Abstract
Background
Anlotinib is a multi-targeted receptor tyrosine kinase inhibitor (TKI) which has exhibited encouraging clinical activity in advanced non-small cell lung cancer (NSCLC) and soft tissue sarcoma. Raltitrexed is well known to be effective in the treatment of colorectal cancer in China. The present study aims to investigate the combinatory antitumor effect of anlotinib and raltitrexed on human esophageal squamous carcinoma cells and further explore the molecular mechanisms in vitro.
Methods
Human esophageal squamous cell lines KYSE-30 and TE-1 were treated with anlotinib or raltitrexed, or both, then cell proliferation was measured by MTS and colony formation assay; cell migration and invasion were detected by wound-healing and transwell assays; cell apoptosis rate was studied by flow cytometry and the transcription of apoptosis-associated proteins were monitored by quantitative polymerase chain reaction (qPCR) analysis. Finally, western blot was performed to check phosphorylation of apoptotic proteins after treatment.
Results
Treatment with raltitrexed and anlotinib showed enhanced inhibitory effects on cell proliferation, migration and invasiveness compared with raltitrexed or anlotinib monotherapy. Meanwhile, raltitrexed combined with anlotinib strongly increased cell apoptosis percentage. Moreover, the combined treatment down-regulated mRNA level of the anti-apoptotic protein Bcl-2 and invasiveness-associated protein matrix metalloproteinases-9 (MMP-9), while up-regulated pro-apoptotic Bax and caspase-3 transcription. Western blotting showed that the combination of raltitrexed and anlotinib could inhibit the expression of phosphorylated Akt (p-Akt), Erk (p-Erk) and MMP-9.
Conclusions
This study indicated that raltitrexed enhanced the antitumor effects of anlotinib on human ESCC cells by down-regulating phosphorylation of Akt and Erk, providing a novel treatment option for patients with esophageal squamous cell carcinoma (ESCC).
Similar content being viewed by others
Background
Esophageal cancer has been identified as the eighth most common cause of cancer-related death all over the world [1]. Esophageal squamous cell carcinoma (ESCC) accounts for more than 95% of the pathological types of esophageal cancer in China [2]. Despite radical surgery, systemic chemotherapy, and radiotherapy are often administered in clinical practice, disease recurrence often develops within a few years, the five-year survival rate is only 8 to 20% [3, 4]. Since more than one third of patients with esophageal cancer are already advanced at the time of diagnosis, and the overall physical tolerance of patients is slightly poor, it is urgent to develop targeted therapy with less toxic and side effects.
Anlotinib is a novel oral multi-targeted receptor tyrosine kinase inhibitor (TKI), which can effectively inhibit VEGFR, PDGFR, FGFR, C-KIT and other kinases, and has anti-tumor angiogenesis and anti-tumor growth effects [5,6,7,8]. Results from a number of previous phase II and III clinical trials have shown that amlotinib exhibits good antitumor activity in a variety of solid tumors, including non-small-cell lung cancer, renal carcinoma, gastric cancer, hepatocarcinoma and soft tissue sarcoma [9]. In addition, anlotinib has been approved by CFDA in 2018 for the treatment of locally advanced or metastatic NSCLC patients who have progressed or relapsed following prior treatment with two systemic chemotherapy treatments. However, there is little experience in the treatment of ESCC patients with anlotinib.
Raltitrexed, also named ZD1694, has been considered as an antimetabolic folate analogue that specifically inhibits thymidylate synthase (TS). TS is a key enzyme in the synthesis of thymidine deoxynucleoside triphosphate (TTP), which is an essential nucleotide for DNA synthesis. Inhibition of TS can lead to DNA breakage and apoptosis [10]. The efficacy of raltitrexed is similar to that of 5-FU, but it can prolong survival and improve quality of life. At present, it is mainly used for the treatment of colorectal cancer patients. In addition, previous studies have demonstrated encouraging antitumor effects of raltitrexed in a variety of tumors, including liver cancer, gastric cancer, malignant mesothelioma, and head and neck cancer, based on its antiproliferative and antiapoptotic activity [11,12,13,14].
This is the first attempt to investigate the combined therapeutic effect of raltitrexed and anlotinib on human ESCC and its possible internal mechanism. Since vascular endothelial growth factor receptor-2 (VEGFR-2) is considered to be the primary performer of VEGF-induced antitumor angiogenesis, anlotinib has shown a highly selective inhibitory effect on VEGFR-2 [15,16,17]. We further hypothesis that the combinatory antitumor effects of raltitrexed and anlotinib are achieved through inhibition of the downstream signaling pathways of VEGFR-2. Two signaling pathways PI3K/Akt/mTOR and Raf/Mek/Erk1/2 are explored as possible mechanisms. Our work will provide a reliable scientific theoretical basis for the combined application of the two drugs in the treatment of human ESCC.
Methods
Cell culture and reagents
Human esophageal cancer cell lines KYSE-30 and TE-1 were acquired from the department of experimental research center in Beijing Friendship Hospital (Beijing, China). These two human esophageal squamous cell carcinoma cells were cultured in Roswell Park Memorial Institute (RPMI)-1640 (Hyclone, Termo Scientifc, MA) supplemented with 10% FBS (fetal bovine serum; Biological Industries, Tel Aviv, Israel) and 1% penicillin/streptomycin (KeyGen, Nanjing, China) at 37 °C in a humidified atmosphere of 5% CO2. Anlotinib and raltitrexed were kindly given as gifts by Chia Tai Tianqing Co., Ltd. (Nanjing, China). Anlotinib and raltitrexed were dissolved in dimethyl sulfoxide (DMSO, Sigma, St. Louis, USA) and stored at − 20 °C for in vitro studies, and diluted with medium before each test.
