Abstract
Background
Pembrolizumab is a first-line therapy for certain patients with advanced/metastatic non-small cell lung cancer (NSCLC). Combining pembrolizumab with other immunotherapies may enhance tumor cell killing and clinical outcomes. Epacadostat is a selective inhibitor of indoleamine 2,3-dioxygenase 1, an immuno-regulatory enzyme involved in tryptophan to kynurenine metabolism that inhibits T cell-mediated immune responses.
Methods
In this randomized phase II study, patients with metastatic NSCLC expressing high (≥ 50%) programmed death-ligand 1 (PD-L1) levels received pembrolizumab 200 mg every 21 days plus oral epacadostat 100 mg twice daily (combination) or matching placebo (control). The primary objective was objective response rate (ORR); secondary objectives were progression-free survival (PFS), overall survival (OS), duration of response (DOR) and safety/tolerability.
Results
154 patients were randomized (77 per group). Median (range) follow-up was 6.8 months (0.1–11.4) and 7.0 months (0.2–11.9) in the combination and control groups, respectively Confirmed ORR was similar between groups (combination: 32.5%, 95% CI 22.2–44.1; control: 39.0%, 95% CI 28.0–50.8; difference: − 6.5, 95% CI − 21.5 to 8.7; 1-sided P = 0.8000). Median (range) DOR was 6.2 months (1.9 + to 6.5 +) and not reached (1.9 + to 8.6 +) in the combination and control groups, respectively. Although not formally tested, median PFS was 6.7 and 6.2 months for the combination and control groups, respectively, and median OS was not reached in either group. Circulating kynurenine levels increased from C1D1 to C2D1 (P < 0.01) in the control group and decreased from C1D1 to C2D1 (P < 0.01) in the combination group but were not normalized in most patients. The most frequent serious adverse events (AEs) (≥ 2%) were pneumonia (4.0%), anemia (2.7%), atelectasis (2.7%) and pneumonitis (2.7%) in the combination group and pneumonia (3.9%), pneumonitis (2.6%) and hypotension (2.6%) in the control group. Two deaths due to drug-related AEs were reported, both in the control group.
Conclusions
Addition of epacadostat to pembrolizumab therapy for PD-L1–high metastatic NSCLC was generally well tolerated but did not demonstrate an improved therapeutic effect. Evaluating higher doses of epacadostat that normalize kynurenine levels when given in combination with checkpoint inhibitors may be warranted.
Trial registration
ClinicalTrials.gov, NCT03322540. Registered 10/26/2017.
Similar content being viewed by others
Background
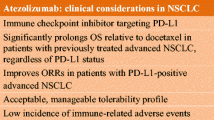
Approximately 84% of all lung cancers are non-small cell lung cancers (NSCLC) [1]. At diagnosis, most patients with NSCLC have advanced disease, which is generally not curable [1, 2]. Pembrolizumab monotherapy is the current first-line standard-of-care therapy for patients with advanced or metastatic NSCLC tumors expressing programmed death-ligand 1 (PD-L1) and with no EGFR or ALK genomic tumor aberrations [3,4,5,6]. However, there are multiple ways cancer cells escape the host immune response [7]. Combining pembrolizumab with other immunotherapy approaches may provide enhanced immune-mediated killing of tumor cells and further increase therapeutic benefit.
Indoleamine 2,3-dioxygenase 1 (IDO1) is an immuno-regulatory enzyme involved in the metabolism of tryptophan to kynurenine [8]. Upregulated expression of the IDO1 enzyme is associated with dampened anticancer T-cell immunity [8, 9]). Many human tumor types constitutively express IDO1 [8, 10]. Co-expression of IDO1 and PD-L1 is found in some NSCLC tumors, but different studies have reported varying degrees of co-expression [11,12,13]. Furthermore, regardless of baseline expression levels, IDO1 can counter anticancer inflammatory immune responses because it is induced by interferon-y [8, 14,15,16,17]. Thus, IDO1 inhibition may facilitate the activity of checkpoint inhibitors by preventing this resistance mechanism. Epacadostat is a potent selective oral inhibitor of IDO1 [18, 19]; twice-daily (BID) epacadostat monotherapy at doses ≥ 100 mg in patients with advanced solid tumors reduced plasma kynurenine to levels observed in healthy volunteers [19].
