Abstract
Background
Heterozygous isocitrate dehydrogenase (IDH) mutations occur in about half of conventional central bone chondrosarcomas (CCBC). Aim of this study was to assess the frequency and prognostic impact of IDH mutations in high grade CCBC patients.
Methods
64 patients with G2 and G3 CCBC were included. DNA extraction, PCR amplification of IDH1/2 exon 4s, and sequencing analysis with Sanger were performed.
Results
IDH mutations were detected in 24/54 patients (44%): IDH1 in 18, IDH2 in 4, and both IDH1/2 in 2 patients. The frequency of mutations was 37% in G2 vs. 69% in G3 (p = 0.039), and 100% in three Ollier disease associated chondrosarcoma. 5-year overall survival (OS) at 124 months (range 1-166) was 51%, with no significant difference based on the IDH mutational status: 61% in IDHmut vs. 44% in IDH wild type (IDHwt). The 5-year relapse free survival (RFS) was 33% (95% CI:10–57) for IDHmut vs. 57% (95%CI: 30–77) for IDHwt. Progression free survival (PFS) was 25% (95%CI:1–65) IDHmut vs. 16% (95%CI: 0.7–52) IDHwt. 55% (5/9) of IDHmut G2 became higher grade at the recurrence, as compared with 25% (3/12) of G2 IDHwt.
Conclusions
This study shows a higher frequency of IDH mutations in G3 CCBC as compared with G2. No significant differences in OS, RFS, and PFS by mutational status were detected. After relapse, a higher rate of G3 for IDH mutated CCBC was observed.
Similar content being viewed by others
Background
Cartilaginous bone sarcomas are the second most frequent bone tumors in adults with roughly 3 new cases per 106 population per year, while in children and young adults they represent only 3% of bone malignancies [1]. They include different histologic subtypes, all characterized by the production of a hyaline cartilaginous matrix, and conventional chondrosarcoma is the most common (85–90%) [2]. Conventional central bone chondrosarcoma (CBCC) arises from the inner bone, while peripheral chondrosarcoma from the surface. Both can rise as primary, de novo, lesions or from the transformation of pre-existing benign lesions, through mutations in different genes: central chondrosarcoma from enchondroma (IDH mutations), peripheral from osteochondroma (EXT1, EXT2 mutations) [3]. Dedifferentiated chondrosarcoma arises from conventional chondrosarcoma and behaves more aggressively; in the last WHO classification [2] it is considered a separate high-grade chondrosarcoma subtype, defined by a bimorphic histological appearance of a conventional chondrosarcoma component and a high-grade non-cartilaginous sarcoma (more often undifferentiated pleomorphic sarcoma or osteosarcoma, rarely it demonstrates features of angiosarcoma, leiomyosarcoma, rhabdomyosarcoma, or shows epithelial differentiation) [2]. The cartilaginous and sarcomatous components are juxtaposed, generally with an abrupt transition between them, and IDH mutations have been described in both components. In the largest series reported in literature, the percentage of dedifferentiation occurring in conventional chondrosarcomas is around 15% [2, 4,5,6].
Tumor grade is the main prognostic factor. It is defined by cellular atypia, mitoses, and cellularity [7]. Metastasis occurs exceptionally in grade 1 lesions, 10% in grade 2, but up to 70% in grade III lesions [7]. The 5-year overall survival (OS) is 80–90% for grade I but drops to about 50–60% for grade II-III conventional chondrosarcoma [8,9,10].
Surgery is the cornerstone therapy. Chemotherapy has limited efficacy in CCBC [11,12,13], comparing with dedifferentiated chondrosarcoma [14], the response rate in CCBC is low. [15, 16]. Novel therapeutic approaches urge the understanding of underlying pathogenetic mechanisms [17,18,19].
Somatic mutations in the Krebs cycle enzyme isocitrate dehydrogenase (IDH) have been described in gliomas, acute myeloid leukemia, cholangiocarcinoma, melanoma, colorectal, prostate cancer, and thyroid carcinoma [20]. In mesenchymal tumors, IDH mutations are present in about half of central cartilaginous tumors: in 52% of central low-grade, 58.9% of G2-G3 CCBC, and 56.5% of dedifferentiated chondrosarcoma [5]. Patients with Ollier disease and Maffucci syndrome carry IDH mutations with evidence of somatic and intraneoplastic mosaicism (mutation in 81% Ollier e 77% Maffucci) [21, 22].
Biological mechanisms by which cancerogenesis is induced by mutant IDH are to be fully elucidated. Mutant isoforms 1 and 2 of IDH form with the wild-type protein a heterodimeric enzyme that gains a neomorphic activity, which consists in the NADPH dependent reduction of α-ketoglutarate to D-2-hydroxyglutarate (D-2-HG). D-2-HG behaves as an oncometabolite, competitively inhibiting α-Kg-dependent dioxygenases, inducing DNA methylation rewiring, HIF1α a stabilization independently of oxygen levels, and alteration of the cellular redox balance [23,24,25,26].
