Abstract
Background
Epstein Barr virus (EBV)-associated endemic Burkitt’s Lymphoma pediatric cancer is associated with morbidity and mortality among children resident in holoendemic Plasmodium falciparum regions in western Kenya. P. falciparum exerts strong selection pressure on sickle cell trait (SCT), alpha thalassemia (-α3.7/αα), glucose-6-phosphate dehydrogenase (G6PD), and merozoite surface protein 2 (MSP-2) variants (FC27, 3D7) that confer reduced malarial disease severity. The current study tested the hypothesis that SCT, (-α3.7/αα), G6PD mutation and (MSP-2) variants (FC27, 3D7) are associated with an early age of EBV acquisition.
Methods
Data on infant EBV infection status (< 6 and ≥ 6–12 months of age) was abstracted from a previous longitudinal study. Archived infant DNA (n = 81) and mothers DNA (n = 70) samples were used for genotyping hemoglobinopathies and MSP-2. The presence of MSP-2 genotypes in maternal DNA samples was used to indicate infant in-utero malarial exposure. Genetic variants were determined by TaqMan assays or standard PCR. Group differences were determined by Chi-square or Fisher’s analysis. Bivariate regression modeling was used to determine the relationship between the carriage of genetic variants and EBV acquisition.
Results
EBV acquisition for infants < 6 months was not associated with -α3.7/αα (OR = 1.824, P = 0.354), SCT (OR = 0.897, P = 0.881), or G6PD [Viangchan (871G > A)/Chinese (1024 C > T) (OR = 2.614, P = 0.212)] and [Union (1360 C > T)/Kaiping (1388G > A) (OR = 0.321, P = 0.295)]. There was no relationship between EBV acquisition and in-utero exposure to either FC27 (OR = 0.922, P = 0.914) or 3D7 (OR = 0.933, P = 0.921). In addition, EBV acquisition in infants ≥ 6–12 months also showed no association with -α3.7/αα (OR = 0.681, P = 0.442), SCT (OR = 0.513, P = 0.305), G6PD [(Viangchan (871G > A)/Chinese (1024 C > T) (OR = 0.640, P = 0.677)], [Mahidol (487G > A)/Coimbra (592 C > T) (OR = 0.948, P = 0.940)], [(Union (1360 C > T)/Kaiping (1388G > A) (OR = 1.221, P = 0.768)], African A (OR = 0.278, P = 0.257)], or in utero exposure to either FC27 (OR = 0.780, P = 0.662) or 3D7 (OR = 0.549, P = 0.241).
Conclusion
Although hemoglobinopathies (-α3.7/αα, SCT, and G6PD mutations) and in-utero exposure to MSP-2 were not associated with EBV acquisition in infants 0–12 months, novel G6PD variants were discovered in the population from western Kenya. To establish that the known and novel hemoglobinopathies, and in utero MSP-2 exposure do not confer susceptibility to EBV, future studies with larger sample sizes from multiple sites adopting genome-wide analysis are required.
Similar content being viewed by others
Background
Endemic Burkitt’s lymphoma (eBL) is a B-cell tumor and the most common cancer amongst children from malaria-endemic regions of Sub-Saharan Africa, Asia, and South America [1,2,3,4]. Endemic BL has a greater than 90% association with Epstein Barr virus (EBV) infection [2]. Even though the distribution of EBV is ubiquitous, with 95% of the world’s population having been infected at some point in life, there are geographical disparities in the distribution of EBV-associated eBL with high incidence rates in malaria holoendemic regions of Western and coastal Kenya [5,6,7]. In Kenya, 48% of children born in the malaria-endemic lake belt region of Kisumu have an abnormal α-thalassemia genotype [8, 9]. Additionally, sickle cell trait (SCT) and P. falciparum have a similar distribution within malaria-endemic areas of sub-Saharan Africa with an estimated prevalence above 16.2% within Western and coastal regions of Kenya [9,10,11]. Carriers of the heterozygous state (HbAS) benefit from reduced malaria severity and mortality [12,13,14]. Mutation of the glucose-6-phosphate dehydrogenase (G6PD) gene is also widely prevalent, with an estimated 8% frequency across malaria-endemic countries [15]. Approximately 400 million people living in tropical and sub-tropical areas exhibit G6PD deficiency, with a high diversity of variants in different parts of the world [16]. Additionally, there is a causal relationship between exposure to malaria, the early age of EBV infection, and the development of eBL in children from malaria-endemic regions [17]. Although these heritable traits (i.e., SCT, α-thalassemia, and G6PD deficiency) are associated with a protective advantage against malaria disease severity [18], their association with early ages of EBV acquisition in children from malaria-endemic regions such as Western Kenya, compared to other parts of the world has not been fully characterized.
There are additional factors that influence malaria disease severity, including allele-specific MSP-2 antibodies that are associated with reduced severity [19]. Previous investigations found an association between chronic exposures to P. falciparum infection and expansion of latently EBV-infected B-cells, leading to high viral loads that predispose children to eBL [20]. Furthermore, infants exposed to malaria during pregnancy and children resident in malaria-endemic regions have an earlier age of EBV infection and reactivation due to repeated malaria infections, thereby increasing the risk for the development of eBL [21, 22]. Children in malaria-endemic regions are typically infected by EBV within 6 months of age with early infection associated with poorly controlled and persistently elevated EBV viral loads over time [22]. Research has also shown that infants in non-malaria endemic regions of Kenya acquire EBV at the mean age of 8 months and have a lower risk of eBL development [22]. Collectively, being infected with EBV at an early age is linked to the risk of developing eBL [22,23,24]. To address current gaps in knowledge, we examined the relationship between hemoglobinopathies, merozoite surface protein-2 gene polymorphisms, and the acquisition of EBV among infants (0–12 months) in a holoendemic P. falciparum transmission region of western Kenya.
Materials and methods
Study site
The study was conducted in Chulaimbo Sub-County hospital in Western Kenya, a high-risk region for eBL [23, 25]. The hospital is located 18 km Northwest of Kisumu City at an altitude of 1300 m above sea level (-0.39 latitude and 34.6383 longitudes). P. falciparum malaria is holoendemic with two relative peaks during the long (March to May) and short rains (October to December) [26]. This region also has high morbidity and mortality rates due to infectious diseases such as malaria, HIV-1, and eBL [6, 27]. The SCT prevalence is 16.2%, and about 40% of children are heterozygous for α-thalassemia [9, 28]. Perennial P. falciparum is responsible for ~ 97% of malarial infections, resulting in high childhood mortality rates [27].
Study population
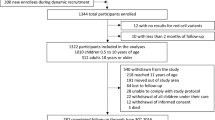
The details of the study population have been previously described [29]. In brief, mothers attending the antenatal clinic (ANC) at Chulaimbo Sub-County hospital between 2011 and 2015 were screened and then enrolled based on the following inclusion criteria: mother being a resident within a 10 km radius of the hospital, willingness to participate in the study, HIV negative status, uncomplicated vaginal delivery, singleton pregnancy, positive or negative peripheral malaria parasitemia, and < 30 weeks of gestation (See Supplementary File I). As described in [29], exclusion from the study was based on the mother’s HIV status and unwillingness to participate in the study where all mothers who were HIV positive and any that were not willing to participate in the study were excluded.