A number of clinical trials were initiated to investigate the potential of combining epacadostat and pembrolizumab to improve outcomes in several cancers, including NSCLC. Promising efficacy was observed in the melanoma and a NSCLC cohort of the phase I/II ECHO-202/KEYNOTE-037 study [20] assessing epacadostat plus pembrolizumab for advanced tumors. For patients with previously treated NSCLC, the objective response rate (ORR) was 24.4% in the PD-L1 tumor proportion score (TPS) < 50% group. In a small number of patients with NSCLC and PD-L1 TPS ≥ 50%, the ORR was 30.8% [21]. Here, we present results from the primary analysis of a randomized phase II study assessing the safety and efficacy of epacadostat plus pembrolizumab (combination) versus placebo plus pembrolizumab (control) in patients with metastatic NSCLC expressing high levels of PD-L1 (TPS ≥ 50%) (NCT03322540).
Methods
Study design and conduct
ECHO-305/KEYNOTE-654 was a multicenter, active-controlled, double-blind, parallel-group randomized phase II study. This study was originally designed as a phase III study. On May 31, 2018, the protocol was amended to a phase II study after emerging data from the phase III ECHO-301/KEYNOTE-252 study in unresectable or metastatic melanoma showed that addition of epacadostat to pembrolizumab did not improve the primary endpoint of progression-free survival (PFS) [22]. Specific changes made in this protocol amendment are detailed in the relevant methods sections below.
This study conformed to the ethical principles of the Declaration of Helsinki, Good Clinical Practice, and applicable country and/or local statutes and regulations.
Study population
Patients ≥ 18 years old with previously untreated, confirmed stage IV NSCLC not suitable for primary EGFR-, ALK- or ROS1-directed therapy and measurable disease per Response Evaluation Criteria in Solid Tumors version 1.1 (RECIST v1.1), an Eastern Cooperative Oncology Group performance status (ECOG PS) of 0 or 1, and tumor tissue with PD-L1 TPS ≥ 50% were eligible. Exclusion criteria included any prior treatment for metastatic NSCLC and untreated central nervous system metastases and/or carcinomatous meningitis.
Study procedure and interventions
Patients were randomized to receive treatment in one of two arms: epacadostat plus pembrolizumab (combination) or placebo plus pembrolizumab (control). The stratification factors in the original study design were tumor histology (squamous vs. nonsquamous), ECOG PS and geographical region. The protocol amendment changing the study to a phase II study updated the study design so that tumor histology (squamous vs. nonsquamous) was the only stratification factor.
Pembrolizumab 200 mg was administered intravenously every 21 days (day 1 of each cycle) for up to 35 doses and epacadostat 100 mg or matching placebo was administered orally BID. Pembrolizumab could be withheld for up to 12 weeks from the last dose to mitigate immune-related adverse events (AEs). Epacadostat could be reduced to 50 or 25 mg BID to mitigate immune-related AEs. Discontinuation of study therapy due to disease progression was based on immune-related RECIST criteria (iRECIST) as evaluated by investigators. Blood was drawn from fasted patients before dosing, on day 1 of cycle 1 (C1D1) and day 1 of cycle 2 (C2D1). Serum kynurenine levels were determined by a proprietary validated liquid chromatography–tandem mass spectrometry assay using calibrated standards at Worldwide Clinical Trials, Morrisville, NC.
Study objectives and endpoints
In the original study design, the primary endpoints were overall survival (OS) and PFS. The protocol amendment changed the study to a phase II study with the primary objective comparing ORR of the combination and control groups. Response and disease progression were assessed by blinded independent central review (BICR) based on modified RECIST v1.1 criteria allowing a maximum of 10 target lesions in total and five per organ. The secondary objectives were PFS, OS, duration of response (DOR) and safety/tolerability. National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) version 4.0 was used to grade and record AEs. The pharmacodynamic activity of epacadostat, assessed by changes in circulating kynurenine levels from baseline, was among the exploratory objectives.
