Abstract
Introduction
Endoscopic ultrasound (EUS) may play a role in evaluating treatment response after definitive chemoradiation therapy (dCRT) for esophageal squamous cell carcinoma (ESCC). This study explored the prognostic markers of EUS with biopsies and developed two nomograms for survival prediction.
Methods
A total of 821 patients newly diagnosed with ESCC between January 2015 and December 2019 were reviewed. We investigated the prognostic value of the changes in tumor imaging characteristics and histopathological markers by an interim response evaluation, including presence of stenosis, ulceration, tumor length, tumor thickness, lumen involvement, and tumor remission. Independent prognostic factors of progression-free survival (PFS) and overall survival (OS) were determined using Cox regression analysis and further selected to build two nomogram models for survival prediction. The receiver operating characteristic (ROC) curve, calibration curve, and decision curve analysis (DCA) were used to respectively assess its discriminatory capacity, predictive accuracy, and clinical usefulness.
Results
A total of 155 patients were enrolled in this study and divided into the training (109 cases) and testing (46 cases) cohorts. Tumor length, residual tumor thickness, reduction in tumor thickness, lumen involvement, and excellent remission (ER) of spatial luminal involvement in ESCC (ER/SLI) differed significantly between responders and non-responders. For patients undergoing dCRT, tumor stage (P = 0.001, 0.002), tumor length (P = 0.013, 0.008), > 0.36 reduction in tumor thickness (P = 0.004, 0.004) and ER/SLI (P = 0.041, 0.031) were independent prognostic markers for both PFS and OS. Time-dependent ROC curves, calibration curves, and DCA indicated that the predicted survival rates of our two established nomogram models were highly accurate.
Conclusion
Our nomogram showed high accuracy in predicting PFS and OS for ESCC after dCRT. External validation and complementation of other biomarkers are needed in further studies.
Similar content being viewed by others
Introduction
Definitive chemoradiation therapy (dCRT) is a superior alternative for patients with unresectable esophageal cancer (EC) or those unwilling to undergo operative management [1]. In China, the pathological type of EC is, in the majority, esophageal squamous cell carcinoma (ESCC), which is dramatically inconsistent with the adenocarcinomas in Western countries [2]. In all, 40–75% of patients with ESCC may develop local recurrence after dCRT, with an increased risk of poor survival [3]. It has been reported that the clinical outcomes of EC significantly correlate with the tumor response to dCRT. Patients with a complete response (CR) to dCRT appear to be more likely to develop long-term survival, while those with residual disease are recommended to continue with reinforced or salvage treatment [4]. As a result, patients with less sensitivity to treatment are recommended to receive 60 Gy as a definitive radiation dose to improve localized control, rather than the international recommended standard dose of 50 Gy [5,6,7,8]. It is essential to evaluate the tumor response to dCRT, especially at an early timepoint, to predict the prognosis of patients with ESCC and determine whether additional reinforced therapeutic strategies are required.
Numerous studies have been carried out to evaluate the essential role of endoscopic ultrasound (EUS) in staging primary EC and treating early-stage EC with minimal local involvement [9]. EUS evaluations have been suggested to play a role in predicting pathological CR in patients with EC after neoadjuvant chemoradiation therapy (nCRT), and tumor thickness was significantly correlated with tumor remission grade. To date, relatively few studies have investigated the potential role of EUS in assessing tumor treatment response and predicting the prognosis of patients with ESCC who receive dCRT [10, 11].
At our institution, patients who underwent dCRT and had not received treatment previously for EC were recommended to have an interim response evaluation. EUS with biopsies was conducted when the radiation dose reached 40 Gy. Additional information was obtained about the tumor response to dCRT, which would greatly help guide subsequent management and assess prognosis [12, 13].
The current study aimed to evaluate the role of interim response evaluation in predicting treatment response and patient survival for ESCC according to a comparison of the results of pre- and interim-treatment EUS-based measurements.