IDH prognostic role is controversial in different reported series of chondrosarcoma patients [27,28,29,30,31,32,33] However, a limitation of most of these studies is the inclusion of patients with different histological types and different histological grade [34]. In addition, some of these studies are multicentric [34]. The aim of our study is to assess the frequency of IDH mutations, their relationship with clinical characteristics, and their prognostic role in patients with high grade CBCC treated in the same institution.
Methods
Study design
The aim of the study was to describe the frequency and type of IDH mutations in G2 and G3 CBCC and identify correlations with clinical characteristics and outcome. Inclusion criteria: surgery of primary tumor at our institution from 2002 to 2012, confirmed diagnosis of G2 or G3 conventional chondrosarcoma, availability of both paraffin-embedded and fresh frozen tissue samples. A comprehensive written informed consent was signed for the surgical procedure and related diagnostic procedures in accordance with the standard institutional procedure. After Ethical Institutional Committee approval, clinical data on the diagnosis, treatments, and follow-up (according to institutional guidelines) were collected retrospectively from the patient charts. Surgical margins were defined according to the Enneking score system [33].
Molecular analyses were performed on formalin-fixed and paraffin-embedded tissues (FFPET) and/or frozen tumor samples of patients included in the study. All information regarding the human material was managed using anonymous numerical codes, clinical data were not used, and samples were handled in compliance with the Helsinki declaration.
DNA extraction
Total DNA extraction from FFPET samples was performed as previously described [33]. A representative tumor area selected on hematoxylin-eosin by the pathologist, which has more than 80% tumor cells, was selected on paraffin block using Multi-Purpose Sampling Tool (Harris UNI-CORE, TedPella Inc, USA) which allows to take tissue cores from the sample, purifying DNA from two cores for each sample. With some modifications, the same QIAamp FFPE Tissue kit (Qiagen) was used for DNA purification of frozen samples. In brief, a fragment of less than 10 mg of tumor tissue was selected using scalpel blades. For each sample 180 µl of lysis buffer and 20 µl of Proteinase K Solution were added. After mechanical stirring, samples were incubated in a water bath overnight at 56 °C. Hematoxylin-eosin cryostat sections were performed to evaluate if the area of tissue selected was representative of the tumor. Quantitative and qualitative analysis was carried out on DNA obtained from both FFPET and frozen tissue by measuring the absorbance (A) in a spectrophotometer to determine the concentration and purity. DNA was considered suitable for molecular analysis only if the A260/A280 ratio was greater than 1.8.
Sequencing of polymerase chain reaction products
The PCR conditions have been previously described [33]. The Sanger sequencing was performed by Bio-Research Fab (www.biofabresearch.it, Rome, Italy). Mutation analysis was conducted with Basic Local Alignment Search Tool (BLAST), in the NCBI database “National Center of Biotechnology Information Database” (http://www.ncbi.nlm.nih.gov/BLAST). Electropherograms were exported to fasta format and were aligned to the NCBI BLAST sequences.
Statistical analysis
Continuous variables were summarized as mean and range; discrete and categorical variables were summarized using frequencies and percentages. Patient characteristics at diagnosis (age, site, grade, margins according to Enneking [35], and stage), were compared between IDH mutation using Chi-Square test. OS was defined as the time from the date of surgery to the date of death. Patients who did not experience the outcome of interest were censored at the time of last follow-up. RFS was calculated in localized patients and was defined as the time from date of surgery to the date of first relapse. PFS was calculated in metastatic patients and was defined as the time from date of surgery to the date of progression. Patients who died for surgery complications were excluded from survival analysis. Kaplan-Meier methods were used to estimate OS, RFS and PFS and the curves were compared using log-rank test. A value of p < 0.05 was considered statistically significant. All p values were 2-sided. Data were analyzed using the SAS 9.4 software (SAS Institute).
Results
Frequency and type of mutations
DNA extraction was performed on tumor samples derived from the first surgical procedure in 64 patients included in the protocol.
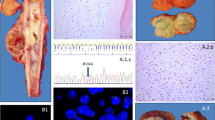
Molecular analysis was not evaluable in 10 patients, for scarcity of extracted DNA, due to aged slides and decalcification procedures. In 54/64 (84%) cases the quality of tissue was adequate: IDH mutations were detected in 24 patients (44%): in 18 IDH1mut only (34%), in 4 IDH2mut only (7%), and in 2 patients both IDH1 and 2mut (3%). IDH1 was mutated on residue 132 of arginine while IDH2 on residue 172, in the substrate-binding site. Details on mutation types are described in Table 1 and Fig. 1.
Sanger sequencing performed on IDH1 gene, exon 4. (A) Electropherogram data from a wild-type sequence in one of the tested samples; (B) chondrosarcoma sample harboring a R132C IDH1 (arrow) mutation (c.394 C>T); (C) chondrosarcoma sample harboring R132G (arrow) mutation (c.394 C>G); (D) sample harboring R132S (arrow) mutation (c.394 C>A)
Sanger sequencing performed on IDH2 gene, exon 4. (A) Electropherogram data from a wild-type sequence in one of the tested samples; (B) chondrosarcoma sample harboring a R172S (arrow) mutation (c.516 G>T); (C) chondrosarcoma sample harboring R172S (arrow) mutation (c.516 G>C); (D) sample harboring R172G (arrow) mutation (c.514 A>G)
Patients’ clinical characteristics by mutational status
Of the 54 analyzed patients 18 (33%) were males and 36 (67%) females; the median age was 63 (range 17–85 years). Distribution by site is illustrated in Fig. 2.
