Abstract
Introduction
Breast cancer is presently the most commonly diagnosed cancer in women, and it stands as the leading cause of cancer-related deaths worldwide. Notably, breast cancer rates have seen a significant increase in sub-Saharan African countries, including Ethiopia. Several risk factors contribute to breast cancer, some of which can be modified, while others are inherent. Promoting a healthier diet is strongly encouraged as a preventive measure against breast cancer. However, it’s noteworthy that no previous research has investigated the connection between dietary patterns and the risk of breast cancer among Ethiopian women. Therefore, the primary objective of the current study is to examine the relationship between dietary patterns, socioeconomic and behavior factors associated with breast cancer in Ethiopian women.
Methods
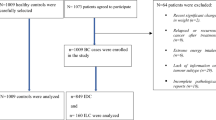
A case-control study was conducted at an institution in Bahir Dar, Northwest Ethiopia, involving 260 women, comprising 86 cases and 174 controls. We administered a standardized and validated questionnaire to assess a range of sociodemographic, reproductive, clinical, lifestyle, and dietary characteristics through face-to-face interviews. To analyze the differences between the cases and controls, we employed the Chi-square test. Furthermore, we assessed the relationships between these variables using binary multivariate logistic regression. To measure the association between variables, we utilized odds ratios with 95% confidence intervals.
Results
The results of the multivariate analysis indicated that participants in the younger age group had significantly lower odds of developing breast cancer (AOR = 0.05; 95% CI: 0.00-0.91) compared to those in the older age group. Additionally, women who breastfed their children for shorter durations were 3.66 times more likely to develop breast cancer (AOR = 3.66; 95% CI: 2.78–6.89) than those who breastfed for longer periods. Furthermore, women with sedentary lifestyles faced a significantly higher risk of breast cancer, with odds 10.53 times greater (AOR = 10.53; 95% CI: 5.21–21.36) than their counterparts who engaged in moderate or highly active lifestyles. Lastly, participants who had previously undergone chest therapy were 6.43 times more likely to develop breast cancer (AOR = 6.43; 95% CI: 3.20–13.90) compared to those who had not.
Conclusions
Breast cancer prevention interventions, including breastfeeding counseling and increased physical activity should be recognized as a central strategy for lowering breast cancer risk. Furthermore, healthcare providers should aim to minimize exposure to chest radiation therapy.
Similar content being viewed by others
Background
Breast cancer is currently the most commonly diagnosed cancer among women and is the leading cause of cancer-related deaths worldwide [1]. Shockingly, one in every eight women globally will face a breast cancer diagnosis during her lifetime [2]. In sub-Saharan African countries, including Ethiopia, the incidence of breast cancer has been on the rise, resulting in high mortality-to-incidence ratios due to advanced stage at presentation and limited access to effective treatments [3]. In Ethiopia, the incidence of breast cancer has shown a continuous and rapid increase year by year. It now stands as the most prevalent cancer, accounting for 33% of all cancers in women and 23% of all cancers overall [4]. What’s particularly concerning is that breast cancer tends to occur at a younger age in Ethiopian women compared to their Western counterparts, often presenting at an advanced stage [5].
While several well-established risk factors for breast cancer, such as family history, early menarche, late menopause, adult-attained height, and other reproductive histories, are challenging to modify [6], diet stands out as a modifiable factor. Extensive research has examined the associations between various single foods and nutrients with breast cancer, revealing that dietary modifications could prevent approximately one-third of breast cancer cases [7]. Presently, the emphasis is on shifting toward a healthier diet, one that favors nutrient-rich and less energy-dense foods. This dietary approach is strongly encouraged by the World Cancer Research Fund (WCRF) as a means to prevent various cancers, including breast cancer [8]. High energy intake and low physical activity significantly contribute to the risk of breast cancer, and adopting healthier dietary patterns is the most impactful way to mitigate this risk [9]. Among specific dietary factors, alcohol consumption stands out as a well-established risk factor for breast cancer [10]. Likewise, high consumption of red meat, animal fats, and refined carbohydrates has been linked to an increased risk of breast cancer [11]. Conversely, compelling evidence indicates that adopting healthy dietary patterns, characterized by increased consumption of fruits, vegetables, whole grains, and dietary fiber, is associated with a reduced risk of breast cancer [12] [13] [14].
