Abstract
Background
Precise prognostication is the key to optimum and effective treatment planning for early-stage hormone receptor (HR) positive, HER2/neu negative breast cancer patients. Differences in the breast cancer incidence and tumor anatomical features at diagnosis, pharmacogenomics data between Western and Indian women along with the vast diversity in the economic status and differences in insurance policies of these regions; suggest recommendations put forward for Western women might not be applicable to Indian/Asian women. Opinions from oncologists through a voting survey on various prognostic factors/tools to be considered for planning adjuvant therapy are consolidated in this report for the benefit of oncologists of the sub-continent, SAARC and Asia’s LMIC (low and middle-income countries).
Methods
A three-phase DELPHI survey was conducted to collect opinions on prognostic factors considered for planning adjuvant therapy in early-stage HR+/HER2/neu negative breast cancer patients. A panel of 25 oncologists with expertise in breast cancer participated in the survey conducted in 2021. The experts provided opinions as ‘agree’ or disagree’ or ‘not sure’ in phases-1 and 2 which were conducted virtually; in the final phase-3, all the panel experts met in person and concluded the survey.
Results
Opinions on 41 statements related to prognostic factors/tools and their implications in planning adjuvant endocrine/chemotherapy were collected. All the statements were supported by the latest data from the clinical trials (prospective/retrospective). The statements with opinions of consensus less than 66% were disseminated in phase-2, and later in phase-3 with supporting literature. In phase-3, all the opinions from panelists were consolidated and guidelines were framed.
Conclusions
This consensus guideline will assist oncologists of India, SAARC and LMIC countries in informed clinical decision-making on adjuvant treatment in early HR+/HER2/neu negative breast cancer patients.
Similar content being viewed by others
Introduction
Breast cancer continues to be public health focus in many parts of the world, including the SAARC region and India [1, 2]. Age-adjusted incidence in India is 25.8 per 100,000 women and mortality is 12.7 per 100,000 women, this is increasing since 1982 in all our population-based cancer registries (PBCRs; up to 2.84%); by 2020, it was projected to have as many as 17,97,900 cases [3]. The median age at diagnosis is 44.6 years with a peak between 40 and 50 years [4]. Real-world Indian data showed that hormone receptor (HR) positive and HER2 negative constitute 50–60% of all breast cancer (BC) patients [5].
To improve their outcome, especially with respect to cure, it is crucial to identify high-risk individuals requiring a more aggressive approach as well as separate out low-risk patients to prevent them from getting unnecessary and non-beneficial treatment [6,7,8,9]. Because of significant differences in the natural history, disease biology, as well as pharmacogenomics; treatment of Asian patients based on Western guidelines and/or recommendations that lack validation data on Asian patients and more specifically on Indian patients need caution. Such an approach would either result in overtreatment (and associated toxicity–medical, financial, and societal issues) or in undertreatment (reducing cure rates) [8, 9].
In the current manuscript, we conducted a survey by the DELPHI method to collect opinions on various prognostic factors/tools used to estimate the cancer recurrence risk and thereby plan therapy in HR+, HER2/neu negative BC patients; that could be used pragmatically by oncologists of India, SAARC and LMIC countries in day-to-day clinical practice.
Materials and methods
The DELPHI survey model was conducted in three phases over 12 months. During the first phase, a Steering Committee including 4 experts in breast cancer (BC) was asked to define relevant statements on various topics related to prognostication and therapy in the Indian scenario. After an advisory board meeting, of the 68 statements, the Steering Committee identified 41 preliminary relevant recommendation statements on prognostic factors/tests and adjuvant endocrine treatment in ER-positive early breast cancer (EBC), based on available published data. In the second phase, an expert committee was put together. It consisted of 25 oncologists (medical oncologists-21, surgical-2, radiation-2) specifically dealing with the day-to-day management of breast cancer. They represented several academic organizations, government and private hospitals and societies across India and have an experience in managing large volumes of breast cancer patients. In the second phase, we conducted a voting survey consisting of 3 rounds. In the first round, a web-based survey was carried out under the aegis of the Integrated Academic Society of Clinical Oncology (IASCO). The panelists were asked to express anonymously their level of agreement with each statement, using a three-point Likert scale (where 1 = completely agree; 2 = not sure; 3 = completely disagree) [10]. The panelists were guided by published evidence as well as intricate analysis of practical experience fromthe real-world patient management by national and international experts on all the statements [11]. Our panel experts were provided with previous SAARC publications, including the results of an online poll of oncologists (involving medical oncologists, radiation oncologists, surgical oncologists, molecular oncologists, and policymakers) [12,13,14]. A consensus was deemed as achieved if “answer 1” exceeded 66%, as described in previous studies conducted with this method [15,16,17]. In cases where consensus was not achieved, voting process was repeated after the experts were provided additional publications/data. This virtual voting survey was conducted twice, and the last round of voting involved an in-person meeting, held in Bengaluru on 12th Dec 2021. In the final third round, in the in-person meeting, panel experts finalized these consensus guidelines statements for the benefit of community oncologists, so that they would have ready-to-use practical recommendations for India and the SAARC regions. We believe that these guidelines are also applicable to other LMIC [8, 11, 12].