Materials and methods
Patients and treatments
Between January 1, 2015, and December 31, 2019, a cohort of 821 patients who underwent dCRT and had not received treatment previously for EC (stage I-IVA) at the Tianjin Medical University Cancer Institute and Hospital were enrolled. Only biopsy-confirmed squamous cell carcinoma with pre- and interim-treatment EUS measurements was eligible for inclusion (Supplementary Figure S1). The included patients were categorized into training and testing cohorts (7:3) according to the timing of treatment initiation. The tumor-node-metastasis (TNM) staging system proposed by the American Joint Committee on Cancer (8th edition) was used. In patients who received dCRT, radiotherapy was performed with conventional fractionation schedules (5 days/week, 1.8–2.0 Gy/daily fraction). The radiation dose ranged from 45.0 to 63.0 Gy, with a median dose of 54.0 Gy, in 30 fractions using intensity modulated radiotherapy (IMRT) with concomitant chemotherapy, mainly 4 to 6 cycles (docetaxel and cisplatin, weekly).
Treatment evaluation
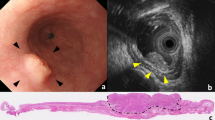
EUS examinations with biopsies were performed in patients with EC before dCRT treatment. When the radiation dose reached 40 Gy, usually four to five weeks into treatment, EUS with biopsies was repeated. At least three different sites of any suspicious lesions in the esophagus were considered for biopsies. Examination records were reviewed for the presence of stenosis, ulceration, tumor length, tumor thickness, lumen involvement, and tumor remission. Among them, the tumor length was the distance between the upper and lower edges of the esophageal tumor. The tumor thickness was measured in millimeters from the esophageal lumen to the outer tumor edge (Fig. 1A). In cases of an impassable esophagus, the maximum tumor thickness of the passable part was measured instead. Lumen involvement was defined as the proportion of spartial and circumferential tumors involving the esophageal lumen (Fig. 1A). The proportion of lumen involvement ≤ 0.67 during the interim evaluation was recorded as spatial luminal involvement (SLI). Histopathological evaluation was based on a scoring system originally designed to evaluate microscopic response to chemoradiation therapy (CRT) in ESCC [12, 14, 15]. Tumor remission was classified into three grades, and details are given in Fig. 1B and Supplementary Table S1. All patients were assessed clinically based on CT, esophagography, and ultrasonography of the neck and abdomen 1 month after dCRT, according to the Response Evaluation Criteria for Solid Tumors (RECIST 1.1) [16].
Tumor thickness, lumen involvement and histopathologic response of esophageal squamous cell carcinoma tissues during dCRT. (A) EUS-based evaluation of tumor thickness (white line) and lumen involvement (blue shaded area) pre- and interim-treatment in the same patient. (B) Tumor remission during dCRT was graded in 3 levels: excellent remission, good remission, and minor remission (arrows indicate residual tumor). Abbreviations: T, tumor thickness; LI, lumen involvement; dCRT, definitive chemoradiation therapy; EUS, endoscopic ultrasound
Follow-up
Patients were monitored approximately every 3 months for 1 year, every 6 months for the next 2 years, and annually thereafter. Overall survival (OS) was measured from the initiation of treatment to the date of death or the date of the last follow-up. Progression-free survival (PFS) was calculated from the initiation of treatment to the date of lesion progression, including the primary tumor, regional lymph nodes, and distant areas. Locoregional recurrence (LRR) was defined as the time from the initiation of therapy to the progression of the irradiated regions. Patients with a LRR ≥ 24 months were classified as the group of responders [17].
Statistical analyses
Continuous variables were analyzed using Mann-Whitney U test, and categorical variables were tested using the chi-square test or the Fisher exact test. Age, tumor length, baseline tumor thickness, residual tumor thickness, and lumen involvement were grouped with the median value. The cutoff value of the reduction in tumor thickness was calculated by the Youden index. Survival curves were plotted by the Kaplan–Meier method and assessed using the log-rank test. Univariate and multivariate Cox regression analyses were performed to generate hazard ratios (HR) and 95% confidence intervals (CI), and to explore the prognostic variables for constructing nomograms. The “pec,” “rms,” and “ggDCA” packages of R were applied to generate time-dependent receiver operating characteristic (ROC) curves, calibration curves, and decision curve analysis (DCA) for validating the nomogram, respectively [18]. All statistical tests were 2-tailed. A P < 0.05 represented a significant value. All analyses and data visualization were performed in SPSS (Version 25.0) and the R programming language (version 4.0.5).