While specific foods have been implicated in breast cancer risk in some instances, it’s important to recognize that food is a complex interplay of various nutrients. As a result, the overall body of evidence remains inconclusive [15]. Many epidemiological studies examining the role of dietary patterns in breast cancer have predominantly taken place in developed countries. Dietary patterns are known to vary significantly across populations, influenced by factors such as geography, socioeconomic status, and cultural food habits, preferences, and availability [16]. In the Ethiopian context, the dietary pattern exhibits unique characteristics, primarily consisting of cereals, roots, tubers, and pulses. This diet is characterized by low dietary diversity and limited consumption of fruits, vegetables, fish, and animal products [17].
Due to limited treatment options with poor prognoses, a significant number of Ethiopian women are diagnosed with advanced breast cancer [3]. Consequently, primary prevention strategies, including the promotion of healthy dietary patterns, emerge as the most cost-effective means of reducing cancer incidence rates and high mortality in low-income countries like Ethiopia, where incidence rates are on the rise. To the best of our knowledge, no previous studies have explored the association between dietary patterns and breast cancer risk among Ethiopian women. Therefore, the primary aim of this study is to investigate the relationship between dietary patterns, socio-economic, reproductive and behavioral factors and breast cancer risk among Ethiopian women while controlling for other important covariates. We hypothesized that regular consumption of healthy dietary pattern, high socio-economic status, long duration of breastfeeding and increased physical activity reduce the risk of breast cancer.
Methods
Study design and setting
We conducted an institution-based case-control study from May 16 to July 16, 2021, at Felege Hiwot Comprehensive Specialized Hospital (FHCSH) in Bahir Dar, Northwest Ethiopia. In the first phase, we selected all 88 cases of women aged 18 and above with pathologically confirmed breast cancer who were referred to the chemotherapy clinics of FHCSH, which serves as a cancer diagnosis referral center. In the second phase, we chose 175 control participants from among women aged 18 and above admitted to other sections of the same hospital for various non-neoplastic diseases unrelated to long-term modification of diet.
Sample size determination
The sample size was determined based on several factors: a 1 to 2 ratio of cases to controls, a confidence level of 95%, a power of 80%, and an odds ratio of 2.7. The odds ratio was derived from a prior case-control study conducted in Addis Ababa, Ethiopia. To arrive at the total sample size, we started with 239 individuals. To account for potential non-responses, we added a 10% contingency, resulting in an additional 24 individuals. Therefore, the final sample size was 263 participants, comprising 88 cases and 175 controls.
Data collection
Dietary assessment
The study’s data collection was conducted by trained nurse professionals who conducted private face-to-face interviews and reviewed medical records. These interviewers received training from nutritionist professionals. Dietary patterns were categorized into ‘healthy’ and ‘unhealthy’. A healthy dietary pattern includes the daily consumption of fruits, vegetables, and whole grains, as well as never to little (never to 1–3 per month) consumption of processed food, red meat, and sweetened beverages ,.An unhealthy dietary pattern includes 1–2 times per week to daily consumption of fatty and greasy foods, sweetened beverages and foods, highly flavored food, overly pungent food, canned and processed foods, and excessive alcohol consumption includes (1–2 times per week to daily).