Cell viability assay
The in vitro cytotoxicity were measured by MTS (Vicmed, Xuzhou, Jiangsu, China) assay [18]. Briefly, cells were seeded in 96-well plates at a density of 4 × 103 cells/well at 37 °C overnight. Subsequently, treated with anlotinib or raltitrexed at indicated concentrations or time. After incubating for 24 or 48 h, the cells were washed twice with PBS and then MTS working solution was added into each well and incubated for 1 h at 37 °C according to the manufacturer’s protocol. The resulting absorbance (A) was measured at 490 nm by an microplate reader (Bio-Tek Instruments, USA). The proliferation inhibition rate was calculated by the following formula [cell proliferation inhibition rate (%) = 1-(A value of experimental group-A value of blank group)/(A value of control group-A value of blank group) × 100%]. Triplicate experiments were performed in parallel manner for each concentration point.
Colony formation assay
ESCC cell lines KYSE-30 and TE-1 were placed into six-well plates at a density of 500 cells/well and treated with appropriate drug conditions (20 μM anlotinib, 2.5 μM raltitrexed, 20 μM anlotinib plus 2.5 μM raltitrexed or its corresponding control) at 37 °C, 5% CO2 for approximately 14 days, the medium needs to be replaced every 3–4 days during this period. After 14 days, cells were washed with 1 × PBS, and fixed with 4% paraformaldehyde reagent in methanol for 15 min at room temperature. When visible colonies were observed, the cells were stained with 0.1% crystal violet for 30 min. The colonies were photographed with a digital camera (Olympus, Corporation, Tokyo, Japan) and colonies containing more than 50 cells were counted using the Image J software and the survival fractions were calculated. We took three pictures of each well in this experiment. The percentage rate of colony formation = number of colonies/number of seeded cells × 100%.
Wound healing assay
Cell migration was assessed by wound healing assay. Cells were seeded into 6-well plates at a density of 6 × 105 cells/well and grown until they reached full confluence. A linear wound was scratched across the cell monolayer with a 200 μL pipette tip. The plates were washed with PBS to remove detached cells, and then fresh medium containing different agents (20 μM anlotinib, 2.5 μM raltitrexed, 20 μM anlotinib plus 2.5 μM raltitrexed or DMSO) were subsequently added to the wells. Cell migration was observed by a light microscope (Olympus, Lake Success, NY, USA) at 0 h, 24 h or 48 h. Migration distance were analyzed using ImageJ software (National Institutes of Health, MD) and three randomly chosen fields were analyzed for each well.
Transwell invasion assay
Cell invasion assay was performed using transwell coculture chambers inserts with Matrigel (Corning, USA). KYSE-30 and TE-1 cells were re-suspended in the upper chambers at a density of 1 × 105 cells/well and treated with different agents (20 μM anlotinib, 2.5 μM raltitrexed, 20 μM anlotinib plus 2.5 μM raltitrexed or DMSO). About 600 μL of RPMI-1640 per well with 10% fetal bovine serumwas added to the lower chambers. After incubated for 24 h at 37 °C, the invaded cells which passed through the membrane were fixed with 4% paraformaldehyde for 30 min and stained with 0.1% crystal violet (Macklin, Shanghai, China) for 10 min at room temperature. Images were acquired by an inverted microscope (Olympus), and the invaded cells were counted after air-drying in 6 random visual fields for each chamber manually. The average invaded cell numbers per view were calculated, and three independent experiments were carried out in triplicate.
Cell apoptotic analysis
For apoptosis analysis, KYSE-30 and TE-1 cells were seeded in 6-well plates at a concentration of 1 × 106 cells/well with different agents for 48 h and divided into the four groups: control, anlotinib (20 μM), raltitrexed (2.5 μM) and anlotinib combined with raltitrexed (20 μM + 2.5 μM), the negative control for apoptosis analysis was the equivalent volume of DMSO. Apoptotic cells were distinguished by Annexin V-FITC/7AAD dual staining using apoptosis detection kit (BD Biosciences, Franklin Lakes, NJ, USA). Cells were collected and washed twice with cold PBS and centrifuged for 10 min at 20,000 rpm at 4 °C. Cells were cultured in 300 μL / 1 × 106 cells of 1 × annexin-binding buffer at room temperature for 5 min to prepare the cell samples for flow cytometry, and then double stained with annexin V-FITC (green) and 7AAD-PerCP (red) for 15 min. The percentage of apoptotic cells was analyzed with a FACS Calibur flow cytometer (BD Biosciences) using Flow Jo software (version 9.8.1). The apoptosis rate in every group was described by Q2 (late apoptosis) + Q3 (early apoptosis). All experiments were repeated for three times.
Quantitative polymerase chain reaction (qPCR) analysis
The qPCR experiments were performed as described previously [19, 20]. The total RNA (Ribonucleic Acid) of cells were extracted using the Trizol buffer (Beyotime) and were reverse-transcribed by Multiscribe™ Reverse Transcriptase (Applied Biosystems, Thermo Scientific Corporation) according to the manufacturer’s instructions. The relative expression was calculated by the comparative Ct method. The primers used for qPCR analysis were shown in Table 1.