Sample size determination and data collection
The sample size of 81 was based on the findings of a previously described study [29] where significant differences in anti EBV antibodies were observed in neonates drawn from two groups of mothers; one with malaria exposure during pregnancy and another without any malaria exposure during pregnancy in a sample size of 70. Taking a sample size of 81 in our study would thus have given an 80% power to detect any expected differences at an alpha = 0.05. In brief, available archived infant DNA previously extracted from whole blood samples collected at any longitudinal time point between 6, 8, 14, 18 weeks, and 6, 9, and 12 months were used to test for α-thalassemia, SCT, and G6PD genotypes. Of the 81 samples genotyped, the following were excluded during analysis: two that failed to amplify for the SCT, one sample homozygous α-/α-/, and one sample that failed to amplify for the African G6PD variant. Achieved mothers’ DNA, extracted from venous blood at delivery, was genotyped for the presence of MSP-2 alleles (FC27 and 3D7). The MSP-2 genotyping was performed using 70 mother-child pair DNA samples. An infant was considered in utero exposed to MSP-2 if the MSP-2 variant was detected in maternal venous blood collected at delivery. An infant was considered non-exposed if the MSP-2 variants were not detected from the mothers’ sample.
Determination of infant EBV infection status
The mothers’ EBV viral loads were determined using real-time bi-plex Q-PCR as previously described [21, 22]. From the EBV viral loads generated, the following formula was used in the determination of infant EBV infection status: EBV copies per cell = EBV SQ/ (beta-actin SQ/2) where SQ is starting quantity and, 2 are the copies of beta-actin per cell. Excel spreadsheet was used for analysis and results were interpreted as EBV positive if the value from the calculation was ≥ 0.5. Results were considered negative if the value from the calculation was < 0.5. The data on infant EBV infection status was abstracted from the available records and stratified into those who were EBV-positive at any of the following time points 6, 8, 14, 18 weeks: henceforth characterized as EBV status < 6 months. The second category included EBV status ≥ 6 to 12 months, capturing EBV status at 6, 9, and 12 months.
Laboratory procedures
Sickle-cell polymerase chain reaction genotyping test
A previously established protocol was adapted for this study [30]. Briefly, a TaqMan SNP genotyping assay was used following the manufacturer’s protocols (Life Technologies, Grand Island, NY). Amplification was performed in a Real-time PCR StepOne Plus thermocycler from Applied Biosystems® (Foster City, CA, USA) with a triplicate of control samples for genotype Hb AA, Hb AS, and Hb SS with molecular grade water was used as a negative control.
Alpha-thalassemia genotyping
Genotyping for the different α-thalassemia mutations was performed with optimization to the described method [31]. In brief, PCR was performed using the GeneAmp PCR system 9700 (Applied Biosystems) in a 25 µL reaction volume containing 2.5x GoTaq Buffer-MgCl2, (Invitrogen), 4.0 mM MgCl2, 0.4 mM mixture of deoxynucleotide phosphates, α-thalassemia 3.7 primers (Integrated DNA Technologies, IDT) 0.3 µM Forward primer (“5 AAG TCC ACC CCT TCC TTC CTC ACC 3”), 0.25 µM Reverse1 primer (“ 5ATG AGA GAA ATG TTC TGG CAC CTG GAC TT 3’), 0.25 µM Reverse 2 primer (“5 TCC ATC CCC TCC TCC CGC CCC TGC CTT TT 3’), 5 Units/µL of GoTaq DNA polymerase (Promega M3005), 5% dimethyl sulfoxide (DMSO), 0.75 M betaine (Sigma), and 3 µL genomic DNA. The following cycling conditions of initial heat activation at 94 °C for 15 min, with 39 amplification cycles of denaturation at 94 °C for 45 s, annealing at 67 °C for 1 min, and elongation for 2 min at 72 °C and a final extension at 72 °C for 10 min were used. Molecular-grade water was used as a negative control. The housekeeping gene, glyceraldehyde-3-phosphate dehydrogenase (GAPDH), was amplified to confirm the presence of human DNA from randomly picked study samples. PCR products were run against a 1 kb DNA ladder (Promega Madison, WI USA) on 2% agarose gel at 80 volts for 2 h. The resulting gel image was visualized using a UV-transilluminator gel reader (UVITEC Cambridge), and generated images were captured, labeled, scored, and stored. The generated base pair (bp) sizes were identified by [2213–2217 bp for (α α /α α)] normal gene, [2213–2217 bp (α α /α α) and 1963 bp (α-/α-/)] as heterozygous and [1963 bp (α-/α-/)] for homozygous mutant gene deletions.
Multiplex PCR amplification for glucose-6-Phosphate dehydrogenase gene mutation
The Glucose-6-Phosphate dehydrogenase genotyping was adopted and modified from a previously used protocol [32]. Multiplex PCR was optimized such that each of the 6 mutation positions of the G6PD gene was amplified in fragments ranging from 164 to 384 bp (Table 1). The 15 µL PCR reaction concentrations consisted of 1µL of genomic DNA, 10X reaction buffer (Promega), 10 mM mixture of deoxynucleotide phosphates, 50 mM MgCl2, 10 µM of each primer set, and 2 Units/µL of Go Taq DNA polymerase (Promega M3005). The housekeeping gene, glyceraldehyde-3-phosphate dehydrogenase (GAPDH), was amplified from randomly selected samples to confirm the presence of human DNA. Molecular-grade water was used as a negative control. The Gene-Amp PCR system 9700 Thermal Cycler (Applied Biosystems) machine was used for (PCR) under the following cycling conditions and optimized for each primer set: an initial denaturation step at 95 °C for 3 min, 11 cycles of 94 °C for 15 s, 62 °C for 15 s, and 72 °C for 30 s. This was then followed by 24 cycles of 94 °C for 15 s, 56 °C for 15 s, and 72 °C for 30 s and a 3-minute final extension at 72 °C. After amplification, 20 µL of the PCR product was loaded on a 1.5% agarose gel and run against a 50 bp DNA ladder (Invitrogen) at 80 volts for 1 h 30 min. The gel was visualized using a UV-transilluminator gel reader (UVITEC Cambridge), and the resulting images were scored and stored.
G6PD african A- genotyping assay
According to the manufacturer’s instructions, the G6PD 376T > C and 202 C > T polymorphisms were genotyped using the TaqMan® 5’ allelic discrimination Assay-By-Design high-throughput method [Assay ID: C_2228694_20 for rs1050829 and C_2228686_20 for rs1050828; Thermo Fisher Scientific, Carlsbad, CA, USA). The PCR was performed in a total reaction volume of 10 µL with the following amplification cycles: initial denaturation at 60 °C for 30 s and 95 °C for 10 min followed by 40 cycles of 95 °C for 15 s and 60 °C for 60 s and, a final extension at 60 °C for 30 s using allele-specific fluorescence on the StepOne Plus™ Real-Time PCR Systems. The StepOne Plus™ Software (Version 2.3) was used for allelic discrimination (Thermo Fisher Scientific, Carlsbad, CA, USA).