Data were gathered using a validated semi-quantitative food frequency questionnaire (FFQ) [18] [19], which was adapted to include Ethiopian food items. This FFQ has previously demonstrated relative validity and reproducibility in assessing food and nutrient intakes among adults. Compared to other dietary assessment methods like short-term recall or diet records, FFQ is more user-friendly, places fewer burdens on respondents, and provides a quick estimate. This makes the FFQ a practical and suitable tool for measuring long-term dietary intake in most epidemiological studies [20], making it an appropriate choice for our study population. Dietary habits for cases were assessed for the year prior to diagnosis, while for controls, it was the year before the interview. Using this FFQ, the consumption frequency of each food item was evaluated on a daily, weekly, or monthly basis. The questionnaire was initially prepared in English, then translated into Amharic, the local language. To ensure consistency, it was translated back into English by a professional translator.
Assessment of Breast cancer
Pathologically confirmed breast cancer was the outcome of this study. Pathologically confirmed breast cancer refered to a diagnosis of breast cancer that has been definitively confirmed through the examination of tissue samples (biopsy) obtained from the breast.
Assessment of potential sociodemographic factors
We gathered self-reported demographic and socioeconomic information including age (18–29, 30–49 and > 50 years old); marital status (Married/unmarried); residence (urban/rural); religion (orthodox/others); education (illiterate, primary, secondary and college and above); occupation (house wife, self-employed, government employed); and income/monthly (≤ 1000, 1001–3000, 3001–6000 and > 6000 birr) was collected. Detailed information was collected regarding history of health, family history of breast cancer, reproductive risk factors, age at menarche (≥ 15/>15 years old) and menopause status (pre-menopause/post-menopause), history of child birth(yes/no), age at first birth (14–18, 19–24 and > 25), breast-feeding history at for each live birth (≤ 1 year/>1 year), and use of modern contraceptives (yes/no). Anthropometric measurements (weight, height) were also collected. BMI was calculated using measured height and weight (kg/m2) [21] [22]. BMI was categorized as under- underweight (18. >18.5 kg/m2), Normal weight (18.5–24.9 kg/m2) and overweight/obese ( > = 25.0 kg/m2). Physical activity level was assessed as sedentary (such as reading, working on a computer, watching television), light activity (including slow waking, standing with minor efforts), moderate activity (such as brisk waking, swimming), very active and, extremely active (including running and carrying heavy load). Cigarette Smoking (yes/no) and alcohol drinking (Never, 1–3/month, 1–2/week, 3–4/week and daily) behaviors were also collected furthermore. We also collected data on breast cancer cases including stage of breast cancer (I-IV) and affected breast (right/left) Previous chest radiation therapy (yes/no) was collected for both case and control patients as well. See the supplementary information (questionnaire) on annex 1.
Statistical analysis
We conducted data analysis using SPSS version 20, a statistical software package. To evaluate the differences between cases and controls, we employed the Chi-square test, presenting the results as frequencies and percentages. For assessing the relationships between the explanatory variables and breast cancer, we utilized both bivariate and multivariate logistic regression, calculating odds ratios and 95% confidence intervals (95% CI). Variables with a p-value of less than 0.25 in the bivariate analysis were included in the multivariable model. We assessed the goodness-of-fit of each model using the Hosmer and Lemeshow Test, where a higher p-value indicates a better model fit. Importantly, all models demonstrated p-values greater than 0.05.
Ethical consideration
Since the Bahir Dar Institute of Technology (BiT) lacks an institutional review board, we obtained ethical clearance through our partner institute, the Amhara Public Health Institute (APHI). Furthermore, we ensured the informed consent of all study participants by explaining the study’s objectives. For participants who were unable to read the consent form, healthcare providers read it aloud to them. Those who willingly volunteered to participate provided their consent by either signing the form or applying a thumb impression. We assured respondents that their names would not be disclosed, and all information provided would remain confidential. Additionally, participants were given the opportunity to ask questions about the study and had the option to refuse or discontinue their participation at any time. The APHI research review committee approved that all methods adhered to the applicable ethical standards and regulations outlined in the Declaration of Helsinki.