Statistical analyses
Originally, 588 patients were planned for enrollment in the phase III study. Target enrollment was reduced to 148 patients when the study was amended to a phase II study. The efficacy analysis included all randomized patients (i.e., the intention-to-treat population), and the safety analysis included all patients who received at least one treatment dose. ORR was compared between treatment arms using the Miettinen and Nurminen method [23] stratified by predominant tumor histology (squamous vs. non-squamous). Based on the number of patients planned to be randomized (N = 148), the study had 81.7% power to detect a 20-percentage point difference in ORR between combination and control groups at α = 5% (one-sided). PFS and OS were compared between treatment arms using a stratified log-rank test. Event rates were estimated using the Kaplan–Meier method, and hazard ratios (HRs) were estimated using a stratified Cox regression model with Efron’s method of tie handling. Circulating kynurenine levels were compared within each treatment arm using paired t-tests.
Results
Patient characteristics
A total of 154 patients were randomized (1:1) to combination (n = 77) or control (n = 77) treatment arms (Fig. 1). Most patients remained in the study at data cutoff. The majority were male, white, non-Hispanic or Latino, older than 65 years of age, former smokers, with an ECOG PS of 1 and a metastatic stage of M1c (with a slightly higher occurrence in the combination group) (Table 1). More patients were older than 65 years in the control group compared with the combination group. The predominant tumor histology was balanced between the combination and control groups.
Treatment duration
The median number of days on treatment, days on pembrolizumab, and days on epacadostat/placebo were all similar for both treatment groups (see Additional file 1). The median follow-up was 6.8 months (range 0.1–11.4) in the combination group and 7.0 months (range 0.2–11.9) in the control group. Upon study termination, treatments were unblinded and epacadostat was discontinued. All remaining patients had the option to continue open-label pembrolizumab monotherapy.
Efficacy
The confirmed ORR based on BICR was similar in both treatment groups at 32.5% (95% confidence interval [CI] 22.2–44.1) in the combination group compared with 39.0% (95% CI 28.0–50.8) in the control group (Table 2). The difference in estimated ORR percentage between groups was − 6.5 (95% CI − 21.5 to 8.7; one-sided P = 0.8000). More patients in the control group (39.0%) had a best overall response of partial response compared with the combination group (32.5%), while more patients in the combination group had a best overall response of stable disease (41.6%) compared with the control group (29.9%). The disease control rate was numerically higher in the combination group compared with the control group. The median DOR in the combination and control group was 6.2 months (range 1.9 + to 6.5 +) and not reached (range 1.9 + to 8.6 +), respectively (plus symbols indicate no progressive disease at the time of last disease assessment) (Table 2).
At data cutoff, PFS data were not conclusive, with 71 of the 95 required PFS events having been reported (37/77 [48.1%] in the combination group; 34/77 [44.2%] in the control group) (Fig. 2A, Table 3). Median PFS was 6.7 months for the combination group and 6.2 months for the control group (HR 1.10, 95% CI 0.69–1.76). The PFS rates at 3 and 6 months were similar for both groups. The median OS was not reached in either group (combination: 13 events; control: 17 events; HR 0.74, 95% CI 0.36–1.52) (Fig. 2B, Table 3).
Subgroup analyses showed results similar to those from the overall analyses (ORR, PFS and OS) (data on file). Subgroups included predominant tumor histology, age, gender, race (white vs. nonwhite), smoking status, geographic region (East Asian vs. non-East Asian), baseline ECOG status, baseline metastatic stage and history of brain metastasis. Investigator assessments were consistent with BICR assessments for ORR, PFS and DOR.
Safety and tolerability
The proportions of patients with AEs, drug-related AEs, grade ≥ 3 AEs, drug-related grade ≥ 3 AEs, serious AEs (SAEs) and drug-related SAEs were similar between treatment groups (Table 4). The most frequent SAEs (≥ 2%) in the combination group were pneumonia (4.0%), anemia (2.7%), atelectasis (2.7%) and pneumonitis (2.7%) and in the control group pneumonia (3.9%), pneumonitis (2.6%) and hypotension (2.6%). All drug-related SAEs were reported by ≤ 2 patients. Two deaths due to drug-related AEs were reported in the control group, one from pneumonia and the other from respiratory failure. No deaths due to drug-related AEs were reported in the combination group.
Pharmacodynamic activity of epacadostat
Median baseline levels of circulating kynurenine in both treatment arms (Fig. 3) were numerically above that observed in healthy subjects (1.5 μM) [19]. Compared with baseline levels (C1D1), median circulating kynurenine levels were reduced after one cycle of treatment (C2D1) in the combination group (2.3 µM vs. 1.8 µM; P < 0.01), albeit not to levels reported in healthy volunteers. The opposite was observed for the control group where compared with C1D1, median circulating kynurenine levels were increased at C2D1 (2.1 µM vs. 2.6 µM; P < 0.01).