MSP-2 genotyping assay
To genotype the different MSP-2 variants in these samples, the polymorphic regions of the merozoite surface protein 2 (MSP-2) were amplified by a nested PCR assay using oligonucleotide primer pairs specific for P. falciparum MSP-2 alleles. The primary PCR in a 15 µL reaction volume contained 1 µL of genomic DNA, 7.5 µL GoTaq master mix, 0.5 µL forward primer (M2-OF sequence 5”-ATGAAGGTAATTAAAACA TTGTCTATTATA-3”), 0.5 µL reverse primer (M2-OR primer sequence 5”-CTTTGTTACCATCGGTACATTCTT-3”) and 5.5 µL PCR water. The PCR reaction involved 30 amplification cycles composed of initial denaturation at 94 °C for 2 min, a further denaturing step at 94 °C for 30 s, followed by annealing at 60 °C for 1 min, and an extension step for 1 min at 72 °C. Nested PCR for the specific alleles was done in a 15 µL reaction volume containing 7.5 µL GoTaq green master mix 2x (Promega M791A protocol), 0.25 µM of each primer pair (M2 forward /M2-reverse) and 1 µL of primary PCR product. Molecular-grade water was used as a negative control. Nested allele-specific primers M5 reverse for 3D7 and N5 reverse for FC27 alleles (MSP-2 family-specific nested PCR primers M5 rev 5 “- GCA TTG CCA GAA CTT GAA-3” and N5 rev5 “-CTG AAG AGG TAC TGG TAG A-3”) were used. The PCR reaction involved 30 amplification cycles composed of initial denaturation at 94 °C for 2 min, a denaturing step at 94 °C for 30 s, followed by annealing at 60 °C for 60 s, and an extension step for 90 s at 72 °C. The PCR product was then run on 1.5% agarose gel and visualized using a UV-transilluminator gel reader (UVITEC Cambridge). Due to the presence of different MSP-2 clones, the genotypes were scored based on bp within the range of 250-450 bp for each genotype.
Data analysis
Analyses of sickle cell, G6PD, α-thalassemia genotypes, and EBV acquisition
Data were analyzed using IBM SPSS Statistics version 23. Before analysis, children in the study were stratified based on follow-up visits into < 6 months and ≥ 6–12 months. Chi-Square or Fisher’s test was used to compare proportions. A binary logistic regression model was used to determine the relationship between variants for SCT, G6PD, and α-thalassemia [normal α globin (αα/αα) 2213-2217bps fragments], [heterozygous carriers (-α3.7/αα) 1963bps and 2213-2217bps], and EBV acquisition. The association between MSP-2 variants and EBV acquisition was also determined using binary logistic regression modeling. There were no covariates included in the model. Statistical significance was defined as p ≤ 0.05.
Results
Demographic and clinical characteristics of study participants
The demographic and clinical characteristics of the study participants are presented in (Table 2). The level of education, maternal age, gestational age, and marital status was captured for the mothers upon enrollment. The median age for the mothers was 22.0 years. Most of the mothers enrolled had secondary education (n = 43, 53.1%), were in their second trimester of pregnancy (n = 53, 65.4%), and were married (n = 57, 70.4%). Data on the prevalence of specific protozoal and helminthic infections in the mothers was also determined. Pathogenic protozoal infections of Trichomonas vaginalis 2.5% [2], Entamoeba histolytica 17.3% [13], and Giardia lamblia 7.4% [6], were the most prevalent. Among all the infant samples, (n = 21, 26.6%) had at least one malaria episode by 12 months of age.
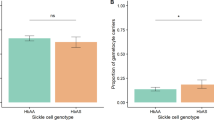
Distribution of alpha thalassemia, SCT, G6PD, and MSP-2 mutations based on EBV status < 6 months of age
A total of 81 (100%) infant samples were successfully genotyped for α-thalassemia. One infant had a -α3.7/-α3.7 genotype and was excluded from the analysis. There were 46 infants without the thalassemia mutation (αα/αα) of which, 37/46 (80.4%) were EBV-positive. There were 34 infants’ carriers of -α3.7/αα and 30/34 (88.2%) of these were EBV-positive with the difference between the two genotypic groups being comparable (P = 0.615). Among (n = 81) samples genotyped for SCT, two samples failed to amplify, therefore, n = 79 samples were used for the analysis. There were 62 infant carriers of HbAA, of which 52/62 (83.9%) were EBV-positive. A total of 17 infants had the HbAS genotype, of which 14/17 (82.4%) were EBV-positive. The differences between the groups were also comparable (P = 1.000). The EBV infection status for the 7 G6PD mutation types (n = 81) was as follows; 72 infants had the Viangchan/Chinese genotype with 62/72 (86.1%) being EBV-positive. The difference between carriers and non-carriers of the genotypes was comparable (P = 0.153). There were 76 infants with the Mahidol/Coimbra mutation of which 63/76 (82.9%) were EBV-positive. The difference between carriers and non-carriers of the genotype was comparable (P = 0.407). There were 66 infants with the Union/ Kaiping mutation, of which 54/66 (81.8%) were EBV-positive. The difference between carriers and non-carriers of the genotype was comparable across groups (P = 0.197). Among 80 infant samples genotyped for African A- variant, 19 were carriers of A-, of which 13/19 (68.4%) were EBV positive. There were 55 infants’ carriers of the A variant with 48/55 (87.3%) being EBV-positive and 6 carriers of the B variant of which 6/6 (100%) were EBV-positive. The distribution of the African A- alleles across the three groups was also comparable (P = 0.084). There were 70 mother samples genotyped for the MSP-2 genotypes as an indicator of in-utero exposure to malaria. There were 20 infants exposed in utero to the FC27 genotype of which 17/20 (85%) were EBV positive. There were 41 infants exposed in utero to the 3D7 genotype, of which 35/41 (85.4%) were EBV-positive. The difference between groups was comparable between the exposed and the unexposed for both the FC27 and 3D7 allelic groups (P = 0.914 and P = 0.921) respectively (Table 3).