Results
Table 1 displays the distribution of selected characteristics among breast cancer cases and control participants. Age showed a significant difference between the two groups, with a higher percentage of younger individuals among the controls (p = 0.000). Additionally, education, occupation, and income status were significantly different between cases and controls, with controls generally having higher levels of education, occupation, and income. Regarding disease and behavioral characteristics, a larger percentage of breast cancer cases had undergone chest radiation therapy (p = 0.000), reported sedentary behavior (p = 0.000), and experienced under-nutrition (p = 0.000). In terms of reproductive-related factors, the duration of breastfeeding significantly varied between cases and controls (p = 0.000). The higher proportion of controls were breastfed their children for longer duration than their case counterparts. All participants belonged to the same ethnic group (Amhara).
Table 2 presents factors associated with breast cancer risk. The crude analysis (bivariate analysis) indicated that several factors were statistically significant in relation to breast cancer risk, including age, residence, education level, occupation, monthly income, number of children ever born, age at first birth, duration of breastfeeding, physical exercise status, age at menarche, and menopause status. However, there was no observed association between dietary patterns and breast cancer risk (OR = 0.74; 95% CI: 0.43–1.27).
The results of the multivariate analysis are shown in Table 2 as well. The age group 18–29 years has a significantly lower risk of breast cancer (AOR: 0.05, 95% CI: 0.003–0.91) compared to the reference group (age > 50 years). Breastfeeding for equal or less than 1 year was associated with a significantly higher risk of breast cancer (AOR: 4.33, 95% CI: 2.78–6.89) compared to breastfeeding for more than 1 year. Additionally, women with sedentary behavior and light physical exercise had 10.53- and 6.13-times higher odds of developing breast cancer (AOR = 10.53; 95% CI: 5.21–21.36 and AOR = 6.13; 95% CI: 1.042-16.00, respectively) compared to their moderately or highly active counterparts. Finally, having received chest radiation therapy was associated with a significantly higher risk of breast cancer (AOR: 6.43, 95% CI: 3.20–13.90) compared to not having received chest radiation therapy.
Discussion
Our study makes a significant contribution to our understanding of the factors associated with breast cancer risk among Ethiopian women, especially in a region where the prevalence and incidence of this cancer are notably high. The current study found that women’s age, duration of breastfeeding, physical exercise status, and chest radiation therapy were statistically significant associated with breast cancer. Despite the fact that this study has significant limitations due to its reliance on self-reported data and recall bias, it is the first to investigate the connection of dietary patterns and other factors with breast cancer risk in Ethiopia.
Contrary to our initial hypothesis and in contrast to the findings of previous studies [23] [24] [25], our research did not identify any association between dietary patterns and the risk of breast cancer. This unexpected outcome could potentially be attributed to methodological considerations. Food frequency questionnaires, as a retrospective method, involve querying participants about their food and drink consumption patterns over extended periods. This approach relies on participants’ memory, literacy, and numerical skills, which can introduce inaccuracies and subjectivity into the reported data. Responses to dietary questions can result in both over-reporting and under-reporting.
This study uncovered a notable finding: younger participants demonstrated a lower likelihood of developing breast cancer compared to their older counterparts. This observation aligns with extensive evidence indicating an increased breast cancer risk with advancing age [26] [27] [28]. Several factors might contribute to this lower incidence of breast cancer in younger women.
Firstly, hormonal differences [29] could play a role, as well as varying exposure to risk factors like alcohol consumption [29] [30] and obesity [31], which tend to be more prevalent among older women. Additionally, research has consistently shown that younger women are more inclined to engage in regular exercise when compared to their older counterparts [32]. Regular physical activity carries various health benefits, including a potential reduction in the risk of breast cancer [32]. Similarly, overweight and obesity rates tend to be higher among older women [33] [34]. Several studies have highlighted obesity as a significant risk factor for various cancers, including breast cancer [35] [36].