Results
Patient characteristics and overall treatment response
A total of 155 patients were enrolled in this study, with a median age of 62 years (range, 44 to 82 years), and were divided into training (109 patients) and testing cohorts (46 patients). The median follow-up was 43.4 months (95% CI, 41.3 to 45.4 months). By December 2021, fifty (32.3%) patients were still alive and 119 (76.8%) patients experienced relapse, of which 62 (52.1%) suffered a local recurrence (LR), 45 (37.8%) suffered a regional recurrence (RR), and 35 (29.4%) suffered distant metastases (DMs). The 1-, 2-, and 3-year OS rates were 73.4%, 48.1%, and 36.1%, respectively. Fifty-nine (42.8%) patients were classified as active responders, and 79 (57.2%) patients as non-responders.
Interim analysis
The presence of stenosis and ulceration were observed in 63 (40.6%) of 155 and 30 (19.4%) of 155 patients, respectively. Excellent remission (ER), good remission (GR), and minor remission (MR) were achieved by 77 (49.7%), 47 (30.3%), and 31 (20.0%) patients, respectively (Fig. 2A). The interim response evaluation revealed that, after CRT, tumor thickness was significantly reduced in patients with ESCC (P < 0.001) (Fig. 2B). However, no obvious changes of lumen involvement were observed during the treatment in these patients (P = 0.072) (Fig. 2 C).
Prognostic significance of the interim analysis
A significant correlation was found between the interim response evaluation outcomes and responders. Stenosis (P = 0.043), tumor length (P < 0.001), residual tumor thickness (P < 0.001), reduction of tumor thickness (P < 0.001), and tumor remission (P = 0.024) were significantly different between responders and non-responders (Table 1). No significant correlations were found for ulceration (P = 0.399), baseline tumor thickness (P = 0.363) and lumen involvement at baseline (P = 0.057) and during treatment (P = 0.052) (Table 1). Responders had a lower proportion of lumen involvement than non-responders; however, the p-value was not significant. We then combined tumor remission with spatial luminal involvement (SLI) during treatment; ER and SLI tumors achieved higher predictive values for responders, with a specificity of 83.6% (66/79, 95%CI 73.1–90.6%, P < 0.001) (Table 1). Tumor clinical characteristics of responders and non-responders are shown in Supplementary Table S2.
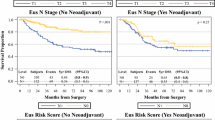
Independent prognostic factors for PFS and OS
Survival data for the primary cohort were analyzed. Patients with ER or SLI tended to have improved PFS and OS compared to those without, although the difference was not significant (PFS, P = 0.058, 0.086; OS, P = 0.11, 0.12). However, patients with both ER and SLI had significantly better PFS and OS than those with ER alone, SLI alone, or neither (PFS, P = 0.004; OS, P = 0.002) (Fig. 3).
Table 2 shows the results of the univariate Cox regression analysis. Stenosis, baseline T, baseline N, TNM stage, tumor length, and reduction in tumor thickness were associated with PFS and OS. Residual tumor thickness was only associated with OS (P = 0.042), but not with PFS (P = 0.109). Since the TNM stage combines the depth of tumor infiltration and the status of lymph node metastasis, we only included the TNM stage for further multivariate Cox regression analysis. Finally, TNM stage (P = 0.001, 0.002), tumor length (P = 0.013, 0.008), reduction in tumor thickness (P = 0.004, 0.004), and ER/SLI (P = 0.041, P = 0.031) were found to be independent prognostic factors for PFS and OS (Table 3).
Development and validation of nomograms
Using the four independently prognostic markers, we constructed two nomograms to predict the 1-, 2-, and 3-year PFS and OS for ESCC patients who received dCRT (Fig. 4A, D). The possibilities of PFS and OS at 1, 2 and 3 years were estimated by adding the points of each item on the nomogram.