Western blot analysis
KYSE-30 and TE-1 cells were treated with reagents at indicated concentrations and harvested 24 h. Cells were collected and lysed with radio immunoprecipitation assay buffer (RIPA) (Beyotime Biotechnology, Jiangsu, China). Protein concentrations were determined using bicinchoninic acid (BCA) protein assay kit (Merck, Darmstadt, Germany). An equal amount of protein (50 μg) for each sample was resolved using 5% or 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS/PAGE) with MOPs running bufer and electrophoretically transferred onto a polyvinylidene difuoride (PVDF) membranes (IPVH00010, Millipore, Massachusetts, USA). After blocking with 5% bovine serum albumin at 37 °C for 1 h, the membranes were incubated with diluted primary antibodies at 4 °C overnight. After washing with cold PBS, the corresponding secondary antibodies were added and followed by ECL detection. The following primary antibodies were used to detect the proteins: Bax (1:1000, Cell Signaling Technology), Bcl-2 (1:1000, Abclonal, Wuhan, China), MMP-9 (1:100, Santa Cruz Biotechnology, Santa Cruz, CA, USA), ERK and p-ERK (1:1000, Cell Signaling Technology), AKT and p-AKT (1:1000, Beverly, MA, USA), VEGFR-2 and p-VEGFR-2 (1:1000, Abcam, Cambridge, UK). Subsequently, the membranes were incubated with anti-rabbit IgG conjugated to HRP secondary antibody (1:5000; Cell Signaling Technology, Inc.) for 1.5 h at room temperature. Finally, immunoreactive bands after incubation with secondary antibodies conjugated to peroxidase were detected using an ECL kit (Beyotime, Nangjing, Jiangsu, China) according to the manufacturer’s instructions. Bands were imaged by using the Fusion Fx7 imager (Vilber Lourmat, France) and analyzed with the ImageJ software (NIH, Bethesda, MD). We tailored the membranes, the upper and lower boundaries according to protein molecular weight, and the left and right boundaries according to different cell lines.
Statistical analysis
All statistical analysis was performed using the GraphPad Prism software package version 6.0 (GraphPad Software, Inc., La Jolla, CA, USA). All data were collected from three independent experiments and expressed as the mean ± standard deviation (SD). Differences between groups were analyzed using one-way analysis of variance (ANOVA). The statistical differences were evaluated by SPSS 20.0 soft ware (IBM Corp., Armonk, NY, USA). P value less than 0.05 (P < 0.05) was considered statistically significant.
Results
Anlotinib combined with raltitrexed inhibited cell proliferation
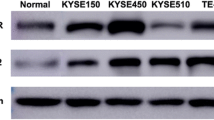
At present, the treatment of tumors is progressing rapidly, but the treatment effect of advanced ESCC is still not ideal and the prognosis is poor. It is worth exploring whether the combination of anlotinib and raltitrexed, a conventional chemotherapy drug, can produce synergistic effects in the treatment of ESCC. To test the efficacy of anlotinib, raltitrexed and the combination of drugs on the proliferation of ESCC cells, we co-cultured different concentrations of anlotinib and raltitrexed with KYSE-30 and TE-1 cell lines which expressed the vascular endothelial growth factor receptor, VEGFR-2 [21,22,23]. As shown in Fig. 1A and B, anlotinib treatment on KYSE-30 and TE-1 cells at a concentrations of 10 μM, 20 μM, 30 μM and 50 μM decreased the cell proliferation rate after 24 or 48 hours of incubation. And it became significantly different from the control group when incubating with 20 μM anlotinib after 24 or 48 hours of incubation. Similarly, when incubated with raltitrexed (Fig. 1C and D) at concentrations of 1.5 μM, 2.0 μM, 2.5 μM, 3.0 μM and 5.0 μM, a significant reduction effect appeared after incubating 24 or 48 hours in comparison to the control. These data indicate both anlotinib and raltitrexed reduced the viability of ESCC cells in a concentration-dependent manner by MTS assay. Based on the above results as well as previous data from our research group [23,24,25], we chose 20 μM anlotinib and 2.5 μM raltitrexed to treat KYSE-30 cells and checked if any combinatory effect existed. As is shown in Fig. 1E, results revealed that anlotinib at 20 μM combined with raltitrexed at 2.5 μM produced stronger inhibition on cell proliferation compared with the anlotinib (P < 0.001) and raltitrexed (P < 0.05) monotherapy groups after incubation with both reagents for 24 h or 48 h. Exactly similar effects were gained for the same treatment on TE-1 cells (Fig. 1F).
Combinated effects of raltitrexed and anlotinib on cell proliferation in ESCC cells. A and B Anlotinib reduced cell proliferation rates of KYSE-30 (A) and TE-1 (B) cells in a dose-dependent manner after 24 h and 48 h treatment. C and D Raltitrexed reduced cell proliferation rates of KYSE-30 (C) and TE-1 (D) cells in a dose-dependent manner after 24 h and 48 h treatment. E and F Cell proliferation rates of KYSE-30 (E) and TE-1 (F) cells after treated with control, 20 μM anlotinib, 2.5 μM raltitrexed or 20 μM anlotinib + 2.5 μM raltitrexed for the indicated time in MTS assays. Data indicate means + SD of three biological replicates. Student’s t test; **P < 0.01, ***P < 0.001 (versus control); #P < 0.05, ###P < 0.001 (versus 20 μM anlotinib or 2.5 μM raltitrexed)
Subsequently, the anti-proliferation effects of anlotinib and raltitrexed on ESCC cells were further verified by colony formation assay. According to the results of the MTS study, 20 μM anlotinib and 2.5 μM raltitrexed were selected as the final concentration of our study, and each cell line was incubated for 14 days with anlotinib or raltitrexed monotherapy or the combination group. From the results in Fig. 2, we observed that the number of colonies formed in the anlotinib and raltitrexed monotherapy groups were significantly decreased than the control group (P < 0.001), while the number of colonies formed in the combination group became almost invisible in the combination group compared with the anlotinib and raltitrexed monotherapy groups (all P < 0.01) in KYSE-30 (Fig. 2A and B) and TE-1 (Fig. 2C and D) cells. Combined with the above results, we concluded that raltitrexed enhanced the anti-proliferation ability of anlotinib on ESCC cells.