Circulating kynurenine levels at baseline (C1D1) and after one cycle of treatment (C2D1). The number of samples assessed was 56 in the pembrolizumab plus placebo group and 57 in the pembrolizumab plus epacadostat group. Kynurenine levels at C1D1 and C2D1 were compared using paired t-tests within each treatment arm. The dotted line indicates median kynurenine levels in healthy subjects (1.5 μM) [19]. C cycle, D day
Discussion
In the ECHO-305/KEYNOTE-654 study, the addition of epacadostat 100 mg BID to pembrolizumab did not improve ORR in patients with previously untreated metastatic PD-L1 TPS ≥ 50% NSCLC. The PFS data were not conclusive to confirm an effect of combination therapy with epacadostat plus pembrolizumab. Although baseline characteristics were generally balanced between treatment arms, a higher proportion of M1C patients in the combination arm may have affected ORR comparisons between arms. The combination of epacadostat plus pembrolizumab was generally well tolerated with an acceptable safety profile that was generally consistent with that of pembrolizumab monotherapy with respect to AEs and treatment discontinuations due to AEs. No new safety concerns were identified.
This study was based on the phase III KEYNOTE-024 [5] and the phase I/II ECHO-202/KEYNOTE-037 [20] studies. The ORR of the epacadostat plus pembrolizumab group in the current study (32.5%) was similar to that in the open-label PD-L1 TPS ≥ 50% group in ECHO-202/KEYNOTE-037 (30.8%) [21]. Also, the ORR of the placebo plus pembrolizumab group in this study (39.0%) was similar to that in the pembrolizumab monotherapy group of the phase III KEYNOTE-024 study (44.8%), which also included patients with previously untreated, PD-L1 TPS ≥ 50% NSCLC [5]. Finally, OS rates at 6 months were also similar between the placebo plus pembrolizumab group in this study (81.5%) and the pembrolizumab monotherapy group of the KEYNOTE-024 study (80.2%) [5].
The findings of this study are consistent with results reported in this supplement from the ECHO-306/KEYNOTE-715 study in NSCLC [24] and also with the previously published ECHO-301/KEYNOTE-252 study in metastatic melanoma [22]. ECHO-306/KEYNOTE-715 assessed epacadostat 100 mg BID plus pembrolizumab with chemotherapy in NSCLC [24]; however, enrollment did not require PD-L1 TPS ≥ 50%. The ECHO-301/KEYNOTE-252 study in metastatic melanoma showed that the addition of epacadostat 100 mg BID to pembrolizumab did not improve the primary endpoint of PFS [22].
The pharmacodynamic findings reported here show that circulating kynurenine levels were increased after treatment with pembrolizumab monotherapy. This is consistent with reports suggesting that anti-PD-1 treatment may stimulate IDO1 expression by inducing interferon production [16, 25]. Although epacadostat (≥ 100 mg BID) monotherapy was previously shown to normalize circulating kynurenine levels in patients with solid tumors [19], the addition of epacadostat 100 mg BID to pembrolizumab in our study only reduced pembrolizumab-associated increases in circulating kynurenine levels but did not normalize these levels, and durability of the effect was not evaluated. Similar findings and their interpretation regarding the effects of epacadostat and pembrolizumab on circulating kynurenine levels were reported in patients with urothelial carcinoma [26]. To overcome pembrolizumab-induced kynurenine production, higher doses of epacadostat than those tested in prior monotherapy studies may be needed, and this may be investigated in future combination clinical trials. This rationale is supported by longitudinal plasma kynurenine data from a retrospective pooled analysis of clinical studies evaluating epacadostat in combination with a checkpoint inhibitor. These data showed that epacadostat 100 or 300 mg BID in combination with a checkpoint inhibitor did not control plasma kynurenine levels, whereas epacadostat ≥ 600 mg BID durably controlled plasma and intratumoral kynurenine levels [27]. It should be noted that limitations of plasma kynurenine as a pharmacodynamic biomarker have been described, [28] and studies evaluating other markers to guide epacadostat dose selection may be warranted.