Results
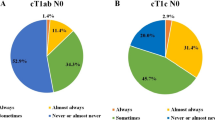
Of the 41 statements, 30 statements achieved the threshold for positive consensus in the first round. The remaining 11 statements were circulated in the second round with supportive literature from various clinical trials. An additional statement on the treatment of luminal sub-types was formed in the final and in-person rounds. In the end, 35 statements obtained positive agreement. These statements are clustered under various categories of prognostic and predictive factors, online prognostic tools, multigene tests for prognostication and the use of hormonal therapy (Table 1). The recommendation statements that obtained consensus in rounds 1 and 2, along with other recommendations on surgery and radiotherapy are represented in Table 2.
Diagnostic workup
Although the survey did not include any questions on diagnostic workup, the panelists discussed assessments to be made based on various parameters for each patient during the disease diagnosis. Similarly, opinions on surgery and radiotherapy were consolidated. The steps to be followed for each patient vary on case-to-case basis and the recommendations framed in this survey are in line with guidelines provided by international committees [18]. The diagnostic workup should follow the recommendations mentioned in Table 3. Primary tumor and regional lymph node assessments are key to optimizing therapy in this potentially curative group of EBC. Not all the features are necessary for each patient. Systemic staging of asymptomatic patients is not warranted as routine practice [19]. Further tests are required only when clinically indicated. The bone scan is to be performed in patients with pain in the bone and with elevated alkaline phosphatase if clinically the disease is of stage II [20,21,22]. Bone mineral density test is recommended in post-menopausal women who would be treated with aromatase inhibitors for more than 5 years, to avoid the risk of fractures in these women. Abdominal with or without pelvic CT or MRI to be done in cases of abnormal LFT, abnormal physical examination of abdomen/pelvis. Hereditary cancer assessment requires appropriate utilization. The panel experts recommended genetic counselling in women diagnosed with high-risk disease.
Prognostic factors deciding the risk of recurrence and use of chemotherapy in HR + ve, HER/neu-ve EBC
The expert committee identified the following factors that are important to assess the risk of recurrence in patients with HR + ve, HER2/neu–ve EBC (Table 1). All the committee members considered nodal status as the most important prognostic factor that also predicts chemotherapy benefit. A total of 96% also considered tumor size to be correlating with the risk of recurrence. For the remaining five features (age, histopathological grade, ER expression, Ki67 levels and gene expression profiling) 88% of experts considered them crucial for predicting the risk of recurrence. The experts opined that tumor size, tumor grade, age of the patient at the time of diagnosis, levels of ER, Ki-67 were more or less of similar importance and correlated with chemotherapy benefit (at least 72% of panelists agreed). Higher clinical risk like big tumors, higher nodal involvement, and moderate and high-grade disease was associated with worst survival and higher recurrence rates [23, 24]. Data from clinical trials have shown that women under 50 years derive a survival benefit of 7–11% with chemotherapy while the benefit of 2–3% in patients aged between 50 and 69 [25]. Besides these factors, the role of proliferation markers, ER and Ki-67 in making systemic adjuvant therapy decisions was discussed. More than 80% of panelists voted for the prognostic role of ER and Ki-67. The threshold for ER positivity has undergone revision from 10 to 1%, with data suggesting a limited endocrine therapy benefit in patients with ER lower than 10% [26]. Nonetheless, panelist agreed to 1% of ER as being positive honouring ASCO and CAP recommendations [27]. However, PR status failed to achieve a positive consensus threshold in both rounds 1 and 2 and hence was excluded from the table. In view of the subjective nature of Ki-67 staining and grading, 80% of panelists expressed their opinion that expression levels of Ki-67 of 14% and above are considered high-risk. The latest recommendations from the International Ki-67 in Breast Cancer working group opined that Ki-67 above 30% could be considered high-risk and for patients with Ki-67 between > 5-<30% advice from a prognostic test should be considered for deciding on chemotherapy use [28]. The panelists discussed the importance of gene expression profiles for decision-making on the use of chemotherapy at length. 88% of the panelists voted for the use of prognostic tests that assess the risk of recurrence based on the expression of genes that provide significant information on cancer progression which clinical parameters and proliferation indices might miss out [29]. Hence the consensus guidelines statement is that all seven features are important for assessing the aggressiveness of the disease thereby predicting the risk of recurrence and to be considered for making decisions on whether to use chemotherapy or not (Table 2).