Combinated effects of raltitrexed and anlotinib on viability of ESCC cells. A and C Colony formation ability of KYSE-30 (A) and TE-1 (C) cells inhibited by control, 20 μM anlotinib, 2.5 μM raltitrexed or 20 μM anlotinib + 2.5 μM raltitrexed. B and D Quantitative analysis of the number of colonies in KYSE-30 (B) and TE-1 (D) cells. Data indicate means + SD of three biological replicates. Student’s t test; ***P < 0.001 (versus control); ##P < 0.01 (versus 20 μM anlotinib or 2.5 μM raltitrexed)
Anlotinib combined with raltitrexed enhanced the inhibition of cell migration and invasion
The migration and invasion ability of tumor cells are closely related to the occurrence of distant metastasis. We used wound-healing and transwell assays to evaluate the effects of 20 μM anlotinib, 2.5 μM raltitrexed alone or both on migration and invasion of ESCC cells. As shown in Fig. 3, both 20 μM anlotinib and 2.5 μM raltitrexed monotherapy effectively inhibited cell migration in KYSE-30 (Fig. 3A-C) and TE-1 (Fig. 3D-F) cells compared with the control group after scratching for 24 h and 48 h (all P < 0.001). Meanwhile, the inhibitory effects were more obvious in the combination group compared with 20 μM anlotinib and 2.5 μM raltitrexed monotherapy groups.
Combinated effects of raltitrexed and anlotinib on cell migration in ESCC cells. A and D KYSE-30 (A) and TE-1 (D) cells treated with control, 20 μM anlotinib, 2.5 μM raltitrexed or 20 μM anlotinib + 2.5 μM raltitrexed were scraped and imaged immediately (0 h) and later (24 h and 48 h), and images of the wound gap were taken. Scale bar = 100 μm. Quantitative analysis of the wound healing rate in KYSE-30 (B and C) and TE-1 (E and F) cells. Data indicate means + SD of three biological replicates. Student’s t test; ***P < 0.001 (versus control); #P < 0.05, ##P < 0.01, ###P < 0.001 (versus 20 μM anlotinib or 2.5 μM raltitrexed)
Consistent with the wound-healing results, we also observed anlotinib and raltitrexed monotherapy inhibited cell invasion through transwell assay in KYSE-30 (Fig. 4A and B) and TE-1 (Fig. 4C and D) cells compared with the control group after statistical analysis (all P < 0.001). It is worth noting that the inhibitory effect in cell invasion was further reduced by combined treatment of 20 μM anlotinib and 2.5 μM raltitrexed compared with anlotinib and raltitrexed monotherapy. MMP-9 is a major member of the zinc metalloproteinase family because it stimulates cancer metastasis by degrading ECM and collagens, facilitating cancer cell invasion and metastasis [26]. Therefore, MMP-9 is a potentially key molecule in cancer invasion and is considered a target for drug development. In order to explore the mechanisms behind the results above, the level of MMP-9 mRNA was detected by qPCR. As shown in Fig. 6B and F, the level of MMP-9 mRNA expression were significantly decreased following treatment with 20 μM anlotinib and 2.5 μM raltitrexed in KYSE-30 and TE-1 cells (all P < 0.01), and when anlotinib was combined with raltitrexed, further inhibition in MMP-9 expression was observed (P < 0.01). Similar conclusions were found in the results of western blot, as shown in Fig. 7D and L. After 24 hours of anlotinib and raltitrexed treatment of KYSE-30 and TE-1 cell lines, the expression level of MMP-9 showed a significant downward trend compared with the control group, and the downward trend was more significant in the combination group than in 20 μM anlotinib and 2.5 μM raltitrexed monotherapy group (P < 0.01). Taken together, these results demonstrated that raltitrexed enhanced the ability of anlotinib to inhibit the migration and invasion of ESCC cells.
Combinated effects of raltitrexed and anlotinib on cell invasion in ESCC cells. A and C After treatment with control, 20 μM anlotinib, 2.5 μM raltitrexed or 20 μM anlotinib + 2.5 μM raltitrexed for 24 h, invaded cells were stained and counted using microscopy in KYSE-30 (A) and TE-1 (C) cells. B and D Quantitative analysis of the number of invaded cells in KYSE-30 (B) and TE-1 (D) cells. Data indicate means + SD of three biological replicates. Student’s t test; ***P < 0.001 (versus control); ##P < 0.01, ###P < 0.001 (versus 20 μM anlotinib or 2.5 μM raltitrexed)
Anlotinib combined with raltitrexed increased cell apoptosis
To reveal the effects of anlotinib and raltitrexed on cell apoptosis in human esophageal squamous cells, Annexin V and 7AAD staining assay were performed to detect apoptosis rates of KYSE-30 and TE-1 cell lines treated with various reagents for 24 h and then the apoptosis percentage was analyzed by flow cytometry. As shown in Fig. 5, the apoptosis rates of KYSE-30 (Fig. 5A and B) and TE-1 (Fig. 5C and D) cells in both anlotinib and raltitrexed monotherapy groups were significantly higher than those in the control group (all P < 0.001), indicating both of them had strong apoptosis-inducing effects in ESCC cells. More obviously, the apoptosis rates of the combination treatment group were significantly higher than anlotinib and raltitrexed monotherapy groups (all P < 0.01), suggesting that combined treatment could further induce apoptosis.