Combined inhibition of IDO1 and programmed cell death protein-1 (PD-1)/PD-L1 were also evaluated in other advanced solid tumors, including the phase I/II ECHO-204 study assessing epacadostat plus PD-1 inhibitor nivolumab [29] and a phase I study assessing IDO1 inhibitor navoximod with PD-L1 inhibitor atezolizumab [30]. These studies have reported preliminary antitumor activity in certain cancers. Clarification of patient populations that could benefit from combined IDO1 and PD-1/PD-L1 inhibition through identification of associated biomarkers could guide further investigation in clinical trials.
This study was limited by its small sample size and short median follow-up. Other limitations include that the study design was changed from phase III to phase II during the study and that the study was discontinued early.
Conclusions
In this primary analysis, addition of epacadostat 100 mg BID to pembrolizumab therapy for metastatic NSCLC was generally well tolerated but did not demonstrate improved outcomes when compared with placebo plus pembrolizumab. However, the pharmacodynamic findings suggest that further combination studies testing higher doses of epacadostat and using circulating kynurenine levels or other appropriate pharmacodynamic biomarkers to guide dose selection are warranted.
Availability of data and materials
Access to individual patient-level data is not available for this study.
Abbreviations
- AE:
-
Adverse event
- BICR:
-
Blinded independent central review
- BID:
-
Twice daily
- C#D#:
-
Cycle # day #
- CI:
-
Confidence interval
- CR:
-
Complete response
- DOR:
-
Duration of response
- ECOG PS:
-
Eastern Cooperative Oncology Group performance status
- HR:
-
Hazard ratio
- IDO1:
-
Indoleamine 2,3-dioxygenase 1
- iRECIST:
-
Immune-related Response Evaluation Criteria in Solid Tumors
- MedDRA:
-
Medical Dictionary for Regulatory Activities
- NCI CTCAE:
-
National Cancer Institute Common Terminology Criteria for Adverse Events
- NE:
-
Not evaluable
- NR:
-
Not reached
- NSCLC:
-
Non-small cell lung cancer
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PD-1:
-
Programmed cell death protein-1
- PD-L1:
-
Programmed death-ligand 1
- PFS:
-
Progression-free survival
- PR:
-
Partial response
- RECIST v1.1:
-
Response Evaluation Criteria in Solid Tumors version 1.1
- SAE:
-
Serious adverse event
- SD:
-
Stable disease
- TPS:
-
Tumor proportion score
- TTR:
-
Time to response
References
American Cancer Society. Cancer Facts & Figures 2019. Atlanta: American Cancer Society; 2019.
Besse B, Adjei A, Baas P, Melgaard P, Nicolson M, Paz-Ars L, et al. 2nd ESMO Consensus Conference on Lung Cancer: non-small-cell lung cancer first-line/second and further lines of treatment in advanced disease. Ann Oncol. 2014;25(8):1475–84.
Govindan R, Aggarwal C, Antonia SJ, Davies M, Dubinett SM, Ferris A, et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immunotherapy for the treatment of lung cancer and mesothelioma. J Immunother Cancer. 2022;10(5):e003956.
Planchard D, Popat S, Kerr K, Novello S, Smit EF, Faivre-Finn C, et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Update published 18 Sep 2019. https://www.esmo.org/content/download/227453/3874538/file/ESMO-CPG-mNSCLC-18SEPT2019.pdf. Accessed 18 Aug 2020.
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375(19):1823–33.
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al. Updated analysis of KEYNOTE-024: Pembrolizumab versus platinum-based chemotherapy for advanced non-small-cell lung cancer with PD-L1 tumor proportion score of 50% or greater. J Clin Oncol. 2019;37(7):537–46.
Vinay DS, Ryan EP, Pawelec G, Talib WH, Stagg J, Elkord E, et al. Immune evasion in cancer: mechanistic basis and therapeutic strategies. Semin Cancer Biol. 2015;35(Suppl):S185–98.
Mellor AL, Munn DH. IDO expression by dendritic cells: tolerance and tryptophan catabolism. Nat Rev Immunol. 2004;4(10):762–74.
Fallarino F, Grohmann U, You S, McGrath BC, Cavener DR, Vacca C, et al. The combined effects of tryptophan starvation and tryptophan catabolites down-regulate T cell receptor zeta-chain and induce a regulatory phenotype in naive T cells. J Immunol. 2006;176(11):6752–61.