At the time of surgery 40 patients (74%) presented with localized disease, and 14 (26%) with lung metastases. 41 patients had G2 chondrosarcoma at pathological examination, while 13 had G3 tumors. 8 (19%) G2 patients, and 6 (42%) G3 patients presented with metastases.
A comparison of clinical characteristics between IDHmut and IDHwt cohorts is illustrated in Table 2. On histological examination, no different morphological features have been reported for mutant versus wild-type tumors.
As expected, syndromic conditions were confirmed to be a substrate for IDHmut conventional chondrosarcoma. The three chondrosarcomas of patients with Ollier syndrome (100%) harbored a mutation of IDH1, and all 3 cases shared the same mutation: R132C(TGT); none of the patients presented IDH2 mutation. One patient with Maffucci’s syndrome had a metacarpal chondrosarcoma IDH1wt and IDH2 not evaluable.
In Table 3 the comparison between G2 and G3 groups is reported.
Evolution/dedifferentiation
We observed a different grade progression over time (at relapse) in the 2 groups (IDH1/2mut or wt): IDHmut chondrosarcoma had a higher rate of grade progression at relapse, as compared to IDHwt. In particular 25 patients (21 cases presenting with G2 at diagnosis and 4 presenting with G3) had a new histologic evaluation at recurrence/progression: 5/9 (55%) of G2 IDH1/2mut tumors became higher grade at recurrence (1 became G3 and 4 dedifferentiated); while only 3/12 (25%) of G2 IDH1/2wt acquired a higher grade in the recurrence (3 became dedifferentiated).
Two IDH1wt patients developed second malignancies: 1 desmoid fibromatosis (and had had a previous prostatic adenocarcinoma) and 1 non-Hodgkin lymphoma.
Two patients with IDHmut developed a second malignancy: 1 prostatic adenocarcinoma and 1 patient with Maffucci Syndrome developed second chondrosarcoma at a different site. Three IDHmut patients with Ollier disease, had evidence of pre-existing enchondroma. Moreover, one IDH1/2 patient had evidence of enchondroma, G2 chondrosarcoma, and dedifferentiated chondrosarcoma recapitulating in his history all the phases of cancerogenesis.
Treatment
Surgery consisted o: 42 resections, 11 amputations, and 1 curettage. Wide margins were obtained in 39 pts. None of the 40 cases with localized disease received adjuvant chemotherapy. 6/14 patients metastatic at diagnosis (4 IDHmut, 2 IDHwt) underwent first line chemotherapy.
Treatment at recurrence/progression consisted of surgery (19 patients) chemotherapy (9 patients), and radiotherapy (8 patients).
Number and duration of chemotherapy lines are summarized in Fig. 3.
Chemotherapy lines and their duration. Number of chemotherapy (CT) lines in 15 patients treated with chemotherapy at recurrence/progression of disease, and duration in month for each CT line, by mutational status. Only the patient with IDH1/2 mut who received chemotherapy according to Euro-B.O.S.S. protocol [11] for a dedifferentiated recurrence, had tumor shrinkage. One patient received adjuvant chemotherapy after dedifferentiated recurrence. The other 13 patients had disease progression after 2-6 months in all chemotherapy lines: 5 of them received rapamycin and cyclophosphamide (but only one achieved a disease stabilization as best response) and 2 with hedgehog inhibitors
Outcome
Survival analysis was performed on 50 patients: 4 patients died of surgical complications and were excluded from the outcome analysis. After a median follow-up of 124 months (range 1-166) relapse occurred in 21/40 localized patients (10 IDHmut): 11 local recurrences, 5 lung metastases, 1 lymph node metastases, and 4 both local relapse and metastasis. Disease progression was reported for all metastatic patients.
The 5-years OS was 51% (95% CI:36–64), and was significantly higher in patients with localized vs. metastatic disease at diagnosis (69% vs. 7%, p < 0.001), and in patients with G2 vs. G3 (59% vs. 29%, p = 0.0078) chondrosarcoma.
The 5-years OS in IDHmut vs. IDHwt was not significantly different in the general population, nor in the split group of G2 and G3, as reported in Fig. 4a, 4b, 4c. No differences between IDHmut and IDHwt in the 5-years RFS and PFS for localized and metastatic patients respectively has been detected, as reported in Fig. 5a and 5b).
Discussion
IDH mutations were first identified in 2006 in colon cancer [36], and next in many other tumor types, but only in glioma a clear correlation between genetic alteration and disease phenotype and prognosis has been established [37].
Amary and Pansuriya pioneering works show that IDH mutations in mesenchymal tumors: 1- are prevalent in cartilaginous tumors rather than in other connective tissue sarcomas; 2- are present in 80% of benign enchondromas and in almost half of conventional chondrosarcomas; 3- occur early in the tumorigenesis; 4- both local and distant recurrences of central conventional chondrosarcoma maintain the same IDH mutational status of the primary lesion; 5- are almost always present in enchondromas of Ollier and Maffuci syndromes [21, 22, 38].