Combinated effects of raltitrexed and anlotinib on cell apoptosis in ESCC cells. A and C KYSE-30 (A) and TE-1 (C) cells were exposed to control, 20 μM anlotinib, 2.5 μM raltitrexed or 20 μM anlotinib + 2.5 μM raltitrexed for 48 h before Annexin V-FITC and 7AAD-PerCP staining and apoptosis percentage was detected by flow cytometry. B and D Quantitative analysis of the apoptotic rate in KYSE-30 (B) and TE-1 (D) cells. Q1 (necrosis), Q2 (late apoptosis), Q3 (early apoptosis) and Q4 (viable). Data indicate means + SD of three biological replicates. Student’s t test; ***P < 0.01 (versus control); ##P < 0.01 (versus 20 μM anlotinib or 2.5 μM raltitrexed)
Subsequently, we further used qPCR method to investigate the effects of anlotinib and raltitrexed monotherapy and the combination therapy on the transcription levels of apoptosis-related protein in KYSE-30 and TE-1 cell lines. Results as shown in Fig. 6, compared with the control group, the expression levels of pro-apoptotic protein Bax (Fig. 6C and G) and caspase-3 (Fig. 6D and H) mRNA were significantly increased in anlotinib and raltitrexed monotherapy groups, and the elevation became more noticeable in the combination treatment group compared with anlotinib and raltitrexed monotherapy groups. On the contrary, the expression level of anti-apoptotic protein Bcl-2 mRNA decreased in both anlotinib and raltitrexed monotherapy groups compared with the control group, KYSE-30 (P < 0.05) (Fig. 6A) and TE-1 (P < 0.01) (Fig. 6E), and the decrease was more significant in the combination group than in anlotinib and raltitrexed monotherapy groups (all P < 0.001). Consistent with the results assayed by qPCR method, western blot analysis showed the expression of Bax and cleaved caspase-3 were increased in the combination group in both KYSE-30 (Fig. 7B and H) and TE-1 (Fig. 7J and P) cells compared with anlotinib and raltitrexed monotherapy groups. Conversely, the quantitative results in Fig. 7C and K also indicated that the expression of Bcl-2 was decreased in both anlotinib and raltitrexed monotherapy groups compared with the control group (P < 0.05), and the down regulation became more significantly in the combination group compared with anlotinib and raltitrexed monotherapy groups (P < 0.01). Taken together, these results support that retitrexed enhances the apoptosis induced by anlotinib.
Combinated effect of raltitrexed and anlotinib on gene transcription in ESCC cells. mRNA levels of Bcl-2, MMP-9, Bax and Caspase-3 were measured by qPCR in either KYSE-30 (A-D) or TE-1 (E-H) cells after treated by 20 μM anlotinib, 2.5 μM raltitrexed, or both. Data indicate means + SD of three biological replicates. Student’s t test; *P < 0.05, **P < 0.01, ***P < 0.01 (versus control); ##P < 0.01, ###P < 0.001 (versus 20 μM anlotinib or 2.5 μM raltitrexed)
Protein expression after various treatments detected and quantified by Western blot analysis. KYSE-30 (A-H) and TE-1 (I-P) cells were treated with various treatments for 24 h. The protein levels of BAX, BCL-2, MMP-9, p-AKT, AKT, p-ERK, ERK, p-VEGFR-2, VEGFR-2, Caspase-3 and Cleaved Caspase-3 were determined by western blot analysis. β-ACTIN was detected as loading control. *P < 0.05, **P < 0.01 (versus control); #P < 0.05, ##P < 0.01 (versus 20 μM anlotinib or 2.5 μM raltitrexed)
Anlotinib combined with raltitrexed downregulated the expression of p-Akt and p-Erk
Western blot analysis was carried out to clarify the antitumor molecular mechanisms of anlotinib and raltitrexed. We examined PI3K/Akt and Ras/Erk, two major signaling pathways downstream of VEGF signaling pathway [27]. After 24 hours of treatment, it turned out that the expression of phosphorylated Akt (p-Akt) and Erk (p-Erk), which represent the activity of Akt and Erk signaling pathways, were inhibited noticeably by 20 μM anlotinib and 2.5 μM raltitrexed respectively, and the combinatory treatment further decreased p-Akt (Fig. 7E and M) and p-Erk (Fig. 7F and N) level compared with anlotinib and raltitrexed monotherapy group (all P < 0.01). In addition, the level of phosphorylated VEGFR-2 expression was significantly reduced in the anlotinib and raltitrexed monotherapy groups compared with the control group in both KYSE-30 and TE-1 cells, and the decrease was more significant in the combination group compared with the monotherapy group (Fig. 7G and O) (all P < 0.01). These results suggest that raltitrexed may enhance the antitumor effect of anlotinib on human ESCC cells by inhibiting Akt and Erk signaling pathways and affecting the phosphorylation of VEGFR-2.
Discussion
Although in the past decades, the choice of treatment options for advanced ESCC has been greatly developed, getting rid of the constraints of conventional chemotherapy regimens, the overall treatment effect of ESCC patients still needs to be improved due to the characteristics of drug resistance and highly invasive of ESCC, as well as the reduced physical endurance of patients after repeated chemotherapy.
The concept of tumor growth relied on the formation of tumor blood vessels was proposed by professor Folkman in 1971, which suggested that anti-tumor angiogenesis would be a potential strategy for cancer treatment [28]. Vascular endothelial growth factor receptors (VEGFRs) play an important role in pathological angiogenesis, VEGF-targeting has emerged as a viable therapeutic options for several malignancies [29]. VEGFR-2 is functionally activated through autophosphorylation of its carboxyl terminus and subsequently stimulates PI3K/Akt and Ras/Erk signaling pathways mediated cell proliferation and metastasis. Anlotinib is an orally, multi-targeted small molecule TKI that blocks VEGFR-2 phosphorylation. Previous clinical trials have demonstrated antitumor activity of anlotinib in a variety of solid tumors. Nevertheless, there are very few studies detailing the clinical efficacy of anlotinib in patients with ESCC. At the same time, with the extension of treatment time, drug resistance becomes an inevitable clinical problem. In addition, oral TKI alone can not achieve the optimal anti-tumor effect. 5-FU is an indispensable routine drug in chemotherapy for ESCC patients. However, drug side effects have been encountered in numerous patients, therefore, it is necessary to establish alternatives with lower levels of toxicity. Different from 5-FU, raltitrexed is a more suitable choice for ESCC patients with a history of heart disease because of its low incidence of cardiotoxicity and digestive system adverse reactions [30, 31]. In our study, we conducted cytological studies of antitumor effects of anlotinib and raltitrexed in two VEGFR-2 positive ESCC cell lines KYSE-30 and TE-1, and we found that the combination of anlotinib and raltitrexed significantly enhanced antitumor effects compared with anlotinib and raltitrexed monotherapy.