Uyttenhove C, Pilotte L, Theate I, Stroobant V, Colau D, Parmentier N, et al. Evidence for a tumoral immune resistance mechanism based on tryptophan degradation by indoleamine 2,3-dioxygenase. Nat Med. 2003;9(10):1269–74.
Schalper KA, Carvajal-Hausdorf D, McLaughlin J, Altan M, Velcheti V, Gaule P, et al. Differential expression and significance of PD-L1, IDO-1, and B7–H4 in human lung cancer. Clin Cancer Res. 2017;23(2):370–8.
Takada K, Kohashi K, Shimokawa M, Haro A, Osoegawa A, Tagawa T, et al. Co-expression of IDO1 and PD-L1 in lung squamous cell carcinoma: potential targets of novel combination therapy. Lung Cancer. 2019;128:26–32.
Volaric A, Gentzler R, Hall R, Mehaffey JH, Stelow EB, Bullock TN, et al. Indoleamine-2,3-dioxygenase in non-small cell lung cancer: a targetable mechanism of immune resistance frequently coexpressed with PD-L1. Am J Surg Pathol. 2018;42(9):1216–23.
Botticelli A, Cerbelli B, Lionetto L, Zizzari I, Salati M, Pisano A, et al. Can IDO activity predict primary resistance to anti-PD-1 treatment in NSCLC? J Transl Med. 2018;16(1):219.
Holmgaard RB, Zamarin D, Munn DH, Wolchok JD, Allison JP. Indoleamine 2,3-dioxygenase is a critical resistance mechanism in antitumor T cell immunotherapy targeting CTLA-4. J Exp Med. 2013;210(7):1389–402.
Taylor MW, Feng GS. Relationship between interferon-gamma, indoleamine 2,3-dioxygenase, and tryptophan catabolism. FASEB J. 1991;5(11):2516–22.
Toulmonde M, Penel N, Adam J, Chevreau C, Blay J-Y, Le Cesne A, et al. Use of PD-1 targeting, macrophage infiltration, and IDO pathway activation in sarcomas: a phase 2 clinical trial. JAMA Oncol. 2018;4(1):93–7.
Liu X, Shin N, Koblish HK, Yang G, Wang Q, Wang K, et al. Selective inhibition of IDO1 effectively regulates mediators of antitumor immunity. Blood. 2010;115(17):3520–30.
Beatty GL, O’Dwyer PJ, Clark J, Shi JG, Bowman KJ, Scherle PA, et al. First-in-human phase I study of the oral inhibitor of indoleamine 2,3-dioxygenase-1 epacadostat (INCB024360) in patients with advanced solid malignancies. Clin Cancer Res. 2017;23(13):3269–76.
Mitchell TC, Hamid O, Smith DC, Bauer TM, Wasser JS, Olszanski AJ, et al. Epacadostat Plus Pembrolizumab in Patients With Advanced Solid Tumors: Phase I Results From a Multicenter, Open-Label Phase I/II Trial (ECHO-202/KEYNOTE-037). J Clin Oncol. 2018;36(32):3223–30.
ClinicalTrials.gov. Study to explore the safety, tolerability and efficacy of MK-3475 in combination with INCB024360 in participants with selected cancers. Identifier NCT02178722. https://clinicaltrials.gov/ct2/show/results/NCT02178722. Accessed 18 Aug 2020.
Long GV, Dummer R, Hamid O, Gajewski TF, Caglevic C, Dalle S, et al. Epacadostat plus pembrolizumab versus placebo plus pembrolizumab in patients with unresectable or metastatic melanoma (ECHO-301/KEYNOTE-252): a phase 3, randomised, double-blind study. Lancet Oncol. 2019;20(8):1083–97.
Miettinen O, Nurminen M. Comparative analysis of two rates. Stat Med. 1985;4(2):213–26.
Boyer M, Hui R, Urban D, Clingan P, Su W-C, Devaux C, et al. Epacadostat plus pembrolizumab with platinum-based chemotherapy versus placebo plus pembrolizumab with platinum-based chemotherapy as first-line treatment for metastatic non-small cell lung cancer: a randomized, double-blind, phase II study. BMC Cancer. This issue.
Castro F, Cardoso AP, Gonçalves RM, Serre K, Oliveira MJ. Interferon-gamma at the crossroads of tumor immune surveillance or evasion. Front Immunol. 2018;9:847.