Utility of online prognostic tools for taking decisions on chemotherapy use
The expert committee evaluated three online predictive tools – NPI, IHC4 and PREDICT. The opinion on their utility was variable (Table 1). NPI uses a simple equation that estimates overall survival based on clinical parameters while PREDICT along with clinical parameters uses information on age, menopausal status, ER and Ki-67 for making survival estimates post-surgery for various adjuvant treatment regimens [30, 31]. Contrary to these two tools, IHC4 is purely based on information derived from immunohistochemistry of ER, PR, Ki-67 and HER2 without considering the clinical parameters [32]. Even after extensive discussion and re-review of updated literature, there was no confidence in the value of such predictive tools. Although these online tools provide reliable prognostic information in some cohorts, they have been shown to overestimate or underestimate survival in patients of certain age groups. NPI is sub-optimal in predicting prognosis in patients < 40 years and underestimated overall survival in patients aged between 55 and 60 years [33]. In a study on a cohort of 600 patients, aged below 40 years PREDICT overestimated chemotherapy benefits and 10-year mortality by 8% [34, 35]. Moreover, NPI and IHC4 have ambiguous intermediate-risk zones, failing to provide a definite treatment option to these patients. The panelists highly opined cancer recurrence and progression are driven by key biological markers, which manifest in upstaging of tumor anatomical features by transforming clinical low risk into high risk. AJCC revised the staging definition from anatomic staging to a prognostic staging system with the incorporation of biomarkers in its 8th edition [36]. As a result, a recent study conducted on 4729 patients with T1-T2N1mi disease with 5-year follow-up found that approximately 84.4% of patients were downstaged and 3.7% of patients were upstaged and reported that 8th AJCC system predicted better breast cancer-specific survival compared to 7th AJCC staging system [37]. Hence the consensus guidelines statement is that these online predictive tools that primarily use clinical parameters to predict survival benefits, are not to be used in patient decision-making (Table 2).
Use of multi-marker prognostic test in clinical practice
The expert committee spent substantial time discussing the role of multi-marker prognostic tests. Five tests were considered for the discussion in this survey (Table 1). A total of 84% of experts were in favour of CanAssist Breast and 80% were also in the favour of Oncotype DX. The usage of the other three tests ranged between 20% and 28% of the experts. Oncotype DX and MammaPrint are the first-generation prognostic signatures. Oncotype DX is a 21 gene signature that has been developed in the NSABP-14 cohort and validated in NSABP-20, TransATAC and SWOG8814 cohorts. Other than these, Oncotype DX has been validated in large clinical trials in a prospective manner in patients with node-negative (TAILORx trial) and node-positive patients (RxPONDER). MammaPrint is a 70 gene signature validated in prospective trials, RASTER and MINDACT. Prosigna is a 50-gene signature initially developed to distinguish luminal subtypes. This test is validated only in post-menopausal women with different risk zones for node-negative (3 zones) and node-positive patients (2 zones). EndoPredict is a 12-gene signature that later along with clinical parameters (node and tumor size) was called EPClin. This test has been validated retrospectively on ABCSG6 and 8 cohorts [29]. While all the above mentioned tools use logistic regression, CanAssist Breast is an IHC based tool that uses an Artificial Intelligence-based Machine (SVM) algorithm for the prediction of recurrence risk with inputs from immunohistochemistry information of 5 critical biomarkers of cancer progression and recurrence pathways along with 3 clinical parameters [38]. CanAssist Breast has been validated in multiple cohorts from Southeast Asia, the USA and Europe [39,40,41] and in a DUTCH sub-cohort of TEAM trial- a prospective randomized trial [42]. The consensus guidelines state that CanAssist Breast and Oncotype DX are the recommended multi-marker prognostic tests that are the preferred choice (Table 2).