Other authors investigated on the presence and role of IDH mutations in chondrosarcomas, but most of the reported series include benign with high grade, tumors from different sites, and also different chondrosarcoma histotypes. In these series the number of G2 and G3 chondrosarcoma account from 24 to 51. [27,28,29,30,31,32,33,34]. In the current study, we decided to focus on G2-3 CCBC, in order to have a homogeneous population, reporting data on 54 patients all treated in one institution.
Although the use of sole Sanger sequencing detects somatic variants at frequency levels above 10% [39], and might lead to false-negative IDHwt cases, the results obtained were consistent with literature data: the type of mutations (R132 in IDH1 and R172 in IDH2, but not R140 in IDH2), the frequency (44%) and the IDH1 to IDH2 mutation ratio 20:6. In a future work it would be possible to confirm the wt cases with a more sensitive technique such as NGS.
The IDH mutation rate was significantly higher in G3 (69%) than in G2 (37%) tumors (p = 0.0390). At recurrence, CBCC is estimated to exhibit a higher grade of malignancy in more than 10% of cases, but the biological mechanisms involved in the progression are still unknown [9]. We observed a higher rate of grade progression at recurrence in IDHmut CBCC: 55% IDHmut vs. 25% IDH wt G2 became higher grade at relapse. One patient with IDH1/2mut G2 had evidence of pre-existing enchondroma, and developed a dedifferentiated chondrosarcoma. Taken together, our data suggest that IDH mutation is one of the events responsible for low to high grade progression, and that IDH mutant cells are more susceptible to changes toward dedifferentiation. It’s reported that p16/CDKN2A copy number variation, in IDHmut CBCC, occurs only after the onset of IDH mutation [38], and that the methylation status changes from low grade and high grade IDHmut chondrosarcoma. [40, 41].
The impact of IDH mutation on chondrosarcoma prognosis is still unclear. Stage, grade, size, and surgical margins are the main factors to consider for survival prediction in CCBC. In our series grade and stage were confirmed to be prognostic, but not the mutational status. The 5-year OS was 51%, but dropped to 7% in metastatic patients, and to 29% in G3 patients, but did not differ significantly by mutational status. The 5-year RFS was worse in IDHmut localized patients, but not statistically significant. Similarly, Lugowska et al. [27] found a shorter survival in IDH1/2mut patients, but in that series different histotypes other than CBCC have been included, while Zhou et al. [28] reported longer RFS and metastasis-free survival (MFS) in IDHmut CCBC (51 G2-3), but did not detect a significant impact of mutational status on OS. Cleven et al. [29], and Amary et al. [5] could not find differences in DFS and MFS, and survival period respectively. A meta-analysis using individual patient data from 14 studies found a significant negative impact of IDH1/2 mutations on patient survival, but not on RFS and MFS [34]. Possible explanations for the discrepancies in defining IDH mutations prognostic role between available studies could in part rely on the rarity of the disease (small sample size), heterogeneity of included population (patients with different chondrosarcoma subtypes and different grade), the employment of different sequencing tools. Moreover, even if IDH mutation is considered one of the most important drivers of chondrosarcoma, other genes seem to be involved in tumor progression (p53, Rb, histone deacetylase, and others) and may impact on patient prognosis.
Target therapies with potential activity in chondrosarcoma include antiangiogenic agents, mTOR inhibitors, hedgehog inhibitors, histone deacetylase inhibitors, immunotherapy, and, more recently, IDH inhibitors. [18, 19]. IDH inhibitors are approved for the treatment of IDHmut acute myeloid leukemia. Ivosidenib, a first-in-class selective oral IDH1 inhibitor, has shown clinical activity in preclinical studies [42, 43] and in a phase 1, open-label, multicenter study with 168 patients with advanced solid tumors. Chondrosarcoma dose-escalation and expansion cohorts included 21 patients (14 with G2-G3 CCBC) with recurrent/progressing disease: 11 (52%) achieved stable disease, and 4 of them for more than 2.5 years [43]. Ongoing trials are still recruiting chondrosarcoma patients [19] to understand the more appropriate setting for IDH1/2 inhibitors.
Conclusion
No different clinical characteristics were found between IDHwt and IDHmut high grade CCBC, except a higher frequency of mutations in syndromic patients and in G3 lesions. No statistically significant difference in prognosis was detected between IDHwt and IDHmut A different trend in histologic evolution was detected, with IDHmut G2 tumors having a higher rate of grade progression at relapse, as compared to IDHwt.
Data Availability
The Sanger sequencing data analyzed during the current study have been deposited in Genome Sequence Archive for Human and made available publicly with the accession number: HRA003467.
References
Zając AE, Kopeć S, Szostakowski B, Spałek MJ, Fiedorowicz M, Bylina E, Filipowicz P, Szumera-Ciećkiewicz A, Tysarowski A, Czarnecka AM, Rutkowski P. Chondrosarcoma-from Molecular Pathology to Novel Therapies. Cancers (Basel). 2021;13(10):2390. https://doi.org/10.3390/cancers13102390. PMID: 34069269; PMCID: PMC8155983.