In line with findings from studies conducted in other countries [26] [37] [38] [39], our research uncovered a significant link between breastfeeding duration and breast cancer risk. Specifically, our study revealed that women who breastfed their children for a year or less faced a 3.66 times higher risk of developing breast cancer compared to those who breastfed for over a year. This association can be attributed to the mechanisms by which breastfeeding reduces the risk of breast cancer. Notably, breastfeeding has been shown to lower the levels of hormones such as estrogen and progesterone, which have been linked to an increased risk of breast cancer. Additionally, breastfeeding leads to a shorter menstrual cycle in lactating mothers, limiting the exposure of breast tissue to these hormones and thereby inhibiting the development of cancer cells. Furthermore, breastfeeding promotes the shedding of breast tissue, aiding in the removal of cells with potential DNA damage within the breasts [40]. As such, breastfeeding has emerged as an exceptionally effective method for protecting mothers from breast cancer. In light of these findings, breast cancer interventions, such as breastfeeding counseling and programs aimed at enhancing breastfeeding practices, assume critical importance in reducing the risk of breast cancer.
This study uncovered a statistically significant relationship between physical activity levels and the risk of breast cancer. Notably, women who engaged in sedentary behavior faced a higher risk of developing breast cancer compared to those who maintained moderate or vigorous physical activity. This finding is consistent with previous research, which has consistently shown that regular exercise can significantly lower the risk of breast cancer [41] [42] [43]. The mechanisms through which exercise helps to reduce breast cancer risk are multifaceted. Firstly, exercise can contribute to a reduction in body fat [44], which, in turn, lowers the levels of certain hormones, such as estrogen, known to promote the growth of breast cancer cells. Additionally, physical activity can strengthen the immune system and reduce inflammation [32] [45], both of which are factors that may play a role in the initiation and progression of cancer. Given these compelling findings, it is imperative to view increasing physical activity as a central strategy in the effort to lower the risk of breast cancer.
Consistent with findings from other studies [46] [47], our research revealed that participants who had undergone chest radiation therapy were at a higher risk of developing breast cancer compared to their counterparts. Notably, a history of radiation exposure from chest X-rays was associated with an elevated risk of breast cancer. The underlying mechanism behind this association lies in the direct impact of radiation on the structure of the DNA double helix. This radiation-induced damage triggers DNA damage sensors, leading to processes such as apoptosis and necrosis, disrupting normal mitotic events, and ultimately reshaping various biological characteristics of neoplasm cells [47].
It is important to acknowledge potential limitations when interpreting these results. One notable limitation is the possibility of misclassification due to our reliance on self-reported dietary patterns. Additionally, the lengthy recall periods could lead to inaccurate reporting of past exposures. In light of these limitations, future studies should aim to address these issues for a more comprehensive understanding of the topic.
Conclusion
In our study, we identified several statistically significant associations with breast cancer risk, including women’s advanced age, duration of breastfeeding, physical exercise status, and chest radiation therapy. These findings underscore the importance of focusing on primary prevention strategies. Interventions should prioritize counseling on optimal breastfeeding duration, encouraging moderate to vigorous physical activity, and emphasizing the need for healthcare providers to limit chest radiation therapy exposure. These measures collectively contribute to reducing the risk of breast cancer.
Data Availability
The datasets analyzed during the current study will be available from the corresponding author on reasonable request.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- BMI:
-
Body mass index
- CI:
-
Confidence Interval
- COR:
-
Crude Odds Ratio
- FFQ:
-
Food Frequency Questionnaire
- FHCSH:
-
Felege Hiwot Comprehensive Specialized Hospital
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Kumar A, Singla A. Epidemiology of Breast cancer: current figures and trends. Prev Oncol Gynecol 2019:335–9.