Other more recent prognostic tools which are not considered in this survey are DigiStain and a test developed in Korea named GenesWell BCT [43, 44]. Both these tests are relatively new in SAARC countries; DigiStain is available for patients in select regions and the Korean test is undergoing additional validation studies to be available for patients, we can perhaps include them in the survey in the next updating of the guidelines.
Scenarios where multi-marker prognostic tests are used in clinical practice
The appropriate clinical utility of multi-marker prognostic tests was also discussed. A total of 92% of the experts agreed that their use is based on patient affordability and on inclusion in international treatment guidelines (Table 1). An identical number (92%) also agreed that Western tests have not been validated in Indian patients; also 88% said that the TAILORx trial that assessed Oncotype DX performance in node-negative patients included a few Indian/Asian patients and hence is not applicable to this ethnic/geographical group [45]. While 88% used multi-marker prognostic tests routinely and 84% said they recommended use when facing a clinical dilemma in treatment decision- making. The consensus guidelines statement is that multi-marker prognostic tests should be used routinely based on patient affordability and especially when facing a clinical dilemma. Even if Western tests are included in international guidelines they should not be used blindly since they have not been validated in Asian and Indian patients (Table 2).
Differences in breast cancer between Asian (including indian) versus western women
Aligning with the data published from multiple cohorts, 76% of the panelists agreed that differences exist in breast cancer between Asian and Western women and therefore would require different treatment approaches [46]. Asian women are diagnosed more at a premenopausal age, with larger luminal B tumors, with node-positive disease, and have active tumor micro-environments with frequent TP53 mutations vs. Caucasian women warranting aggressive treatment strategies [47,48,49,50]. The consensus was that Asian (including Indian) younger women have the more aggressive disease (84%); high expression of proliferative genes (80%); and higher involvement of genes involving endocrine resistance (80%) (Table 1). In a study involving a large SEER database of 86,030 patients who underwent Oncotype DX testing, it was found that a large number of Black women were likely to have RS greater than 25 (high-risk requiring chemotherapy) compared to White women with lower accuracy of Oncotype DX in identifying low-risk patients (RS 0–25) [51]. This data along with post-hoc analysis of TAILORx showed differential performance of Oncotype DX in Black vs. White women, a total of 88% agreed that Black women had higher mortality compared to White women of the same type, grade and stage of breast cancer within the same RS score. The consensus guidelines statement is that Asian/Indian patients have a biologically different disease which is more aggressive in younger patients and can have higher expression of poor prognostic genes compared to Western women (Table 2).
Applicability of an indian made prognostic test, CanAssist breast in making decisions on chemotherapy use
Regarding CanAssist Breast as a prognostic and predictive test, 84% confirmed that it predicted risk of recurrence based on tumor biology; 80% said it is affordable in LMIC; and 76% stated that it predicts risk of recurrence across diverse ethnic backgrounds and geographies (Table 1). CanAssist Breast is the only test that has been extensively validated on Southeast breast cancer patients [36,37,38]. Along with this data, CanAssist Breast has validation data on Caucasian patients, who are different from its development cohort (Indian). This data clearly demonstrated its unparalleled performance in the cohorts from Europe and USA [41]. Despite the differences in the disease (breast cancer) between Asian and Caucasian women, CanAssist Breast’s prognostication was similar across these diverse cohorts unlike Oncotype DX, MammaPrint. Post-hoc analysis of the TAILORx trial showed altered performance of Oncotype DX with a higher hazard ratio in Black women vs. White women and non-Hispanic women vs. Hispanic women for the same RS category [45]. Likewise, MammaPrint showed lower low-risk proportions in Asian patients compared to European breast cancer patients [52]. Along with this outstanding performance across the various cohorts, CanAssist Breast showed greater than 83% concordance in the low-risk category with Oncotype DX and MammaPrint, the greatest agreement shown between two prognostic tests ever [41, 53]. Optima prelim trial that assessed the agreement between Oncotype DX, MammaPrint, Prosigna, IHC4 and IHC4 Aqua reported a disagreement between these tests in 60.6% of tumors [54]. The accuracy of the test and its cost are the major determining factors in the choice of a prognostic test. With the five times higher price of Oncotype DX and MammaPrint [55, 56] than that of CanAssist Breast [40], the use of these Western multi-gene tests for many patients from India, SAARC countries would be a far-fetched option. The consensus guidelines statement is that CanAssist Breast is a prognostic test that predicts the risk of recurrence; is applicable across ethnic backgrounds and geographies and is affordable in LMIC (Table 2).