WHO Classification of Tumours 5th Edition.: Soft Tissue and Bone Tumours. Edited by the WHO Classification of Tumours Editorial Board. IARC press: Lyon, France 2020; Vol 5.
Pansuriya TC, Kroon HM, Bovée JV. Enchondromatosis: insights on the different subtypes. Int J Clin Exp Pathol. 2010;3(6):557–69. PMID: 20661403; PMCID: PMC2907117.
Staals E, Cancer, Donati D, Bianchi G “Diagnosis of Musculoskeletal Tumors and Tumor-like Conditions” Chap. 34, pp.157–180;, Inwards CY, Bloem JL. Hogendoorn. Dedifferentiated Chondrosarcoma, WHO 2021, pp. 3388 – 390.
18Amary MF, Bacsi K, Maggiani F, Damato S, Halai D, Berisha F, Pollock R, O’Donnell P, Grigoriadis A, Diss T, Eskandarpour M, Presneau N, Hogendoorn PC, Futreal A, Tirabosco R, Flanagan AM. IDH1 and IDH2 mutations are frequent events in central chondrosarcoma and central and periosteal chondromas but not in other mesenchymal tumours. J Pathol. 2011;224(3):334–43. https://doi.org/10.1002/path.2913. Epub 2011 May 19. PMID: 21598255.
Meijer D, de Jong D, Pansuriya TC, van den Akker BE, Picci P, Szuhai K, Bovée JV. Genetic characterization of mesenchymal, clear cell, and dedifferentiated chondrosarcoma. Genes Chromosomes Cancer. 2012;51(10):899–909. https://doi.org/10.1002/gcc.21974. Epub 2012 Jun 4. PMID: 22674453.
Evans HL, Ayala AG, Romsdahl MM. Prognostic factors in chondrosarcoma of bone: a clinicopathologic analysis with emphasis on histologic grading. Cancer. 1977;40(2):818–31. https://doi.org/10.1002/1097-0142(197708)40:2<818::aid-cncr2820400234>3.0.co;2-b. PMID: 890662.
Mavrogenis AF, Gambarotti M, Angelini A, Palmerini E, Staals EL, Ruggieri P, Papagelopoulos PJ. Chondrosarcomas revisited. Orthopedics. 2012;35(3):e379-90. https://doi.org/10.3928/01477447-20120222-30. PMID: 22385450.
Gelderblom H, Hogendoorn PC, Dijkstra SD, van Rijswijk CS, Krol AD, Taminiau AH, Bovée JV. The clinical approach towards chondrosarcoma. Oncologist. 2008;13(3):320-9. https://doi.org/10.1634/theoncologist.2007-0237. Erratum in: Oncologist. 2008;13(5):618. PMID: 18378543.
Bongers MER, Karhade AV, Setola E, Gambarotti M, Groot OQ, Erdoğan KE, Picci P, Donati DM, Schwab JH, Palmerini E. How does the skeletal Oncology Research Group Algorithm’s prediction of 5-year Survival in patients with Chondrosarcoma perform on International Validation? Clin Orthop Relat Res. 2020;478(10):2300–8. https://doi.org/10.1097/CORR.0000000000001305. PMID: 32433107; PMCID: PMC7491905.
ESMO/European Sarcoma Network Working Group. Bone sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25 Suppl 3:iii113-23. https://doi.org/10.1093/annonc/mdu256. Erratum in: Ann Oncol. 2015;26 Suppl 5:v174-7. PMID: 25210081.
Bovée JV, Hogendoorn PC, Wunder JS, Alman BA. Cartilage tumours and bone development: molecular pathology and possible therapeutic targets. Nat Rev Cancer. 2010;10(7):481–8. https://doi.org/10.1038/nrc2869. Epub 2010 Jun 10. PMID: 20535132.
Monga V, Mani H, Hirbe A, Milhem M. Non-conventional treatments for Conventional Chondrosarcoma. Cancers (Basel). 2020;12(7):1962. https://doi.org/10.3390/cancers12071962. PMID: 32707689; PMCID: PMC7409290.
Hompland I, Ferrari S, Bielack S, Palmerini E, Hall KS, Picci P, Hecker-Nolting S, Donati DM, Blattmann C, Bjerkehagen B, Staals E, Kager L, Gambarotti M, Kühne T, Eriksson M, Ferraresi V, Kevric M, Biagini R, Baumhoer D, Brosjø O, Comandone A, Schwarz R, Bertulli R, Kessler T, Hansson L, Apice G, Heydrich BN, Setola E, Flörcken A, Ruggieri P, Krasniqi F, Hofmann-Wackersreuther G, Casali P, Reichardt P, Smeland S. Outcome in dedifferentiated chondrosarcoma for patients treated with multimodal therapy: Results from the EUROpean Bone Over 40 Sarcoma Study. Eur J Cancer. 2021;151:150–158. https://doi.org/10.1016/j.ejca.2021.04.017. Epub 2021 May 11. PMID: 33990016.