Distribution of alpha thalassemia, SCT, G6PD and MSP-2 mutations based on EBV status ≥ 6-12months of age
The EBV infection status ≥ 6–12 months of age was as follows: Among the 46 (56.8%) infants with the αα/αα genotype 19/46 (41.3%) were EBV-infected. Of the 34 infants’ carriers of -α3.7/αα, 10/34 (29.4%) were EBV-infected with a comparable difference between the two genotypic groups (P = 0.413). Out of the 79 infant samples analyzed for SCT genotype, there were 62 infants’ carriers of HbAA of which, 25/62 (40.3%) were EBV-infected. Of the 17 infant carriers of HbAS, 4/17 (13.8%) were EBV-infected and the difference between the two genotypic groups was comparable (P = 0.249). The distribution of the 7 G6PD variants, based on EBV status among the 81 infants was as follows: there were 72 infants with Viangchan 871G > A /Chinese 1024 C > T mutation type with 26/72 (32.1%) EBV-infected [carriers vs. non-carriers were comparable (P = 0.616)]. There were 76 infants’ carriers of the Mahidol 487G > A/Coimbra 592 C > T mutation type, of which 28/76 (34.6%) were EBV-infected with the difference between carriers and non-carriers being comparable (P = 0.442). There were 66 infants’ carriers of the Union 1360 C > T/ Kaiping 1388G > A mutation type with 25/66 (30.9%) EBV-infected [carriers vs. non-carriers were also comparable (P = 0.494)]. There were 55 infants’ carriers of the G6PD A variant of which 24/55 (30.0%) were EBV-infected. Infants’ carriers of the A- variant were 19 of which 5/19 (6.3%) were EBV-infected. Of the 6 infants with the B variant, 1/6 (1.3%) was EBV-infected and the difference between carriers of the three variants was comparable (P = 0.280). The MSP-2 genotyping used 70 mother samples of which 41 (50.6%) and 20 (24.7%) had the 3D7 and FC27 alleles, respectively. There were 41 infants with in-utero exposure to 3D7 with 13/41 (31.7%) EBV-infected, while 20 infants with in utero exposure to the FC27 [7/20 (24.1%) were EBV-infected]. The difference between carriers of FC27 and 3D7 and non-carriers was comparable (P = 0.814 and P = 0.263, respectively, Table 3).
Association between carriage of hemoglobinopathy gene, MSP-2 allele, and EBV acquisition < 6 months of age
The relationship between hemoglobinopathies and EBV acquisition is presented in Table 4. There was no statistically significant association between hemoglobinopathies and EBV acquisition < 6 months. Neither the -α3.7/αα [OR = 1.824, (95% CI = 0.511–6.512), P = 0.354] nor the SCT [OR = 0.897, (95% CI = 0.217–3.708), P = 0.881) were associated with the acquisition of EBV. The odds of EBV infection were, however, higher in infants < 6 months compared to the ≥ 6–12 months age category. There was no association between EBV acquisition and the Viangchan 871G > A /Chinese 1024 C > T variant [OR = 2.614, (95% CI = 0.578–11.820), P = 0.212], Mahidol 487G > A/Coimbra592C > T variant [OR = 0.000, (95% CI = 0.000), P = 0.999, or Union 1360 C > T/Kaiping 1388G > A variant [OR = 0.321, (95% CI = 0.038–2.686), P = 0.295]. For the G6PD African variant, the regression model did not generate odds ratios and/or 95% CI, likely due to the smaller sample sizes within the individual group variants. However, a combination of B and A variants as the reference category established a significant association of A- and EBV acquisition [OR = 0.281, (95% CI = 0.081–0.978), P = 0.046]. In utero exposure to MSP-2 alleles (n = 70) did not show any significant associations between exposure to FC 27 [OR = 0.922, (95% CI = 0.213–3.990), P = 0.914] or 3D7 [OR = 0.933, (95% CI = 0.238–3.656), P = 0.921] and EBV acquisition (Table 4).
Association between carriage of hemoglobinopathy gene, MSP-2 allele, and EBV acquisition ≥ 6–12 months of age
Infants with -α3.7/αα were not significantly protected from EBV acquisition ≥ 6-12months [OR = 0.681, (95% CI = 0.256–1.812), P = 0.442]. The Hb AS genotype was not associated with EBV acquisition in the ≥ 6–12 months group [OR = 0.513, (95% CI = 0.143–1.836), P = 0.305]. None of the seven G6PD variants was associated with EBV acquisition nor were the Viangchan 871G > A /Chinese 1024 C > T variant [OR = 0.640, (95% CI = 0.079–5.205), P = 0.677], Mahidol 487G > A/Coimbra592C > T variant [OR = 0.948, (95% CI = 0.240–3.755), P = 0.940], or Union 1360 C > T/Kaiping 1388G > A variant [OR = 1.221, (95% CI = 0.325–4.592), P = 0.768]. The G6PD African A- mutation also showed no association with EBV acquisition [OR = 1.000, (95% CI = 0.000–0.000), P = 0.235], nor did the A variant [OR = 0.278 (95% CI = 0.030–2.544), P = 0.257]. An analysis of the MSP-2 genotypes and EBV acquisition demonstrated that in utero exposure to either of the MSP-2 alleles was not associated with EBV acquisition in FC 27 [OR = 0.780, (95% CI = 0.256–2.373), P = 0.662] or 3D7 [OR = 0.549, (95% CI = 0.201–1.496), P = 0.241]. Based on the odds ratios the probability of an EBV infection was generally higher < 6 months compared to ≥ 6–12 months.
Discussion
Despite the long-held hypothesis that EBV infection during infancy and P. falciparum infection are risk factors for eBL, the causal relationship between early EBV infection and eBL development in children from malaria-endemic regions remains unknown [22, 33]. Endemic BL and malaria have a similar geographic distribution, and polymorphisms of RBCs such as sickle cell trait (SCT), α-thalassemia, and G6PD deficiency have been associated with protection against malaria in malaria-endemic regions [18, 34, 35]. For instance, in Western Kenya, there is a high prevalence rate of clinically relevant hemoglobinopathies [36, 37]. However, whether these hemoglobinopathies could also influence EBV acquisition is yet to be determined. Therefore, the current study sought to understand the significance of these hemoglobinopathies—SCT, alpha-thalassemia, and G6PD-mutations, in the early ages of EBV acquisition. This study hypothesized that certain hemoglobinopathies may protect against EBV acquisition at an early age.
There is a high prevalence of alpha thalassemia along the lake belt region of Kenya with the advantage of being protective in P. falciparum malaria disease severity [38]. Data on its role in viral infections is scanty, with studies pointing at susceptibility to transfusion-related hepatitis B and C viral infections in homozygous individuals [39, 40]. Similarly, in an experimental setup, a significant reduction in susceptibility of erythroid committed precursor cells to Dengue virus from -α3.7/αα compared to normal control cells has also been documented [41]. In a binary regression model, with the wild-type gene as a reference group, there was no association between the -α3.7/αα variants and susceptibility to EBV infection. The lack of an association could be attributed to the mechanistic effect of erythrocytic phagocytosis processes established in P. falciparum parasitized thalassemic red blood cells (RBCs) [42]. Based on this fact, we hypothesize that there are likely additional molecular mechanisms between thalassemic RBCs and EBV acquisition that was beyond the scope of the current study.
The effect of SCT on malaria disease has also been studied in Western Kenya revealing a 16.2% prevalence in the child population from this malaria-endemic region [9, 11]. The clinical importance of SCT in viral diseases has also been demonstrated in HIV where SCT has a protective effect in reducing the progression of HIV-1 to AIDS, and consequently a reduced prevalence of HIV-1 in the African American population [43, 44]. A combined synergistic effect between SCT and blood group O in reducing the risk of eBL in Nigeria has also been reported [45]. Nevertheless, the current study revealed that children with SCT were not significantly protected from the acquisition of EBV contrary to the previously established protective association of SCT in HIV-1 infection and malaria disease. It can be speculated that in malaria disease, SCT reduces parasite densities and inhibit intracellular parasite growth, thereby, reducing the probability of suffering from severe malaria [46]. Additionally, molecular mechanisms through the upregulation of complex proteins have been proposed as protective against HIV-1 infection for individuals with SCT [44]. Similarly, a previous study in Western Kenya suggested that chronic malaria and elevated EBV viral loads are factors in eBL disease, rather than the presence of the SCT [14]. Therefore, these mechanisms cannot be definitively ascertained as protective in EBV susceptibility for individuals with SCT.