Extended hormonal therapy in high-risk HR + ve, HER2/neu-ve EBC
The use of hormonal therapy for more than 5 years in postmenopausal women reduced the risk of recurrence as well as the risk of contralateral breast cancer was the opinion of 92% of panelists (Table 1). These opinions were based on the results of a placebo-controlled clinical trial and ATLAS trial [57, 58]. In line with the results from aTTOM trial [59] where BCI (Breast Cancer Index) high-risk patients derived significant benefit from extended hormonal therapy, 80% of panelists voted for the opinion that recurrence after 5 years of adjuvant endocrine therapy is seen in patients who have been identified as having high risk based on multi-marker prognostic testing. Another factor worth considering for treating post-menopausal women with extended hormonal therapy is bone health. The results of bone mineral density test will be a guiding factor for prescribing hormonal therapy beyond 5 years. All members of the expert committee agreed that hormonal therapy should be used for male patients (Table 1) and 96% stated the preferred choice of treatment is tamoxifen. The consensus guidelines statement is that hormonal therapy with tamoxifen should be used in male patients; use of hormonal therapy for more than 5 years reduces the risk of recurrence as well as contralateral breast cancer; recurrence after 5 years of endocrine therapy occurs in patients who have been identified as having high risk by multi-marker prognostic testing (Table 2).
Use of prognostic tests for luminal sub-type
Although there were no questions asked in the survey regarding luminal sub-types, in the final in-person round the panelists discussed the adjuvant systemic treatment strategies for luminal-like patients (Table 4). The panelists concluded that luminal-A like patients have a good prognosis with endocrine therapy alone. Few patients are identified as ‘high-risk’ by the multi-marker prognostic tests and patients with high tumor burden with large tumors or high nodal involvement or poorly differentiated tumors derive benefit from chemotherapy. Patients whose tumors are Luminal-A like are generally suitable for endocrine therapy alone. In case they have high-risk features (on biomarker testing or high tumor burden), chemotherapy should be added. St Gallen’s expert panel also recommends chemotherapy for luminal-A patients with large tumor volume [60]. For patients who have Luminal-B like tumors and are HER2/neu negative, both chemotherapy and endocrine therapy are to be used. If biomarker testing indicates a low risk for cancer recurrence, chemotherapy can be avoided in such patients. Oncotype DX and CanAssist Breast are known to identify high-risk patients from luminal-A like patients and low-risk patients from luminal-B like patients [40, 61].
Conclusions
Based on the opinions collected in this survey, the expert committee developed a flow chart (Fig. 1) that the community oncologist can refer to for quick implementation of these consensus guidelines and recommendations; for robust decision making while dealing with patients with HR+/HER2- EBC; and as a handy tool for patient counseling as well as teaching purposes, especially for fellows and postgraduates in oncology.
Data Availability
The data generated in the current work will be available from the corresponding author on reasonable request.
References
Youlden DR, Cramb SM, Yip CH, Baade PD. Incidence and mortality of female breast cancer in the Asia-Pacific region. Cancer Biol Med. 2014;11:101–15.
Madhav MR, Nayagam SG, Biyani K, Pandey V, Kamal DG, Sabarimurugan S, et al. Epidemiologic analysis of breast cancer incidence, prevalence, and mortality in India: protocol for a systematic review and meta-analyses. Med (Baltim). 2018;97:e13680.
Malvia S, Bagadi SA, Dubey US, Saxena S. Epidemiology of breast cancer in indian women. Asia-Pac J Clin Oncol. 2017;13:289–95.
Chopra B, Kaur V, Singh K. Age shift: breast cancer is occurring in younger age groups: is it true? Clin. Cancer Investig J. 2014;3:526–9.
Sandhu GS, Erqou S, Patterson H, Mathew A. Prevalence of triple-negative breast cancer in India: systematic review and meta-analysis. J Glob oncol. 2016;2:412–21.
Doval DC, Radhakrishna S, Tripathi R, et al. A multi-institutional real world data study from India of 3453 non-metastatic breast cancer patients undergoing upfront surgery. Sci Rep. 2020;10:5886.