Italiano A, Mir O, Cioffi A, Palmerini E, Piperno-Neumann S, Perrin C, Chaigneau L, Penel N, Duffaud F, Kurtz JE, Collard O, Bertucci F, Bompas E, Le Cesne A, Maki RG, Ray Coquard I, Blay JY. Advanced chondrosarcomas: role of chemotherapy and survival. Ann Oncol. 2013;24(11):2916–22. https://doi.org/10.1093/annonc/mdt374. Epub 2013 Oct 7. PMID: 24099780; PMCID: PMC3811906.
Fox E, Patel S, Wathen JK, Schuetze S, Chawla S, Harmon D, Reinke D, Chugh R, Benjamin RS, Helman LJ. Phase II study of sequential gemcitabine followed by docetaxel for recurrent ewing sarcoma, osteosarcoma, or unresectable or locally recurrent chondrosarcoma: results of Sarcoma Alliance for Research through collaboration Study 003. Oncologist. 2012;17(3):321. https://doi.org/10.1634/theoncologist.2010-0265. Epub 2012 Feb 23. PMID: 22363068; PMCID: PMC3316916.
Jones RL, Katz D, Loggers ET, Davidson D, Rodler ET, Pollack SM. Clinical benefit of antiangiogenic therapy in advanced and metastatic chondrosarcoma. Med Oncol. 2017;34(10):167. https://doi.org/10.1007/s12032-017-1030-2. PMID: 28852958; PMCID: PMC5574947.
Polychronidou G, Karavasilis V, Pollack SM, Huang PH, Lee A, Jones RL. Novel therapeutic approaches in chondrosarcoma. Future Oncol. 2017;13(7):637–48. https://doi.org/10.2217/fon-2016-0226. Epub 2017 Jan 30. PMID: 28133974.
Cojocaru E, Wilding C, Engelman B, et al. Is the IDH mutation a good target for Chondrosarcoma Treatment? Curr Mol Bio Rep. 2020;6:1–9. https://doi.org/10.1007/s40610-020-00126-z.
Clark O, Yen K, Mellinghoff IK. Molecular Pathways: Isocitrate dehydrogenase mutations in Cancer. Clin Cancer Res. 2016;22(8):1837–42. https://doi.org/10.1158/1078-0432.CCR-13-1333. Epub 2016 Jan 27. PMID: 26819452; PMCID: PMC4834266.
Amary MF, Damato S, Halai D, Eskandarpour M, Berisha F, Bonar F, McCarthy S, Fantin VR, Straley KS, Lobo S, Aston W, Green CL, Gale RE, Tirabosco R, Futreal A, Campbell P, Presneau N, Flanagan AM. Ollier disease and Maffucci syndrome are caused by somatic mosaic mutations of IDH1 and IDH2. Nat Genet. 2011;43(12):1262-5. https://doi.org/10.1038/ng.994. PMID: 22057236.
Pansuriya TC, van Eijk R, d’Adamo P, van Ruler MA, Kuijjer ML, Oosting J, Cleton-Jansen AM, van Oosterwijk JG, Verbeke SL, Meijer D, van Wezel T, Nord KH, Sangiorgi L, Toker B, Liegl-Atzwanger B, San-Julian M, Sciot R, Limaye N, Kindblom LG, Daugaard S, Godfraind C, Boon LM, Vikkula M, Kurek KC, Szuhai K, French PJ, Bovée JV. Somatic mosaic IDH1 and IDH2 mutations are associated with enchondroma and spindle cell hemangioma in Ollier disease and Maffucci syndrome. Nat Genet. 2011;43(12):1256–61. https://doi.org/10.1038/ng.1004. PMID: 22057234; PMCID: PMC3427908.
Lu C, Venneti S, Akalin A, Fang F, Ward PS, Dematteo RG, Intlekofer AM, Chen C, Ye J, Hameed M, Nafa K, Agaram NP, Cross JR, Khanin R, Mason CE, Healey JH, Lowe SW, Schwartz GK, Melnick A, Thompson CB. Induction of sarcomas by mutant IDH2. Genes Dev. 2013;27(18):1986–98. https://doi.org/10.1101/gad.226753.113. PMID: 24065766; PMCID: PMC3792475.
Hirata M, Sasaki M, Cairns RA, Inoue S, Puviindran V, Li WY, Snow BE, Jones LD, Wei Q, Sato S, Tang YJ, Nadesan P, Rockel J, Whetstone H, Poon R, Weng A, Gross S, Straley K, Gliser C, Xu Y, Wunder J, Mak TW, Alman BA. Mutant IDH is sufficient to initiate enchondromatosis in mice. Proc Natl Acad Sci U S A. 2015;112(9):2829–34. https://doi.org/10.1073/pnas.1424400112. Epub 2015 Feb 17. PMID: 25730874; PMCID: PMC4352794.
Li L, Hu X, Eid JE, Rosenberg AE, Wilky BA, Ban Y, Sun X, Galoian K, DeSalvo J, Yue J, Chen XS, Blonska M, Trent JC. Mutant IDH1 depletion downregulates integrins and impairs Chondrosarcoma Growth. Cancers (Basel). 2020;12(1):141. https://doi.org/10.3390/cancers12010141. PMID: 31935911; PMCID: PMC7017040.