Çiçin I, Plimack ER, Gurney H, Leibowitz-Amit R, Alekseev BY, Parnis FX, et al. Epacadostat plus pembrolizumab versus placebo plus pembrolizumab for advanced urothelial carcinoma: results from the ECHO-303/KEYNOTE-698 study. BMC Cancer. This issue.
Smith M, Newton R, Owens S, Gong X, Tian C, Malesk J, Leopold L. Retrospective pooled analysis of epacadostat clinical studies identifies doses required for maximal pharmacodynamic effect in anti-PD-1 combination studies. J Immunother Cancer. 2020; 8(Suppl 3): Abstract 28. https://doi.org/10.1136/jitc-2020-SITC2020.0028.
Yao Y, Liang H, Fang X, Zhang S, Xing Z, Shi L, Kuang C, Seliger B, Yang Q. What is the prospect of indoleamine 2,3-dioxygenase 1 inhibition in cancer? Extrapolation from the past. J Exp Clin Cancer Res. 2021;40(1):60.
Perez RP, Reis MJ, Lewis KD, Saleh MN, Daud A, Berlin J, et al. Epacadostat plus nivolumab in patients with advanced solid tumors: Preliminary phase I/II results of ECHO-204. J Clin Oncol. 2017;35(suppl 15):3003.
Jung KH, LoRusso P, Burris H, Gordon M, Bang YJ, Hellmann MD, et al. Phase I study of the indoleamine 2,3-dioxygenase 1 (IDO1) inhibitor navoximod (GDC-0919) administered with PD-L1 inhibitor (atezolizumab) in advanced solid tumors. Clin Cancer Res. 2019;25(11):3220–8.
Acknowledgements
The authors wish to thank the investigators, site coordinators, and the patients for participating in this study.
About this supplement
This article has been published as part of BMC Cancer Volume 23 Supplement 1, 2023: Epacadostat, an IDO1 inhibitor, in combination with pembrolizumab: results from clinical trials in patients with advanced solid tumors. The full contents of the supplement are available online at https://bmccancer.biomedcentral.com/articles/supplements/volume-23-supplement-1.
Funding
This study was funded by Incyte Corporation (Wilmington, DE, USA) in collaboration with Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. The funding body was involved in the design of the study, data analysis, and data interpretation. Medical writing and editorial assistance were provided by Christina Khodr, PhD, and Mary Kacillas of Ashfield Healthcare Communications, part of UDG Healthcare, plc, and was funded by Incyte Corporation.
Author information
Authors and Affiliations
Contributions
Conceived or designed the work: LL, MM, LP-A, AS, JS, MA. Collected, analyzed, or interpreted the data: LL, MM, JD, MH, MP, LP-A, AS, CB, J-SL, MA, JS, TT, OK, MLQ. Wrote or contributed to the writing of the manuscript: TT, OK, JS, MA, MLQ, J-SL, MH, MP, LP-A, LL, JD, MM, AS, LX, CB.
All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Independent ethics committees, as defined by the US CFR Title 21, Part 56 or equivalent country-specific regulations, reviewed and approved the protocol and any amendments. This study was conducted to conform with the Declaration of Helsinki, Good Clinical Practice guidelines, applicable country and/or local statutes, regulations regarding independent ethics committee review, and the protection of human patients in biomedical research. The study was approved by the ethics committees at each institution (Akdeniz University Clinical Trials Ethics Committee; Austin Health Human Research Ethics Committee; Chungbuk National Univ. Hospital IRB; Clinical Research Ethics Committee—University College Cork; Comitato Etico Regione Liguria c/o IRCCS Ospedale Policlinico San Martino—Istituto di Ricovero e Cura a Carattere Scientifico per l’Oncologia; Comite Autonomico de Etica de la Investigacion de Galicia Calle San Lazaro sn Secretaria Xeral. Conselleria de Sanidade; Copernicus Group Independent Review Board; De Videnskabsetiske Komiteer For Region Hovedstaden; EC of Central Clinical Hospital with polyclinic of the Presidential Administration of the RF; Gachon University Gil Medical Center IRB/IEC; Health Research Ethics Board of Alberta; Helsinki Committee Chaim Sheba Medical Center; Horizon Health Network Ethics Committee; H.U. Vall de Hebron Passeig de la Vall d.Hebron sn; Joint Group Health