Construction and validation of the nomogram for predicting PFS and OS. The nomogram for predicting 1-, 2-, and 3-year PFS (A) and OS (D) of patients with ESCC. Time-dependent ROC curves of the nomogram for PFS (B, C) and OS (E, F) prediction in the training and the testing cohorts. Abbreviations: ER, excellent remission; SLI, spatial luminal involvement; PFS, progression-free survival; OS, overall survival
We mainly evaluated the predictability of the nomograms from three aspects: discrimination, calibration, and clinical effectiveness. Our nomograms yielded a C-index of 0.713 (95% CI 0.663–0.762) in predicting PFS and 0.711 (95% CI 0.657–0.765) in predicting OS. Additionally, the time-dependent ROC curves of the nomograms demonstrated a better discrimination of PFS (Fig. 4B, C) and OS (Fig. 4E, F) than those of the TNM stage at almost all time points in the follow-up, in both the training and testing cohorts. The calibration curves and the DCA diagrams also indicated the superior accuracy of the predictions (Supplementary Figure S2).
Discussion
In the current study, we assessed both tumor imaging characteristics and histopathological performance by EUS with biopsies to capture the changes in tumor burden from the macro and micro perspectives, which indicated the response of tumors to dCRT. We found that reduction in tumor thickness, tumor length, ER/SLI, and TNM stage were significantly associated with local control and the survival probability of patients with ESCC. Furthermore, we established two visualized nomogram models combining these prognostic markers, which may enable clinicians to stratify prognostic subgroups and adapt the therapeutic schedule for patients with ESCC.
Most studies try to assess the early response of tumors to dCRT in patients with EC using magnetic resonance imaging (MRI), positron emission tomography with integrated computed tomography (PET/CT), or other imaging examinations. Quantitative imaging values, especially for classical MRI parameters, such as ADC values, differ between scanners and might not be standardized, as the values of ADC vary in different MRI devices [19, 20]. Another nonnegligible disadvantage is that MRI or PET/CT cannot discern the lesions confined to the mucosal layer [17]. Sakurada et al. combined high-resolution T2-weighted images with diffusion-weighted magnetic resonance imaging (DWI) for the detection of early EC, and only 33% of T1 carcinomas were detected accurately [21]. Subsequently, some other studies have highlighted the value of EUS in overcoming these limitations, which had become a standard measurement to identify tumor histological types and assist in tumor staging of patients with EC.
The predictive value of EUS has been confirmed in the nCRT field. A single-center retrospective study revealed that tumor thickness reduced by more than 50% after neoadjuvant therapy was significantly associated with tumor downgrade and long-term survival [22]. Another substudy of the preSANO trial did not find an association between tumor response and the reduction ratio of tumor thickness [11]. However, an absolute value of tumor thickness > 4.5 mm after completion of nCRT could predict residual disease with a sensitivity of 87%. In our present study, both residual thickness and changes in tumor thickness showed a significant correlation with active responders (Residual, P < 0.001; reduction in thickness, P < 0.001). However, survival analysis showed that only changes in tumor thickness were correlated with patient survival rates and were considered as an independent prognostic marker of PFS and OS. The possible causes for this discrepancy may be the difference in tumor histological types and the varied cutoff values of tumor thickness in different studies.
Compared with esophageal adenocarcinoma, posttreatment endoscopic biopsy played an improved role in predicting treatment response to CRT of ESCC. Qian et al. found that ER combined with tumor-infiltrating lymphocytes > 60% (LPE, lymphocyte-predominant ESCC) during CRT correlated with pCR and cancer-specific survival for patients with ESCC. During the interim response evaluation, patients evaluated with ER/LPE tended to have more improved survival rates compared with other patients who had ESCC [12]. Similar results were found in our present study, patients with ER or SLI were associated with a better PFS and OS in ESCC; however, the difference was not significant. When we combined both factors, patients with ER/SLI obtained significantly improved PFS (P = 0.004) and OS (P = 0.002) rates than other patients. We have also found a significant correlation between ER/SLI and responders. ER/SLI showed high predictive values for 2-year locoregional control, with a specificity of 83.6%. In other words, cases that did not achieve both ER and LIE during treatment tended to have locoregional failure after dCRT. This information obtained at the early timepoint of the treatment would have great importance in guiding subsequent management and assessing prognosis.