Pirozzi CJ, Yan H. The implications of IDH mutations for cancer development and therapy. Nat Rev Clin Oncol. 2021;18(10):645–61. https://doi.org/10.1038/s41571-021-00521-0. Epub 2021 Jun 15. PMID: 34131315.
Lugowska I, Teterycz P, Mikula M, Kulecka M, Kluska A, Balabas A, Piatkowska M, Wagrodzki M, Pienkowski A, Rutkowski P, Ostrowski J. IDH1/2 mutations predict shorter survival in Chondrosarcoma. J Cancer. 2018;9(6):998–1005. https://doi.org/10.7150/jca.22915. PMID: 29581779; PMCID: PMC5868167.
Zhu GG, Nafa K, Agaram N, Zehir A, Benayed R, Sadowska J, Borsu L, Kelly C, Tap WD, Fabbri N, Athanasian E, Boland PJ, Healey JH, Berger MF, Ladanyi M, Hameed M. Genomic profiling identifies Association of IDH1/IDH2 mutation with longer relapse-free and metastasis-free survival in High-Grade Chondrosarcoma. Clin Cancer Res. 2020;26(2):419–27. https://doi.org/10.1158/1078-0432.CCR-18-4212. Epub 2019 Oct 15. PMID: 31615936; PMCID: PMC6980683.
Cleven AHG, Suijker J, Agrogiannis G, Briaire-de Bruijn IH, Frizzell N, Hoekstra AS, Wijers-Koster PM, Cleton-Jansen AM, Bovée JVMG. IDH1 or -2 mutations do not predict outcome and do not cause loss of 5-hydroxymethylcytosine or altered histone modifications in central chondrosarcomas. Clin Sarcoma Res. 2017;7:8. https://doi.org/10.1186/s13569-017-0074-6. PMID: 28484589; PMCID: PMC5418698.
Tarpey PS, Behjati S, Cooke SL, Van Loo P, Wedge DC, Pillay N, Marshall J, O’Meara S, Davies H, Nik-Zainal S, Beare D, Butler A, Gamble J, Hardy C, Hinton J, Jia MM, Jayakumar A, Jones D, Latimer C, Maddison M, Martin S, McLaren S, Menzies A, Mudie L, Raine K, Teague JW, Tubio JM, Halai D, Tirabosco R, Amary F, Campbell PJ, Stratton MR, Flanagan AM, Futreal PA. Frequent mutation of the major cartilage collagen gene COL2A1 in chondrosarcoma. Nat Genet. 2013;45(8):923–6. https://doi.org/10.1038/ng.2668. Epub 2013 Jun 16. PMID: 23770606; PMCID: PMC3743157.
Chen S, Fritchie K, Wei S, Ali N, Curless K, Shen T, Brini AT, Latif F, Sumathi V, Siegal GP, Cheng L. Diagnostic utility of IDH1/2 mutations to distinguish dedifferentiated chondrosarcoma from undifferentiated pleomorphic sarcoma of bone. Hum Pathol. 2017;65:239–246. https://doi.org/10.1016/j.humpath.2017.05.015. Epub 2017 May 25. Erratum in: Hum Pathol. 2017;69:143. PMID: 28552826.
Tallegas M, Miquelestorena-Standley É, Labit-Bouvier C, Badoual C, Francois A, Gomez-Brouchet A, Aubert S, Collin C, Tallet A, de Pinieux G. IDH mutation status in a series of 88 head and neck chondrosarcomas: different profile between tumors of the skull base and tumors involving the facial skeleton and the laryngotracheal tract. Hum Pathol. 2019;84:183–191. doi: 10.1016/j.humpath.2018.09.015. Epub 2018 Oct 5. PMID: 30296521.
Asioli S, Ruengwanichayakun P, Zoli M, Guaraldi F, Sollini G, Greco P, Facco C, Gibertoni D, Jiménez BV, Benini S, Turri-Zanoni M, Pasquini E, Mazzatenta D, Foschini MP, Righi A. Association of Clinicopathological features with outcome in Chondrosarcomas of the Head and Neck. Otolaryngol Head Neck Surg. 2021;164(4):807–14. Epub 2020 Sep 15. PMID: 32928034.
Vuong HG, Ngo TNM, Dunn IF. Prognostic importance of IDH mutations in chondrosarcoma: an individual patient data meta-analysis. Cancer Med. 2021;10(13):4415–23. https://doi.org/10.1002/cam4.4019. Epub 2021 Jun 3. PMID: 34085407; PMCID: PMC8267117.
Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980 Nov-Dec;(153):106 – 20. PMID: 7449206.
Sjöblom T, Jones S, Wood LD, Parsons DW, Lin J, Barber TD, Mandelker D, Leary RJ, Ptak J, Silliman N, Szabo S, Buckhaults P, Farrell C, Meeh P, Markowitz SD, Willis J, Dawson D, Willson JK, Gazdar AF, Hartigan J, Wu L, Liu C, Parmigiani G, Park BH, Bachman KE, Papadopoulos N, Vogelstein B, Kinzler KW, Velculescu VE. The consensus coding sequences of human breast and colorectal cancers. Science. 2006;314(5797):268–74. https://doi.org/10.1126/science.1133427. Epub 2006 Sep 7. PMID: 16959974.