Centre/Sault Area Hospital REB; Kanagawa Cancer Center Institutional Review Board; Kanazawa University Hospital Institutional Review Board; Kantonale Ethikkommission Zuerich; Kindai University Hospital Institutional Review Board; Komisja Bioetyczna przy Bydgoskiej Izbie Lekarskiej; Kurume University Institutional Review Board; Kyiv City Clinical Oncological Center; Kyushu University Hospital Institutional Review Board; LEC of Leningrad Regional Clinical Hospital; London Central Research Ethics Committee; Medical and Diagnostic Centre LLC Dobryi Prognoz IRB/IEC; Medical Research Ethics Committee Kompleks Pendidikan Sains Kejururawatan Tingkat 2 Pusat Perubatan Univ Malaya; Medical Ethics & Research Committee No.1 Jalan Setia Murni U13 52 Seksyen Block A Kompleks Institut Kesihatan Negara; MI Kryviy Rih Center of Dnipropetrovsk Regional Council IRB/IEC; MI Odessa Regional Oncological Centre; National Cancer Center Institutional Review Board; National Hospital Organization Nagoya Medical Center IRB; National Hospital Organization Shikoku Cancer Center IRB; Niigata Cancer Center Hospital Institutional Review Board; Okayama University Hospital Institutional Review Board; Ontario Cancer Research Ethics Board; Rabin Medical Center IRB-Committee; Rambam—MC – ERC; Segreteria tecnico-scientifica del Comitato Etico Fondazione Policlinico Universitario; Sendai Kousei Hospital Institutional Review Board; Seoul National University Bundang Hospital, Institutional Review Board; Shizuoka Cancer Center Hospital and Research Institute IRB; Soroka M.C IRB; St. John of God Health Care Human Research Ethics Committee IRB/IEC; US Oncology, Inc. IRB; Wakayama Medical University Institutional Review Board; Western IRB; WIRB-Copernicus Group WCG; and Zaporizhzhya Regional Clinical Oncology Center). All patients provided written informed consent before initiating treatment.
Consent for publication
Not applicable.
Competing interests
TT has received honorarium from Merck Sharp & Dohme, Chugai, and AstraZeneca. OK and JS have nothing to disclose. MA reports honoraria from Roche, Pfizer, Amgen, and Merck & Co., Inc. MLQ reports travel expenses from Merck Sharp & Dohme, Roche, Pfizer, Ipsen, Astellas, Lilly, and AstraZeneca; advisory board participation for Roche, Boehringer Ingelheim, Bristol Myers Squibb, AstraZeneca, Takeda, Eusa Pharma, and Pfizer; and conference participation for Astellas, Vifor, Roche, AstraZeneca, Bristol-Myers Squibb, Janssen, Ipsen, and Pfizer. J-SL has nothing to disclose. MH reports a consulting or advisory role with IntegraConnect. MP reports advisory board participation for AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Merck & Co., Inc., Merck Sharp & Dohme, Pfizer, Roche, and Takeda. LP-A reports honoraria from Advanced Accelerator Applications, Amgen, AstraZeneca, Bayer, Blueprint Medicines, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Eli Lilly and Company, Incyte Corporation, Ipsen, Merck & Co., Inc., Merck Sharp & Dohme, Novartis, Pfizer, PharmaMar, S.A., Roche, Sanofi, Servier Laboratoires, Sysmex Corporation, and Takeda; research funding from AstraZeneca, Bristol-Myers Squibb, Merck Sharp & Dohme, and Pfizer; a leadership role at Altum Sequencing and is an officer/board of directors role at Genómica. LL, JD, and MM report employment and stock ownership with Incyte Corporation. AS and LX are salaried employees of Merck & Co., Inc., Rahway, NJ, USA and own stock in the company. CB reports no conflicts to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1.Supplementary Table 1.
Treatment duration and follow-up.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tokito, T., Kolesnik, O., Sørensen, J. et al. Epacadostat plus pembrolizumab versus placebo plus pembrolizumab as first-line treatment for metastatic non-small cell lung cancer with high levels of programmed death-ligand 1: a randomized, double-blind phase 2 study. BMC Cancer 23 (Suppl 1), 1251 (2024). https://doi.org/10.1186/s12885-023-11203-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11203-8