In our study, we confirmed the proliferation inhibition effect of anlotinib and raltitrexed on human ESCC cell lines by MTS and colony formation methods, and we observed that the combination of anlotinib and raltitrexed was more effective than anlotinib and raltitrexed monotherapy groups (Figs. 1 and 2). Therefore, we believe that anlotinib combined with raltitrexed can be used as a treatment option for ESCC patients. In addition, we used wound-healing and transwell experiments to confirm that both anlotinib and raltitrexed could inhibit the migration and invasion of ESCC cells KYSE-30 and TE-1, and the inhibitory effect of the combination therapy was better than anlotinib and raltitrexed monotherapy groups (Figs. 3 and 4). In order to reveal the mechanism, we further detected the expression level of invasion-related protein MMP-9 and its mRNA transcription level by western blot and qPCR methods. The results showed that both of anlotinib and raltitrexed could inhibit the expression of MMP-9 protein and inhibit transcription, and the inhibition effect was stronger in the combination group (Figs. 6 and 7). Based on the above findings, we concluded that anlotinib inhibits the migration and invasion of human ESCC cell lines KYSE-30 and TE-1 by inhibiting the expression of MMP-9, and the addition of raltitrexed enhances the inhibitory effect of anlotinib on cell migration and invasion.
In addition, flow cytometry results showed that compared with anlotinib or raltitrexed monotherapy group, the apoptotic rate of KYSE-30 and TE-1 cells in the combination treatment group was significantly increased (Fig. 5). To further verify the results of flow cytometry, qPCR assay was used to detect the mRNA expression levels of anti-apoptotic protein Bcl-2 and pro-apoptotic proteins Bax and caspase-3. The results showed that the mRNA expression of Bcl-2 were decreased in anlotinib and raltitrexed groups. The reduction were more pronounced in the combination treatment group. On the contrary, the expression levels of Bax and caspase-3 mRNA in anlotinib or raltitrexed monotherapy groups were higher than those in the control group, and were further increased in the combination treatment group (Fig. 6). The western blot analysis showed similar results (Fig. 7). These conclusions indicated that raltitrexed could enhance the promoted apoptosis effect of anlotinib on human ESCC cell lines KYSE-30 and TE-1 by affecting the expression of apoptosis-related proteins.
Previous studies have shown that overactivation of p-Akt and p-Erk could inhibit the apoptosis of tumor cells and promote cell proliferation and invasion. In our study, we found anlotinib and raltitrexed decreased the level of p-Akt and p-Erk expression, and anlotinib combined with raltitrexed inhibited p-Akt and p-Erk expression in even greater extent (Fig. 7). Based on our findings, we believe that raltitrexed potentiates the antitumor effects of anlotinib on KYSE-30 and TE-1 cells by blocking PI3K/Akt and Ras/Erk signaling pathways.
It is well known that the histopathological types of esophageal cancer differ significantly between eastern and western countries. Adenocarcinoma is the main type in western countries, while in China, more than 95% of esophageal cancers are esophageal squamous cell carcinoma (ESCC) [2]. Therefore, due to the different biological behaviors, patients with ESCC in Chinese population should have unique treatment options and choices, which are different from esophageal adenocarcinoma. Cisplatin combined with 5-FU or paclitaxel is the standard first-line treatment for patients with advanced ESCC. However, cisplatin combined with 5-FU regimen only resulted in 5.5 months of progression-free survival (PFS) and 10 months of overall survival (OS) benefit in patients with advanced ESCC [32]. The PFS of cisplatin plus paclitaxel regimen was 6 months, and the OS was extended to 12 months. As second-line treatment options, the median PFS and OS of irinotecan and docetaxel could reached 3 months and 7.1 months, respectively [33]. There is still lack of standard treatment options for third-line and posterior treatment of ESCC. In particular, research data on the use of targeted drugs in advanced ESCC are relatively limited. In the results of the Phase II clinical trial of ALTER1102, we saw promising results with anlotinib as a second-line treatment for advanced ESCC, with an objective response rate (ORR) of 7.34%, median PFS of 3.02 months and OS of 6.11 months, respectively [34]. After the early multi-line chemotherapy, the physical condition of most patients already decline, so, the multi-target oral small molecule TKI maybe a good treatment option.