To our knowledge, our study is the first to assess EUS-based measurements pre- and interim-dCRT to evaluate the tumor response to dCRT in ESCC patients. Compared with the individual value before or during treatment, we believed that the reduction in tumor thickness was more significant in tumor assessment clinically for patients with ESCC who received dCRT, which was also consistent with the findings from other previous studies [22,23,24,25]. Using changes in tumor thickness appears superior for early tumor response evaluation compared to downgrading traditional EUS-based T staging [24, 26]. Another strength of this study was the relatively complete clinical data, including both tumor imaging characteristics and histopathological evaluation at baseline and during the treatment, which helped to assess the tumor response to dCRT comprehensively. In addition, at least three different sites of any suspicious lesions were considered for biopsies. Similar to bite-on-bite biopsies in the preSANO trial [10], a second biopsy sample was conducted at the same site, which helped detect residual tumors. Finally, we integrated the clinical parameters and pathological markers of tumors and established two visualized nomogram models with high accuracy in predicting PFS and OS.
Many studies have built prognostic models to predict the treatment response and survival probability of patients with EC who receive CRT [20, 27,28,29]. However, few studies have been specifically designed for squamous histology, whose clinicopathological features and biological behavior remarkably differ from adenocarcinoma. Only patients with ESCC who had complete clinical data and evaluation records were included in our study to ensure the reliability and accuracy of our nomograms. In addition, our nomograms are the first EUS-based models that are well-validated in another relatively independent cohort of patients with ESCC who were treated with dCRT. The selected prognostic markers in our nomograms were available to clinicians and easily applied to clinical practice. With great predictive performance in both the training cohort and testing cohorts, we believed that our models would have great potential to guide clinicians in assessing the overall treatment response and adapting therapy strategies of patients with ESCC. Low-risk cases may have satisfactory long-term survival, so close surveillance is recommended. However, other cases with poor treatment response may require a multidisciplinary approach, and a more intensive radiation dose is suggested.
We acknowledge the limitations of our analysis. In the interim response evaluation of 29 impassable esophagi, we measured the tumor thickness of the passable part, which may be less than the actual maximum tumor thickness, resulting in a limited influence on the results. Second, it is the genome that determines the sensitivity of esophageal cancer to CRT; from this point of view, our nomograms may not adequately assess the true response. A nomogram based on CD8, Foxp3, CD33, and PD-L1 yielded an AUC of 0.764 for 5-year OS prediction [30]. Other molecular biomarkers, such as ALDH1 and GLI1/HH, which have been reported to be associated with the therapeutic response [31], could be of complementary value to develop the current models. Finally, this was a retrospective single-institution analysis, and the performance of our models need to be validated in a larger external cohort.
Conclusion
Based on prognostic markers acquired from EUS with biopsies, we constructed and validated two individual nomograms to estimate PFS and OS in patients with ESCC who underwent dCRT. Before application in clinical practice, our current models must be validated and further refined, and their incorporation with other critical molecular biomarkers should also be further explored.
Data availability
The clinicopathological data used to support the findings of this study are available from the corresponding author upon request.
Change history
25 July 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12885-023-11206-5
Abbreviations
- dCRT:
-
Definitive chemoradiation therapy
- EC:
-
Esophageal cancer
- ESCC:
-
Esophageal squamous cell carcinoma
- CR:
-
Complete response
- EUS:
-
Endoscopic ultrasound
- nCRT:
-
Neoadjuvant chemoradiation therapy
- CRT:
-
Chemoradiation therapy
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- LRR:
-
Locoregional recurrence
- HR:
-
Hazard ratios
- CI:
-
Confidence intervals
- ROC:
-
Receiver operating characteristic()
- DCA:
-
Decision curve analysis
- ER:
-
Excellent remission
- GR:
-
Good remission
- MR:
-
Minor remission
- SLI:
-
Spatial luminal involvement
- MRI:
-
Magnetic resonance imaging
- PET/CT:
-
Positron emission tomography with integrated computed tomography
- DWI:
-
Diffusion-weighted magnetic resonance imaging
- LPE:
-
Lymphocyte-predominant esophageal squamous cell carcinoma
References
Kamarajah SK, Phillips AW, Hanna GB, et al. Definitive Chemoradiotherapy compared to Neoadjuvant Chemoradiotherapy with Esophagectomy for Locoregional Esophageal Cancer: National Population-based Cohort Study. Ann Surg. 2022;275:526–33.