Black E, Richmond R. Improving early detection of Breast cancer in sub-saharan Africa: why mammography may not be the way forward. Global Health. 2019;15:1–11. https://doi.org/10.1186/s12992-018-0446-6
Memirie ST, Habtemariam MK, Asefa M, Deressa BT, Abayneh G, Tsegaye B, et al. Estimates of cancer incidence in Ethiopia in 2015 using population-based registry data. J Glob Oncol. 2018;2018:1–11. https://doi.org/10.1200/JGO.17.00175
Gemta E, Bekele A, Mekonen W, Seifu D, Bekurtsion Y, Kantelhardt E. Patterns of Breast Cancer among Ethiopian patients: presentations and histopathological features. J Cancer Sci Ther. 2019;11:38–42.
Maas P, Barrdahl M, Joshi AD, Auer PL, Gaudet MM, Milne RL, et al. Breast cancer risk from modifiable and nonmodifiable risk factors among white women in the United States. JAMA Oncol. 2016;2:1295–302.
Masala G, Bendinelli B, Assedi M, Occhini D, Zanna I, Sieri S, et al. Up to one-third of Breast cancer cases in post-menopausal Mediterranean women might be avoided by modifying lifestyle habits: the EPIC Italy study. Breast Cancer Res Treat. 2017;161:311–20. https://doi.org/10.1007/s10549-016-4047-x
Shams-White MM, Brockton NT, Mitrou P, Romaguera D, Brown S, Bender A, et al. Operationalizing the 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) cancer prevention recommendations: a standardized scoring system. Nutrients. 2019;11:1572.
Marzbani B, Nazari J, Najafi F, Marzbani B, Shahabadi S, Amini M, et al. Dietary patterns, nutrition, and risk of Breast cancer: a case-control study in the west of Iran. Epidemiol Health. 2019;41:e2019003. https://doi.org/10.4178/epih.e2019003
Holmes MD, Willett WC. Does diet affect Breast cancer risk? Breast Cancer Res. 2004;6:170–8. https://doi.org/10.1186/bcr909
Cho E, Chen WY, Hunter DJ, Stampfer MJ, Colditz GA, Hankinson SE, et al. Red meat intake and risk of Breast cancer among premenopausal women. Arch Intern Med. 2006;166:2253–9.
Brennan SF, Cantwell MM, Cardwell CR, Velentzis LS, Woodside JV. Dietary patterns and Breast cancer risk: a systematic review and meta-analysis. Am J Clin Nutr. 2010;91:1294–302.
Dong J-Y, He K, Wang P, Qin L-Q. Dietary fiber intake and risk of Breast cancer: a meta-analysis of prospective cohort studies–. Am J Clin Nutr. 2011;94:900–5.
Malin AS, Qi D, Shu X, Gao Y, Friedmann JM, Jin F, et al. Intake of fruits, vegetables and selected micronutrients in relation to the risk of Breast cancer. Int J Cancer. 2003;105:413–8.
Wiseman M. The second world cancer research fund/american institute for cancer research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective: nutrition society and BAPEN Medical Symposium on ‘nutrition support in canc. Proc Nutr Soc. 2008;67:253–6.
Ahmadnia Z, Hasavari F, Roushan ZA, Khalili M. Dietary patterns and risk of Breast cancer in women in Guilan province, Iran. Asian Pac J Cancer Prev. 2016;17:2035–40.
Sheehy T, Carey E, Sharma S, Biadgilign S. Trends in energy and nutrient supply in Ethiopia: a perspective from FAO food balance sheets. Nutr J. 2019;18:1–12. https://doi.org/10.1186/s12937-019-0471-1
Shahar D, Shai I, Vardi H, Brener-Azrad A, Fraser D. Development of a semi-quantitative food frequency questionnaire (FFQ) to assess dietary intake of multiethnic populations. Eur J Epidemiol. 2003;18:855–61.