Shet T. Improving the accuracy of breast cancer biomarker testing in India. Indian J Med Res. 2017;146:449–58.
Aggarwal S, Vaid A, Ramesh A, Parikh PM, Purohit S, Avasthi B, et al. Practical consensus recommendations on the management of HR + ve early breast cancer with specific reference to genomic profiling. South Asian J Cancer. 2018;7:96–101.
Monticciolo DL, Helvie MA, Hendrick RE. Current issues in the overdiagnosis and overtreatment of breast Cancer. AJR Am J Roentgenol. 2018;210:285–91.
Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67:401–9.
Purvish MP, Hingmire Patil, Bhavesh KG, Prashant Mehta A, Verma SA, Bondarde, et al. Oncology Gold Standard™ consensus statement on counseling patients for molecular testing and personalized cancer care. Int J Mol ImmunoOncol. 2017;2:47–57.
Purvish M, Parikh P, Narayanan A, Vora A, Gulia SK, Mullapally B, Rangrajan, et al. Conflict of interest disclosure and interpretation - rest assured the medical professional in the audience is perceptive, alert and smart. Indian J Med Sci. 2019;71:4–8.
Purvish MP, Hingmire SS, Patil Bhavesh K, Govind P, Mehta A, Verma, et al. Oncology Gold Standard™ consensus statement on counseling patients for molecular testing and personalized cancer care. Int J Mol ImmunoOncol. 2017;2:47–57.
Purvish MP, Vora PNarayana, Gulia AG, Mullapally SK, Rangrajan B, et al. Conflict of interest disclosure and interpretation - rest assured the medical professional in the audience is perceptive, alert and smart. Indian J Med Sci. 2019;71:4–8.
Pelizzari G, Arpino G, Biganzoli L, et al. An italian Delphi study to evaluate consensus on adjuvant endocrine therapy in premenopausal patients with breast cancer: the ERA project. BMC Cancer. 2018;18:932.
Puglisi F, Bisagni G, Ciccarese M, Fontanella C, Gamucci T, Leo L, et al. A Delphi consensus and open debate on the role of first-line bevacizumab for HER2-negative metastatic breast cancer. Future Oncol. 2016;12:2589–602.
Mohile SG, Velarde C, Hurria A, Magnuson A, Lowenstein L, Pandya C, et al. Geriatric assessment-guided care processes for older adults: a Delphi consensus of geriatric oncology experts. J Natl Compr Cancer Netw. 2015;13:1120–30.
NCCN Breast. Cancer Treatment guidelines 2022.
Soares GP, Pereira AAL, Vilas Boas MS, Vaisberg VV, Magalhães MCF, Linck RDM, Mano MS. Value of systemic staging in asymptomatic early breast Cancer. Rev Bras Ginecol Obstet. 2018;40:403–9.
Sarvari BK, Sankara Mahadev D, Rupa S, Mastan SA. Detection of bone metastases in breast Cancer (BC) patients by serum tartrate-resistant acid phosphatase 5b (TRACP 5b), a bone resorption marker and serum alkaline phosphatase (ALP), a bone formation marker, in Lieu of whole body skeletal scintigraphy with Technetium99m MDP. Indian J Clin Biochem. 2015;30:66–71.
White DR, Maloney JJ, Muss HB, et al. Serum alkaline phosphatase determination: value in the staging of advanced breast Cancer. JAMA. 1979;242:1147–9.
Chen WZ, Shen JF, Zhou Y, et al. Clinical characteristics and risk factors for developing bone metastases in patients with breast cancer. Sci Rep. 2017;7:11325.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomized trials. Lancet. 2005;365:1687–717.
Pan H, Gray R, Jeremy Bray Brooke BM, et al. 20 years risks of breast-Cancer recurrence after stopping endocrine therapy at 5 years. N Eng J Med. 2017;377:1836–46.
Early breast cancer. Trialists’ collaborative group polychemotherapy for early breast cancer: an overview of the randomised trials. Lancet. 1998;352:930e42.
Bouchard-Fortier A, Provencher L, Blanchette C, Diorio C. Prognostic and predictive value of low estrogen receptor expression in breast cancer. Curr Oncol. 2017;24:e106–14.
Kimberly HAM, Elizabeth HH, Dowsett M, Shannon EM, Lisa AC, Patrick LF, et al. Estrogen and progesterone receptor testing in breast Cancer: ASCO/CAP Guideline Update. J Clin Oncol. 2020;38:1346–66.