Worldwide, over 300 variants of the G6PD gene have been characterized [47]. The World Health Organization (WHO) has proposed the reclassification of G6PD based on the biochemical and phenotypic characteristics of variants [48, 49]. Genetic variations of the G6PD gene have been reported with significant clinical implications in different populations [15] as exemplified in West Africa and, within ethnically diverse populations in South Africa [50, 51]. The current study established the presence of non-synonymous mutations from the sampled population from Western Kenya (Mahidol 487G > A, Kaiping 1388G > A, Union 1360 C > T, and Viangchan 871G > A, Chinese4 392G > T). These mutations have been associated with known G6PD deficient phenotypes [52]. The G6PD Mahidol is associated with moderate enzyme activity, comparable to the African A- [53, 54], and is considered the predominant variant in Southeast Asia [55,56,57]. The G6PD Kaiping 1388G > A and Union 1360 C > T are the most common variants in Southern China [52]. The effects of the G6PD mutation in viral infections have previously been studied in Asia where the Mahidol variant is predominant and has no significant protective role against Dengue [58]. An ex vivo study from the same Asian population established that immune cells (monocytes) from G6PD patients were at a higher risk of viral infections [59] and recent studies have linked G6PD deficiency with susceptibility to coronavirus (COVID-19) [60, 61]. The current study established a high prevalence of these mutation types from the sampled population, but they did not influence EBV acquisition. In the West African and Asian populations, the G6PD 968 C and the Mediterranean 563 C > T variant were associated with enzyme deficiency and protection against severe malaria [51, 52]. The 968 C mutation has a similar phenotypic characteristic to the African A- variant [55]. It is estimated that within sub-Saharan Africa, 10% of the population have the phenotypic G6PD A (376 A > G) or G6PD A- (202G > A) mutation with the 376 A > G mutation as a modifier [62]. The current study did not establish a significant association between the African A or A- variants and EBV acquisition. It is however important to note that the distribution of G6PD variants within the malaria-endemic region of Western Kenya has solely been based on the detection of the A- haplotype [63], even though other studies have shown that the distribution of G6PD variants can vary based on geographical and ethnic groups [55, 57, 64, 65]. The current study highlights significant G6PD variants that have previously not been studied in this population for their role in EBV acquisition. Overall, the lack of protective association of the G6PD genotypes could suggest that the mechanism of protection of G6PD in malaria might differ from that in viral infections [58].
The EBV-associated eBL has a geographically similar distribution pattern to endemic malaria [20, 66]. In EBV-associated eBL pathogenesis, environmental, genetic, and immune-related factors have been implicated. For example, it has been established that children residing in malaria-endemic regions acquire EBV infection by six months of age on average, compared to those from non-endemic regions, thus implicating P. falciparum as well as EBV in breast milk as a causal factor in EBV transmission or eBL development [22, 67, 68]. Immune-related interactions in malaria and EBV infection share a disease-causal relationship considering that exposure to repeated malarial infections and early ages of EBV infections lead to eBL occurrence [24, 69, 70]. These facts have contributed to studies that aim to establish causal relationships between the two endemic diseases to inform interventions for eBL management [70].
A study of the MSP-2 genotype confirmed that antibodies against this blood-stage parasite gene are protective against severe malaria outcomes [71,72,73]. The current study aimed to establish the role of in-utero exposure to MSP-2 genotypes (3D7 and FC27) in the acquisition of EBV. Based on the fact that previous findings reported 35% of infants born in Western Kenya, compared to those from the highlands, are EBV-infected before 6 months of age [22]. This study explored how in-utero exposure to 3D7 and FC27 MSP-2 allelic variants alter susceptibility to EBV infection before and after 6 months of age. The current study did not find any relationship between in-utero exposure to MSP-2 and EBV acquisition. These findings are in line with previous observations in which there was no demonstration of a protective role of the gene in arthropod-borne viral infection [74]. The lack of an association of MSP-2 in EBV acquisition could therefore be attributed to immune-modulating mechanisms and the presence of other P. falciparum antigens that are not invoked in EBV infection [75,76,77,78]. Other mechanisms involving inhibition of erythrocyte invasion and replication, such as complement-dependent mechanisms [79], and elimination of infected blood cells by circulating immune cells in malaria disease, could also be factors [80]. Additionally, EBV could employ survival mechanisms that enable it to evade immune responses as has been established in its latency cycle within immune B-cells [81]. To the best of our knowledge, the current study established novel G6PD mutations within the population from western Kenya and suggests that further studies should explore enzyme levels and phenotypic characteristics for the G6PD variants detected in this population. Such future studies may offer important clinical relevance for the management and treatment of childhood malaria in endemic regions. Additionally, this study was limited in that larger sample sizes from multiple study sites and with higher age groups above 12 months of age would be required to demonstrate that SCT, α-thalassemia, G6PD, and MSP-2 mutations are not significantly associated with EBV acquisition. The current study only explored the value of a few genes that drive the differential presentation of malaria in EBV acquisition within one geographical region in Western Kenya. To establish that the known and novel hemoglobinopathies, and infant in utero MSP-2 exposure to EBV do not confer susceptibility to EBV, future studies with larger sample sizes and that use advanced techniques like transcriptome and epigenetics analysis could be used. This will highlight the gene variants that are important in EBV susceptibility.
Conclusions
Based on the findings from this study, we conclude that SCT, α-thalassemia, G6PD mutations, and in-utero exposure to MSP-2 do not influence EBV susceptibility in infants from the malaria holoendemic region of Western Kenya. Therefore, hemoglobinopathies and in-utero exposure to MSP-2 genotypes do not appear to alter susceptibility to EBV acquisition.
Data Availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- DNA:
-
Deoxyribonucleic Acid
- eBL:
-
Endemic Burkitt’s Lymphoma
- EBV:
-
Epstein Barr virus
- G6PD:
-
Glucose-6-Phosphate Dehydrogenase
- MSP-2:
-
Merozoite Surface Protein-2
- NADPH:
-
Nicotinamide Adenine Dinucleotide Phosphate
- P. f :
-
Plasmodium falciparum
- PCR:
-
Polymerase Chain Reaction
- RBC:
-
Red Blood Cell
- SCT:
-
Sickle Cell Trait
- SCD:
-
Sickle Cell Disease
- µL:
-
Microliter
- α:
-
alpha
- HIV:
-
Human Immunodeficiency Virus
- NADPH:
-
Nicotinamide Adenine Dinucleotide Phosphate
- COVID-19:
-
Corona Virus Disease-19
- SNP Single:
-
Nucleotide polymorphism
- Hb AA:
-
Sickle Cell Normal
References
Queiroga EM, Gualco G, Weiss LM, Dittmer DP, Araujo I, Klumb CEN, et al. Burkitt Lymphoma in Brazil is characterized by geographically distinct clinicopathologic features. Am J Clin Pathol. 2008;130(6):946–56.