Macedo-Ojeda G, Vizmanos-Lamotte B, Márquez-Sandoval YF, Rodríguez-Rocha NP, López-Uriarte PJ, Fernández-Ballart JD. Validation of a semi-quantitative food frequency questionnaire to assess food groups and nutrient intake. Nutr Hosp. 2013;28:2212–20.
Rutishauser I. Principles of Nutritional Assessment. Nutr Diet. 2006;63:188–90.
Tałałaj M, Bogołowska-Stieblich A, Wąsowski M, Sawicka A, Jankowski P. The influence of body composition and fat distribution on circadian blood pressure rhythm and nocturnal mean arterial pressure dipping in patients with obesity. PLoS ONE. 2023;18:e0281151.
Neupane S, K C P, Doku DT. Overweight and obesity among women: analysis of demographic and health survey data from 32 sub-saharan African countries. BMC Public Health. 2016;16:30. https://doi.org/10.1186/s12889-016-2698-5
Xiao Y, Xia J, Li L, Ke Y, Cheng J, Xie Y, et al. Associations between dietary patterns and the risk of Breast cancer: a systematic review and meta-analysis of observational studies. Breast Cancer Res. 2019;21:1–22.
Bach KE, Kelly JT, Campbell KL, Palmer SC, Khalesi S, Strippoli GFM. Healthy dietary patterns and incidence of CKD: a meta-analysis of cohort studies. Clin J Am Soc Nephrol. 2019;14:1441–9. https://doi.org/10.2215/CJN.00530119
Buja A, Pierbon M, Lago L, Grotto G, Baldo V. Breast cancer primary prevention and diet: an umbrella review. Int J Environ Res Public Health. 2020;17:4731.
Bernstein L, Henderson BE, Hanisch R, Sullivan-Halley J, Ross RK. Physical exercise and reduced risk of Breast cancer in young women. JNCI J Natl Cancer Inst. 1994;86:1403–8.
Alkabban FM, Ferguson T. Breast cancer. Updated 7 August 2021. StatPearls [Internet] Treasure Isl StatPearls Publ; 2022.
Centers for Disease Control and Prevention (CDC). What Are the Risk Factors for Breast Cancer? Div Cancer Prev Control 2023. https://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm (accessed September 26, 2022).
Zhang X, Tworoger SS, Eliassen AH, Hankinson SE. Postmenopausal plasma sex hormone levels and Breast cancer risk over 20 years of follow-up. Breast Cancer Res Treat. 2013;137:883–92.
Jung S, Wang M, Anderson K, Baglietto L, Bergkvist L, Bernstein L, et al. Alcohol consumption and Breast cancer risk by estrogen receptor status: in a pooled analysis of 20 studies. Int J Epidemiol. 2016;45:916–28. https://doi.org/10.1093/ije/dyv156
Lorincz AM, Sukumar S. Molecular links between obesity and Breast cancer. Endocr Relat Cancer. 2006;13:279–92.
Peng B, Ng JYY, Ha AS. Barriers and facilitators to physical activity for young adult women: a systematic review and thematic synthesis of qualitative literature. Int J Behav Nutr Phys Act. 2023;20:1–17.
Park B, Cho HN, Choi E, Seo DH, Kim S, Park Y-R, et al. Self-perceptions of body weight status according to age-groups among Korean women: a nationwide population-based survey. PLoS ONE. 2019;14:e0210486.
Nglazi MD, Ataguba JE-O. Overweight and obesity in non-pregnant women of childbearing age in South Africa: subgroup regression analyses of survey data from 1998 to 2017. BMC Public Health. 2022;22:395.
Devericks EN, Carson MS, McCullough LE, Coleman MF, Hursting SD. The obesity-breast cancer link: a multidisciplinary perspective. Cancer Metastasis Rev. 2022;41:607–25.
Agurs-Collins T, Ross SA, Dunn BK. The many faces of obesity and its influence on Breast cancer risk. Front Oncol. 2019;9:765.