Nielsen TO, Leung SCY, Rimm DL, et al. Assessment of Ki67 in breast cancer: updated recommendations from the international Ki67 in breast Cancer Working Group. J Natl Cancer Inst. 2020;113:808–19.
Vieira A, Filipe S. Fernando. An Update on Breast Cancer Multigene Prognostic Tests—Emergent Clinical Biomarkers. Front. Med. 5, 2018, 1–2.
Haybittle JL, Blamey RW, Elston CW, et al. A prognostic index in primary breast cancer. Br J Cancer. 1982;45:361.
Wishart GC, Azzato EM, Greenberg DC, Rashbass J, Kearins O, Lawrence G, et al. PREDICT: a new UK prognostic model that predicts survival following surgery for invasive breast cancer. Breast Cancer Res. 2010;12(1):R1.
Cuzick J, Dowset M, Pinada S, et al. Prognostic value of a combined estrogen receptor, progesterone receptor, Ki-67, and human epidermal growth factor receptor 2 immunohistochemical score and comparison with the genomic health recurrence score in early breast cancer. J Clin Oncol. 2011;29:4274–8.
Lambertini M, Pinto AC, Ameye L, et al. The prognostic performance of adjuvant! Online and Nottingham Prognostic Index in young breast cancer patients. Br J Cancer. 2016;115:1471–8.
Wong HS, Subramaniam S, Alias Z, et al. The predictive accuracy of PREDICT: a personalized decision-making tool for southeast asian women with breast cancer. Med (Baltim). 2015;94:e593.
Maishman T, Copson E, Stanton L, Gerty S, Dicks E, Durcan L, et al. An evaluation of the prognostic model PREDICT using the POSH cohort of women aged ≤ 40 years at breast cancer diagnosis. Br J Cancer. 2015;112:983e91.
Giuliano AE, Connolly JL, Edge SB, Mittendorf EA, Rugo HS, Solin LJ, et al. Breast Cancer-major changes in the american Joint Committee on Cancer eighth edition cancer staging manual. Ca-Cancer J Clin. 2017;67:290–303.
Shi Jian L, Chen-Lu C, Feng Z, Ping L, Jian H, Li, et al. Prognostic and predictive value of the american Joint Committee on Cancer pathological prognostic staging system in nodal micrometastatic breast Cancer. Front Oncol. 2020;10:570175.
RamKumar C, Buturovic L, Malpani S, et al. Development of a Novel Proteomic Risk-Classifier for Prognostication of patients with early-stage hormone receptor-positive breast Cancer. Biomark. Insights. 2018;13:1–9.
Bakre MM, Ramkumar C, Attuluri AK, Basavaraj C, Prakash C, Buturovic L, et al. Clinical validation of an immunohistochemistry-based CanAssist-Breast test for distant recurrence prediction in hormone receptor positive breast cancer patients. Cancer Med. 2019;8:1755–64.
Doval DC, Mehta A, Somashekhar SP, et al. The usefulness of CanAssist breast in the assessment of recurrence risk in patients of ethnic indian origin. The Breast. 2021;59:1–7.
Gunda A, Basavaraj C, Chandra Prakash SV, Adinarayan M, Kolli R, Eshwaraiah MS, Saura C, et al. A retrospective validation of CanAssist breast in european early-stage breast cancer patient cohort. The Breast. 2022;63:1–8.
Zhang X, Gunda A, Kranenbarg EM, Liefers GJ, Savitha BA, Shrivastava P, et al. Ten-year distant-recurrence risk prediction in breast cancer by CanAssist breast (CAB) in dutch sub-cohort of the randomized TEAM trial. Breast Cancer Res. 2023;25:40.
https://digistain.co.uk/how-digistain-works/.
Gong G, Kwon MJ, Han J, Lee HJ, Lee SK, Lee JE, et al. A new molecular prognostic score for predicting the risk of distant metastasis in patients with HR+/HER2- early breast cancer. Sci Rep. 2017;7:45554.
Albain KS, Gray RJ, Makower DF, Faghih A, Hayes DF, Geyer CE, et al. Ethnicity, and clinical outcomes in hormone Receptor-Positive, HER2-Negative, node-negative breast Cancer in the Randomized TAILORx Trial. J Natl Cancer Inst. 2021;113:390–9.
Leong SP, Shen ZZ, Liu TJ, et al. Is breast cancer the same disease in asian and western countries? World J Surg. 2010;34:2308–24.