Orem J, Mbidde EK, Lambert B, Sanjose Sd, Weiderpass E. Burkitt’s lymphoma in Africa, a review of the epidemiology and etiology. Afr Health Sci. 2007;7(3):166.
Rowe M, Fitzsimmons L, Bell AI. Epstein-Barr virus and Burkitt lymphoma. Chin J Cancer. 2014;33(12):609–19.
Suh JK, Gao YJ, Tang JY, Jou ST, Lin DT, Takahashi Y, et al. Clinical characteristics and treatment outcomes of Pediatric patients with Non-Hodgkin Lymphoma in East Asia. Cancer Res Treat. 2020;52(2):359–68.
Walter MO, R R, M MA, L WM. A M, C W,. Burkitt’s lymphoma in Kenya: geographical, age, gender and ethnic distribution. 2004.
Rainey JJ, Mwanda WO, Wairiumu P, Moormann AM, Wilson ML, Rochford R. Spatial distribution of Burkitt’s lymphoma in Kenya and association with malaria risk. Trop Med Int Health. 2007;12(8):936–43.
Kanda T, Yajima M, Ikuta K. Epstein-Barr virus strain variation and cancer. Cancer Sci. 2019;110(4):1132–9.
Derby KS, Sullivan KM, Ruth LJ, Williams TN, Suchdev PS. The relationship between inherited blood disorders and iron biomarkers among young children in Kenya. FASEB J. 2013;27(1supplement):1078–8.
Byrd KA, Williams TN, Lin A, Pickering AJ, Arnold BF, Arnold CD, et al. Sickle cell and α+-Thalassemia Traits Influence the Association between Ferritin and Hepcidin in rural kenyan children aged 14–26 months. J Nutr. 2018;148(12):1903–10.
Piel FB, Patil AP, Howes RE, Nyangiri OA, Gething PW, Williams TN, et al. Global distribution of the sickle cell gene and geographical confirmation of the malaria hypothesis. Nat Commun. 2010;1:104.
Piel FB, Patil AP, Howes RE, Nyangiri OA, Gething PW, Dewi M, et al. Global epidemiology of sickle haemoglobin in neonates: a contemporary geostatistical model-based map and population estimates. Lancet. 2013;381(9861):142–51.
Croke K, Ishengoma DS, Francis F, Makani J, Kamugisha ML, Lusingu J, et al. Relationships between sickle cell trait, malaria, and educational outcomes in Tanzania. BMC Infect Dis. 2017;17(1):568.
Gong L, Parikh S, Rosenthal PJ, Greenhouse B. Biochemical and immunological mechanisms by which sickle cell trait protects against malaria. Malar J. 2013;12(1):317.
Mulama DH, Bailey JA, Foley J, Chelimo K, Ouma C, Jura WGZO, et al. Sickle cell trait is not associated with endemic Burkitt lymphoma: an ethnicity and malaria endemicity-matched case–control study suggests factors controlling EBV may serve as a predictive biomarker for this pediatric cancer. Int J Cancer. 2014;134(3):645–53.
Howes RE, Piel FB, Patil AP, Nyangiri OA, Gething PW, Dewi M et al. G6PD Deficiency Prevalence and estimates of affected populations in Malaria endemic countries: a geostatistical model-based map. PLoS Med. 2012;9(11).
Cappellini MD, Fiorelli G. Glucose-6-phosphate dehydrogenase deficiency. Lancet. 2008;371(9606):64–74.
Donati D, Espmark E, Kironde F, Mbidde EK, Kamya M, Lundkvist A, et al. Clearance of circulating Epstein-Barr virus DNA in children with acute malaria after antimalaria treatment. J Infect Dis. 2006;193(7):971–7.
Kariuki SN, Williams TN. Human genetics and malaria resistance. Hum Genet. 2020;139(6–7):801–11.
Osier FHA, Murungi LM, Fegan G, Tuju J, Tetteh KK, Bull PC, et al. Allele-specific antibodies to Plasmodium falciparum merozoite surface protein-2 and protection against clinical malaria. Parasite Immunol. 2010;32(3):193–201.
Moormann AM, Bailey JA. Malaria – how this parasitic infection aids and abets EBV-associated Burkitt lymphomagenesis. Curr Opin Virol. 2016;20:78.
Daud II, Ogolla S, Amolo AS, Namuyenga E, Simbiri K, Bukusi EA, et al. Plasmodium falciparum infection is associated with Epstein-Barr virus reactivation in pregnant women living in malaria holoendemic area of western Kenya. Matern Child Health J. 2015;19(3):606–14.
Piriou E, Asito AS, Sumba PO, Fiore N, Middeldorp JM, Moormann AM, et al. Early Age at Time of Primary Epstein–Barr virus infection results in poorly controlled viral infection in Infants from Western Kenya: clues to the etiology of endemic Burkitt Lymphoma. J Infect Dis. 2012;205(6):906–13.
Moormann AM, Chelimo K, Sumba OP, Lutzke ML, Ploutz-Snyder R, Newton D, et al. Exposure to holoendemic malaria results in elevated Epstein-Barr virus loads in children. J Infect Dis. 2005;191(8):1233–8.
Rochford R. Epstein-Barr virus infection of infants: implications of early age of infection on viral control and risk for Burkitt lymphoma. Boletín Médico del Hospital Infantil de México. 2016;73(1):41–6.
Rainey JJ, Omenah D, Sumba PO, Moormann AM, Rochford R, Wilson ML. Spatial clustering of endemic Burkitt’s lymphoma in high-risk regions of Kenya. Int J Cancer. 2007;120(1):121–7.
Ndenga B, Githeko A, Omukunda E, Munyekenye G, Atieli H, Wamai P, et al. Population dynamics of malaria vectors in western Kenya highlands. J Med Entomol. 2006;43(2):200–6.
Kapesa A, Kweka EJ, Atieli H, Afrane YA, Kamugisha E, Lee MC, et al. The current malaria morbidity and mortality in different transmission settings in western Kenya. PLoS ONE. 2018;13(8):e0202031.
Wanjiku CM, Njuguna F, Chite Asirwa F, Mbunya S, Githinji C, Roberson C, et al. Establishing care for sickle cell disease in western Kenya: achievements and challenges. Blood Adv. 2019;3(Suppl 1):8–10.
Ogolla SO, Daud II, Asito AS, Sumba OP, Ouma C, Vulule J, et al. Reduced Transplacental transfer of a subset of Epstein-Barr Virus-Specific antibodies to neonates of mothers infected with Plasmodium falciparum Malaria during pregnancy. Clin Vaccine Immunol. 2015;22:1197–205.
Kosiyo P, Otieno W, Gitaka J, Munde EO, Ouma C. Association between haematological parameters and sickle cell genotypes in children with Plasmodium falciparum malaria resident in Kisumu County in Western Kenya. BMC Infect Dis. 2020;20(1):887.