Yang S, Lin S, Li N, et al. Burden, trends, and risk factors of esophageal cancer in China from 1990 to 2017: an up-to-date overview and comparison with those in Japan and South Korea. J Hematol Oncol. 2020;13:146.
Teoh AY, Chiu PW, Yeung WK, et al. Long-term survival outcomes after definitive chemoradiation versus surgery in patients with resectable squamous carcinoma of the esophagus: results from a randomized controlled trial. Ann Oncol. 2013;24:165–71.
Shah MA, Kennedy EB, Catenacci DV, et al. Treatment of locally Advanced Esophageal Carcinoma: ASCO Guideline. J Clin Oncol. 2020;38:2677–94.
Markar S, Gronnier C, Duhamel A, et al. Salvage surgery after Chemoradiotherapy in the management of Esophageal Cancer: is it a viable therapeutic option? J Clin Oncol. 2015;33:3866–73.
Welsh J, Settle SH, Amini A, et al. Failure patterns in patients with esophageal cancer treated with definitive chemoradiation. Cancer. 2012;118:2632–40.
Ren X, Wang L, Han C, et al. Retrospective analysis of safety profile of high-dose concurrent chemoradiotherapy for patients with oesophageal squamous cell carcinoma. Radiother Oncol. 2018;129:293–9.
Chang CL, Tsai HC, Lin WC, et al. Dose escalation intensity-modulated radiotherapy-based concurrent chemoradiotherapy is effective for advanced-stage thoracic esophageal squamous cell carcinoma. Radiother Oncol. 2017;125:73–9.
Short MW, Burgers KG, Fry VT. Esophageal Cancer. Am Fam Physician. 2017;95:22–8.
Noordman BJ, Spaander MCW, Valkema R, et al. Detection of residual disease after neoadjuvant chemoradiotherapy for oesophageal cancer (preSANO): a prospective multicentre, diagnostic cohort study. Lancet Oncol. 2018;19:965–74.
van der Bogt RD, Noordman BJ, Krishnadath KK, et al. Endoscopic ultrasound measurements for detection of residual disease after neoadjuvant chemoradiotherapy for esophageal cancer. Endoscopy. 2019;51:326–32.
Qian D, Wang Y, Zhao G, et al. Tumor Remission and Tumor-Infiltrating lymphocytes during chemoradiation therapy: predictive and prognostic markers in locally advanced esophageal squamous cell carcinoma. Int J Radiat Oncol Biol Phys. 2019;105:319–28.
Yeom JG, Kim JH, Kim JW et al. Prognostic Significance of Interim Response Evaluation during Definitive Chemoradiotherapy for Locally Advanced Esophageal Squamous Cell Carcinoma.Cancers (Basel)2021;13.
Yu JP, Lu WB, Wang JL, et al. Pathologic response during chemo-radiotherapy and variation of serum VEGF levels could predict effects of chemo-radiotherapy in patients with esophageal cancer. Asian Pac J Cancer Prev. 2015;16:1111–6.
Brun E, Zatterstrom U, Kjellen E, et al. Prognostic value of histopathological response to radiotherapy and microvessel density in oral squamous cell carcinomas. Acta Oncol. 2001;40:491–6.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Qiu B, Wang D, Yang H, et al. Combined modalities of magnetic resonance imaging, endoscopy and computed tomography in the evaluation of tumor responses to definitive chemoradiotherapy in esophageal squamous cell carcinoma. Radiother Oncol. 2016;121:239–45.
Balachandran VP, Gonen M, Smith JJ, et al. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16:e173–180.
Schob S, Meyer HJ, Dieckow J et al. Histogram Analysis of Diffusion Weighted Imaging at 3T is Useful for Prediction of Lymphatic Metastatic Spread, Proliferative Activity, and Cellularity in Thyroid Cancer.Int J Mol Sci2017;18.
Borggreve AS, Goense L, van Rossum PSN, et al. Preoperative prediction of pathologic response to Neoadjuvant Chemoradiotherapy in patients with Esophageal Cancer using (18)F-FDG PET/CT and DW-MRI: a prospective Multicenter Study. Int J Radiat Oncol Biol Phys. 2020;106:998–1009.