Lao C, Lawrenson R, Edwards M, Campbell I. Treatment and survival of asian women diagnosed with breast cancer in New Zealand. Breast Cancer Res Treat. 2019;177:497–505.
Farooq S, Coleman MP. Breast cancer survival in south asian women in England and Wales. J Epidemiol Community Health. 2005;59:402–6.
Iqbal J, Ginsburg O, Rochon PA, et al. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA. 2015;313:165–73.
Chen M, Kwong A, Hendricks C et al. Molecular profiles and clinical-pathological features of Asian early-stage breast cancer patients. Presented at 2020 San Antonio Breast Cancer Virtual Symposium December 8–11, 2020; San Antonio, Texas.
Hoskins KF, Danciu OC, Ko NY, Calip GS. Association of Race/Ethnicity and the 21-Gene recurrence score with breast Cancer-specific mortality among US women. JAMA Oncol. 2021;7:370–8.
Ishitobi M, Goranova TE, Komoike Y, Motomura K, Koyama H, Glas AM, et al. Clinical utility of the 70-gene MammaPrint profile in a japanese population. Jpn J Clin Oncol. 2010;40:508–12.
Sengupta AK, Gunda A, Malpani S, Serkad CPV, Basavaraj C, Bapat A, et al. Comparison of breast cancer prognostic tests CanAssist breast and oncotype DX. Cancer Med. 2020;9:7810–8.
Bartlett JM, Bayani J, Marshall A, Dunn JA, Campbell A, Cunningham C, et al. OPTIMA TMG. Comparing breast Cancer multiparameter tests in the OPTIMA Prelim Trial: no test is more equal than the others. J Natl Cancer Inst. 2016;108:djw050.
Özmen V, Çakar B, Gökmen E, Özdoğan M, Güler N, Uras C, et al. Cost effectiveness of Gene expression profiling in patients with early-stage breast Cancer in a Middle-Income Country, Turkey: results of a prospective Multicenter Study. Eur J Breast Health. 2019;15:183–90.
Crnobrnja B, Knez J, Pakiž M. EP200 MammaPrint testing can reduce the costs of treatment in breast cancer patients. 2019; https://ijgc.bmj.com/content/29/Suppl_4/A177.3.
Goss PE, Ingle JN, Pritchard KI, Robert NJ, Muss H, Gralow J, et al. Extending aromatase-inhibitor adjuvant therapy to 10 years. NEJM. 2016;375:209–19.
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, et al. Adjuvant tamoxifen: longer against shorter (ATLAS) Collaborative Group. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805–16.
Bartlett JMS, Sgroi DC, Treuner K, Zhang Y, Ahmed I, Piper T, Salunga R, Brachtel EF, Pirrie SJ, Schnabel CA, Rea DW. Breast Cancer Index and prediction of benefit from extended endocrine therapy in breast cancer patients treated in the adjuvant Tamoxifen-To offer more? (aTTom) trial. Ann Oncol. 2019;30:1776–83.
Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, et al. Panel members. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast Cancer 2013. Ann Oncol. 2013;24:2206–23.
Yoshio Mizuno H, Fuchikami N, Takeda J, Yamada Y, Inoue H, Seto. Kazuhiko Sato. Comparing oncotype DX Recurrence score categories with immunohistochemically defined Luminal subtypes. J of Cancer Ther. 2016;7:223–31.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
PP conducted the survey and coordinated with all the other authors who acted as subject matter expert panelists in the survey process. All authors contributed to the concept and study design. All authors also participated in the discussion and in finalizing of the survey questions. Manuscript was drafted by PP. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
As the study involves a survey on obtaining consensus on adjuvant therapies in HR+/HER2 negative early breast cancer, ethics approval and informed consent is deemed unnecessary as per national legislation, DCGI (Drug Controller General of India).
Consent for publication
Not applicable.
Competing interests
All other authors have no other competing interests to declare. All authors are practicing oncologists.
Experimental methods
The study does not involve any experimental protocols on human subjects. It uses a method that is well-adapted internationally for conducting a survey of this kind.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Parikh, P., Babu, G., Singh, R. et al. Consensus guidelines for the management of HR-positive HER2/neu negative early breast cancer in India, SAARC region and other LMIC by DELPHI survey method. BMC Cancer 23, 714 (2023). https://doi.org/10.1186/s12885-023-11121-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11121-9