With the data described above, our study further revealed the inhibitory effect of anlotinib on ESCC cells through in vitro cytological experiments, and confirmed that the combination of raltitrexed and anlotinib could produce a synergistic effect, which provides more treatment options for ESCC posterior line treatment. From an objective point of view, limitations were still observed in our study. Firstly, our conclusions are limited to the cytological level at present. In the future, we will conduct animal experiments and further promote clinical application to verify our conclusions. The ultimate purpose of in vitro and in vivo drug research is to serve clinical treatment, so we need to pay more attention to whether the results of cytology experiments and animal experiments can be applied to clinical treatment. A case report confirmed that a 57-year-old man with recurrent ESCC after surgery, the patient had a failed immunotherapy course, but benefited from anlotinib combined with chemotherapy [nedaplatin (110 mg) and raltitrexed (4 mg) plus anlotinib (12 mg, D1-D14, Q3W)] for a fourth-line therapy. Survival after the combined therapy was greater than 19 months, and the overall patient survival was greater than 32 months [35]. The results confirmed that anlotinib combined with raltitrexed is effective in the posterior line treatment of advanced ESCC patients. Of course, more clinical cases are needed to confirm the conclusion. In addition, whether the incidence of adverse reactions increases after the combination of anlotinib and raltitrexed will be the focus of our follow-up observation. Secondly, with respect to raltitrexed increasing the antitumor efficacy of anlotinib in ESCC cells, besides the mechanism we found above, whether there are other possible underlying mechanisms is still worth further exploration in our future work. Finally, the combinatory efficacy of anlotinib and raltitrexed with other therapy methods, such as immune checkpoint inhibitors for ESCC treatment also need to be studied.
Conclusion
Our study first demonstrated that anlotinib combined with raltitrexed produced significant inhibition on cell proliferation, migration, and invasion in ESCC cell lines KYSE-30 and TE-1 by down-regulating the expression of p-Akt and p-Erk. Our results will provide an important reference for the application of targeted drugs toward ESCC, and the combination of anlotinib and raltitrexed might be a potential therapeutic mixture in ESCC patients. However, the clinical application of anlotinib and raltitrexed is hampered by the lack of clinical trial evaluation and should be studied in randomized controlled clinical trials in the future.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ESCC:
-
Esophageal squamous cell carcinoma
- TKI:
-
Tyrosine kinase inhibitor
- NSCLC:
-
Non-small cell lung cancer
- qPCR:
-
Quantitative polymerase chain reaction
- MMP-9:
-
Matrix metalloproteinases-9
- TS:
-
Thymidylate synthase
- TTP:
-
Thymidine deoxynucleoside triphosphate
- VEGFR-2:
-
Vascular endothelial growth factor receptor-2
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- ORR:
-
Objective response rate.
References
Sardaro A, Ferrari C, Carbonara R, Altini C, Lavelli V, Rubini G. Synergism between immunotherapy and radiotherapy in esophageal Cancer: an overview of current knowledge and future perspectives. Cancer Biother Radiopharm. 2021;36(2):123–32.
Yang CS, Chen XL. Research on esophageal cancer: with personal perspectives from studies in China and Kenya. Int J Cancer. 2021;149(2):264–76.
Yang YS, Hu WP, Ni PZ, Wang WP, Yuan Y, Chen LQ. Esophageal luminal stenosis is an independent prognostic factor in esophageal squamous cell carcinoma. Oncotarget. 2017;8(26):43397–405.
Jiao R, Luo H, Xu W, Ge H. Immune checkpoint inhibitors in esophageal squamous cell carcinoma: progress and opportunities. Onco Targets Ther. 2019;12:6023–32.
Wang C, Chen J, Cao W, Sun L, Sun H, Liu Y. Aurora-B and HDAC synergistically regulate survival and proliferation of lymphoma cell via AKT, mTOR and notch pathways. Eur J Pharmacol. 2016;779:1–7.
Ambrogio C, Gómez-López G, Falcone M, Vidal A, Nadal E, Crosetto N, et al. Combined inhibition of DDR1 and notch signaling is a therapeutic strategy for KRAS-driven lung adenocarcinoma. Nat Med. 2016;22(3):270–7.
Ashton S, Song YH, Nolan J, Cadogan E, Murray J, Odedra R, et al. Aurora kinase inhibitor nanoparticles target tumors with favorable therapeutic index in vivo. Sci Transl Med. 2016;8(325):325ra17.
Kakiuchi-Kiyota S, Lappin PB, Heintz C, Brown PW, Pinho FO, Ryan AM, et al. Expression of proto-oncogene cFMS protein in lung, breast, and ovarian cancers. Appl Immunohistochem Mol Morphol. 2014;22(3):188–99.
Sun Y, Niu W, Du F, Du C, Li S, Wang J, et al. Safety, pharmacokinetics, and antitumor properties of anlotinib, an oral multi-target tyrosine kinase inhibitor, in patients with advanced refractory solid tumors. J Hematol Oncol. 2016;9(1):105.
Hagner N, Joerger M. Cancer chemotherapy: targeting folic acid synthesis. Cancer Manag Res. 2010;2:293–301.
Zhao H, Zhang Y, Sun J, Zhan C, Zhao L. Raltitrexed inhibits HepG2 cell proliferation via G0/G1 cell cycle arrest. Oncol Res. 2016;23(5):237–48.
Xue S, Chen YX, Qin SK, Yang AZ, Wang L, Xu HJ, et al. Raltitrexed induces mitochondrial-mediated apoptosis in SGC7901 human gastric cancer cells. Mol Med Rep. 2014;10(4):1927–34.
van Meerbeeck JP, Gaafar R, Manegold C, Van Klaveren RJ, Van Marck EA, Vincent M, et al. Randomized phase III study of cisplatin with or without raltitrexed in patients with malignant pleural mesothelioma: an intergroup study of the European Organisation for Research and Treatment of Cancer lung Cancer group and the National Cancer Institute of Canada. J Clin Oncol. 2005;23(28):6881–9.
Planting A, de Jong M, Jansen P, Kerrebijn J, Smith M, Verweij J. Phase I study of concomitant chemoradiation with raltitrexed in locally advanced head and neck cancer. Eur J Cancer. 2005;41(1):93–7.
Olsson AK, Dimberg A, Kreuger J, Claesson-Welsh L. VEGF receptor signalling - in control of vascular function. Nat Rev Mol Cell Biol. 2006;7(5):359–71.