Liu O, Miles, Fisher, Weatherall C. Rapid detection of α-thalassaemia deletions and α-globin gene triplication by multiplex polymerase chain reactions. Br J Haematol. 2000;108(2):295–9.
Zhang L, Yang Y, Liu R, Li Q, Yang F, Ma L, et al. A multiplex method for detection of glucose-6-phosphate dehydrogenase (G6PD) gene mutations. Int J Lab Hematol. 2015;37(6):739–45.
de-The G. Is Burkitt’s lymphoma related to perinatal infection by Epstein-Barr. virus? Lancet. 1977;1(8007):335–8.
Allen SJ, O’Donnell A, Alexander ND, Alpers MP, Peto TE, Clegg JB, et al. alpha+-Thalassemia protects children against disease caused by other infections as well as malaria. Proc Natl Acad Sci USA. 1997;94(26):14736–41.
Mbanefo EC, Ahmed AM, Titouna A, Elmaraezy A, Trang NTH, Phuoc Long N et al. Association of glucose-6-phosphate dehydrogenase deficiency and malaria: a systematic review and meta-analysis. Sci Rep. 2017;7.
Aidoo M, Terlouw DJ, Kolczak MS, McElroy PD, ter Kuile FO, Kariuki S, et al. Protective effects of the sickle cell gene against malaria morbidity and mortality. Lancet. 2002;359(9314):1311–2.
Williams TN, Weatherall DJ. World distribution, Population Genetics, and Health Burden of the Hemoglobinopathies. Cold Spring Harb Perspect Med. 2012;2(9).
Buckle G, Maranda L, Skiles J, Ong’echa JM, Foley J, Epstein M, et al. Factors influencing survival among kenyan children diagnosed with endemic Burkitt lymphom between 2003 and 2011: a historical cohort study. Int J Cancer. 2016;139(6):1231–40.
Shah T, Hussain W, Ali N, Sardar S, Ishaq M, Ur Rahman M, et al. Frequency distribution and risk factors of hepatitis B virus and hepatitis C virus infections among thalassemia patients: a regional study. Eur J Gastroenterol Hepatol. 2019;31(2):248–52.
de Melo Silva J, Pinheiro-Silva R, Dhyani A, Pontes GS. Cytomegalovirus and Epstein-Barr Infections: Prevalence and Impact on Patients with Hematological Diseases. Biomed Res Int. 2020;2020:1627824.
Sornjai W, Khungwanmaythawee K, Svasti S, Fucharoen S, Wintachai P, Yoksan S, et al. Dengue virus infection of erythroid precursor cells is modulated by both thalassemia trait status and virus adaptation. Virology. 2014;471–473:61–71.
Krause MA, Diakite SA, Lopera-Mesa TM, Amaratunga C, Arie T, Traore K, et al. α-Thalassemia impairs the cytoadherence of Plasmodium falciparum-infected erythrocytes. PLoS ONE. 2012;7(5):e37214.
Kumari N, Ammosova T, Diaz S, Lin X, Niu X, Ivanov A, et al. Increased iron export by ferroportin induces restriction of HIV-1 infection in sickle cell disease. Blood Adv. 2016;1(3):170–83.
Nekhai S, Kumari N. HIV-1 infection in sickle cell disease and sickle cell trait: role of iron and innate response. Expert Rev Hematol. 2022;15(3):253–63.
Ahamed SG, Ibrahim UA, Kagu MB. Synergistic protective effect of Sickle Cell Trait and Blood Group-O on the risk of endemic Burkitt’s Lymphoma. Gulf J Oncol. 2018;1(28):11–6.
Archer NM, Petersen N, Clark MA, Buckee CO, Childs LM, Duraisingh MT. Resistance to Plasmodium falciparum in sickle cell trait erythrocytes is driven by oxygen-dependent growth inhibition. Proc Natl Acad Sci USA. 2018;115(28):7350–5.
Nkhoma ET, Poole C, Vannappagari V, Hall SA, Beutler E. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: a systematic review and meta-analysis. Blood Cells Mol Dis. 2009;42(3):267–78.
Tong Y, Liu B, Zheng H, Bao A, Wu Z, Gu J, et al. A novel G6PD deleterious variant identified in three families with severe glucose-6-phosphate dehydrogenase deficiency. BMC Med Genet. 2020;21(1):150.
Organization WH. WHO malaria policy advisory group (MPAG) meeting: meeting report, March 2022. 2022 924004843X.
da Rocha J, Othman H, Tiemessen CT, Botha G, Ramsay M, Masimirembwa C et al. G6PD variant distribution in sub-Saharan Africa and potential risks of using chloroquine/hydroxychloroquine based treatments for COVID-19. medRxiv: the preprint server for health sciences. 2020.
Clark TG, Fry AE, Auburn S, Campino S, Diakite M, Green A, et al. Allelic heterogeneity of G6PD deficiency in West Africa and severe malaria susceptibility. Eur J Hum genetics: EJHG. 2009;17(8):1080–5.
Li Q, Yang F, Liu R, Luo L, Yang Y, Zhang L, et al. Prevalence and molecular characterization of Glucose-6-Phosphate Dehydrogenase Deficiency at the China-Myanmar Border. PLoS ONE. 2015;10(7):e0134593.
Laosombat V, Sattayasevana B, Chotsampancharoen T, Wongchanchailert M. Glucose-6-phosphate dehydrogenase variants associated with favism in thai children. Int J Hematol. 2006;83(2):139–43.
Burgoine KL, Bancone G, Nosten F. The reality of using primaquine. Malar J. 2010;9:376.
Howes RE, Dewi M, Piel FB, Monteiro WM, Battle KE, Messina JP, et al. Spatial distribution of G6PD deficiency variants across malaria-endemic regions. Malar J. 2013;12:418.
Yi H, Li H, Liang L, Wu Y, Zhang L, Qiu W, et al. The glucose-6-phosphate dehydrogenase Mahidol variant protects against uncomplicated Plasmodium vivax infection and reduces disease severity in a Kachin population from northeast Myanmar. Infect Genet evolution: J Mol Epidemiol evolutionary Genet Infect Dis. 2019;75:103980.
Phompradit P, Kuesap J, Chaijaroenkul W, Rueangweerayut R, Hongkaew Y, Yamnuan R, et al. Prevalence and distribution of glucose-6-phosphate dehydrogenase (G6PD) variants in Thai and burmese populations in malaria endemic areas of Thailand. Malar J. 2011;10:368.
May WL, Kyaw MP, Blacksell SD, Pukrittayakamee S, Chotivanich K, Hanboonkunupakarn B, et al. Impact of glucose-6-phosphate dehydrogenase deficiency on dengue infection in Myanmar children. PLoS ONE. 2019;14(1):e0209204.
Chao YC, Huang CS, Lee CN, Chang SY, King CC, Kao CL. Higher infection of dengue virus serotype 2 in human monocytes of patients with G6PD deficiency. PLoS ONE. 2008;3(2):e1557.