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, Kos I, Batinic-Haberle I, Jones S, Riggins GJ, Friedman H, Friedman A, Reardon D, Herndon J, Kinzler KW, Velculescu VE, Vogelstein B, Bigner DD. IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009;360(8):765–73. https://doi.org/10.1056/NEJMoa0808710. PMID: 19228619; PMCID: PMC2820383.
Amary MF, Ye H, Forbes G, Damato S, Maggiani F, Pollock R, Tirabosco R, Flanagan AM. Isocitrate dehydrogenase 1 mutations (IDH1) and p16/CDKN2A copy number change in conventional chondrosarcomas. Virchows Arch. 2015;466(2):217–22. https://doi.org/10.1007/s00428-014-1685-4. Epub 2014 Nov 29. PMID: 25432631; PMCID: PMC4325180.
Rohlin A, Wernersson J, Engwall Y, Wiklund L, Björk J, Nordling M. Parallel sequencing used in detection of mosaic mutations: comparison with fourdiagnostic DNA screening techniques. Hum Mutat. 2009;30:1012–20. https://doi.org/10.1002/humu.20980.
Nicolle R, Ayadi M, Gomez-Brouchet A, Armenoult L, Banneau G, Elarouci N, Tallegas M, Decouvelaere AV, Aubert S, Rédini F, Marie B, Labit-Bouvier C, Reina N, Karanian M, le Nail LR, Anract P, Gouin F, Larousserie F, de Reyniès A, de Pinieux G. Integrated molecular characterization of chondrosarcoma reveals critical determinants of disease progression. Nat Commun. 2019;10(1):4622. https://doi.org/10.1038/s41467-019-12525-7. PMID: 31604924; PMCID: PMC6789144.
Venneker S, Kruisselbrink AB, Baranski Z, Palubeckaite I, Briaire-de Bruijn IH, Oosting J, French PJ, Danen EHJ, Bovée JVMG. Beyond the influence of IDH mutations: exploring epigenetic vulnerabilities in Chondrosarcoma. Cancers (Basel). 2020;12(12):3589. https://doi.org/10.3390/cancers12123589. PMID: 33266275; PMCID: PMC7760027.
Li L, Paz AC, Wilky BA, Johnson B, Galoian K, Rosenberg A, Hu G, Tinoco G, Bodamer O, Trent JC. Treatment with a small molecule mutant IDH1 inhibitor suppresses tumorigenic activity and decreases production of the Oncometabolite 2-Hydroxyglutarate in human chondrosarcoma cells. PLoS ONE. 2015;10(9):e0133813. https://doi.org/10.1371/journal.pone.0133813. PMID: 26368816; PMCID: PMC4569544.
Tap WD, Villalobos VM, Cote GM, Burris H, Janku F, Mir O, Beeram M, Wagner AJ, Jiang L, Wu B, Choe S, Yen K, Gliser C, Fan B, Agresta S, Pandya SS, Trent JC. Phase I study of the mutant IDH1 inhibitor ivosidenib: safety and clinical activity in patients with Advanced Chondrosarcoma. J Clin Oncol. 2020;38(15):1693–701. Epub 2020 Mar 24. PMID: 32208957; PMCID: PMC7238491.
Acknowledgements
Thanks to Associazione Mario Campanacci.
We are grateful to Biobank (MUSCOLO SKELETAL TUMOR BIOBANK- BIOBANCA DEI TUMORI MUSCOLOSCHELETRICI (BIOTUM)) member of the CRB-IOR —which provided us the biological samples.
Thanks to Cecilia Foglini, for support in data deposition process.
Funding
This work was supported by Ministero della Salute (5 × 1000, contributions to the IRCCS, Istituto Ortopedico Rizzoli).
Author information
Authors and Affiliations
Contributions
S. E., B. S, R. A.: conceptualization, methodology, validation, investigation, data curation, writing original draft, writing review and editing, project administration.C. E.: formal analyses, data curation, writing original draft, writing review and editing.G. G., F. C, M. G., (A) S., P. E., G. M.: investigation, data curation, writing review and editing.L. A., (B) N., D. M. D., L. P. L.: conceptualization, methodology, investigation, resources, supervision, All authors: writing review and editing. All authors have approved the submitted versionAll authors have agreed both to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the they were not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Comprehensive written informed consent was signed for the surgical procedure and related diagnostic procedures in accordance with the standard institutional procedure.
All information regarding the human material was managed using anonymous numerical codes, clinical data were not used, and samples were handled in compliance with the Helsinki declaration.
Ethics approval and consent to participate
The study has been approved by Ethical Institutional Committee CE-AVEC (Comitato Etico di Area Vasta Emilia Centro, regione Emilia Romagna) under the name “IDH-Chondro” protocol.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Setola, E., Benini, S., Righi, A. et al. IDH mutations in G2-3 conventional central bone chondrosarcoma: a mono institutional experience. BMC Cancer 23, 907 (2023). https://doi.org/10.1186/s12885-023-11396-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11396-y