Fontanella C, Ongaro E, Bolzonello S, Guardascione M, Fasola G, Aprile G. Clinical advances in the development of novel VEGFR2 inhibitors. Ann Transl Med. 2014;2(12):123.
Xie C, Wan X, Quan H, Zheng M, Fu L, Li Y, et al. Preclinical characterization of anlotinib, a highly potent and selective vascular endothelial growth factor receptor-2 inhibitor. Cancer Sci. 2018;109(4):1207–19.
Tsunedomi R, Yoshimura K, Kimura Y, Nishiyama M, Fujiwara N, Matsukuma S, et al. Elevated expression of RAB3B plays important roles in chemoresistance and metastatic potential of hepatoma cells. BMC Cancer. 2022;22(1):260.
Li L, Liang Y, Kang L, Liu Y, Gao S, Chen S, et al. Transcriptional regulation of the Warburg effect in Cancer by SIX1. Cancer Cell. 2018;33(3):368–385.e7.
Roskoski R Jr. Targeting oncogenic Raf protein-serine/threonine kinases in human cancers. Pharmacol Res. 2018;135:239–58.
Xu WW, Li B, Lam AK, Tsao SW, Law SY, Chan KW, et al. Targeting VEGFR1- and VEGFR2-expressing non-tumor cells is essential for esophageal cancer therapy. Oncotarget. 2015;6(3):1790–805.
Li H, Juan L, Xia L, Wang Y, Bao Y, Sun G. Thioridazine sensitizes esophageal carcinoma cell lines to radiotherapy-induced apoptosis in vitro and in vivo. Med Sci Monit. 2016;22:2624–34.
Zhen H, Li G, Zhao P, Zhang Y, Wang J, Yu J, et al. Raltitrexed enhances the antitumor effect of Apatinib in human esophageal squamous carcinoma cells via Akt and Erk pathways. Onco Targets Ther. 2020;13:12325–39.
Wu J, Yu J, Wang J, Zhang C, Shang K, Yao X, et al. Astragalus polysaccharide enhanced antitumor effects of Apatinib in gastric cancer AGS cells by inhibiting AKT signalling pathway. Biomed Pharmacother. 2018;100:176–83.
Ma Y, Yu J, Li Q, Su Q, Cao B. Addition of docosahexaenoic acid synergistically enhances the efficacy of apatinib for triple-negative breast cancer therapy. Biosci Biotechnol Biochem. 2020;84(4):743–56.
Hong OY, Jang HY, Lee YR, Jung SH, Youn HJ, Kim JS. Inhibition of cell invasion and migration by targeting matrix metalloproteinase-9 expression via sirtuin 6 silencing in human breast cancer cells. Sci Rep. 2022;12(1):12125.
Qiu H, Li J, Liu Q, Tang M, Wang Y. Apatinib, a novel tyrosine kinase inhibitor, suppresses tumor growth in cervical cancer and synergizes with paclitaxel. Cell Cycle. 2018;17(10):1235–44.
Ferrara N, Adamis AP. Ten years of anti-vascular endothelial growth factor therapy. Nat Rev Drug Discov. 2016;15(6):385–403.
Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9(6):669–76.
Kelly C, Bhuva N, Harrison M, Buckley A, Saunders M. Use of raltitrexed as an alternative to 5-fluorouracil and capecitabine in cancer patients with cardiac history. Eur J Cancer. 2013;49(10):2303–10.
Saif MW, Shah MM, Shah AR. Fluoropyrimidine-associated cardiotoxicity: revisited. Expert Opin Drug Saf. 2009;8(2):191–202.
Hayashi K, Ando N, Watanabe H, Ide H, Nagai K, Aoyama N, et al. Phase II evaluation of protracted infusion of cisplatin and 5-fluorouracil in advanced squamous cell carcinoma of the esophagus: a Japan esophageal oncology group (JEOG) trial (JCOG9407). Jpn J Clin Oncol. 2001;31(9):419–23.
Kojima T, Shah MA, Muro K, Francois E, Adenis A, Hsu CH, et al. Randomized phase III KEYNOTE-181 study of Pembrolizumab versus chemotherapy in advanced esophageal Cancer. J Clin Oncol. 2020;38(35):4138–48.
Huang J, Xiao J, Fang W, Lu P, Fan Q, Shu Y, et al. Anlotinib for previously treated advanced or metastatic esophageal squamous cell carcinoma: a double-blind randomized phase 2 trial. Cancer Med. 2021;10(5):1681–9.
Yang D, Xu F, Lai X, Li Y, Gao H, Xu Y, et al. Combined treatment with anlotinib and chemotherapy for advanced esophageal squamous cell carcinoma improved patient survival: a case report. Am J Transl Res. 2020;12(10):6578–83.
Acknowledgements
Thanks for the help of the members of the cancer center in Beijing Friendship Hospital, Capital Medical University.
Funding
This work was supported by grants from National Natural Science Foundation of China, Grant/Award Number: 82173056; Beijing Natural Science Foundation, Grant/Award Number: 7222032; The capital health research and development of special: Grant/Award Number: 2022–2-1113.
Author information
Authors and Affiliations
Contributions
H.C.Z. and B.W.C. designed experiments, J.Z.T. and G.X.L. performed the experiments, P.F.Z. made the acquisition of data, Y.Z. and J.J.C. did the analysis and interpretation of data, and H.C.Z. wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All the authors declared that they had no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhen, H., Tian, J., Li, G. et al. Raltitrexed enhanced antitumor effect of anlotinib in human esophageal squamous carcinoma cells on proliferation, invasiveness, and apoptosis. BMC Cancer 23, 207 (2023). https://doi.org/10.1186/s12885-023-10691-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-10691-y