Yang HC, Ma TH, Tjong WY, Stern A, Chiu DT. G6PD deficiency, redox homeostasis, and viral infections: implications for SARS-CoV-2 (COVID-19). Free Radic Res. 2021:1–11.
Jamerson BD, Haryadi TH, Bohannon A. Glucose-6-Phosphate dehydrogenase Deficiency: an actionable risk factor for patients with COVID-19? Arch Med Res. 2020;51(7):743–4.
Town M, Bautista JM, Mason PJ, Luzzatto L. Both mutations in G6PD A — are necessary to produce the G6PD deficient phenotype. Hum Mol Genet. 1992;1(3):171–4.
Shah SS, Macharia A, Makale J, Uyoga S, Kivinen K, Craik R, et al. Genetic determinants of glucose-6-phosphate dehydrogenase activity in Kenya. BMC Med Genet. 2014;15:93.
Charoenkwan P, Tantiprabha W, Sirichotiyakul S, Phusua A, Sanguansermsri T. Prevalence and molecular characterization of glucose-6-phosphate dehydrogenase deficiency in northern Thailand. Southeast Asian J Trop Med Public Health. 2014;45(1):187–93.
Manjurano A, Sepulveda N, Nadjm B, Mtove G, Wangai H, Maxwell C, et al. African glucose-6-phosphate dehydrogenase alleles associated with protection from severe malaria in heterozygous females in Tanzania. PLoS Genet. 2015;11(2):e1004960.
Aka P, Kawira E, Masalu N, Emmanuel B, Brubaker G, Magatti J, et al. Incidence and Trends in Burkitt Lymphoma in Northern Tanzania from 2000 to 2009. Pediatr Blood Cancer. 2012;59(7):1234–8.
Legason ID, Pfeiffer RM, Udquim K-I, Bergen AW, Gouveia MH, Kirimunda S, et al. Evaluating the Causal Link between Malaria infection and endemic Burkitt Lymphoma in Northern Uganda: a mendelian randomization study. EBioMedicine. 2017;25:58–65.
Daud II, Coleman CB, Smith NA, Ogolla S, Simbiri K, Bukusi EA, et al. Breast milk as a potential source of Epstein-Barr Virus Transmission among Infants living in a Malaria-Endemic Region of Kenya. J Infect Dis. 2015;212(11):1735–42.
Yone CL, Kube D, Kremsner PG, Luty AJ. Persistent Epstein-Barr viral reactivation in young african children with a history of severe Plasmodium falciparum malaria. Trans R Soc Trop Med Hyg. 2006;100(7):669–76.
Shannon-Lowe C, Rickinson A. The Global Landscape of EBV-Associated Tumors. Front Oncol. 2019;9:713.
Osier FH, Fegan G, Polley SD, Murungi L, Verra F, Tetteh KK, et al. Breadth and magnitude of antibody responses to multiple Plasmodium falciparum merozoite antigens are associated with protection from clinical malaria. Infect Immun. 2008;76(5):2240–8.
Taylor RR, Allen SJ, Greenwood BM, Riley EM. IgG3 antibodies to Plasmodium falciparum merozoite surface protein 2 (MSP2): increasing prevalence with age and association with clinical immunity to malaria. Am J Trop Med Hyg. 1998;58(4):406–13.
Metzger WG, Okenu DM, Cavanagh DR, Robinson JV, Bojang KA, Weiss HA, et al. Serum IgG3 to the Plasmodium falciparum merozoite surface protein 2 is strongly associated with a reduced prospective risk of malaria. Parasite Immunol. 2003;25(6):307–12.
Niang M, Loucoubar C, Sow A, Diagne MM, Faye O, Faye O, et al. Genetic diversity of Plasmodium falciparum isolates from concurrent malaria and arbovirus co-infections in Kedougou, southeastern Senegal. Malar J. 2016;15:155.
Murungi LM, Sondén K, Llewellyn D, Rono J, Guleid F, Williams AR, et al. Targets and Mechanisms Associated with Protection from severe Plasmodium falciparum malaria in kenyan children. Infect Immun. 2016;84(4):950–63.
al-Yaman F, Genton B, Kramer KJ, Chang SP, Hui GS, Baisor M, et al. Assessment of the role of naturally acquired antibody levels to Plasmodium falciparum merozoite surface protein-1 in protecting Papua New guinean children from malaria morbidity. Am J Trop Med Hyg. 1996;54(5):443–8.
Egan AF, Morris J, Barnish G, Allen S, Greenwood BM, Kaslow DC, et al. Clinical immunity to Plasmodium falciparum malaria is associated with serum antibodies to the 19-kDa C-terminal fragment of the merozoite surface antigen, PfMSP-1. J Infect Dis. 1996;173(3):765–9.
Riley EM, Wagner GE, Ofori MF, Wheeler JG, Akanmori BD, Tetteh K, et al. Lack of association between maternal antibody and protection of african infants from malaria infection. Infect Immun. 2000;68(10):5856–63.
Boyle MJ, Reiling L, Feng G, Langer C, Osier FH, Aspeling-Jones H, et al. Human antibodies fix complement to inhibit Plasmodium falciparum invasion of erythrocytes and are associated with protection against malaria. Immunity. 2015;42(3):580–90.
Osier FH, Feng G, Boyle MJ, Langer C, Zhou J, Richards JS, et al. Opsonic phagocytosis of Plasmodium falciparum merozoites: mechanism in human immunity and a correlate of protection against malaria. BMC Med. 2014;12:108.
Long HM, Taylor GS, Rickinson AB. Immune defence against EBV and EBV-associated disease. Curr Opin Immunol. 2011;23(2):258–64.
Acknowledgements
We are grateful to Chulaimbo Sub-County Hospital, the caregivers, and the children whose samples were used in this study. We also appreciate Dr. Sarah Kituyi for her assistance with corrections and edits during the review process.
Funding
This work was supported by National Research Fund (NRF-Prof. Collins Ouma) and Fogarty International Center (FIC)-National Institutes of Health (NIH)-[(7R01-TW008306-05-CO) and D43TW05884-05 grant (Prof. Douglas J. Perkins)].
Author information
Authors and Affiliations
Contributions
PKO, SSA, ASA, SO, RR, DJP and CO conceptualised the study. PKO, EM, SBA, ER, EN, COO participated in data collection, data analysis and write-up of the manuscript. All co-authors reviewed and provided intellectual input in the completed manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval for this study was granted by Jaramogi Oginga Odinga University of Science and Technology, ethics committee. Informed consent was obtained from all subjects and/or their legal guardian(s). The study permit was granted by National Commission for Science, Technology, and Innovation (NACOSTI), Kenya. All the experiments were performed following relevant guidelines and regulations as per the Declaration of Helsinki. Consent to publish was obtained from the legal guardians of all the study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Olewe, P.K., Awandu, S.S., Munde, E.O. et al. Hemoglobinopathies, merozoite surface protein-2 gene polymorphisms, and acquisition of Epstein Barr virus among infants in Western Kenya. BMC Cancer 23, 566 (2023). https://doi.org/10.1186/s12885-023-11063-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11063-2