Sakurada A, Takahara T, Kwee TC, et al. Diagnostic performance of diffusion-weighted magnetic resonance imaging in esophageal cancer. Eur Radiol. 2009;19:1461–9.
Ribeiro A, Franceschi D, Parra J, et al. Endoscopic ultrasound restaging after neoadjuvant chemotherapy in esophageal cancer. Am J Gastroenterol. 2006;101:1216–21.
Mesenas S, Vu C, McStay M, et al. A large series, resection controlled study to assess the value of radial EUS in restaging gastroesophageal cancer following neoadjuvant chemotherapy. Dis Esophagus. 2008;21:37–42.
Chak A, Canto MI, Cooper GS, et al. Endosonographic assessment of multimodality therapy predicts survival of esophageal carcinoma patients. Cancer. 2000;88:1788–95.
Wu Y, Li J. Change in maximal esophageal Wall Thickness provides prediction of survival and recurrence in patients with esophageal squamous cell Carcinoma after Neoadjuvant Chemoradiotherapy and surgery. Cancer Manag Res. 2021;13:2433–45.
Shim CN, Song MK, Lee HS, et al. Prediction of survival by tumor area on endosonography after definitive chemoradiotherapy for locally advanced squamous cell carcinoma of the esophagus. Digestion. 2014;90:98–107.
Suzuki A, Xiao L, Hayashi Y, et al. Nomograms for prognostication of outcome in patients with esophageal and gastroesophageal carcinoma undergoing definitive chemoradiotherapy. Oncology. 2012;82:108–13.
Yip C, Landau D, Kozarski R, et al. Primary esophageal cancer: heterogeneity as potential prognostic biomarker in patients treated with definitive chemotherapy and radiation therapy. Radiology. 2014;270:141–8.
Larue R, Klaassen R, Jochems A, et al. Pre-treatment CT radiomics to predict 3-year overall survival following chemoradiotherapy of esophageal cancer. Acta Oncol. 2018;57:1475–81.
Duan J, Xie Y, Qu L, et al. A nomogram-based immunoprofile predicts overall survival for previously untreated patients with esophageal squamous cell carcinoma after esophagectomy. J Immunother Cancer. 2018;6:100.
Noordman BJ, van Lanschot JJB, group Ss. Oesophageal preservation in locally advanced oesophageal cancer - authors’ reply. Lancet Oncol. 2018;19:e431.
Acknowledgements
We would like to acknowledge the patients who participated in this study.
Funding
This work is supported by the National Natural Science Foundation of China (Grant No.82073348 and No.81872462) and Tianjin Key Medical Discipline (Specialty) Construction Project (TJYXZDXK-009 A).
Author information
Authors and Affiliations
Contributions
PQ, CX, and WP conceptualized the study. DQ, WX, and ZK collected the patient date. PQ, CX, and WP contributed to data curation. CF and ZG analyzed and interpreted data. DQ and WX drafted the manuscript. ZW, PQ, and CX revised the manuscript for critical intellectual content. All authors have seen and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
All authors have completed the ICMJE uniform disclosure form. The authors have no conflicts of interest to declare.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Tianjin Medical University Cancer Institute and Hospital (approval number: bc2022102). The need for written informed consent was waived by the Tianjin Medical University Cancer Institute and Hospital Ethics Committee due to retrospective nature of the study.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Materials
: Supplementary Figure S1: Patient selection. Supplementary Figure S2: Figure S2 Validation of the nomogram for predicting PFS and OS. (A-D) Calibration curves and DCA of the nomogram for PFS prediction in the training and the testing cohorts. (E-H) Calibration curves, and DCA of the nomogram for OS prediction in the training and the validation cohorts. Abbreviations: PFS, progression-free survival; OS, overall survival; DCA, decision curve analysis. Supplementary Table S1: The scoring grades of chemoradiotherapy effect†,1-4. Supplementary Table S2: Figure S2 Tumor Characteristics of responders and non-responders.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Du, Q., Wu, X., Zhang, K. et al. Predictive and prognostic markers from endoscopic ultrasound with biopsies during definitive chemoradiation therapy in esophageal squamous cell carcinoma. BMC Cancer 23, 681 (2023). https://doi.org/10.1186/s12885-023-10803-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-10803-8