoni M, Candiani M, Calligaro A, et al. Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause. 2015;22(8):845–9.
Karcher C, Sadick N. Vaginal rejuvenation using energy-based devices. Int J Womens Dermatol. 2016;2(3):85–8.
Athanasiou S, Pitsouni E, Antonopoulou S, Zacharakis D, Salvatore S, Falagas ME, et al. The effect of microablative fractional CO2 laser on vaginal flora of postmenopausal women. Climacteric. 2016;19(5):512–8.
O’Hanlon DE, Moench TR, Cone RA. Vaginal pH and microbicidal lactic acid when lactobacilli dominate the microbiota. PLoS One. 2013;8(11).
Chan RC, Reid G, Irvin RT, Bruce AW, Costerton JW. Competitive exclusion of uropathogens from human uroepithelial cells by Lactobacillus whole cells and cell wall fragments. Infect Immun. 1985;47(1):84–9.
Pearce MM, Hilt EE, Rosenfeld AB, Zilliox MJ, Thomas-White K, Fok C, et al. The female urinary microbiome: a comparison of women with and without urgency urinary incontinence. mBio. 2014;5(4):e01283–14.
Mortensen OE, Christensen SE, Løkkegaard E. The evidence behind the use of LASER for genitourinary syndrome of menopause, vulvovaginal atrophy, urinary incontinence and lichen sclerosus: a state-of-the-art review. Acta Obstet Gynecol Scand. 2022;101(6):657–92.
Li F, Picard-Fortin V, Maheux-Lacroix S, Deans R, Nesbitt-Hawes E, McCormack L, et al. The efficacy of vaginal laser and other energy-based treatments on genital symptoms in postmenopausal women: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2021;28(3):668–83.
Salvatore S, Athanasiou S, Candiani M. The use of pulsed CO2 lasers for the treatment of vulvovaginal atrophy. Curr Opin Obstet Gynecol. 2015;27(6):504–8.
Pearson A, Booker A, Tio M, Marx G. Vaginal CO 2 laser for the treatment of vulvovaginal atrophy in women with breast cancer: LAAVA pilot study. Breast Cancer Res Treat. 2019;178(1):135.
Quick AM, Zvinovski F, Hudson C, Hundley A, Evans C, Stephens JA, et al. Patient-reported sexual function of breast cancer survivors with genitourinary syndrome of menopause after fractional CO2 laser therapy. Menopause (New York, NY). 2021;28(6):642–9.
Bartula I, Sherman KA. The Female Sexual Functioning Index (FSFI): evaluation of acceptability, reliability, and validity in women with breast cancer. Support Care Cancer. 2015;23(9):2633–41.
Giraldi A, Rellini A, Pfaus JG, Bitzer J, Laan E, Jannini EA, et al. Questionnaires for assessment of female sexual dysfunction: a review and proposal for a standardized screener. J Sex Med. 2011;8(10):2681–706.
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol. 1997;104(12):1374–9.
Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P. The bristol female lower urinary tract symptoms questionnaire: development and psychometric testing. Br J Urol. 1996;77(6):805–12.
González Isaza P, Jaguszewska K, Cardona JL, Lukaszuk M. Long-term effect of thermoablative fractional CO(2) laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J. 2018;29(2):211–5.
Arroyo C. Fractional CO(2) laser treatment for vulvovaginal atrophy symptoms and vaginal rejuvenation in perimenopausal women. Int J Womens Health. 2017;9:591–5.
Cruz VL, Steiner ML, Pompei LM, Strufaldi R, Fonseca FLA, Santiago LHS, et al. Randomized, double-blind, placebo-controlled clinical trial for evaluating the efficacy of fractional CO2 laser compared with topical estriol in the treatment of vaginal atrophy in postmenopausal women. Menopause. 2018;25(1):21–8.
Castelo-Branco C, Mension E, Torras I, Cebrecos I, Anglès-Acedo S. Treating genitourinary syndrome of menopause in breast cancer survivors: main challenges and promising strategies. Climacteric. 2023:1–6.
Mension E, Alonso I, Anglès-Acedo S, Ros C, Otero J, Villarino Á, et al. Effect of fractional carbon dioxide vs sham laser on sexual function in survivors of breast cancer receiving aromatase inhibitors for genitourinary syndrome of menopause: the LIGHT randomized clinical trial. JAMA Netw Open. 2023;6(2):e2255697.
Acknowledgements
Not applicable.
Funding
Funding for the trial has been obtain from the below mentioned organisations and foundations, who have no role in the design of the study, collection, analysis, interpretation of the data, nor in writing the manuscript:
Randers Regional Hospital, Denmark.
Health Research Fund of Central Denmark Region.
Danish Cancer Society.
Author information
Authors and Affiliations
Contributions
AF had the idea for the trial. SJ designed the trial with substantial contributions from PB, AB, MGK and AF. The protocol was written by SJ with substantial contributions from PB, AB, MGK and AF. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the Danish Data Protection Agency (1–16-02–327-22) and by the Danish Ethical Committee (1–10-72–183-22).
All the eligible women will have written and oral information by the principal investigator about the aim of the study, the methods of the study and the possible adverse events related to the intervention. All study participants will give written inform consent before inclusion. The consent form will be kept safe during the study period. The study results will be released to the participant.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jacobsen, S., Glavind-Kristensen, M., Jensen, A.B. et al. Vaginal CO2 laser therapy for genitourinary syndrome in breast cancer survivors—VagLaser study protocol: a randomized blinded, placebo-controlled trial. BMC Cancer 23, 1164 (2023). https://doi.org/10.1186/s12885-023-11656-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11656-x