Fortner RT, Sisti J, Chai B, Collins LC, Rosner B, Hankinson SE, et al. Parity, breastfeeding, and Breast cancer risk by hormone receptor status and molecular phenotype: results from the nurses’ Health studies. Breast Cancer Res. 2019;21:1–9.
Sangaramoorthy M, Hines LM, Torres-Mejía G, Phipps AI, Baumgartner KB, Wu AH, et al. A pooled analysis of breast-feeding and Breast cancer risk by hormone receptor status in parous hispanic women. Epidemiology. 2019;30:449.
Figueroa JD, Davis Lynn BC, Edusei L, Titiloye N, Adjei E, Clegg-Lamptey J, et al. Reproductive factors and risk of Breast cancer by Tumor subtypes among Ghanaian women: a population‐based case–control study. Int J Cancer. 2020;147:1535–47.
Jelly P, Choudhary S. Breastfeeding and Breast cancer: a risk reduction strategy. Int J Med Paediatr Oncol. 2019;5:47–50.
Chen X, Wang Q, Zhang Y, Xie Q, Tan X. Physical activity and risk of Breast cancer: a meta-analysis of 38 cohort studies in 45 study reports. Value Heal. 2019;22:104–28.
Papadimitriou N, Dimou N, Tsilidis KK, Banbury B, Martin RM, Lewis SJ, et al. Physical activity and risks of breast and Colorectal cancer: a mendelian randomisation analysis. Nat Commun. 2020;11:597.
Ligibel JA, Basen-Engquist K, Bea JW. Weight Management and physical activity for Breast Cancer Prevention and Control. Am Soc Clin Oncol Educ B. 2019;39:e22–33. https://doi.org/10.1200/edbk_237423
Mcmurray RG, Harrell JS, Bangdiwala SI, Bradley CB, Deng S, Levine A. A school-based intervention can reduce body fat and blood pressure in young adolescents. J Adolesc Heal. 2002;31:125–32.
Simpson RJ, Kunz H, Agha N, Graff R. Exercise and the regulation of immune functions. Prog Mol Biol Transl Sci. 2015;135:355–80.
John EM, Phipps AI, Knight JA, Milne RL, Dite GS, Hopper JL, et al. Medical radiation exposure and Breast cancer risk: findings from the Breast Cancer Family Registry. Int J Cancer. 2007;121:386–94.
Zheng T, Holford TR, Mayne ST, Luo J, Owens PH, Zhang B, et al. Radiation exposure from diagnostic and therapeutic treatments and risk of Breast cancer. Eur J Cancer Prev. 2002;11:229–35. https://doi.org/10.1097/00008469-200206000-00006
Acknowledgements
The authors thank the study participants for providing data.
Funding
No Funding.
Author information
Authors and Affiliations
Contributions
H.F. designed the study, coordinated for data collection. F.N.T. analyzed the data drafted the manuscript. P.A.M.N. revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Ethics approval and consent to participate
Since the Bahir Dar Institute of Technology (BiT) lacks an institutional review board, we obtained ethical clearance through our partner institute, the Amhara Public Health Institute (APHI). Furthermore, we ensured the informed consent of all study participants by explaining the study’s objectives. For participants who were unable to read the consent form, healthcare providers read it aloud to them. Those who willingly volunteered to participate provided their consent by either signing the form or applying a thumb impression. We assured respondents that their names would not be disclosed, and all information provided would remain confidential. Additionally, participants were given the opportunity to ask questions about the study and had the option to refuse or discontinue their participation at any time. The APHI research review committee approved that all methods adhered to the applicable ethical standards and regulations outlined in the Declaration of Helsinki.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fentie, H., Ntenda, P.A.M. & Tiruneh, F.N. Dietary pattern and other factors of breast cancer among women: a case control study in Northwest Ethiopia. BMC Cancer 23, 1050 (2023). https://doi.org/10.1186/s12885-023-11501-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11501-1